Rates of syphilis among women and congenital syphilis have declined nationally since the early 1990s.1 The National Syphilis Elimination Plan has focused on decreasing racial disparities among syphilis diagnoses.2 Despite this national emphasis and decreasing rates, congenital syphilis cases continue to be overrepresented in minority populations.3 Arizona ranked the highest for congenital syphilis (CS) case rates in the United States for the years 2003, 2004, and 2005.3–5 Despite a steady reduction in primary and secondary syphilis among women in Arizona, rates of CS have remained high. Most of congenital syphilis cases diagnosed in Arizona during the previous 5 years were born in Maricopa County to Hispanic women. Compared to live births, infants born with congenital syphilis in Maricopa County during 1998–2002 were more likely be born to: mothers of minority race or ethnicity, unmarried mothers, uninsured mothers, and mothers who did not receive prenatal care (PNC).6 The high rate of CS cases during 2000–2005 prompted us to acquire additional information to identify risk factors that might be used to guide interventions targeting women of childbearing age at risk for syphilis and medical providers in Maricopa County and the rest of Arizona.
State health department records were reviewed for cases of congenital syphilis diagnosed in Maricopa County from 2000 to 2005. Demographic variables (maternal age, race, infant date of birth), reason for diagnosis, type of diagnosis (stillbirth vs. live birth), receipt of PNC, and number of PNC visits were collected from health department records and from the Centers for Disease Control and Prevention (CDC) Congenital Syphilis (CS) Case Investigation and Report (CDC Form 73.126) submitted for each case.
CS cases were defined according to CDC surveillance case definitions for confirmed and presumptive congenital syphilis and syphilitic stillbirths as specified in the CDC Form 73.126 and according to the CDC CS algorithm. Cases were grouped for local use in prevention planning into categories based on contributing factors to the diagnosis. Hospital delivery, prenatal, and laboratory records were reviewed for mothers who gave birth to infants with congenital syphilis near the time of delivery. Demographic variables collected included: age, race or ethnicity, citizenship status, insurance status, marital status, history of PNC, number of prenatal visits, and behavioral risk factors of drug use and prostitution. All mothers of infants with congenital syphilis were interviewed near the time of diagnosis as part of routine case investigation to determine treatment status and to elicit partners requiring testing and treatment. Risk factor information including citizenship, marital status, drug use during pregnancy, exchange of drugs or money for sex, and recent incarceration was collected from these interview records. Disease surveillance, data collection, evaluation, and analysis are ongoing public health surveillance activities, and thus are not subject to review by institutional review boards.
Data were analyzed using SPSS v 13.0 (SPSS Inc., Chicago, IL). Chi-square analysis was used to determine univariate correlates of significance.
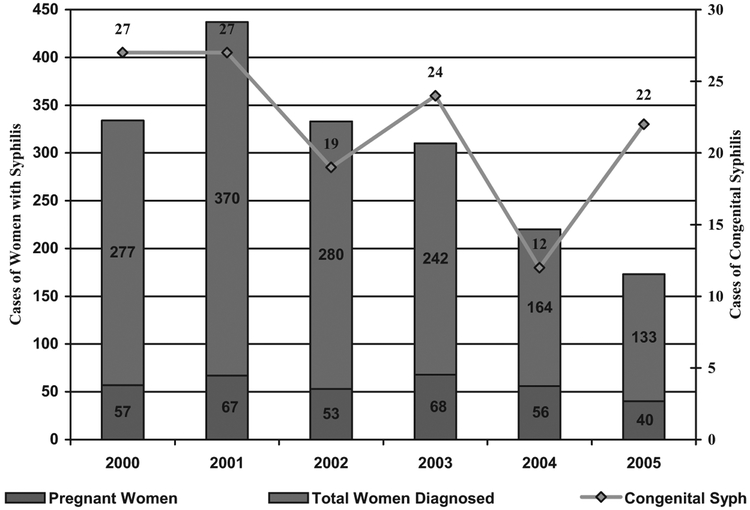
During 2000–2005, 5808 cases of syphilis were reported to the Arizona Department of Health Services. Of these, 2190 (38%) were diagnosed among women, and 4401 (76%) were diagnosed in Maricopa County. A total of 1807 women were diagnosed with syphilis in Maricopa County, of whom 894 (49%) were of Hispanic ethnicity and 341 (19%) of whom were pregnant at the time of diagnosis (Fig. 1). Of the pregnant women with syphilis in Maricopa County, 235 (69%) were of Hispanic ethnicity.
Fig. 1.
Female syphilis cases and congenital syphilis cases in Maricopa County, 2000–2005.
During 2000-2005, 161 cases of CS were reported to Arizona Department of Health Services, 131 (81%) of which were diagnosed in Maricopa County. Ninety-five (73%) of the 131 cases were His panic; the median age of mothers (N = 130) was 23 years (range, 16–42); and 57 (44%) of mothers described themselves as non-citizens. The majority of mothers who classified themselves as noncitizens were of Hispanic ethnicity (98%). A total of 108 (82%) cases were live births and 23 (18%) were stillbirths. One mother gave birth to congenitally infected twins. Of the 130 mothers, 40 (31%) reported drug use during pregnancy, 23 (18%) reported engagement in the exchange of sex for drugs or money, and 6 (5%) reported being incarcerated within the previous year.
Of 130 mothers, 78 (60%) received PNC. Of these mothers, 46 (59%) received early PNC (>60 days before delivery), and 29 (37%) received late PNC (<60 days before delivery). Five women received syphilis screening but no PNC. All 5 of these were screened for syphilis during the third trimester. At the time of delivery, 65 (50%) of the women had insurance (90% through Medicaid). Insured mothers who received PNC were no more likely to be tested for syphilis during the first prenatal (P = 0.7) visit or during the third trimester (P = 0.2) than noninsured mothers who received PNC. Among the 65 women with health insurance, 11 (17%) did not receive PNC.
Citizen mothers and noncitizen mothers obtained PNC with similar frequency (61% vs. 58%, P = 0.7). However, only 9% of noncitizen mothers who received PNC were tested for syphilis during the third trimester when compared with 35% of citizen mothers (P = 0.008). Citizen mothers were more likely to have health insurance than noncitizen mothers were (67% vs. 32%, P = 0.01). Drug use was reported by 50% of the citizen mothers when compared with 5% of noncitizen mothers (P <0.001), and the exchange of sex for drugs or money was reported by 30% of citizen mothers when compared with 1% of the noncitizen mothers (P <0.001).
The most common contributing factors to the diagnosis of congenital syphilis among the 131 infants was no prenatal testing due to no PNC (test performed at delivery) (N = 45, 34%), followed by being tested and having a positive result but not receiving appropriate treatment at least 30 days before delivery (N = 32, 25%) (Table 1). Of these 32 women, 25 (78%) were of Hispanic ethnicity. The median gestational month of testing for these women was the ninth month (range, 3–9 months), with the majority (N = 28, 88%) receiving testing during the third trimester.
TABLE 1.
Contributing Factors to the Diagnosis of Congenital Syphilis in Infants per Delivery Based on Diagnosis and Treatment of Syphilis in Mothers (N = 130)
| Category | N (%) |
| No prenatal testing due to no PNC (test performed at delivery) | 45 (35) |
| Tested and had a positive result but did not receive appropriate treatment at least 30 days before delivery | 32 (25) |
| Tested positive and treated during pregnancy but had inadequate titer response or reinfection | 16 (12) |
| Tested positive during pregnancy but did not receive treatment during pregnancy | 10 (8) |
| First prenatal test negative but delivery test positive (interim infection)/third trimester test not performed | 9 (7) |
| Tested positive and treated during pregnancy but response was equivocal or could not be determined from titer information | 6 (5) |
| Received PNC but not tested for syphilis | 5 (4) |
| Treated before pregnancy but inadequate or equivocal titer response | 4 (3) |
| Treated in pregnancy with nonpenicillin regimen | 1 (0.8) |
| Treated before pregnancy but sustained a fourfold titer increase at delivery | 1 (0.8) |
| Nonreactive test during third trimester, positive early postpartum | 1 (0.8) |
These reported cases represent two general categories: (a) non-citizen Hispanic mothers who have financial and legal barriers to PNC and (b) citizen mothers who have psychosocial problems including drug use and prostitution. Women who have given birth to a child with CS in the second category have been described from many places in the United States.6–9 We describe women in the first category that comprise a significant portion of the CS cases in Maricopa County. The majority of these cases overall can be attributed to lack of accessibility or utilization of early PNC.
Similar to previous studies, most missed opportunities to prevent congenital syphilis in Maricopa County seem to be due to failure to receive prenatal syphilis testing due to lack of PNC7–10 or not receiving adequate syphilis treatment within the 30 days before the delivery of the infant due to receipt of late PNC. Although mothers who described themselves as noncitizens were less likely to have insurance, they were no less likely to receive PNC when compared with citizen mothers. They were less likely, however, to receive a third trimester syphilis test, suggesting that the quality of care they are receiving may be deficient. The availability of adequate PNC for noncitizen pregnant women is not well described, and birthrates among Hispanic women now surpass that of all other race/ethnicities in Arizona.11 Although education of populations at risk and their health care providers should continue and perhaps be expanded, prevention of CS will continue to be challenged until and unless the social and infrastructural determinants can be resolved.
Financial barriers probably contributed to the occurrence of congenital syphilis cases in this study. As of July 1, 2006, proof of citizenship status is required at the time of application for AHCCCS.12 This is likely to result in still fewer pregnant women being eligible for PNC through AHCCCS and may result in increasing rates of CS among this group if the number of uninsured, noncitizen women seeking PNC declines. In November 2004, an Arizona ballot proposition that requires documentation of immigration status on health records was passed. This has prompted additional public health concern regarding presentation for medical care by noncitizen expectant mothers, especially those of Hispanic ethnicity.13
This study has strengths and limitations. It is the first study to describe financial, social, and medical barriers of Hispanic, predominantly noncitizen women residing in the United States who gave birth to infants with congenital syphilis. There was no control group, and thus we were not able to evaluate or compare the circumstances in which pregnant women with syphilis were detected and properly treated before they had an infant with syphilis. The number of reported cases limited the ability to detect important differences for some variables. Finally, the personal nature of some of the questions may have caused underreporting of certain information.
Adequate prenatal screening for syphilis in areas of high incidence is needed to prevent new cases.14–15 Close attention to CS rates in Arizona is needed due to the recent legislation that may adversely affect health care seeking behaviors among recently immigrated women of childbearing age. Additional study is needed to determine the prenatal syphilis screening practices of providers delivering care to pregnant women in Arizona and available PNC options for noncitizen women. Although our analysis suggests that Arizona has the nation’s highest concentration of noncitizen women that gave birth to infants with CS, the nationwide dispersal of disadvantaged Hispanic immigrants is well recognized. Our findings in noncitizen populations may be directly applicable in other states and health jurisdictions.
Footnotes
Presented, in part, at the International Conference on Women and Infectious Diseases. Abstract 59. March 2006. Atlanta, GA.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
References
- 1.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2005 Supplement, Syphilis Surveillance Report. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, December 2006. [Google Scholar]
- 2.Centers for Disease Control and Prevention. The Together We Can SEE. The National Plan to Eliminate Syphilis from the United States. Atlanta, GA: US Department of Health and Human Services, May 2006. [Google Scholar]
- 3.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance, 2005. Atlanta, GA: US Department of Health and Human Services, November 2006:135. [Google Scholar]
- 4.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance, 2003. Atlanta, GA: US Department of Health and Human Services, September 2004. [Google Scholar]
- 5.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance, 2004. Atlanta, GA: US Department of Health and Human Services, September 2005. [Google Scholar]
- 6.Carillo LA, Campos-Outcault D, Coonrod DV, et al. Congenital syphilis in Maricopa County, Arizona. Obstet Gynecol 2005; 105:106S. [Google Scholar]
- 7.Mobley JA, McKeown RE, Jackson KL, et al. Risk factors for congenital syphilis in infants of women with syphilis in South Carolina. Am J Public Health 1998; 88:597–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Warner L, Rochat RW, Fichtner RR, et al. Missed opportunities for congenital syphilis prevention in an urban Southeastern Hospital. Sex Transm Dis 2001; 28:92–98. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Congenital syphilis— United States, 2002. MMWR 2002; 53:716–719. [Google Scholar]
- 10.Centers for Disease Control and Prevention. Epidemic of congenital syphilis-Baltimore, 1996–1997. MMWR 1998; 47:904–907. [PubMed] [Google Scholar]
- 11.Arizona Vital Statistics. Arizona Health Status and Vital Statistics Report. Available at: http://www.azdhs.gov/plan/report/ahs/ahs2005/pdf/1a1.pdf. Accessed May 2, 2007.
- 12.Arizona Department of Economic Security. Division of Benefits and Medical Eligibility. Family Assistance Administration. Available at: http://www.de.state.az.us/faa/medical.asp. Accessed August 7, 2006. [Google Scholar]
- 13.Proposition 200: Arizona Taxpayer and Citizen Protection Act. Available at: http://www.azsos.gov/election/2004/info/PubPamphlet/english/prop200.htm. Accessed June 2, 2005.
- 14.Trepka MJ, Bloom AS, Zhang G, et al. Inadequate syphilis screening among women with prenatal care in a community with a high syphilis incidence. Sex Transm Dis 2006; 33:1–5. [DOI] [PubMed] [Google Scholar]
- 15.Beltrami J, Berman S. Congenital syphilis: A persisting sentinel public health event. Sex Transm Dis 2006; 33:675–676. [DOI] [PubMed] [Google Scholar]