A 41-year-old male patient presented with floaters and decreased vision OD for 3 months. The vision was poor in OS since childhood. Systemic review revealed intermittent dyspnea, weight loss, and fatigability for 8 months.
Examination revealed a best corrected visual acuity (BCVA) of 6/24 right eye and 1/60 left eye. Anterior segments and intraocular pressure were normal in both the eyes. There was no RAPD. Left eye revealed unilateral hypermetropia of +8 diopters and amblyopia. Dilated fundus of right eye revealed minimal vitritis and a 2-disc diameter large optic disc granuloma [Fig. 1a] obscuring the optic disc. Overlying tortuous blood vessels, few hard exudates, flame-shaped hemorrhages, sheathing of blood vessels, and ILM folds at the posterior pole were present. Swept source OCT (SSOCT) through the lesion demonstrated presence of elevated lesion with shadowing underneath [Fig. 2a]. In addition, vitreous attachment was seen attached to the surface of granuloma.
Figure 1.
Color fundus photograph of right eye showing a large optic nerve head granuloma of approximately 2DD size (a), showing regression of the size of the granuloma at 2-month follow up (b), and slight increase in size at 6-month follow up (c)
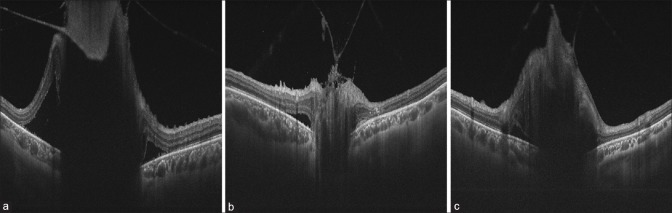
Figure 2.
Swept source image through the granuloma demonstrating presence of an elevated lesion with shadowing underneath (a), decrease in both extension and height of the lesion at 2 months (b) but slight increase in height of the lesion noted at the 6th month of follow up (c)
Complete blood count, liver, and kidney function tests were normal. Mantoux reading was 0 mm at 48 hrs. Serum angiotensin converting enzyme levels were elevated at 276 IU/L (8-52 IU/L). HRCT scan showed bilateral hilar lymphadenopathy. Transbronchial lung biopsy demonstrated presence of noncaseating granulomas, which were reticulin and acid-fast bacilli negative confirming pulmonary sarcoidosis. Patient was started on oral prednisolone 1mg/kg/day dose along with oral calcium supplements and proton pump inhibitors. Regression of granuloma was noted at two months [Figs.1b and 2b] and BCVA improved to 6/9 in right eye, which was maintained at 6-month follow up though the granuloma had increased in size [Figs 1c and 2c]. Patient was on continued on 10 mg/day oral steroid. Since the patient was asymptomatic and vision was stable, we didn’t consider increasing the steroid dosage or starting of immunomodulators.
Ocular sarcoidosis, the commonest type of extra thoracic sarcoidosis, has been reported in 21–80% cases.[1] Optic nerve involvement (approximately in 1% cases) in sarcoidosis has been divided in to 5 different categories: optic disc edema secondary to posterior uveitis, optic disc edema secondary to raised intracranial pressure, optic neuritis, optic atrophy secondary to compression or infiltration and primary granuloma of the optic nerve head.[2] Sarcoid optic nerve involvement should be recognized and treated early to prevent visual field and vision loss. These lesions respond well to corticosteroids or steroid sparing immunosuppressants.[3] Ocular sarcoid can be the initial presentation of the multisystem disease as in our case.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lee SY, Lee HG, Kim DS, Kim J-G, Chung H, Yoon YH. Ocular sarcoidosis in a Korean population. Korean Med Sci. 2009;24:413–9. doi: 10.3346/jkms.2009.24.3.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ingestad R, Stigmar G. Sarcoidosis with ocular and hypothalamic pituitary manifestations. Acta Ophthalmologica. 1971;49:1–10. doi: 10.1111/j.1755-3768.1971.tb08227.x. [DOI] [PubMed] [Google Scholar]
- 3.Ganesh SK, Kaduskar AV. Optic nerve head granuloma as a primary manifestation of ocular sarcoidosis-A tertiary uveitis clinic experience. Oman J Ophthalmol. 2015;8:157–61. doi: 10.4103/0974-620X.169890. [DOI] [PMC free article] [PubMed] [Google Scholar]