Abstract
Background
Foods high in fat, sugar and salt (HFSS) are known to contribute to overweight and obesity. In addition to overweight and obesity, smoking, alcohol consumption and physical inactivity are known risk factors for non-communicable diseases, including several cancers and cardiovascular disease.
Methods
Secondary analysis of UK-representative cross-sectional survey data of 3293 adults aged 18+. Regression analyses were undertaken to understand the relationship between consumption of HFSS food and soft drinks, alcohol and tobacco and socio-demographics. Clustering analysis identified groupings of health risk factors.
Results
Males, those aged 18–24 and those from the more deprived groups consumed ready meals and fast food most frequently. Most of the sample (77.3%) engaged in at least one health risk behaviour. Six clusters were identified in the clustering analysis. Older (65+) female respondents were more likely to be inactive. Smokers exhibiting additional risk behaviours were more likely to be of working age from more deprived groups, and men over 65 were more likely to consume harmful levels of alcohol with additional risk factors.
Conclusion
Policies and services in the UK tend to focus on changing behaviour to address individual risk factors. This study shows that policies and interventions need to address multiple risk factors.
Keywords: alcohol consumption, obesity, physical activity
Background
Health risk factors such as overweight/obesity, poor nutrition, smoking, alcohol consumption and low levels of physical activity each make a significant contribution to a number of non-communicable diseases (NCDs) including some types of cancer,1–7 diabetes4,7,8 and cardiovascular disease.7–9
Since the 1930s, policies have been developed regulate the availability of tobacco and alcohol products in the UK.10 Progress continues to be made to reduce the number of individuals who engage in tobacco or harmful alcohol use in the UK, such as through age and marketing restrictions, to minimize advertising exposure to young people.10–12 Smoking prevalence has fallen following policy interventions, such tobacco taxes, mass media campaigns and the introduction of smoke-free workplaces.13 England has seen general declines in alcohol consumption among young people.14 The introduction of minimum unit pricing in Scotland may encourage further declines in alcohol consumption, particularly among heavy drinkers.15,16
Fewer policies have been introduced to address rising levels of obesity in the UK, aside from the recently announced Soft Drink Industry Levy.17 This could be due to obesity being a complex health issue with no single contributing factor.18 McKinsey19 outlined some potential interventions. These measures included restrictions on the numbers of fast food outlets; food and drink reformulation; and restrictions on junk food advertising.19 One of the known major contributing factors to weight gain is consumption of foods high in fat, sugar and salt (HFSS), such as fast food,20 ready meals, soft drinks and confectionary.21 If implemented, these policies need to consider their contribution to health inequalities, as individuals living in areas of greater deprivation are more likely to have a higher BMI.22
Evidence has shown that populations who engage in multiple risk factors tend to have significantly worse health outcomes than those engaging in one health risk behaviour.23 Identifying groups of individuals whose health is affected by multiple risk factors provides insight to where policies need to be targeted to reduce inequalities in health.24,25
Clustering analysis identifies how different behaviours occur alongside each other and where in a particular population they may occur. Two recent systematic reviews have considered the clustering of multiple health risk factors. Noble et al.,26 took a global perspective, finding that more than half of studies found alcohol and smoking clustered together whilst a health found smoking, nutrition, alcohol and physical inactivity all clustered together. Meanwhile, Meader et al.,27 focused on literature from the UK. Meader et al., found that alcohol and smoking consistently grouped in the study samples, and a strong association was also found between socioeconomic status and health risk behaviours. The principle limitation of the review was that the studies included were not representative of the UK population.
Studies which have considered consumption of HFSS food and drink as a behavioural risk factor have not previously considered this within a UK-wide population.28–31 This study aims to provide new data on this issue by describing the frequency of fast food and takeaways, ready meals, confectionary and soft drink consumption between population groups. Additionally, it examines the clustering of health risk behaviours: smoking, alcohol consumption, physical inactivity and overweight/obesity in adults in the UK to provide information that could inform more refined targeting of health policies and interventions.
Methods
This study was a secondary analysis of data collected in February 2016 as previously described in Hooper et al.32 Data were collected from an online cross-sectional survey of 3490 adults aged 18 and over recruited by market research company, YouGov. A total of 3293 (94%) complete responses to the survey were received.
Demographics
Demographic information for the respondents were held by YouGov and included: gender, age and region of residence (England, Scotland, Wales and Northern Ireland). Four groups from the National Readership Survey system for socio-economic status (SES) classification were used by YouGov. They were: AB (higher and intermediate managerial, administrative, professional occupations), C1 (supervisory, clerical and junior managerial, administrative and professional), C2 (skilled manual worker) and DE (semi-skilled and unskilled manual occupations, unemployed and lowest grade occupations).
Body mass index (BMI) was calculated from respondent self-reported weight and height (kg/m2). The following categories were used: underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2) and obese (>30 kg/m2).33 Underweight and normal were coded as not having weight as a health risk factor, while the overweight and obese categories were coded as having the risk factor.
Health behaviours
Questions were asked about four additional health behaviours: diet, smoking, alcohol and physical activity.
Diet
Consumption of food high in fat was estimated by asking about the consumption frequency of fast food and ready meals. Questions asked were: ‘How often do you have food….—From takeaway places like McDonalds, Burger King, Pizza Hut, KFC or local takeaway food places?’ and ‘How often do you have food….—At home such as ready meals, burgers, pizza, or chips?’. Participants could answer: two to three times a day; once a day, 5–6 times a week; 2–4 times a week; once a week; 1–3 times a month; < once or a month; and never. Responses were coded as either ‘at least once a week’ or ‘less than once a week’ for each category.
The consumption of sugar-sweetened beverages and food that are high in sugar was estimated by asking: ‘How often do you …—Drink soft drinks such as cola, cordials, sports drinks or energy drinks (do not include sugar free drinks)?’ and ‘How often do you …—Eat confectionery (such as sweets and chocolates), cakes, muffins, sweet pies, pastries or biscuits?’. Participants could answer: >6 times a day; 4–5 times a day; 2–3 times a day; once a day; 5–6 times a week; 2–4 times a week; once a week; 1–3 times a month; < once a month; and never. Responses were coded as ‘once a day or more’ and ‘less than once a day’.
Smoking
Smoking status was defined from: ‘I have never smoked’; ‘I used to smoke but haven given up now’; ‘I smoke but I don’t smoke every day’ and ‘I smoke every day’. The first two responses were coded as not having smoking as a risk factor; those who gave the latter two responses were coded as having smoking as a risk factor, in line with published studies.34,35
Alcohol consumption
Weekly alcohol consumption was estimated by asking ‘how often do you have a drink containing alcohol?’ and ‘how many units of alcohol do you drink on a typical day when you are drinking?’. The respondents were then classified as either ‘low-risk drinkers’ (consume 14 or less units of alcohol per week) or ‘increased-risk drinkers’ (more than 14 units per week), with those in the latter category coded as having alcohol consumption as a risk factor. These categories were based on current UK Chief Medical Officers’ recommendations on low-risk drinking.36
Physical activity
Physical activity level questions were taken from the short-form International Physical Activity Questionnaire (IPAQ).37 Respondents were asked three questions—for how many hours and minutes did they partake in: vigorous activity, moderate activity and walking. Respondents were classed as ‘Inactive’, ‘Minimally active’ or ‘Highly active’. For analysis, the latter two categories were merged, and those who were ‘Inactive’ were coded as having physical inactivity as a risk factor.
All risk factors were coded as 0 for no risk and 1 for having that risk factor.
Analysis
IBM SPSS Version 24 was used to analyse the data. Age, gender, socioeconomic status and region were weighted to ensure the results were representative of the population. The weighting was provided by YouGov and counteracted the under-representation of those aged 18–34, residents from England and those from a DE socioeconomic group (as shown in Supplementary Table SI). Unless specified, weighted results are presented.
Cross-tabulations were undertaken to produce descriptive statistics between the diet, alcohol and smoking risk factor variables and the demographic variables. Binary logistic regression—chi-square analysis—was performed to explore relationships between the risk factor variables.
Clustering analysis was performed on unweighted data to identify behaviour patterns. Health risk factors included in the clustering analysis were: smoking, alcohol consumption, physical inactivity and overweight/obesity (BMI). BMI was included as a proxy for diet as there is little indication in the literature around what level of consumption of ready meals, takeaways, soft drinks or confectionary constitutes a risk to health.
As the sample size was more than 1000 participants, the Two-Step Cluster method was chosen.38 Automated cluster selection was used to determine the number of clusters formed. An average silhouette coefficient was produced to determine how well each case within a cluster matched to each other and how separate each cluster was from the other clusters.38 Additional regression analyses were conducted to test for associations between clusters and demographic variables.
Results
Data for gender, age, nation of residence and socioeconomic status were available for all 3293 respondents. A total of 259 respondents (7.8%) of the unweighted sample (290 (8.8%) of the weighted sample) did not provide height and weight details, so their BMI could not be calculated. These cases were subsequently excluded from the analysis. See Supplementary Table SI for further details.
Males were significantly more likely to consume ready meals and fast food at least once a week, consume soft drinks at least once a day, and consume more than 14 units of alcohol per week. Females were significantly more likely to be physically inactive (shown in Tables 1 and 2).
Table 1.
Multiple regression of convenience food and sugar-sweetened soft drinks
| Ready meals | Fast food and takeaways | Confectionary | Soft drinks | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| At least once a week (%) | OR | CI | At least once a week (%) | OR | CI | At least once a day (%) | OR | CI | At least once a day (%) | OR | CI | |
| Total | 49.9 | 16.0 | 17.4 | 40.4 | ||||||||
| Gender | ||||||||||||
| Male (n = 1604) | 55.6 | – | – | 19.3 | – | – | 42.0 | – | – | 20.3 | – | – |
| Female (n = 1690) | 44.4 | 0.603** | 0.519–0.700 | 12.9 | 0.602** | 0.489–0.741 | 39.0 | 0.936 | 0.807–1.086 | 14.7 | 0.644** | 0.526–0.788 |
| Age | ||||||||||||
| 18–24 (n = 283) | 61.1 | – | – | 27.6 | – | – | 49.1 | – | – | 23.0 | – | – |
| 25–34 (n = 631) | 54.5 | 0.780 | 0.573–1.062 | 26.3 | 1.052 | 0.743–1.491 | 45.2 | 0.835 | 0.631–1.152 | 23.3 | 1.103 | 0.755–1.612 |
| 35–44 (n = 571) | 56.6 | 0.802 | 0.584–1.101 | 21.2 | 0.728 | 0.504–1.053 | 43.5 | 0.795 | 0.584–1.083 | 22.4 | 0.979 | 0.662–1.448 |
| 45–54 (n = 562) | 54.4 | 0.736 | 0.533–1.014 | 14.9 | 0.460** | 0.310–0.683 | 38.1 | 0.653* | 0.476–0.895 | 20.5 | 0.795 | 0.530–1.190 |
| 55–64 (n = 510) | 45.5 | 0.480** | 0.347–0.664 | 9.4 | 0.269** | 0.174–0.415 | 32.9 | 0.521** | 0.377–0.720 | 10.4 | 0.368** | 0.235–0.578 |
| 65+ (n = 736) | 35.7 | 0.326** | 0.239–0.444 | 4.2 | 0.098* | 0.059–0.162 | 37.6 | 0.635* | 0.470–0.858 | 8.7 | 0.309** | 0.201–0.476 |
| Social grade | ||||||||||||
| AB (n = 725) | 47.2 | – | – | 13.1 | – | – | 41.6 | – | – | 14.9 | – | – |
| C1 (n = 988) | 49.4 | 0.972 | 0.789–1.198 | 18.1 | 1.175 | 0.872–1.583 | 43.0 | 1.009 | 0.820–1.241 | 16.3 | 0.892 | 0.664–1.197 |
| C2 (n = 494) | 54.3 | 1.359* | 1.063–1.738 | 19.0 | 1.681* | 1.195–2.364 | 41.5 | 1.012 | 0.793–1.292 | 19.0 | 1.266 | 0.906–1.769 |
| DE (n = 1087) | 50.1 | 1.198 | 0.975–1.471 | 14.6 | 1.237 | 0.913–1.677 | 36.8 | 0.869 | 0.708–1.067 | 19.3 | 1.370* | 1.034–1.816 |
| BMI | ||||||||||||
| Underweight (n = 85) | 49.4 | – | – | 16.5 | – | – | 35.3 | – | – | 23.5 | – | – |
| Normal weight (n = 1327) | 49.3 | 0.953 | 0.606–1.498 | 14.6 | 0.858 | 0.462–1.594 | 42.7 | 1.418 | 0.891–2.254 | 12.8 | 0.444* | 0.258–0.763 |
| Overweight (n = 944) | 46.9 | 0.910 | 0.574–1.442 | 14.8 | 1.096 | 0.583–2.060 | 39.5 | 1.321 | 0.823–2.118 | 15.4 | 0.612 | 0.353–1.063 |
| Obese (648) | 57.3 | 1.416 | 0.886–2.264 | 20.7 | 1.719 | 0.909–3.250 | 38.3 | 1.278 | 0.790–2.069 | 25.3 | 1.154 | 0.664–2.005 |
| Nation | ||||||||||||
| England (n = 2762) | 49.1 | – | – | 15.5 | – | – | 39.3 | – | – | 16.4 | – | – |
| Wales (n = 158) | 55.1 | 1.098 | 0.773–1.558 | 18.4 | 1.045 | 0.663–1.645 | 43.0 | 1.050 | 0.744–1.480 | 24.7 | 1.391 | 0.912–2.122 |
| Scotland (n = 280) | 52.1 | 1.025 | 0.787–1.336 | 16.1 | 0.910 | 0.632–1.309 | 48.2 | 1.438* | 1.110–1.863 | 21.1 | 1.278 | 0.919–1.777 |
| Northern Ireland (n = 92) | 56.5 | 1.261 | 0.805–1.975 | 26.1 | 1.796* | 1.066–3.025 | 46.7 | 1.311 | 0.848–2.025 | 23.9 | 1.617 | 0.957–2.733 |
SES: AB is managerial/professional roles, C1 supervisory and clerical roles, C2 skilled manual workers, DE semi-skilled, unskilled and unemployed.
*P < 0.05, **P < 0.005.
Table 2.
Multiple regression of tobacco, alcohol and physical inactivity risk factors
| Tobacco use | Alcohol consumption | Physically inactive | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Current smoker (%) | OR | CI | Consume >14 units per week (%) | OR | CI | Not minimally active (%) | OR | CI | |
| Total | 14.6 | 15.3 | 33.9 | ||||||
| Gender | |||||||||
| Male (n = 1604) | 15.8 | – | – | 23.1 | – | – | 29.0 | – | – |
| Female (n = 1690) | 13.6 | 0.826 | 0.673–1.013 | 7.9 | 0.292** | 0.233–0.365 | 38.6 | 1.584** | 1.348–1.852 |
| Age | |||||||||
| 18–24 (n = 283) | 16.3 | – | – | 9.9 | – | – | 20.5 | – | – |
| 25–34 (n = 631) | 14.6 | 0.932 | 0.622–1.397 | 11.0 | 0.993 | 0.614–1.607 | 30.4 | 1.641* | 1.123–2.398 |
| 35–44 (n = 571) | 17.5 | 1.124 | 0.747–1.692 | 13.5 | 1.314 | 0.813–2.125 | 33.8 | 1.851* | 1.261–2.718 |
| 45–54 (n = 562) | 15.8 | 0.936 | 0.632–1.465 | 18.3 | 1.976* | 1.229–3.178 | 37.5 | 2.104** | 1.430–3.095 |
| 55–64 (n = 510) | 17.6 | 1.045 | 0.686–1.592 | 19.7 | 2.137* | 1.326–3.443 | 31.8 | 1.634* | 1.103–2.422 |
| 65+ (n = 736) | 8.8 | 0.508* | 0.330–0.782 | 17.0 | 1.757* | 1.104–2.795 | 40.9 | 2.529** | 1.746–3.663 |
| Social grade | |||||||||
| AB (n = 725) | 10.2 | – | – | 17.7 | – | – | 32.0 | – | – |
| C1 (n = 988) | 12.2 | 1.195 | 0.869–1.645 | 17.4 | 1.084 | 0.824–1.425 | 29.9 | 0.915 | 0.728–1.151 |
| C2 (n = 494) | 17.0 | 1.757* | 1.238–2.492 | 15.6 | 0.886 | 0.638–1.232 | 34.8 | 1.113 | 0.855–1.449 |
| DE (n = 1087) | 18.6 | 2.046** | 1.517–2.758 | 11.6 | 0.675* | 0.508–0.897 | 38.5 | 1.182 | 0.949–1.472 |
| BMI | |||||||||
| Underweight (n = 85) | 9.9 | – | – | 10.6 | – | – | 37.6 | – | – |
| Normal weight (n = 1327) | 16.9 | 1.810 | 0.869–3.770 | 14.2 | 1.230 | 0.590–2.566 | 25.5 | 0.562* | 0.351–0.897 |
| Overweight (n = 944) | 12.4 | 1.284 | 0.607–2.713 | 19.1 | 1.383 | 0.659–2.903 | 28.8 | 0.655 | 0.407–1.056 |
| Obese (648) | 16.0 | 1.623 | 0.765–3.447 | 15.0 | 1.168 | 0.549–2.487 | 54.3 | 1.859* | 1.149–3.007 |
| Nation | |||||||||
| England (n = 2762) | 14.4 | – | – | 15.6 | – | – | 33.5 | – | – |
| Wales (n = 158) | 15.2 | 1.069 | 0.673–1.699 | 12.7 | 0.925 | 0.558–1.533 | 40.5 | 1.358 | 0.943–1.954 |
| Scotland (n = 280) | 14.3 | 0.908 | 0.628–1.312 | 13.9 | 0.882 | 0.608–1.280 | 31.5 | 0.854 | 0.638–1.143 |
| Northern Ireland (n = 92) | 20.7 | 1.465 | 0.856–2.508 | 12.0 | 0.693 | 0.352–1.366 | 42.4 | 1.559 | 0.987–2.462 |
SES: AB is managerial/professional roles, C1 supervisory and clerical roles, C2 skilled manual workers, DE semi-skilled, unskilled and unemployed.
*P < 0.05, **P < 0.005.
Younger individuals aged 18–24 were more likely to consume: ready meals at least once a week compared to respondents aged 55–65+; fast food at least once a week and confectionary at least once a day compared to those aged 45–65+; soft drinks at least once a day compared to those aged 55–65+ and be more likely to be a current smoker than adults aged 65+. Individuals aged 18–24 were less likely to consume more than 14 units of alcohol in a week than those aged 45–65+; and were less likely to be physically inactive compared to all other age groups (Tables 1 and 2).
Differences also exist between socioeconomic groupings in relation to consumption behaviours. Individuals in the managerial (AB) category were less likely to consume ready meals at least once a week compared to skilled manual workers (C2); consume fast food and takeaways at least once a week than skilled manual workers (C2); consume soft drinks at least once a day relative to unskilled/unemployed (DE) individuals; and were more likely to smoke than skilled manual workers (C2) or unskilled/unemployed (DE) individuals. Meanwhile, individuals in the managerial (AB) group were more likely to consume more than 14 units of alcohol per week compared to unskilled/unemployed (DE) individuals.
Respondents from England were less likely to consume fast food and takeaways at least once a week than those from Northern Ireland, and less likely to consume confectionary at least once a day than those from Scotland.
Risk factors
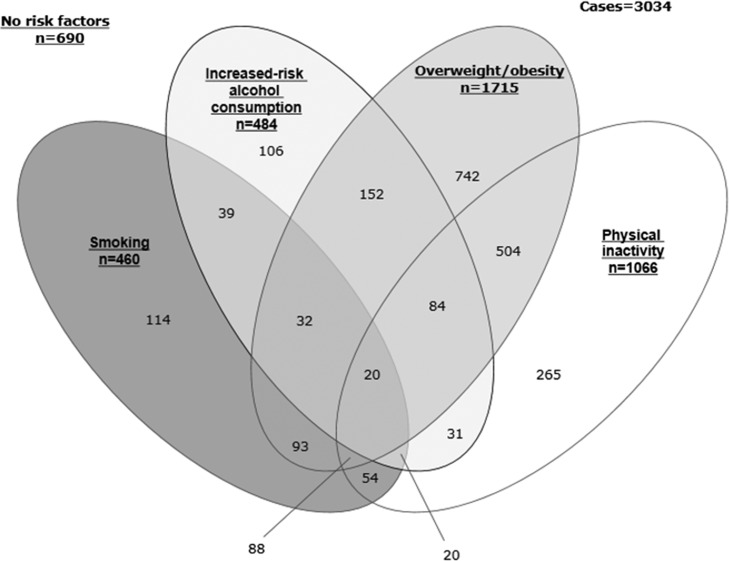
Unweighted data were used to consider the distribution of risk factors. Of the 3034 eligible participants: 690 (22.7%) presented none of the risk factor behaviours; 1227 (40.4%) presented a single risk factor; 873 (28.8%) presented two; 224 (7.4%) presented three; and 20 (0.7%) presented all four risk factor behaviours (Fig. 1).
Fig. 1.
Distribution of risk factors.
Clustering of risk factors
A total of 3034 cases were included in the cluster analysis; 259 cases were excluded prior to the cluster analysis as BMI could not be calculated due to height and weight data not being provided. This analysis produced six clusters. The average silhouette measure of cohesion and separation was 0.8, demonstrating the quality of the clusters is good. The ratio of the largest cluster (cluster 2) to the smallest cluster (cluster 6) was 2.80:1. Descriptions of the clusters are outlined below:
Cluster 1: No risk factors
A total of 690 individuals (22.7%) presenting no risk factors made up this cluster. In total, 32.7% were males. Of the different age categories: 13.9% were 18–24, 27.2% were 25–34, 15.8% were 35–44, 11.7% were 45–54, 12.4% were 55–64 and 19.0% were 65+. This cluster was used as the reference category in the regression analysis.
Cluster 2: Overweight/obese, otherwise low risk
This cluster included 742 (24.5%) individuals, all exclusively only having overweight/obese as a risk-factor. Those in this cluster are: more likely to be male and be aged 65+ than 18–24 or 25–34.
Cluster 3: Inactive and overweight/obese
All individuals (504, 16.6%) only had physical inactivity and overweight/obese risk factors present. Both age and socioeconomic differences are present in this cluster. Individuals are more likely to be aged 65+ than 18–24, 25–34 or 35–44, and are more likely to belong to the C2 socioeconomic category than DE.
Cluster 4: Multiple risk factors (increased-risk alcohol)
In this cluster of 484 (16.0%) cases, all cases were in the increased-risk category for alcohol, 59.5% were overweight/obese, 32% were physically inactive and 22.9% smoked. Individuals in this cluster are more likely to be male and aged 65+ rather than 18–24 or 25–34.
Cluster 5: Multiple risk factors (smoking)
Overall, 349 (11.5%) individuals made up this cluster. All the individuals smoked, 51.9% were overweight or obese and 40.7% were physically inactive. None of the individuals in this cluster had alcohol consumption as a risk factor. Individuals in this cluster were more likely to be in the 35–44, 45–54 or 55–64 age categories than in the 65+ category. Socioeconomic differences were also present; individuals are more likely to belong to the DE category than to either the AB or C1 categories.
Cluster 6: inactive
This cluster contained 265 (8.7%) cases, all of which only had physical inactivity as a risk factor. Individuals are more likely to be female, and be aged 65+ rather than 18–24, 25–34 and 55–64 (shown in full in Table 3).
Table 3.
Multiple regression of the cluster variable
| Healthy, low risk (reference) | Overweight/obese, otherwise low risk | Inactive and overweight/obese | Multiple risk factors (Increased-risk alcohol) | Smoking | Physically inactive | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 | Cluster 5 | Cluster 6 | |||||||
| OR | CI | OR | CI | OR | CI | OR | CI | OR | CI | OR | CI | |
| Gender | ||||||||||||
| Male (n = 1604) | 1.487** | 1.205–1.834 | 0.943 | 0.740–1.203 | 3.830** | 2.968–4.942 | 1.287 | 0.992–1.669 | 0.643* | 0.481–0.860 | ||
| Female (n = 1690) | – | – | – | – | – | – | – | – | – | – | ||
| Age | ||||||||||||
| 18–24 (n = 283) | 0.293** | 0.189–0.455 | 0.118** | 0.062–0.225 | 0.284** | 0.172–0.467 | 0.921 | 0.557–1.522 | 0.576* | 0.344–0.966 | ||
| 25–34 (n = 631) | 0.477** | 0.345–0.660 | 0.328** | 0.227–0.475 | 0.352** | 0.240–0.515 | 0.927 | 0.604–1.424 | 0.641* | 0.423–0.972 | ||
| 35–44 (n = 571) | 0.913 | 0.651–1.279 | 0.554* | 0.376–0.819 | 0.692 | 0.469–1.022 | 1.572* | 1.009–2.450 | 1.231 | 0.807–1.876 | ||
| 45–54 (n = 562) | 1.343 | 0.947–1.905 | 1.057 | 0.724–1.542 | 1.332 | 0.904–1.964 | 1.779* | 1.122–2.822 | 1.012 | 0.632–1.621 | ||
| 55–64 (n = 510) | 1.117 | 0.786–1.588 | 0.887 | 0.606–1.298 | 1.246 | 0.849–1.830 | 1.876* | 1.197–2.941 | 0.411* | 0.230–0.734 | ||
| 65+ (n = 736) | – | – | – | – | – | – | – | – | – | – | ||
| Social grade | ||||||||||||
| AB (n = 725) | 0.958 | 0.717–1.279 | 1.043 | 0.755–1.442 | 1.315 | 0.944–1.833 | 0.465** | 0.319–0.678 | 0.798 | 0.539–1.183 | ||
| C1 (n = 988) | 1.004 | 0.768–1.312 | 0.829 | 0.604–1.137 | 1.410 | 1.032–1.927 | 0.528** | 0.379–0.736 | 0.831 | 0.583–1.186 | ||
| C2 (n = 494) | 1.339 | 0.983–1.881 | 1.479* | 1.017–2.150 | 1.620 | 1.094–2.398 | 1.043 | 0.705–1.543 | 1.435 | 0.936–2.200 | ||
| DE (n = 1087) | – | – | – | – | – | – | – | – | – | – | ||
| Nation | ||||||||||||
| England (n = 2762) | 0.833 | 0.422–1.644 | 0.555 | 0.273–1.129 | 1.038 | 0.465–2.320 | 0.491 | 0.241–0.998 | 0.673 | 0.297–1.526 | ||
| Wales (n = 158) | 1.117 | 0.485–2.569 | 1.193 | 0.502–2.838 | 1.267 | 0.475–3.382 | 0.639 | 0.257–1.577 | 0.749 | 0.267–2.103 | ||
| Scotland (n = 280) | 1.085 | 0.511–2.301 | 0.569 | 0.252–1.286 | 0.982 | 0.401–2.403 | 0.487 | 0.213–1.111 | 0.533 | 0.205–1.386 | ||
| Northern Ireland (n = 92) | – | – | – | – | – | – | – | – | – | – | ||
SES: AB is managerial/professional roles, C1 supervisory and clerical roles, C2 skilled manual workers, DE semi-skilled, unskilled and unemployed.
* P < 0.05, **P < 0.005
Discussion
This study used a UK-wide population representative sample to measure ready meal, fast food and takeaway, confectionary and soft drink consumption and to assess the clustering of preventable risk factors for NCDs. Males reported more frequent consumption of ready meals, fast food and takeaways and soft drinks than females. This is consistent with previous research indicating females are more likely to avoid energy dense foods.39 Despite this, males were less likely to be physically inactive, consistent with global trends.40
Socioeconomic differences existed across consumption behaviours as those from lower socioeconomic categories were more likely to consume convenience foods and be a current smoker than those from the highest socioeconomic group (AB). As there are a higher proportion of fast food outlets in areas of socioeconomic deprivation in the UK,41 this may provide an environment for those who are more deprived to consume more food that is HFSS than those who are less deprived. Previous data have shown that those who live closer to fast food outlets are known to consume more fast food and are likely to have a higher BMI.20
Clustering analysis was performed to identify groups of individuals within the population that engage in behaviours or have a BMI level which is overweight/obese that impacts on mortality and morbidity. We sought to identify populations who engage in multiple health risk behaviours and have overweight/obese BMI that could be at greatest need of targeted public health interventions. Six clusters were formed, with some similarity between groups, especially for clusters 4 and 5. Individuals in these groups exhibit multiple risk factors and represent the greatest potential for targeted health policies. Cluster 4 (Multiple risk factors (increased-risk alcohol), 16.0%, n = 484) contained respondents who were at increased-risk alcohol consumption as a risk factor, supporting data from the Office for National Statistics which suggests older individuals are more likely to drink more frequently.42 Respondents in cluster 5 (Multiple risk factors (smoking)) show similar characteristics to those in cluster 4, with the main behavioural differences being that all respondents in cluster 5 smoked, but none had increased-risk alcohol consumption as a risk factor. The differences between clusters 4 and 5 could be explained by demographic differences. Those in cluster 4 were more likely to be male and be of retirement age (65+ rather than 18–24 or 25–34) compared to individuals with no risk factors (cluster 1). Individuals in cluster 5 were more likely to be of working age (35–64 than 65+) and be classified in a lower socioeconomic group (DE versus AB or C1). This is consistent with previous research which has found that the most disadvantaged were more likely to smoke than the most advantaged.43,44
Cases from clusters 2–5 were more likely to be male, and generally had an age profile indicative of being at least in mid-life. Almost regardless of whichever risk factor an individual had and what that co-occurred with, older men appeared to be more likely to have all the health risk behaviours. This is contradictory to Noble et al. and Meader et al., who found ambiguous associations between gender, age and behavioural clustering. One cause could be limited health knowledge, so novel strategies may be effective in engaging older males, increasing awareness and improving health behaviours.45 Similarly, other factors not included in this study such as partnership status35,46,47 may contribute to the association.
What is already known about the topic
Recent data on consumption of sugar-sweetened soft drinks in the UK have been collected in the National Diet and Nutrition Survey.48 However, few data exist around the consumption of convenience foods such as ready meals and takeaways, and sweet confectionary items. Data on these can improve understanding of dietary factors that contribute to overweight and obesity.
Systematic reviews have been conducted into the clustering or co-occurrence of health risk behaviours. One took a worldwide perspective,26 whilst the other focused on literature solely from the UK.27 The latter review found that most studies considered clustering between two health risk factors; few considered three or more risk factors. Most of the current clustering literature considers clustering between only two risk factors.27 Some studies have considered the clustering of health risk behaviours amongst different adult populations within the UK,35,49–51 while only a single study used a UK-wide sample.52 However, whilst this previous study examined four risk factors, only two were general lifestyle risk factors—smoking and sugar consumption. The remaining two risk factors studied were specific to dental hygiene.
What the study adds
This study is the first to assess UK-wide consumption of ready meals, fast food and takeaways, and sweet confectionary to better understand dietary factors that may contribute to overweight and obesity. Additionally, the study considers the clustering of multiple health risk behaviours as well as BMI across a UK-wide population representative sample. Previously using BMI as a risk factor in this context has only been performed in a non-UK sample.53
Limitations of the study
The nature of secondary data analysis means available variables may limit the analyses that can be conducted, and comparisons made. For example, no data were collected about fruit and vegetable consumption. As much of the existing literature identifies consuming less than five portions as having a poor diet,35,50,51 it may limit the comparisons between this and other studies. The addition of long term outcome data would increase validity to the findings of this study by furthering understanding of how lifestyle choices affect health, but this was beyond the scope of this study.
Whilst the weighted data ensured that the results of the consumption variables analyses were population representative, unweighted data were used for the clustering analysis. Therefore, the results of the clustering analysis may not be truly representative of the UK population. A further limitation of the clustering analyses was the binary coding of variables, as this approach may have prevented certain groupings from emerging in the clustering analysis.
The risk behaviours and BMI data used in the analyses were self-reported by the participants. This could explain why no association was observed between diet and BMI, as respondents may have underestimated either their weight or diet leading to an insignificant association to be observed. Similarly, as the data were cross-sectional they may only reflect the moment in time they were collected.
Implications
Those from more deprived groups are more likely to consume HFSS foods than those from less deprived groups, yet fast food outlet density is highest in deprived areas. Planning laws could be better applied to consider the make-up and health of the local population. Further, older people and those indicating multiple risk factor behaviours are at highest risk of diseases such as heart disease and some cancers. Policies and interventions may need to better target populations at highest risk; including consideration of how to address the clustering of multiple risk factors in particular populations.
This study found that certain groups in the population, especially older males, are at risk from several health risk factors such as smoking, excessive alcohol consumption, physical inactivity and overweight/obesity. Therefore, policies need to target this particular group to prevent the occurrence of many NCDs.
Supplementary Material
Conflict of interest
None.
Supplementary data
Supplementary data are available at the Journal of Public Health online.
Contributors
JB designed the study, analysed the data, interpreted the results and contributed to the article preparation. RP contributed to the study design, analysing the data, results interpretation and article preparation. LH contributed to analysing the data, results interpretation and contributed to the article preparation. LB, GR and JV contributed to the study design and article preparation.
Funding
This research was supported by funding from Cancer Research UK.
References
- 1. Lauby-Secretan B, Scoccianti C, Loomis D et al. . Body fatness and cancer—viewpoint of the IARC Working Group. N Engl J Med 2016;375(8):794–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Parkin DM. 3. Cancers attributable to consumption of alcohol in the UK in 2010. Br J Cancer 2011;105(Suppl 2):S14–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Parkin DM, Boyd L. 8. Cancers attributable to overweight and obesity in the UK in 2010. Br J Cancer 2011;105(Suppl 2):S34–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization. Global Status Report on Alcohol and Health. Geneva: World Health Organization, 2014. [Google Scholar]
- 5. Parkin DM. 2. Tobacco-attributable cancer burden in the UK in 2010. Br J Cancer 2011;105(Suppl 2):S6–S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Parkin DM. 9. Cancers attributable to inadequate physical exercise in the UK in 2010. Br J Cancer 2011;105(Suppl 2):S38–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lee IM, Shiroma EJ, Lobelo F et al. . Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380(9838):219–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. World Health Organization. Global Health Risks—mortality and burden of disease attributable to selected major risks. Geneva: World Health Organisation. [Google Scholar]
- 9. Peto R, Lopez AD, Boreham J et al. . Mortality From Smoking in Developed Countries, 1950–2000: Indirect Estimates from National Statistics. Oxford: Oxford University Press, 1994. [Google Scholar]
- 10.Children and Young Persons Act 1933. The Children and Young Persons (Sale of Tobacco, etc.) Order 2007 2007. http://www.legislation.gov.uk/uksi/2007/767/made.
- 11.Tobacco Advertising and Promotion Act 2002 C36. An Act to Control the Advertising and Promotion of Tobacco Products; and for Connected Purposes http://www.legislation.gov.uk/ukpga/2002/36/introduction.
- 12.The BCAP Code: The UK Code of Broadcast Advertising. C19 Alcohol 2010 https://www.asa.org.uk/type/broadcast/code_section/19.html.
- 13. Department of Health. Choosing Health: Making Healthier Choices Easier. London: The Stationery Office, 2004. [Google Scholar]
- 14. Health and Social Care Information Centre (HSCIC). Smoking, Drinking and Drug Use Among Young People in England—2014. 2015.
- 15. Meier PS, Holmes J, Angus C et al. . Estimated effects of different alcohol taxation and price policies on health inequalities: a mathematical modelling study. PLoS Med 2016;13(2):e1001963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Angus C, Holmes J, Pryce R et al. Model-based appraisal of the comparative impact of Minimum Unit Pricing and taxation policies in Scotland. An Adaptation of the Sheffield Alcohol Policy Model Version 3 2016.
- 17. HM Government. Childhood Obesity: A Plan for Action. 2016.
- 18. Vandenbroeck P, Goossens J, Clemens M. Tackling Obesities: Future Choices: Obesity System Atlas Department of Innovation, Universities and Skills; 2007.
- 19. McKinsey Global Institute. Overcoming Obesity: An Initial Economic Analysis. 2014.
- 20. Burgoine T, Forouhi NG, Griffin SJ et al. . Associations between exposure to takeaway food outlets, takeaway food consumption, and body weight in Cambridgeshire, UK: population based, cross sectional study. BMJ 2014;348:g1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Campbell R, Tasevska N, Jackson KG et al. . Association between urinary biomarkers of total sugars intake and measures of obesity in a cross-sectional study. PLoS One 2017;12(7):e0179508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Health and Social Care Information Centre. Statistics on Obesity, Physical Activity and Diet. 2015.
- 23. Hart CL, Davey Smith G, Gruer L et al. . The combined effect of smoking tobacco and drinking alcohol on cause-specific mortality: a 30 year cohort study. BMC Public Health 2010;10(1):789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Behrens G, Fischer B, Kohler S et al. . Healthy lifestyle behaviors and decreased risk of mortality in a large prospective study of U.S. women and men. Eur J Epidemiol 2013;28(5):361–72. [DOI] [PubMed] [Google Scholar]
- 25. Ford ES, Bergmann MM, Boeing H et al. . Healthy lifestyle behaviors and all-cause mortality among adults in the United States. Prev Med 2012;55(1):23–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Noble N, Paul C, Turon H et al. . Which modifiable health risk behaviours are related? A systematic review of the clustering of Smoking, Nutrition, Alcohol and Physical activity (‘SNAP’) health risk factors. Prev Med 2015;81:16–41. [DOI] [PubMed] [Google Scholar]
- 27. Meader N, King K, Moe-Byrne T et al. . A systematic review on the clustering and co-occurrence of multiple risk behaviours. BMC Public Health 2016;16:657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mawditt C, Sacker A, Britton A et al. . The clustering of health-related behaviours in a British population sample: testing for cohort differences. Prev Med 2016;88:95–107. [DOI] [PubMed] [Google Scholar]
- 29. Maibach EW, Maxfield A, Ladin K et al. . Translating health psychology into effective health communication: the American healthstyles audience segmentation project. J Health Psychol 1996;1(3):261–77. [DOI] [PubMed] [Google Scholar]
- 30. Vermeulen-Smit E, Ten Have M, Van Laar M et al. . Clustering of health risk behaviours and the relationship with mental disorders. J Affect Disord 2015;171:111–9. [DOI] [PubMed] [Google Scholar]
- 31. Becue-Bertaut M, Kern J, Hernandez-Maldonado ML et al. . Health-risk behaviour in Croatia. Public Health 2008;122(2):140–50. [DOI] [PubMed] [Google Scholar]
- 32. Hooper L, Anderson AS, Birch J et al. . Public awareness and healthcare professional advice for obesity as a risk factor for cancer in the UK: a cross-sectional survey. J Public Health (Bangkok) 2017;16:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. World Health Organization. BMI Classification World Health Organization. 2011.
- 34. Schuit AJ, van Loon AJM, Tijhuis M et al. . Clustering of lifestyle risk factors in a general adult population. Prev Med 2002;35(3):219–24. [DOI] [PubMed] [Google Scholar]
- 35. Poortinga W. The prevalence and clustering of four major lifestyle risk factors in an English adult population. Prev Med 2007;44(2):124–8. [DOI] [PubMed] [Google Scholar]
- 36. Department of Health. UK Chief Medical Officers’ Low Risk Drinking Guidelines. 2016.
- 37. The IPAQ Group. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ - Short Form. 2004.
- 38. Norušis MJ. Chapter 17 Cluster Analysis In: IBM SPSS Statistics 19 Statistical Procedures Companion. New Jersey: Prentice Hall, 2011. [Google Scholar]
- 39. Wardle J, Haase AM, Steptoe A et al. . Gender differences in food choice: the contribution of health beliefs and dieting. Ann Behav Med 2004;27(2):107–16. [DOI] [PubMed] [Google Scholar]
- 40. Mielke GI, da Silva ICM, Kolbe-Alexander TL et al. . Shifting the physical inactivity curve worldwide by closing the gender gap. Sports Med 2018;48:481–89. [DOI] [PubMed] [Google Scholar]
- 41. Maguire ER, Burgoine T, Monsivais P. Area deprivation and the food environment over time: a repeated cross-sectional study on takeaway outlet density and supermarket presence in Norfolk, UK, 1990–2008. Health Place 2015;33:142–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Office for National Statistics. Adult Drinking Habits in Great Britain: 2005 to 2016. 2017.
- 43. Hiscock R, Bauld L, Amos A et al. . Socioeconomic status and smoking: a review. Ann N Y Acad Sci 2012;1248(1):107–23. [DOI] [PubMed] [Google Scholar]
- 44. Hiscock R, Bauld L, Amos A et al. . Smoking and socioeconomic status in England: the rise of the never smoker and the disadvantaged smoker. J Public Health (Oxf) 2012;34(3):390–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Pringle A, Zwolinsky S, McKenna J et al. . Health improvement for men and hard-to-engage-men delivered in English Premier League football clubs. Health Educ Res 2014;29(3):503–20. [DOI] [PubMed] [Google Scholar]
- 46. Schneider S, Huy C, Schuessler M et al. . Optimising lifestyle interventions: identification of health behaviour patterns by cluster analysis in a German 50+ survey. Eur J Public Health 2009;19(3):271–7. [DOI] [PubMed] [Google Scholar]
- 47. Silva DA, Peres KG, Boing AF et al. . Clustering of risk behaviors for chronic noncommunicable diseases: a population-based study in southern Brazil. Prev Med 2013;56(1):20–4. [DOI] [PubMed] [Google Scholar]
- 48. Public Health England. National Diet and Nutrition Survey. Results from Years 5 and 6 (Combined) of the Rolling Programme (2012/13–2013/14). 2016.
- 49. Buck D, Frosini F. Clustering of Unhealthy Behaviours Over Time: Implications for Policy and Practice. London: Kings Fund, 2012. [Google Scholar]
- 50. Lawder R, Harding O, Stockton D et al. . Is the Scottish population living dangerously? Prevalence of multiple risk factors: the Scottish Health Survey 2003. BMC Public Health 2010;10:330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Randell E, Pickles T, Simpson SA et al. . Eligibility for interventions, co-occurrence and risk factors for unhealthy behaviours in patients consulting for routine primary care: results from the Pre-Empt study. BMC Fam Pract 2015;16:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Singh A, Rouxel P, Watt RG et al. . Social inequalities in clustering of oral health related behaviors in a national sample of British adults. Prev Med 2013;57:102–6. [DOI] [PubMed] [Google Scholar]
- 53. Liu Y, Croft JB, Wheaton AG et al. . Clustering of five health-related behaviors for chronic disease prevention among adults, United States, 2013. Prev Chronic Dis 2016;13:E70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.