Abstract
Introduction
Among those who misuse prescription opioids, alcohol use disorder (AUD) is associated with progression to opioid use disorder, risk of overdose, and poor treatment outcomes. However, little is known about co-occurring AUD and prescription opioid misuse. Motives, or reasons, for substance use are important factors in substance use initiation and maintenance; characterizing common motives can help inform treatment targets. The aims of the present study were to (1) identify patterns of motives for prescription opioid misuse, and (2) examine the association between AUD and motives.
Methods
Data were extracted from the 2015 National Survey on Drug Use and Health. Analyses included adult respondents with past-year prescription opioid misuse (N=2,627), of which 24.2% had a co-occurring AUD. Latent class analysis was utilized to identify patterns of motives for prescription opioid misuse. AUD was included as a predictor of class membership.
Results
We identified three classes: (1) pain relief (56.1% of the sample), (2) recreational (e.g., to get high; 29.3%), and (3) mixed motives (e.g., coping, pain relief, recreational; 14.6%). AUD was associated with greater odds of membership in the recreational (OR=2.05, 95% CI=1.36, 3.10, p=0.001) and mixed motives (OR=2.11, 95% CI=1.21, 3.67, p=0.008) classes, as compared to the pain relief class.
Results
Pain relief was the most commonly endorsed motive for opioid misuse among those with and without AUD. These results underscore the need to improve pain management among those who misuse prescription opioids. Those with co-occurring AUD might also benefit from interventions targeting negative affect and/or positive outcome expectancies.
Keywords: misuse, opioids, prescription drugs, alcohol use disorder, National Survey on Drug Use and Health
Introduction
Alcohol use disorder (AUD) is common among those with prescription opioid misuse (Garnier et al., 2009; Soyka, 2015), and is associated with progression to opioid use disorder (OUD) (Schepis & Hakes, 2017) and increased risk of opioid overdose (Maloney, Degenhardt, Darke, & Nelson, 2009). Furthermore, AUD is associated with poor OUD treatment outcomes (Friedmann et al., 2018; Roux et al., 2014), and opioid misuse has been associated with more frequent and heavier drinking during and after AUD treatment (Witkiewitz, Votaw, Vowles, & Kranzler, 2018). Despite the range of consequences associated with co-occurring AUD and prescription opioid misuse, very little research has focused on factors that might influence the concurrent use of these substances. The aim of the present study was to examine the association between AUD and motives for prescription opioid misuse.
Motives, or reasons, for substance use are important factors in substance use initiation and maintenance; understanding one’s motives for using substances can inform treatment interventions (Drazdowski, 2016). Most individuals with prescription opioid misuse report use to relieve pain (Han, Compton, Blanco, & Jones, 2018; Hughes et al., 2016), including those with and without OUD (Han et al., 2017). Yet, motives for prescription opioid misuse appear to vary depending on the population sampled. Most adolescents report misusing prescription opioids for recreational purposes (e.g., to get high) (Drazdowski, 2016; Lord, Brevard, & Budman, 2011), whereas opioid-dependent samples report multiple motives for prescription opioid misuse, including pain relief, withdrawal, and recreational motives (Barth et al., 2013; Schulte et al., 2016; Weiss et al., 2014). A recent study of 2015 National Survey on Drug Use and Health (NSDUH) respondents found that younger age was associated with recreational motives for prescription opioid misuse, and that substance use disorders and greater psychiatric severity (e.g., major depressive episode, suicidal ideation) were associated with both recreational and coping motives (Han et al., 2018). However, this study only examined correlates of participants’ primary motive for prescription opioid misuse. Given that many individuals report multiple motives for prescription opioid misuse (Barth et al., 2013; Drazdowski, 2016) and that motives vary based on participant characteristics, there is a need to examine heterogeneous combinations, or patterns, of motives for prescription opioid misuse and factors associated with motive patterns.
Several studies have examined the association between problematic alcohol use (e.g., binge alcohol use, positive drug and alcohol screening tests, AUD) and motives for prescription opioid misuse. Among adolescents, problematic alcohol use is associated with non-pain relief motives for prescription opioid misuse, typically both coping and recreational motives (McCabe, Boyd, Cranford, & Teter, 2009; McCabe, Cranford, Boyd, & Teter, 2007; McCabe, West, & Boyd, 2013). Associations between problematic alcohol use and motives for prescription opioid misuse might differ in adults. Indeed, an analysis of 2015 NSDUH data found that AUD was only associated with misusing opioids to help with sleep, but this this study only examined participants’ primary motive for prescription opioid misuse (Han et al., 2018). Accordingly, little is known about reasons for prescription opioid misuse among adults with co-occurring AUD and prescription opioid misuse.
Emerging evidence suggests that physical pain might be an important factor underlying the concurrent use of alcohol and prescription opioids (Witkiewitz & Vowles, 2018). Individuals presenting to AUD treatment have high rates of chronic pain (Zale, Maisto, & Ditre, 2015). Like opioids, alcohol displays analgesic effects at acute doses and hyperalgesia (i.e., increased pain sensitivity) with continued use (Zale et al., 2015). In addition, experimental pain induction increases the urge to use both alcohol (Moskal, Maisto, De Vita, & Ditre, 2018) and opioids (Lofwall, Nuzzo, & Walsh, 2012), and pain severity has been associated with relapse in AUD (Witkiewitz, McCallion, et al., 2015; Witkiewitz, Vowles, et al., 2015) and OUD treatment (Griffin et al., 2016). Therefore, it is plausible that individuals with co-occurring AUD and prescription opioid misuse use these medications for pain relief.
The present study aimed to address two gaps in the literature. First, few studies have examined patterns of motives for prescription opioid misuse, despite evidence that motives vary by sociodemographic and clinical factors and that many individuals report multiple motives. Previous studies have utilized mixture models (e.g., latent class analysis, latent profile analysis)—person-centered approaches to detect heterogeneity in a population—to identify patterns of motives for alcohol use (Cadigan, Martens, & Herman, 2015) and prescription drug misuse (McCabe & Cranford, 2012) among adolescents. Accordingly, we utilized latent class analysis (LCA) to identify patterns of motives for prescription opioid misuse among a general population sample of adults with past-year prescription opioid misuse. Based on prior studies of motives, we hypothesized that we would identify distinct motives classes defined primarily by coping, recreational, or pain relief motives (Cooper, Frone, Russell, & Mudar, 1995; Hughes et al., 2016).
Second, little is known about factors that might influence co-occurring AUD and prescription opioid misuse. We examined the association between AUD and patterns of motives for prescription opioid misuse. Given evidence that that physical pain might contribute to the concurrent use of alcohol and prescription opioids (Witkiewitz & Vowles, 2018), we hypothesized that AUD would be associated with the latent class(es) characterized by a high probability of endorsing pain relief motives.
Methods
Participants and Procedures
Data for the present analysis are from the 2015 National Survey on Drug Use and Health (NSDUH) public use data file (N=57,146). The NSDUH is an annual, population-based survey of United States citizens ages 12 and older, and is designed to provide estimates of substance use and mental health issues. The present analysis included adult participants (i.e., over 18 years old) who reported prescription opioid misuse in the previous year and had complete data on all relevant variables. Data from 45 participants was excluded from analyses (1.6% of the total eligible sample of 2,672 participants) due to missing data on motives for prescription opioid misuse (n=40), AUD symptoms (n=6), and/or self-reported overall health (n=1). Thus, 2,627 participants were included in analyses. Detailed study methods have been reported elsewhere (Substance Abuse and Mental Health Services Administration, 2016).
Measures
Substance use
To determine prescription opioid misuse, participants were shown cards with names and pictures of commonly used prescription opioids (e.g., oxycodone, hydrocodone, oxymorphone, etc.) and were asked to indicate if they had ever used these drugs in their lifetimes. If participants reported lifetime prescription opioid use, they were asked if they had ever misused these medications, defined as use without a prescription of their own, in greater amounts, more often, or longer than prescribed, or in any other way that was not directed to them. Those who reported lifetime prescription opioid misuse also reported the length of time since their last misuse. This information was used to determine the study population of those with past-year prescription opioid misuse.
Participants were also asked about lifetime, past-year, and past-month use of other prescription drugs (e.g., stimulants; sedatives, such as z-drugs, barbiturates, etc.; tranquilizers, such as benzodiazepines, muscle relaxants, etc.), illicit drugs (e.g., marijuana, crack/cocaine, methamphetamine, inhalants, hallucinogens, heroin, etc.), and alcohol. If a participant endorsed past-year use, they answered a standardized set of questions to determine Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) (American Psychiatric Association, 2000) substance abuse or dependence; presence of either diagnosis will be defined as ‘substance use disorder’ in all analyses. A three-level AUD variable was used in the present analysis: no AUD symptoms, one to two AUD symptoms without disorder (known as diagnostic orphans; Hasin & Paykin, 1998), and AUD diagnosis. This variable was chosen given evidence that DSM-IV AUD diagnostic orphans have increased risk of a range of psychiatric disorders and progression to AUD (McBride, Adamson, Bunting, & McCann, 2009). The NSDUH DSM-IV substance use disorder measure has demonstrated substantial interrater reliability across two time points (5 to 15 days apart; Substance Abuse and Mental Health Services Administration, 2010).
Motives for prescription opioid misuse
Participants with past-year prescription opioid misuse indicated reasons why they used prescription opioids during their last episode of misuse. Specifically, participants were asked: “Now think about the last time you used pain relievers in any way a doctor did not direct you to. What were the reasons you used pain relievers the last time?” Response options included the following: to relieve physical pain, to relax/relieve tension, to experiment/to see what pain relievers are like, to feel good/get high, to help with sleep, to help me with feelings/emotions, to increase/decrease the effect(s) of some other drug, and because I’m hooked/have to have pain relievers. Participants could also indicate that they misused prescription opioids for “some other reason”; however, this variable was not included in the present analysis. Participants were able to choose more than one response.
Sociodemographic measures
Sociodemographic measures in the present analysis included the following: gender, age (categorized as 18–25, 26–34, 35–49, 50+ years), race (Non-Hispanic White, Black/African American, Hispanic, other), educational attainment (< high school, high school graduate, some college, college graduate), employment status (employed full-time, employed part-time, unemployed, or other employment, such as keeping house), insurance status (any insurance coverage vs. uncovered), and self-reported overall health (poor/fair vs. good/very good/excellent health).
Psychological distress
The measure of psychological distress included in the present analysis was the Kessler Psychological Distress Scale (K6 Scale) (Kessler et al., 2003). Specifically, participants’ highest K6 score in the previous year was utilized in the present analysis. The K6 Scale is a nonspecific measure of psychological distress that includes 6 questions about the frequency of mood and anxiety symptoms (e.g., feeling hopeless, feeling nervous, feeling restless/fidgety). Response options raged from “none of the time” to “all of the time,” which corresponds to a range of scores from 0 to 24. Participants were asked to answer questions pertaining to the month in which they felt the most psychological distress in the past year.
Data analysis
Latent class analysis was utilized to identify patterns of motivations for prescription opioid misuse. Indicators were participants’ responses (yes vs. no) on the 8 possible motives for prescription opioid misuse. Model fit was assessed using the Bayesian Information Criteria (BIC) and the sample size adjusted Bayesian Information Criteria (aBIC), which adds a penalty for increasing parameters related to sample size. The optimal number of classes was identified by the lowest BIC and aBIC, with lower values indicating a better fitting model. We also evaluated model entropy, which is a measure of classification precision. We started with a 2-class solution and proceeded to a 5-class solution.
A three-level AUD variable (no AUD symptoms, AUD symptoms without disorder, AUD diagnosis) was included as a predictor of class membership. Covariates (which also served as predictors in the model) were selected based on previous evidence of association with opioid motives (Han et al., 2018) and included the following: sociodemographic factors (i.e., gender, race, age, education, employment, health insurance status), self-reported overall health, past-year psychological distress (i.e., highest K6 score in the previous year), other illicit drug use in the previous year, and past-year prescription OUD. Past-year illicit drug use was recoded into a binary variable, indicating any illicit or prescription drug misuse except prescription opioid misuse. The past-year prescription OUD variable refers to prescription opioid abuse/dependence, and not heroin abuse/dependence; those with past-year prescription opioid misuse were asked questions specific to prescription opioids (as opposed to any opioids) to establish DSM-IV prescription OUD (i.e., abuse or dependence diagnoses). Multinomial logistic regression was utilized to examine predictors of latent class membership (using a model based approach). Effect sizes represent odds ratios (OR), adjusting for all covariates in the model.
All analyses accounted for the complex sampling procedures of the NSDUH using the nesting (to capture stratification and to identify clustering) and weighting variables provided in the public use dataset. Data was prepared using SPSS version 25. All models were estimated using Mplus version 8 (Muthén & Muthén, 2017).
Results
Descriptive Statistics
Overall, 24.2% of those with prescription opioid misuse had a co-occurring AUD and 17.4% endorsed one to two AUD symptoms but did not meet diagnostic criteria for AUD, known as diagnostic orphans. Prevalence rates of the motives for prescription opioid misuse, by AUD status, are presented in Table 1.
Table 1.
Prevalence of Motives for Participants’ Last Episode of Prescription Opioid Misuse by Alcohol Use Disorder (AUD) Status
| All participants (N=2,627) | No AUD Symptoms (n=1,440) | AUD Symptoms without Disorder (n=467) | AUD Diagnosis (n=720) | |||||
|---|---|---|---|---|---|---|---|---|
| Count (n)1 | % | Count (n)1 | % | Count (n)1 | % | Count (n)1 | % | |
| Pain Relief | 1,772 | 72.2% | 1,056 | 77.5% | 319 | 75.4% | 397 | 57.3% |
| To Relax | 730 | 25.8% | 328 | 21.1% | 131 | 24.6% | 271 | 37.8% |
| To Get High | 642 | 20.5% | 262 | 14.8% | 107 | 20.2% | 273 | 34.3% |
| For Sleep | 421 | 15.6% | 192 | 13.5% | 86 | 15.7% | 143 | 20.7% |
| For Emotions | 309 | 9.6% | 133 | 7.4% | 50 | 11.4% | 126 | 13.6% |
| To Experiment | 183 | 4.9% | 63 | 3.2% | 32 | 4.8% | 88 | 9.1% |
| Because I’m Hooked | 100 | 3.5% | 65 | 4.0% | 9 | 2.2% | 26 | 3.3% |
| To Modify Other Drug Effect | 87 | 2.6% | 37 | 2.2% | 15 | 2.5% | 35 | 3.8% |
Note:
Reported prevalence rates were weighted to account for complex sampling procedures of the NSDUH. Therefore, the prevalence rates are not equivalent to the number of individuals reporting each motive divided by the total number of individuals.
Latent Class Analysis
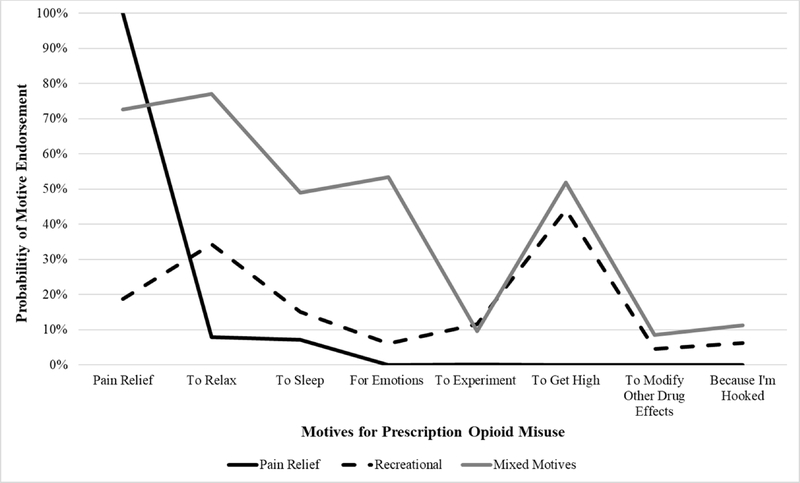
BIC, aBIC, and entropy for the 2- through 5-class solutions are presented in Table 2. The BIC and aBIC were lowest for the 4-class solution, but the rate of decrease was greatest from the 2- to 3-class model. To prevent over-extraction of latent classes and to increase parsimony, we selected a 3-class model as the final solution. The first latent class (pain relief) comprised approximately 56.1% of the sample, and was characterized by a 100% probability of reporting prescription opioid misuse to relieve pain and near-zero probabilities of endorsing all other motives. The second latent class (recreational) consisted of approximately 29.3% of the sample and displayed the highest probability of using prescription opioids to get high (as compared to other motives) and a moderate probability of using prescription opioids “to relax.” The final latent class had moderate to high probabilities of endorsing pain relief, recreational, and coping motives (e.g., for emotions, to sleep, to relax); this mixed motives class consisted of approximately 14.6% of the sample. The probabilities of endorsing each motive, by latent class, are presented in Figure 1.
Table 2.
Indicators of Model Fit for the 2- through 5-Class Solutions based on Motives for Prescription Opioid Misuse
| BIC | aBIC | Entropy | |
|---|---|---|---|
| 2-class | 13482.286 | 13364.726 | 0.777 |
| 3-class | 13266.534 | 13056.832 | 0.799 |
| 4-class | 13192.432 | 12890.590 | 0.745 |
| 5-class | 13201.870 | 12807.886 | 0.862 |
Note: BIC = Bayesian Information Criteria, a measure of model fit, in which the optimal number of classes is indicated by the lowest BIC; aBIC = Adjusted Bayesian Information Criteria,adds a penalty to the BIC estimate for increasing parameters related to sample size. We did not report the Lo-Mendell-Rubin adjusted likelihood ratio test (LRT) as an indicator of model fit given that LRT estimates do not account for complex sampling designs (Muthen, 2016). However, all analyses were conducted without the inclusion of complex sampling variables (i.e., variables that account for clustering and stratification) and these analyses supported the 3-class solution as the final model, as indicated by a significant LRT. Specifically, using the LRT we found a 3-class model fit significantly better than the 2-class model and a 4-class solution did not fit significantly better than a 3-class model.
Figure 1.
Probabilities of Endorsing Prescription Opioid Misuse Motives by Latent Class
AUD as a Predictor of Latent Class Membership
Predictors of identified latent classes are presented in Table 3. AUD was associated with greater odds of membership in the recreational (OR=2.05, 95% CI=1.36, 3.10, p=0.001) and mixed motives (OR=2.11, 95% CI=1.21, 3.67, p=0.008) classes, as compared to the pain relief class. However, AUD symptoms without disorder were not associated with class membership. Using the recreational class as the reference class (see Table 4), AUD was associated with lower odds of membership in the pain relief class (OR=0.49, 95% CI=0.32, 0.74, p=0.001), but was not associated with increased—or decreased—odds of membership in the mixed motives class (OR=1.03, 95% CI=0.57, 1.85, p=0.926). Thus, those with AUD were equally likely to be categorized in the recreational or mixed motives classes, but were less likely to be categorized in the pain relief class.
Table 3.
Multivariate Multinomial Logistic Regression Examining Predictors of Latent Class Membership with Pain Relief Class as Reference
| Recreational Class | Mixed Motives Class | |||
|---|---|---|---|---|
| Variable | OR (95% CI) | p | OR (95% CI) | p |
| Past-Year Alcohol Use Disorder Status | ||||
| No AUD symptoms | Ref | Ref | ||
| AUD symptoms without disorder | 0.84 (0.60–1.18) | 0.327 | 1.47 (0.74–2.92) | 0.269 |
| AUD diagnosis | 2.05 (1.36–3.10) | 0.001 | 2.11 (1.21–3.67) | 0.008 |
| Past-Year Illicit Drug Use | 3.64 (2.56–5.20) | <0.001 | 2.29 (1.29–4.06) | 0.005 |
| Past-Year Prescription Opioid Use Disorder | 2.27 (1.40–3.68) | 0.001 | 4.44 (2.32–8.48) | <0.001 |
| Psychological Distress (K6 Score) | 0.99 (0.96–1.02) | 0.483 | 1.13 (1.08–1.17) | <0.001 |
| Male Gender | 1.31 (0.92–1.87) | 0.133 | 0.88 (0.58–1.34) | 0.560 |
| Age | ||||
| 18–25 | Ref | Ref | ||
| 26–34 | 0.70 (0.50–0.99) | 0.040 | 0.87 (0.48–1.57) | 0.641 |
| 35–49 | 0.52 (0.35–0.79) | 0.002 | 0.54 (0.27–1.06) | 0.074 |
| 50 and older | 0.34 (0.17–0.69) | 0.003 | 0.62 (0.24–1.61) | 0.325 |
| Race | ||||
| Non-Hispanic White | Ref | Ref | ||
| Black | 0.89 (0.57–1.41) | 0.627 | 0.40 (0.14–1.14) | 0.087 |
| Hispanic | 0.80 (0.50–1.28) | 0.350 | 0.56 (0.28–1.10) | 0.094 |
| Other | 1.38 (0.80–2.39) | 0.253 | 1.02 (0.45–2.31) | 0.966 |
| Education | ||||
| Less than high school | Ref | Ref | ||
| High school graduate | 0.75 (0.45–1.25) | 0.272 | 2.22 (1.00–4.93) | 0.051 |
| Some college | 0.61 (0.36–1.03) | 0.066 | 2.79 (1.37–5.69) | 0.005 |
| College graduate | 0.59 (0.30–1.15) | 0.119 | 3.29 (1.37–7.92) | 0.008 |
| Employment | ||||
| Employed full-time | Ref | Ref | ||
| Employed part-time | 1.12 (0.67–1.88) | 0.670 | 2.17 (1.20–3.91) | 0.010 |
| Unemployed | 1.19 (0.68–2.09) | 0.536 | 0.59 (0.28–1.26) | 0.174 |
| Other employment | 0.87 (0.63–1.20) | 0.393 | 0.71 (0.40–1.25) | 0.231 |
| Not covered by health insurance | 0.63 (0.40–1.01) | 0.053 | 0.85 (0.42–1.73) | 0.652 |
| Good/Very Good/Excellent General Health (vs. Poor/Fair Health) | 1.18 (0.79–1.78) | 0.424 | 0.80 (0.40–1.61) | 0.529 |
Table 4.
Multivariate Multinomial Logistic Regression Examining Predictors of Latent Class Membership with Recreational Class as Reference
| Pain Relief Class | Mixed Motives Class | |||
|---|---|---|---|---|
| Variable | OR (95% CI) | p | OR (95% CI) | p |
| Past-Year Alcohol Use Disorder Status | ||||
| No AUD symptoms | Ref | Ref | ||
| AUD symptoms without disorder | 1.18 (0.84–1.66) | 0.327 | 1.74 (0.80–3.81) | 0.164 |
| AUD diagnosis | 0.49 (0.32–0.74) | 0.001 | 1.03 (0.57–1.85) | 0.926 |
| Past-Year Illicit Drug Use | 0.27 (0.19–0.39) | <0.001 | 0.63 (0.29–1.38) | 0.249 |
| Past-Year Prescription Opioid Use Disorder | 0.44 (0.27–0.72) | 0.001 | 1.96 (0.87–4.42) | 0.106 |
| Psychological Distress (K6 Score) | 1.01 (0.98–1.04) | 0.482 | 1.14 (1.08–1.20) | <0.001 |
| Male Gender | 0.76 (0.54–1.09) | 0.133 | 0.67 (0.38–1.18) | 0.167 |
| Age | ||||
| 18–25 | Ref | Ref | ||
| 26–34 | 1.42 (1.02–1.99) | 0.040 | 1.23 (0.60–2.54) | 0.571 |
| 35–49 | 1.92 (1.27–2.89) | 0.002 | 1.03 (0.49–2.18) | 0.941 |
| 50 and older | 2.97 (1.46–6.03) | 0.003 | 1.84 (0.64–5.31) | 0.258 |
| Race | ||||
| Non-Hispanic White | Ref | Ref | ||
| Black | 1.12 (0.71–1.77) | 0.627 | 0.45 (0.16–1.25) | 0.124 |
| Hispanic | 1.25 (0.78–2.00) | 0.350 | 0.70 (0.31–1.59) | 0.395 |
| Other | 0.73 (0.42–1.26) | 0.253 | 0.74 (0.29–1.86) | 0.519 |
| Education | ||||
| Less than high school | Ref | Ref | ||
| High school graduate | 1.33 (0.80–2.22) | 0.272 | 2.95 (1.21–7.22) | 0.018 |
| Some college | 1.63 (0.97–2.74) | 0.066 | 4.55 (2.07–9.99) | <0.001 |
| College graduate | 1.70 (0.87–3.29) | 0.119 | 5.59 (2.08–15.01) | 0.001 |
| Employment | ||||
| Employed full-time | Ref | Ref | ||
| Employed part-time | 0.89 (0.53–1.50) | 0.670 | 1.94 (0.92–4.10) | 0.084 |
| Unemployed | 0.84 (0.48–1.47) | 0.536 | 0.49 (0.19–1.26) | 0.139 |
| Other employment | 1.15 (0.83–1.59) | 0.393 | 0.82 (0.45–1.48) | 0.502 |
| Not covered by health insurance | 1.58 (0.99–2.50) | 0.053 | 1.34 (0.57–3.16) | 0.504 |
| Good/Very Good/Excellent General Health (vs. Poor/Fair Health) | 0.85 (0.56–1.27) | 0.424 | 0.68 (0.28–1.62) | 0.380 |
A number of other factors were associated with latent class membership. Prescription OUD and past-year illicit drug use were associated with greater odds of membership in both the recreational and mixed motives classes, as compared to the pain relief class (Table 3). Older age was associated with greater odds of membership in the pain relief class, as compared to the recreational class (Table 4). Greater psychological distress and educational attainment were associated with greater odds of membership in the mixed motives class, as compared to both the pain relief class (Table 3) and recreational class (Table 4). Lastly, part-time employment (vs. full-time employment) was associated with the mixed motives class, as compared to the pain relief class (Table 3).
Discussion
Despite the range of consequences associated with co-occurring AUD and prescription opioid misuse (e.g., progression to OUD, risk of overdose, poor treatment outcomes), little is known about the motives, or reasons, for opioid misuse in this population. The prevalence of past-year AUD (24.2%) in our sample of adults with past-year prescription opioid misuse was nearly four times greater than among the general population (Substance Abuse and Mental Health Services Administration, 2016). Furthermore, 17.4% of the sample did not meet full AUD criteria but did endorse one or two AUD diagnostic criteria. Elevated rates of AUD and alcohol-related problems in this population underscore the importance of examining factors that might influence the concurrent use of alcohol and prescription opioids, including motives.
The present analysis identified three distinct latent classes of motives for prescription opioid misuse: pain relief, recreational, and mixed motives. Results from the present analysis extend our understanding of reasons for prescription opioid misuse by identifying patterns of motives among a large, heterogeneous sample with prescription opioid misuse. Co-occurring AUD was associated with increased odds of membership in the recreational and mixed motives classes. Among those with prescription drug misuse, both recreational motives (McCabe, West, Teter, & Boyd, 2012) and a greater number of motives (Nattala, Leung, Abdallah, Murthy, & Cottler, 2012) have been associated with the co-ingestion of alcohol and prescription drugs. This is particularly concerning given the increased risk of overdose when alcohol and prescription opioids are combined (Kandel, Hu, Griesler, & Wall, 2017). Characterizing identified patterns based on AUD status can help inform prevention and treatment efforts to reduce the concurrent use of alcohol and prescription opioids and related overdose.
The pain relief class was the most prevalent latent class among a large, population-based sample with past-year prescription opioid misuse, and pain relief was the most commonly reported motive among those with and without AUD (see Table 1). Notably, the pain relief class had near-zero probabilities of reporting any other motives, indicating that pain relief might contribute to the initiation and maintenance of prescription opioid misuse for the majority of those who misuse prescription opioids. Misusing prescription opioids for pain relief is associated with symptoms of opioid dependence (Jones, Spradlin, Robinson, & Tragesser, 2014), and pain severity is associated with a history of overdose and suicide (Sansone, Watts, & Wiederman, 2014). Thus, improving pain management should be a research, policy, and clinical priority. Effective non-opioid forms of pain management include cognitive-behavioral interventions (e.g., acceptance and commitment therapy, mindfulness-based interventions) (McCracken & Vowles, 2014) and movement therapies (e.g., yoga, tai chi) (Lee, Crawford, Schoomaker, & Active Self-Care Therapies for Pain [PACT] Working Group, 2014). Those who were older had greater odds of membership in the pain relief class, and therefore non-opioid forms of pain management might be targeted to older individuals. Overall, increased availability of non-opioid forms of pain management, as well as policies mandating appropriate opioid prescribing and tapering, might help reduce initiation of prescription opioid misuse, opioid dependence, and opioid overdose.
Contrary to our hypothesis, those with AUD were less likely to be included in the pain relief class, as compared to the recreational and mixed motives classes. This finding is consistent with findings among adolescents indicating that problematic alcohol use is associated with non-pain relief motives (McCabe et al., 2009, 2007, 2013). Nevertheless, previous studies indicate that pain influences the maintenance of both alcohol and opioid misuse, separately (Griffin et al., 2016; Lofwall et al., 2012; Moskal et al., 2018; Witkiewitz, McCallion, et al., 2015; Witkiewitz, Vowles, et al., 2015). It is important to note that information on pain, including pain interference, pain severity, and chronic pain status, was not available in the NSDUH public use file. It is therefore unknown if differences in pain relief motives reflect heightened pain severity. Clarifying the relationships between pain severity, pain relief motives, and the concurrent use of alcohol and prescription opioids is an important area for future research.
Interestingly, we did not identify a class with predominantly coping motives. Instead, the mixed motives class was characterized by high probabilities of reporting pain relief, coping, and recreational motives. Greater levels of substance use severity, including AUD, prescription OUD, and past-year illicit substance use, were all associated with greater odds of membership in the mixed motives class. This finding is consistent with research in adults with prescription opioid dependence suggesting a shift in motives over time, with greater pain relief motives at the time of substance initiation, and a shift to multiple motives (and most notably, an increase in withdrawal relief) over time (Barth et al., 2013; Weiss et al., 2014). Substance use disorders are characterized by chronically high negative affect, including blunted natural reward systems, which is a potent motivator of relief (Koob & Le Moal, 2008). Those with AUD might represent a group that has advanced to a later stage of substance use severity, which may be more motivated to use substances to alleviate the negative effects of chronic substance use, in addition to using substances for their reinforcing purposes. Greater psychological distress and greater educational attainment were associated with membership in the mixed motives class, as compared to both the pain relief and recreational classes. Targeting negative affect and decreasing the use of substances to cope with negative affect via psychotherapy (e.g., mindfulness-based treatments, cognitive-behavioral therapy) might improve outcomes among people who misuse opioids with greater substance use and psychiatric severity, including those with co-occurring AUD.
Those with AUD were more likely to be included in the two classes (recreational and mixed motives) characterized by high probabilities of misusing prescription opioids for recreational purposes. Consistent with another recent analysis of NSDUH data (Han et al., 2018), prescription OUD, past-year illicit drug use, and younger age were also associated with membership in the recreational class. Previous research indicates that positive alcohol outcome expectancies meditates the association between recreational motives and greater alcohol consumption (Anthenien, Lembo, & Neighbors, 2017), and that cognitive-behavioral treatment is associated with reductions in positive alcohol outcome expectancies (Coates et al., 2018). Thus, cognitive-behavioral treatment might reduce prescription opioid misuse among subgroups with recreational motives. Yet, future studies are needed to evaluate if those with prescription opioid misuse demonstrate similar relationships between recreational motives, positive opioid outcomes expectancies, and cognitive behavioral treatment.
AUD diagnostic orphan status was not associated with latent class membership. This is consistent with previous analyses indicating that diagnostic orphans and those meeting criteria for AUD are distinct groups in terms of substance use and psychiatric severity (Ray, Miranda, Chelminski, Young, & Zimmerman, 2008). It is important to note that DSM-IV diagnostic orphans are classified by endorsing one to two dependence criteria, given that endorsing one abuse criteria results in an AUD diagnosis (American Psychiatric Association, 2000). Among diagnostic orphans in the present sample, the two most commonly endorsed dependence criteria were spending a great deal of time in alcohol-related activities (54.8%) and alcohol tolerance (49.0%). A recent meta-analysis found that endorsing tolerance is associated with lower AUD severity across a range of studies, whereas time spent in alcohol-related activities is associated with lower AUD severity in NSDUH surveys specifically (Lane, Steinley, & Sher, 2016). These findings indicate that greater alcohol-related severity might uniquely contribute to motives for prescription opioid misuse. For example, consequences of AUD, such as withdrawal, negative affect, and impairment in the natural reward system, might motivate individuals to misuse prescription opioids for coping and recreational motives.
There were several differences in findings between the present analysis and another recent analysis of 2015 NSDUH data examining correlates of motives for prescription opioid misuse. Most notably, Han et al. (2018) found that AUD was only associated with misusing prescription opioids primarily to help with sleep, whereas we found that AUD was associated membership in both the recreational and mixed motives classes. In addition, gender, race, health insurance status, and general health were not associated with latent class membership in our analysis, but were previously associated with participants’ primary motive for opioid misuse (Han et al., 2018). It is possible that these reflect differences in examining multiple motives (in the present study) vs. participants’ primary motive (in the study conducted by Han and colleagues, 2018). Future studies are needed to examine the differential impact of primary and secondary motives on substance use initiation and maintenance. Nevertheless, a greater number of motives for prescription drug misuse has been associated with a number of poor outcomes, including the co-use of alcohol and prescription drugs and more frequent prescription drug misuse (Nattala, Leung, Abdallah, & Cottler, 2011; Nattala et al., 2012), underscoring the importance of examining multiple motives.
Interpretation of the results of the present analysis are limited by several methodological features of the present study. First, data from the present study are cross-sectional. The NSDUH is also limited to non-institutionalized, civilian citizens and exclusion of certain populations (e.g., incarcerated individuals, homeless individuals) might obscure population estimates of substance use. In addition, the question on motives for prescription opioid use asked participants to respond based on their last episode of misuse. Thus, it is unknown if these responses are representative of participants’ typical reasons for using or if these motives were unique to the last episode of prescription opioid use. Indeed, the motives questionnaire included in the NSDUH questionnaire has not yet been validated. This will be an area for future research, given the opportunity to enhance our understanding of motives for a range of prescription drugs (e.g., sedatives, tranquilizers, amphetamines, opioids) using a large, population-based sample. Pain ratings and chronic pain status are not available in the NSDUH public use data file, limiting conclusions about the association between AUD and pain among those with opioid misuse. Information reported also reflected the concurrent misuse of prescription opioids and alcohol (i.e., use over the same time period, but not necessarily at the same time) as opposed to simultaneous use (i.e., co-ingestion). Future studies examining risk factors associated with the co-ingestion of alcohol and prescription opioids are needed to help identify those that are most at risk of overdose related to this combination.
Overall, results of this cross-sectional analysis indicate that those with co-occurring AUD and prescription opioid misuse report a range of reasons for prescription opioid misuse, including use to relieve pain, reduce negative affect, and for recreational purposes. The latent pain relief class was the most prevalent class in our sample, and pain relief was the most common motive among those with and without AUD. These findings underscore the need to improve pain management in order to prevent the initiation of opioid misuse. Those with AUD also had greater odds of class membership in the two subgroups that were characterized by greater probabilities of reporting coping and recreational motives for prescription opioid misuse. Treatments targeting negative affect and/or positive outcome expectancies may be particularly important for reducing prescription opioid misuse among those with AUD. Efforts to reduce prescription opioid misuse among those with AUD (and vice versa) has the potential to reduce rates of prescription OUD and opioid overdose deaths.
Acknowledgments
Financial disclosures
This research was supported by grants funded by the National Institutes of Health R21 AA024926 (Witkiewitz, PI). NIAAA had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. All authors declare they have no conflicts of interest.
References
- American Psychiatric Association. (2000). American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. American Psychiatric Association; 10.1176/appi.books.9780890423349 [DOI] [Google Scholar]
- Anthenien AM, Lembo J, & Neighbors C (2017). Drinking motives and alcohol outcome expectancies as mediators of the association between negative urgency and alcohol consumption. Addictive Behaviors, 66, 101–107. 10.1016/j.addbeh.2016.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barth KS, Maria MM-S, Lawson K, Shaftman S, Brady KT, & Back SE (2013). Pain and motives for use among non-treatment seeking individuals with prescription opioid dependence. The American Journal on Addictions, 22(5), 486–491. 10.1111/j.1521-0391.2013.12038.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadigan JM, Martens MP, & Herman KC (2015). A latent profile analysis of drinking motives among heavy drinking college students. Addictive Behaviors, 51, 100–105. 10.1016/j.addbeh.2015.07.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coates JM, Gullo MJ, Feeney GFX, Young RM, Dingle GA, & Connor JP (2018). Alcohol expectancies pre-and post-alcohol use disorder treatment: Clinical implications. Addictive Behaviors, 80, 142–149. 10.1016/j.addbeh.2018.01.029 [DOI] [PubMed] [Google Scholar]
- Cooper ML, Frone MR, Russell M, & Mudar P (1995). Drinking to regulate positive and negative emotions: a motivational model of alcohol use. Journal of Personality and Social Psychology, 69(5), 990–1005. [DOI] [PubMed] [Google Scholar]
- Drazdowski TK (2016). A systematic review of the motivations for the non-medical use of prescription drugs in young adults. Drug and Alcohol Dependence, 162, 3–25. 10.1016/j.drugalcdep.2016.01.011 [DOI] [PubMed] [Google Scholar]
- Friedmann PD, Wilson D, Nunes EV, Hoskinson R, Lee JD, Gordon M, … O’Brien CP (2018). Do patient characteristics moderate the effect of extended-release naltrexone (XR-NTX) for opioid use disorder? Journal of Substance Abuse Treatment, 85, 61–65. 10.1016/j.jsat.2017.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnier LM, Arria AM, Caldeira KM, Vincent KB, O’Grady KE, & Wish ED (2009). Nonmedical prescription analgesic use and concurrent alcohol consumption among college students. The American Journal of Drug and Alcohol Abuse, 35(5), 334–338. 10.1080/00952990903075059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin ML, McDermott KA, McHugh RK, Fitzmaurice GM, Jamison RN, & Weiss RD (2016). Longitudinal association between pain severity and subsequent opioid use in prescription opioid dependent patients with chronic pain. Drug and Alcohol Dependence, 163, 216–221. 10.1016/j.drugalcdep.2016.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Compton WM, Blanco C, Crane E, Lee J, & Jones CM (2017). Prescription Opioid Use, Misuse, and Use Disorders in U.S. Adults: 2015 National Survey on Drug Use and Health. Annals of Internal Medicine, 167(5), 293 10.7326/M17-0865 [DOI] [PubMed] [Google Scholar]
- Han B, Compton WM, Blanco C, & Jones CM (2018). Correlates of Prescription Opioid Use, Misuse, Use Disorders, and Motivations for Misuse Among US Adults. The Journal of Clinical Psychiatry, 79(5). 10.4088/JCP.17m11973 [DOI] [PubMed] [Google Scholar]
- Hasin D, & Paykin A (1998). Dependence symptoms but no diagnosis: diagnostic “orphans” in a community sample. Drug and Alcohol Dependence, 50(1), 19–26. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9589269 [DOI] [PubMed] [Google Scholar]
- Hughes A, Williams MR, Lipari RN, Bose J, Copello EAP, & Kroutil LA (2016). Prescription drug use and misuse in the United States: Results from the 2015 National Survey on Drug Use and Health. NSDUH Data Review. [Google Scholar]
- Jones RE, Spradlin A, Robinson RJ, & Tragesser SL (2014). Development and validation of the Opioid Prescription Medication Motives Questionnaire: A four-factor model of reasons for use. Psychology of Addictive Behaviors, 28(4), 1290–1296. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Hu M-C, Griesler P, & Wall M (2017). Increases from 2002 to 2015 in prescription opioid overdose deaths in combination with other substances. Drug and Alcohol Dependence, 178, 501–511. 10.1016/j.drugalcdep.2017.05.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, … Zaslavsky AM (2003). Screening for serious mental illness in the general population. Archives of General Psychiatry, 60(2), 184–189. 10.1001/archpsyc.60.2.184 [DOI] [PubMed] [Google Scholar]
- Koob GF, & Le Moal M (2008). Addiction and the Brain Antireward System. Annual Review of Psychology, 59(1), 29–53. 10.1146/annurev.psych.59.103006.093548 [DOI] [PubMed] [Google Scholar]
- Lane SP, Steinley D, & Sher KJ (2016). Meta-analysis of DSM alcohol use disorder criteria severities: structural consistency is only “skin deep”. Psychological Medicine, 46(8), 1769–1784. 10.1017/S0033291716000404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C, Crawford C, Schoomaker E, & Active Self-Care Therapies for Pain (PACT) Working Group. (2014). Movement therapies for the self-management of chronic pain symptoms. Pain Medicine, 15(S1), S40–S53. 10.1111/pme.12411 [DOI] [PubMed] [Google Scholar]
- Lofwall MR, Nuzzo PA, & Walsh SL (2012). Effects of cold pressor pain on the abuse liability of intranasal oxycodone in male and female prescription opioid abusers. Drug and Alcohol Dependence, 123(1–3), 229–238. 10.1016/j.drugalcdep.2011.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord S, Brevard J, & Budman S (2011). Connecting to young adults: An online social network survey of beliefs and attitudes associated with prescription opioid misuse among college students. Substance Use & Misuse, 46(1), 66–76. 10.3109/10826084.2011.521371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maloney E, Degenhardt L, Darke S, & Nelson EC (2009). Are non-fatal opioid overdoses misclassified suicide attempts? Comparing the associated correlates. Addictive Behaviors, 34(9), 723–729. 10.1016/j.addbeh.2009.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride O, Adamson G, Bunting B, & McCann S (2009). Diagnostic orphans: comparing self-report lifetime course to groups with DSM-IV alcohol abuse and dependence. Addictive Behaviors, 34(1), 86–91. 10.1016/j.addbeh.2008.07.019 [DOI] [PubMed] [Google Scholar]
- McCabe SE, Boyd CJ, Cranford JA, & Teter CJ (2009). Motives for Nonmedical Use of Prescription Opioids Among High School Seniors in the United States. Archives of Pediatrics & Adolescent Medicine, 163(8), 739–744. 10.1001/archpediatrics.2009.120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, & Cranford JA (2012). Motivational subtypes of nonmedical use of prescription medications: results from a national study. The Journal of Adolescent Health : Official Publication of the Society for Adolescent Medicine, 51(5), 445–452. 10.1016/j.jadohealth.2012.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Cranford JA, Boyd CJ, & Teter CJ (2007). Motives, diversion and routes of administration associated with nonmedical use of prescription opioids. Addictive Behaviors, 32(3), 562–575. 10.1016/j.addbeh.2006.05.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, & Boyd CJ (2013). Motives for medical misuse of prescription opioids among adolescents. The Journal of Pain: Official Journal of the American Pain Society, 14(10), 1208–1216. 10.1016/j.jpain.2013.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Teter CJ, & Boyd CJ (2012). Co-ingestion of prescription opioids and other drugs among high school seniors: Results from a national study. Drug and Alcohol Dependence, 126(1–2), 65–70. 10.1016/j.drugalcdep.2012.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken LM, & Vowles KE (2014). Acceptance and commitment therapy and mindfulness for chronic pain: Model, process, and progress. American Psychologist, 69(2), 178–187. 10.1037/a0035623 [DOI] [PubMed] [Google Scholar]
- Moskal D, Maisto SA, De Vita M, & Ditre JW (2018). Effects of experimental pain induction on alcohol urge, intention to consume alcohol, and alcohol demand. Experimental and Clinical Psychopharmacology, 26(1), 65 10.1037/pha0000170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen BO (2016, January 29). Re: LCA and sampling weights [Online discussion group]. Retrieved from: http://www.statmodel.com/discussion/messages/13/1202.html?1473360685
- Muthén L, & Muthén B (2017). Mplus user’s guide (8th ed.). Los Angeles: Author; 10.13155/29825 [DOI] [Google Scholar]
- Nattala P, Leung KS, Abdallah A. Ben, & Cottler LB (2011). Heavy use versus less heavy use of sedatives among non-medical sedative users: Characteristics and correlates. Addictive Behaviors, 36(1–2), 103–109. 10.1016/j.addbeh.2010.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nattala P, Leung KS, Abdallah A. Ben, Murthy P, & Cottler LB (2012). Motives and simultaneous sedative-alcohol use among past 12-month alcohol and nonmedical sedative users. The American Journal of Drug and Alcohol Abuse, 38(4), 359–364. [DOI] [PubMed] [Google Scholar]
- Ray LA, Miranda R, Chelminski I, Young D, & Zimmerman M (2008). Diagnostic orphans for alcohol use disorders in a treatment-seeking psychiatric sample. Drug and Alcohol Dependence, 96(1–2), 187–191. 10.1016/j.drugalcdep.2008.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roux P, Lions C, Michel L, Cohen J, Mora M, Marcellin F, … ANRS Methaville Study Group. (2014). Predictors of non-adherence to methadone maintenance treatment in opioid-dependent individuals: implications for clinicians. Current Pharmaceutical Design, 20(25), 4097–4105. [DOI] [PubMed] [Google Scholar]
- Sansone RA, Watts DA, & Wiederman MW (2014). Pain, pain catastrophizing, and history of intentional overdoses and attempted suicide. Pain Practice, 14(2), E29–E32. 10.1111/papr.12094 [DOI] [PubMed] [Google Scholar]
- Schepis TS, & Hakes JK (2017). Age of initiation, psychopathology, and other substance use are associated with time to use disorder diagnosis in persons using opioids nonmedically. Substance Abuse, 38(4), 407–413. 10.1080/08897077.2017.1356791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulte B, Schmidt CS, Strada L, Götzke C, Hiller P, Fischer B, & Reimer J (2016). Non-prescribed use of opioid substitution medication: Patterns and trends in sub-populations of opioid users in Germany. The International Journal on Drug Policy, 29, 57–65. 10.1016/j.drugpo.2015.12.024 [DOI] [PubMed] [Google Scholar]
- Soyka M (2015). Alcohol use disorders in opioid maintenance therapy: Prevalence, clinical correlates and treatment. European Addiction Research, 21(2), 78–87. 10.1159/000363232 [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2016). Results from the 2015 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration, Rockville, MD: Retrieved from https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.htm [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2010). Reliability of Key Measures in the National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration, Rockville, MD. [PubMed] [Google Scholar]
- Weiss RD, Potter JS, Griffin ML, McHugh RK, Haller D, Jacobs P, … Rosen KD (2014). Reasons for opioid use among patients with dependence on prescription opioids: The role of chronic pain. Journal of Substance Abuse Treatment, 47(2), 140–145. 10.1016/j.jsat.2014.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, McCallion EA, Vowles KE, Kirouac M, Frohe T, Maisto SA, … Heather N (2015). Association between physical pain and alcohol treatment outcomes: The mediating role of negative affect. Journal of Consulting and Clinical Psychology, 83(6). 10.1037/ccp0000033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Votaw VR, Vowles KE, & Kranzler HR (2018). Opioid Misuse as a Predictor of Alcohol Treatment Outcomes in the COMBINE Study: Mediation by Medication Adherence. Alcoholism, Clinical and Experimental Research. 10.1111/acer.13772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, & Vowles KE (2018). Alcohol and Opioid Use, Co-Use, and Chronic Pain in the Context of the Opioid Epidemic: A Critical Review. Alcoholism: Clinical and Experimental Research, 42(7), 9–13. 10.1111/acer.13594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Vowles KE, McCallion E, Frohe T, Kirouac M, & Maisto SA (2015). Pain as a predictor of heavy drinking and any drinking lapses in the COMBINE study and the UK Alcohol Treatment Trial. Addiction, 110(8), 1262–1271. 10.1111/add.12964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zale EL, Maisto SA, & Ditre JW (2015). Interrelations between pain and alcohol: An integrative review. Clinical Psychology Review, 37, 57–71. 10.1016/j.cpr.2015.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]