Abstract
For several reasons, cerebral visual impairment (CVI) is emerging as a major cause of visual impairment among children in the developing world and we are seeing an increasing number of such children in our clinics. Owing to lack of early training about CVI and it being a habilitation orientated subject, we need to become equipped to optimally help the affected children. In this paper we have explained our pragmatic approach in addressing children who present with low functioning CVI. Initially we explain briefly, how vision is processed in the brain. We then present what should be specifically looked for in these children in regular clinics as a part of their comprehensive ophthalmic examination. We discuss the process of functional vision evaluation that we follow with the help of videos to explain the procedures, examples of how to convey the conclusions to the family, and how to use our findings to develop intervention guidelines for the child. We explain the difference between passive vision stimulation and vision intervention, provide some common interventions that may be applicable to many children and suggest how to infuse interventions in daily routines of children so that they become relevant and meaningful leading to effective learning experiences.
Keywords: Cerebral visual impairment, developing countries, early intervention, functional vision assessment, interdisciplinary management, multisensory training
Cerebral visual impairment (CVI) is a deficiency in the functions of vision due to damage to or malfunction of the visual pathways and visual processing centres in the brain (specifically those posterior to the lateral geniculate bodies), which may be accentuated by associated disorders of control of eye movements.[1] The spectrum of visual difficulties can range from profound visual impairment (low functioning CVI), to normal/near normal visual acuity but with significant cognitive visual dysfunction (high functioning CVI). It is important to remember that both ocular visual impairment (OVI), and CVI can occur together.
Being a relatively new and complex subject, it is developing differently in different parts of the world. The aim of this article is to present our approach to evaluation and intervention for children with CVI in an Indian setting, developed after studying different set-ups in other parts of the world.
Epidemiology
CVI has recently become the commonest cause of visual impairment in children in developed countries.[2,3,4,5,6,7,8,9,10,11] This is probably due to better management of avoidable causes of childhood blindness like cataract, glaucoma, and ROP in children,[12] combined with improving survival of children who have sustained severe neurological damage during the perinatal period.[13] Improved diagnosis and reporting of this condition may also have led to this reported increase.[14] Children with cerebral palsy have a high probability of additional visual dysfunction due to CVI.[7,15,16,17]
In low-income countries like India, increasing numbers of premature infants and babies with perinatal brain injury are surviving, leading to an increasing prevalence of CVI in children. Data from our centre suggest that CVI is now the most common cause of profound visual impairment in children under 3 years of age - either in isolation or in combination with OVI. Personal experiences shared by several Paediatric Ophthalmologists from different parts of India also indicate that we are increasingly seeing more children with CVI in our clinics. But, neither our residency nor fellowship programs equip eye care professionals to deal adequately with such children. Hence, we felt the need to share our experience with the ophthalmic community.
How Does the Brain See
Fig. 1: Showing the three visual brain areas and the connecting dorsal and ventral streams
Figure 1.
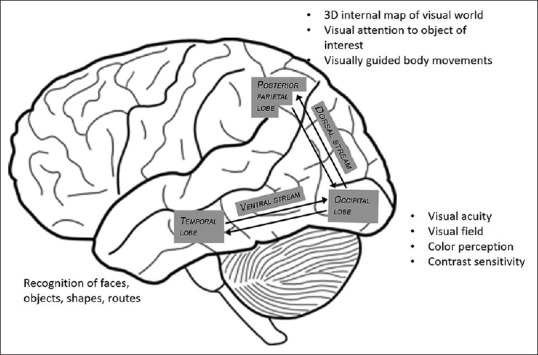
Showing the three visual brain areas, and the connecting dorsal, and ventral streams
The photoreceptors in retina convert light energy into electrical impulses which are transmitted via the bipolar and ganglion cells, through the lateral geniculate bodies to the visual cortices in occipital lobes, where the detail of the picture is resolved (visual acuity), colour is processed, shades of grey are differentiated (contrast sensitivity) and a wide view is created (visual fields). Damage to this area can lead to poor image clarity, impaired ability to perceive colours, and contrast, as well as the typical visual field defects.[18,19,20]
From the occipital lobes, the visual information is sent to 2 destinations which serve the following functions
Bilateral focal dorsal stream damage therefore leads to25 impaired visual guidance of movement (optic ataxia), inability to process many items within the visual scene (simultanagnosia), inability to process multiple sensory inputs like vision and hearing at the same time, inability to move the eyes to look at items that have not been mapped (apraxia of gaze) and often, homonymous lower visual field impairment.
Severe focal damage to the infero-temporal cortices and ventral stream pathways profoundly impairs visual recognition and route finding.
Common causes of CVI and how they affect vision:
Neonatal hypoglycemia
Hydrocephalus[26]
Focal brain lesions like stroke, hemorrhage, focal tumors, and focal cortical dysplasia
Brain injury due to either non-accidental injury (child abuse) or accidental trauma at any age[27]
Brain infections: Meningitis and encephalitis due to bacterial or viral etiology[28]
Brain malformations like holoprosencephaly, lissencephaly, pachygyria, polymicrogyria schizencephaly, and porecephaly[29]
Metabolic disorders like MELAS (mitochondrial myopathy, epilepsy, lactic acidosis, stroke like episodes), Leigh syndrome, several lysosomal disorders, sphingolipidosis, and peroxisomal disorders[30]
Genetic causes: Trisomy 18, trisomy 21, 1p36 deletion syndrome, 17p13.3 deletion syndrome (Miller-Dieker syndrome) and 22q13.3 deletion syndrome (Phelan-McDermid syndrome).[30,31]
Diagnosis
CVI should be suspected in any child whose visual functioning cannot be explained by the ophthalmological findings, more so if the child has a neurological ailment or has a history of an eventful perinatal period.
A close differential diagnosis of CVI in young children is delayed visual maturation (DVM). DVM which, occurring in the absence of other ophthalmic pathology (type 1), is always a retrospective diagnosis. Initially the child appears not to be able to see. No saccades or pursuits or head movement to follow visual targets can initially be elicited. Yet optokinetic eye movements can be evoked and the VEP are normal.[32,33,34]
Clinical Approach
First visit
Knowing details of the medical condition helps understand how the neuro-pathology may influence vision. Details of control of the medical condition (like epilepsy, hydrocephalus) have a significant influence on the visual behavior. The primary goal of the first clinical evaluation in an Ophthalmologist's clinic should be to perform a comprehensive evaluation of accommodation, refraction and eye examination, specifically to look for any treatable ophthalmological problems.
Refractive errors and anomalies of accommodation (Video 1 showing effect of glasses for correcting accommodation) are common in children with CVI.[21,35,36] As a part of the syndrome they may have structural problems like cataract, coloboma, optic atrophy, or retinal dystrophy.[37,38] Retinopathy of prematurity (ROP) may be seen in association with periventricular white matter damage. Optic nerve hypoplasia and optic atrophy are associated with a wide range of brain disorders many of which impair visual function.[39] Disorders of eye movement control are common in children with CVI, like: strabismus, nystagmus, unstable fixation, dysmetric saccades, deficient smooth pursuit movements and paroxysmal deviations, in which the eyes intermittently deviate upwards (most commonly), while evidence of apraxia of gaze needs to be actively sought. Problems with visually guided eye movements can partly be compensated for by head movements (in children with head control).[1,40]
Counselling at the first visit helps families understand what to expect from their interactions with their child. We should focus on the child's strengths and convey that the condition is caused by neural damage which cannot be undone, yet consistent repeated experiences successfully employing measured vision parameters can encourage the brain to make sense of whatever visual, and matched language information is being received. Parents must be made aware that they are the most important people who can optimally teach and communicate with their child. They need to be empowered with knowledge about their child's vision, so as to arrange the environment and select materials to support use of vision and incorporate it into the child's daily routines. We should also guide them about finding experts to control the systemic issues like epilepsy and hydrocephalus.
Second visit
After correcting the treatable ophthalmological problems, the child attends for a second visit, aimed at understanding the child's functional vision. For the sake of convenience, in this article we focus on profound visual impairment, which is the commonest form of CVI seen in our setting.[21]
I. Structured history taking to look for any evidence of vision:[41]
If responses to any of the following questions are positive, measurable visual acuity, using preferential looking methods, is likely to be elicited
-
Does your child:
- Follow people's movements?
- React to someone who is approaching quietly?
- React to lights being turned on and off or to a coloured night light?
- Return a silent smile?
- Reach for food through vision?
- Reach for a bottle or toy left near them?
- React to a reflection of self in a mirror?
- React to and reach for silent objects?
Next seek further details about vision, including-
Place In which locations does your child give the best visual performance?
Time- Does vision vary from hour to hour or from day to day? Are fast moving events seen?
Do some areas of the visual field give better responses than others?
What kinds of distraction interfere with vision? (These include pain, discomfort, auditory noise and visual clutter)
Does your child pay attention to silent or noisy, static or moving targets?
What are the features of the targets that bring about and that maintain attention?
For how long can visual attention be maintained?
What are your child's favourite toys or other things in the environment that he notices visually?
What does your child know and understand about what he or she sees?
If caregivers report limited or no vision, questions can be formulated to address the following possible instances of vision:
Mouth opening when a spoon is brought towards the mouth from the side, but not when brought from straight ahead
Occasional reflex smiling to a moving, large smile from close range when there appears to be little or no other evidence of vision
Improved visual function in darkened conditions (e.g., keeping eyes wide open in the evenings/night)
Discomfort in bright lighting conditions
A tendency to stare at lights.
II. Clinical assessment-
The aim of this assessment is to understand the thresholds for different aspects of vision. In basic terms, in order to be seen by the child:
How big must an object be to be seen (discrimination)?
Proximity within which the child appears to see (visual sphere)
Where is the best seeing part of the visual field?
What level of contrast is needed to see?
Does the child prefer any particular color?
How long does it take for child to look at the object (latency of visual attention)?
How long does the child look at an object (duration of visual attention)?
Is the child able to shift gaze from one visible item to another (saccades and pursuits)?
We find following tests useful:
-
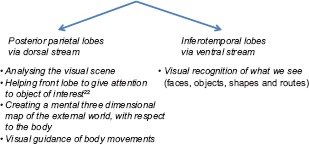
Preferential looking (PL) tests- As per history, if there is some evidence of vision, one of the preferential looking tests, Teller acuity cards or Lea paddles,[42] can be used. These help parents to understand the optimal line thickness and separation between lines that the child can appreciate. While explaining the result to the parents, one should explain the line thickness that the child can appreciate and at what distance, rather than numbers like 20/400 or 2cpd, which in most cases does not make sense to parents
Fig. 2a: Preferential looking test- Lea paddles
Video 2 showing how to use Lea paddles to assess vision in young children
-
Puppet faces- Even when children do not respond to preferential looking tests, many will respond to Puppet faces.[43] The lines are presented in the form of a human face, which is a stronger stimulus for young children than vertical lines. In addition, one can induce a swirling motion to the faces, which tests if the child responds to a moving stimulus instead of a static one
Fig. 2b: Puppet faces to assess vision responsiveness of very low functioning children
If children are unresponsive to either test, playing with the child for a few minutes using a cloth glove in which the tactile features coincide with the visual ones can be a simple way to help them get interested in the test item[44]
Fig. 2c: Cloth glove with puppet face on one side and lines pattern on other side
-
Mirror test- If routine PL tests test are not available, one can use a simple mirror. Place a cloth behind the child to simplify the background visible in the mirror. Start from close to the child's face, gain the child's attention to his/her own image in the mirror and then slowly move away till the child loses eye contact with the mirror image. This distance acts as a rough estimate of the child's visual acuity and has been shown to correlate with TAC[45]
Fig. 2d: Use of mirror to assess vision in young children
The optimal distance at which the child recognizes these stimuli is the visual sphere of the child
-
Visual field - Puppet faces described above can be used for testing the visual field like a confrontation testing, by seeking visual attention when the target is moved out from behind a screen.[43] The Lea wand is also useful for the same purpose[42]
Video 3: Use of Puppet faces to assess visual fields- Infant shown in the video has lower field impairment
Video 4: Use of Lea wand to assess visual fields- The child shown in the video has right hemifield impairment
-
Contrast sensitivity- The Hiding Heidi test also works on the principle of preferential looking and helps one to understand the optimal level of contrast that is needed for the child to see and appreciate an object[42]
Fig. 2e: Hiding Heidi test to assess contrast sensitivity in young children
Video 5: Use of Hiding test to assess contrast sensitivity in young children
-
Color preference- We show illuminated plastic balls of different colors and see if child shows greater interest in certain colours
Video 6: Use of colorful balls to assess any color preference- The child shown in the video has preference for red and yellow color
Latency for visual attention- note how long it takes for the child to take visual cognizance of the stimulus shown
Span of visual attention- Once seen, how long does the child engage with the visual stimulus?
-
Saccades and pursuits: These can be assessed by making the child shift attention between 2 objects (saccades) and follow an interesting object (pursuits).
Video 7: Use of colorful balls separated by a distance being illuminated alternately to assess saccades- child in the video uses head movement rather than eye movement while shifting attention from one ball to the other
Robustness of vision. This refers to the ability to recruit and to sustain visual attention after a change in position (e.g., Supine to sitting or standing, moving and standing still), in the presence of other sensory inputs (sound and touch)
Evidence of blindsight - Response to a moving stimulus in the peripheral visual field but not to a central static stimulus, a silent smile or to an approaching spoon, in the absence of any other evidence of vision, indicates this low level of reflex vision.
Figure 2.
(a) Lea paddles. (b) Puppet faces. (c) Cloth glove with puppet face on one side and lines pattern on other side. (d) Use of mirror to assess vision. (e) Hiding Heidi test. (f) Clutter and noise free room with facility to position the child for functional vision assessment. (g) Simulation of how enhancing facial contrast by make-up may help a child with low visual acuity and low contrast sensitivity-Face without make-up (left), face with make-up (right) as seen by a child with low acuity and contrast sensitivity. (h) Tent with minimal pattern and single plain colour may help reduce visual distractions
Communication with the family and other therapists:
We perform all the above tests in the presence of the parent/care-taker, explaining the purpose and findings of each test, and how they can use the information gained in day-to-day routines. This ensures that all activities fall inside visual threshold so that whatever vision child has gets an opportunity to develop further. This information also needs to be shared with other professionals who deal with the child like the physiotherapist, occupational therapist, speech therapist and special educator.
Examination should be performed in a quiet room with minimal distraction. There should be accommodations to position the child in a way that facilitates maximum use of vision. It is not necessary to finish all assessments in one session. These can be spread over a few sessions depending on the level of reliable cooperation by the child.
Fig. 2f: Clutter free, noise free room with no decorations and facility to position the child in most preferred way is suitable for functional vision assessment
Interventions
Many children with CVI may show little or no useful use of vision. For these children, developing their consciousness and appreciation about visual information is the first step in intervention.
The difference between vision stimulation and vision intervention
Vision stimulation refers to passively watching high contrast visual stimuli in a darkened room. This has little value as it does not develop or utilize the adaptive capacity of the brain. Training of visual functions seems most fruitful when vision activities are adapted to the individual needs and task demands of the child[46]
Vision intervention on the other hand is a dynamic and interactive approach. Here the instructor chooses specific meaningful stimuli found by assessment, and while looking at the child's reaction, makes adjustments to continue to engage the child, by giving meaning to each element of their work together. This helps the child to learn.
Training vision in context:
It is almost always possible to improve visual function at least a little; but interventionists carry a primary responsibility to ensure that the child progresses as age appropriately as possible even in the absence of great improvement in visual function. Therefore vision intervention should be carried out within the context of major developmental activities of childhood including communication, movement, play, and learning activities such reading.
Each of the contexts place a different challenge on the visual system. For example, when we think of vision in the context of social communication, vision provides specific information. We use vision to identify and recognize people, to get information about their emotions and intentions from their expressions and body language, and we compare this visual information with what we hear in the tone of their voice, and the words they speak. Some visual functions and challenges specific to social communication include being able to see low contrast features and slight, fast movements, to visually locate the face, scan visual features, recognize and interpret them, and to hold visual attention in the presence of auditory inputs. Children with CVI may struggle with holding visual attention while listening or when they are under emotional stress or excitement. Thus, visual training in simply locating, following and tracking lights or objects is less likely to help in real life communication situations for these children. Similarly, safe and accurate movement, places different demands on the visual system and is best supported by motor memory and hearing.
By training vision in the context of real situations, we are able to provide vision with appropriate supportive information from other sensory and cognitive systems, so that the child can make sense of the visual inputs available to them. Even in the absence of great improvement of visual functions, if trained appropriately, the child with profound vision impairment, can often learn to use vision effectively as a supportive sense in each life activity area.[47]
Goals and course of intervention
The primary goal of vision intervention is to create opportunity to gain and give meaning to visual information already available. Once the child starts to learn that vision is a valuable source of information, or way to augment information from the other senses, increased periods of visual alertness and self-initiated “looking” behavior become manifest. The child needs support to recruit and use the visual system at this point, because this does not come naturally. Without the reward of success, the more informative sensory system (touch or sound) may otherwise overwhelm the weaker one (vision). Gradually the child learns to meaningfully integrate the sensory inputs.
Children take different pathways in building their ability to use their vision usefully. The important point is not to be afraid of using two sensory systems together as this is how the sensory systems educate and support each other within the child's mind. Another important point is to recognize the limitations of the impairment and not allow it to hold back the child's development - the child may lead with vision to get information for one area of functioning, but have vision as a supporting sense in another.
Making use of limited vision
Often, children with profound CVI may initially only show response to specific strong visual stimuli such as high contrast patterns, movements, and bright colors against a contrasting background, in a dark room, while some simply stare at lights. Reasons for this could be fundamental difficulties in recruiting and activating their attentional systems or the fragmentary and largely meaningless nature of the visual information received. Either way, the strategy is to apply existing vision in situations and ways that are intensely rewarding to the child. For a child who light gazes, hang a toy drum or anklets close to the child's arm and in the path of the light so it is lit and glows and thus captures visual attention. A random movement of the arm brings sound and attention is directed away from the light to the object itself and the child slowly learns how to get more stimulation from the object. When the child reaches to the object the second time, reduce the light, allowing the child to become more interested in the nature of the object itself. The brain starts to recognize that giving visual attention is useful and enjoyable and this is turn results in greater energy being given to recruit and focus visual attention. Attention matures with use and experience, and as ability to sustain attention improves, so also does the quality of information gathered, retained and processed.
In many children with CVI, as the attentional systems mature and as the brain provides alternative ways to process received visual information, dramatic improvements in use of vision can result. Children who begin by giving inconsistent response to light have progressed to using vision to support mobility or even reading. Since this does not always happen, and does not happen across all functional areas, the most effective way to ensure continued improvement in access to information and learning for the child is to always train vision in the context of key areas of normal development.
Making vision part of child's routines
Vision training is most effective when vision is supported throughout the day. Identify and explain opportunities to practice and reinforce natural routines throughout the day. For example, while feeding milk, place shiny paper or a bright colored or a black striped sock on a bottle to make it immediately more visible to the infant, while also giving interesting tactile feedback. Ask the parent to place a single colored towel across their body that contrasts with the color of the sock, get the child to touch the bottle, smell the milk, and then move the bottle just out of reach and within the child's visual sphere, gently supporting the child to reach for it or initially, at least look at it as you pop it unexpectedly into different fields of vision. Later, as the child sucks, place the hands gently around the bottle to give this second source of feedback about the object seen. With an older child, a glass can serve the same purpose. Just 5 minutes of play each mealtime, can become a regular training session and bring great benefits to the child.
General principles of intervention:
Each child with CVI is unique. However, certain general principles apply to most children presenting with profound visual impairment.
Prepare the child: Many children with CVI who present with minimal visual response or interest, need help in activating their attentional and visual systems. A hug, jumping, bouncing, even sucking and blowing, can help center their attention and energy and prepare them for recruiting and using their vision
Importance of posture: Ensure that the child's posture is comfortable to enable him/her to recruit and use vision. Uncomfortable postures tend to drain energy in maintaining the posture. Ensure that the family observes and understands the impact of position on the child's ability to use vision
Prime the child about the object beforehand: Give information before you ask the child to use vision; let the child feel the object so they have a mental construct, which they can use when they search visually
Use descriptive ‘radio’ language (that does not use words which need the child to see the object to understand), to explain what the child is touching, and what information they may be getting through touch – temperature, texture, shape, size, and weight. Providing verbal descriptors helps them to interpret the visual information better and record it better for retrieval
Always insist on looking behavior: – Children with CVI often need time to direct their gaze and bring visual focus to the scene. Waiting for a response for 15 to 30 seconds may be needed, but children must still be encouraged to use vision. They may need some help or support, such target movement, or some other cue, but over time, this need should fade
-
Communication-
Learning how to communicate is a fundamental need for young children. For children with CVI, the following adaptations may be helpful to establish communication and bonding with the care giver.
- The child with CVI should not be left unattended in a cradle for long periods as they learn best through interaction
-
Enhance facial contrast using make-up that matches the measured line thickness, and contrast sensitivity the child can seeFig. 2g: Simulation of how enhancing facial contrast by make-up may help a child with low visual acuity and low contrast sensitivity - Face without make-up (on left), face with make-up (on right) as seen by a child with low acuity and low contrast sensitivity
-
Stay within the child's visual sphere while talkingVideo 8: Showing how to find the distance at which child looks at face comfortably
-
Provide tactile inputs by letting the child touch the faceVideo 9: Communicating with child with profound CVI- putting light on face in dimly lit room to make it high contrast, giving tactile clues by touching hands on face and slow verbal clues
-
Speak slowly and clearly with gaps between repetitions supplemented with matched tactile experiencesVideo 10: Introducing child to ball using high contrast colorful ball of favorite color, tactile clues and slow prolonged pronunciation of word ‘ball’
-
The sensory tent- A single color tent without pattern eliminates visual clutter enabling the child to focus on singular stimuli presented sequentially helps promote visual attention and learning[48]
Fig. 2h: Using tent with minimal pattern and single plain colour may help reduce visual distractions
-
Use of applications (apps) on tablets: We have found the following apps on i-Pad useful for promotion of visual attention, visual tracking and eye-hand coordination: Big Bang Patterns, fluidity, Color Dots, Bubbles, Fluid, BabyShapes-1,2,3 Fireworks, Real Fireworks, Line Art, Glow Lamp, Art Of Glow, Doodle Buddy, EDA PLAY TOBY, Flashlight HD, Kids Doodle, Magic Fingers, Glow Lamp, Splodge, broom-broom. In some of the apps the parameters of the presentation can be modified to match the thresholds of visual processing of the child especially in Big Bang Patterns and Color Dots. Since many children with low functioning CVI have light gazing behavior, we take advantage of it by using an illuminated surface of i-Pad to attract attention to a visual activity. It is important to remember that
- These apps are not substitutes for real objects, which can be ‘felt’, 'smelled’ and ‘experienced’ to create memories for the future
- We recommend their use once the child demonstrates robust self - initiated use of vision for exploration of objects or places. If a child has no or very low visual attention, an app may form a part of the “warm up” for a session, but we quickly move them up to lit objects (objects placed on a light pad for example)[49]
-
Suggestions about objects used for intervention:
- Start with one or two simple chosen items, initially for 5-10 min. Then slowly make changes and additions while being creative
-
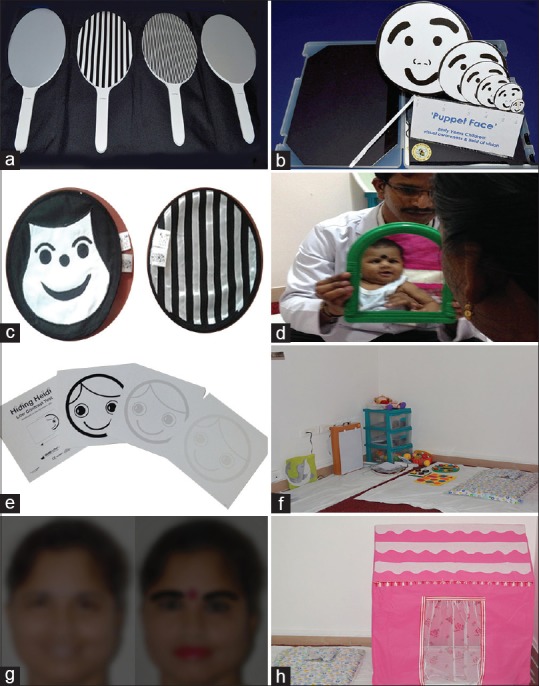
Choose toys that match the threshold of vision as measured during assessment e.g., Toy ‘a’ shown in figure is attractive but not appropriate for a low functioning child, toy ‘b’ is more likely to be perceived being simple, less detail, large line thickness and separation between lines and high contrastFig. 3 showing how to choose appropriate toy as per thresholds of visionToys and items with meaning found in the child's environment are used e.g., stainless steel tumbler, colorful balls
- To attract attention some children need familiar objects, while others need novelty.
- Simplicity of presentation: Presentation of singular simple sequential meaningful stimuli against a simple background is important. Crowded backgrounds tend to render targets invisible for children with simultanagnostic vision due to dorsal stream pathology.
- Competing sensory distractors in the environment such as bright focused ceiling lights, moving ceiling fans, television are eliminated.
Interdisciplinary care - Impaired vision is one of multiple issues that children with brain injury may have. In our published series, close to 60% of children had delay in one or more areas of development.[21] Since, most of the skills impacted are vision dependent, it is important that the experts handling such issues understand how the child sees, and how any visual deficiency compounds the disability. Hence, it is ideal for these therapists to understand the child's vision and provide all therapies under one roof, without requiring children to move from one place to another. We have found that this integrated interdisciplinary approach significantly benefits children and families.
Figure 3.

Showing how to choose appropriate toy as per thresholds of vision: (a) Toy on the left is very attractive but not suitable for a child with profound CVI, but (b) the toy on right would be more appropriate
Conclusion
CVI is one of the most common causes of visual impairment in children in countries like India, but may go unobserved and undetected. One should suspect CVI when ocular examination does not explain the visual behaviour of the child. All ophthalmologists need to ensure that such children undergo a comprehensive eye examination and that all treatable pathologies are identified and addressed early in life. After taking care of such issues, a detailed functional vision evaluation must be done to measure thresholds of multiple parameters of impaired vision that can limit learning like acuity, contrast, and visual fields. Caregivers must be taught how to circumvent these limits and ensure that the child's daily routines are furnished with accessible information and learning. This optimises the environment for the child's limited visual function to develop. Passive stimulation using colourful lights in the dark have no role in the management of such children as it has no meaning, but in our experience, thoughtful and interactive vision intervention activities can make an enormous difference. Vision training in isolation is unlikely to be successful but interdisciplinary integrated care by parents and all the therapists is manifestly effective. Research in this area of study is awaited.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos Available on: www.ijo.in
Acknowledgements
We are thankful the Hyderabad Eye Research Foundation and Hyderabad Eye Institute for assistance in conducting this study.
We are grateful to following experts for their invaluable suggestions in preparation of this manuscript:
Prof Gordon N Dutton, Emeritus Professor of Visual Science, Department of Vision Science, Glasgow Caledonian University, Glasgow, Scotland, UK
Dr Beula Christy, Head, Institute of Vision Rehabilitation, L V Prasad Eye Institute, Kallam Anji Reddy campus, Hyderabad, India.
References
- 1.Dutton GN, Leuck AH. In Vision and the Brain, Amanda Hall Leuck, and Gordon N Dutton (eds) New York: AFB Press; 2015. Impairment of Vision due to damage to the brain; p. 13. [Google Scholar]
- 2.Ozturk T, Er D, Yaman A, Berk AT. Changing trends over the last decade in the aetiology of childhood blindness: A study from a tertiary referral centre. Br J Ophthalmol. 2016;100:166–71. doi: 10.1136/bjophthalmol-2015-306737. [DOI] [PubMed] [Google Scholar]
- 3.Chong C, Dai S. Cross-sectional study on childhood cerebral visual impairment in New Zealand. Eye (Lond) 2008;22:905–11. doi: 10.1016/j.jaapos.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 4.Bunce C, Wormald R. Causes of blind certifications in England and Wales: April 1999-March 2000. J AAPOS. 2014;18:71–4. doi: 10.1038/sj.eye.6702767. [DOI] [PubMed] [Google Scholar]
- 5.Nielsen LS, Skov L, Jensen H. Visual dysfunctions and ocular disorders in children with developmental delay. I. prevalence, diagnoses and aetiology of visual impairment. Acta Ophthalmol Scand. 2007;85:149–56. doi: 10.1111/j.1600-0420.2006.00867.x. [DOI] [PubMed] [Google Scholar]
- 6.Hatton DD, Schwietz E, Boyer B, Rychwalski P. Babies Count: The national registry for children with visual impairments, birth to 3 years. J AAPOS. 2007;11:351–5. doi: 10.1016/j.jaapos.2007.01.107. [DOI] [PubMed] [Google Scholar]
- 7.Matsuba CA, Jan JE. Long-term outcome of children with cortical visual impairment. Dev Med Child Neurol. 2006;48:508–12. doi: 10.1017/S0012162206001071. [DOI] [PubMed] [Google Scholar]
- 8.Flanagan NM, Jackson AJ, Hill AE. Visual impairment in childhood: Insights from a community-based survey. Child Care Health Dev. 2003;29:493–9. doi: 10.1046/j.1365-2214.2003.00369.x. [DOI] [PubMed] [Google Scholar]
- 9.Alagaratnam J, Sharma TK, Lim CS, Fleck BW. A survey of visual impairment in children attending the Royal Blind School, Edinburgh using the WHO childhood visual impairment database. Eye (Lond) 2002;16:557–61. doi: 10.1038/sj.eye.6700149. [DOI] [PubMed] [Google Scholar]
- 10.Rogers M. Vision impairment in Liverpool: Prevalence and morbidity. Arch Dis Child. 1996;74:299–303. doi: 10.1136/adc.74.4.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blohmé J, Tornqvist K. Visual impairment in Swedish children. III. Diagnoses. Acta Ophthalmol Scand. 1997;75:681–7. doi: 10.1111/j.1600-0420.1997.tb00630.x. [DOI] [PubMed] [Google Scholar]
- 12.McClelland J, Saunders KJ, Hill N, Magee A, Shannon M, Jackson AJ. The changing visual profile of children attending a regional specialist school for the visually impaired in Northern Ireland. Ophthalmic Physiol Opt. 2007;27:556–60. doi: 10.1111/j.1475-1313.2007.00523.x. [DOI] [PubMed] [Google Scholar]
- 13.Rudanko SL, Fellman V, Laatikainen L. Visual impairment in children born prematurely from 1972 through 1989. Ophthalmology. 2003;110:1639–45. doi: 10.1016/S0161-6420(03)00498-6. [DOI] [PubMed] [Google Scholar]
- 14.Bamashmus MA, Matlhaga B, Dutton GN. Causes of blindness and visual impairment in the West of Scotland. Eye (Lond) 2004;18:257–61. doi: 10.1038/sj.eye.6700606. [DOI] [PubMed] [Google Scholar]
- 15.Park MJ, Yoo YJ, Chung CY, Hwang JM. Ocular findings in patients with spastic type cerebral palsy. BMC Ophthalmol. 2016;16:195. doi: 10.1186/s12886-016-0367-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghasia F, Brunstrom J, Gordon M, Tychsen L. Frequency and severity of visual sensory and motor deficits in children with cerebral palsy: Gross motor function classification scale. Invest Ophthalmol Vis Sci. 2008;49:572–80. doi: 10.1167/iovs.07-0525. [DOI] [PubMed] [Google Scholar]
- 17.Pennefather PM, Tin W. Ocular abnormalities associated with cerebral palsy after preterm birth. Eye (Lond) 2000;14:78–81. doi: 10.1038/eye.2000.17. [DOI] [PubMed] [Google Scholar]
- 18.Milner AD. How do the two visual streams interact with each other? Exp Brain Res. 2017;235:1297–308. doi: 10.1007/s00221-017-4917-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Milner D, Goodale M. 2nd ed. Oxford: Oxford University Press; 2006. The Visual Brain in Action. [Google Scholar]
- 20.Saur D, Kreher BW, Schnell S, Kümmerer D, Kellmeyer P, Vry MS, et al. Ventral and dorsal pathways for language. Proc Natl Acad Sci U S A. 2008;105:18035–40. doi: 10.1073/pnas.0805234105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pehere N, Chougule P, Dutton GN. Cerebral visual impairment in children: Causes and associated ophthalmological problems. Indian J Ophthalmol. 2018;66:812–5. doi: 10.4103/ijo.IJO_1274_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jacobson LK, Dutton GN. Periventricular leukomalacia: An important cause of visual and ocular motility dysfunction in children. Surv Ophthalmol. 2000;45:1–13. doi: 10.1016/s0039-6257(00)00134-x. [DOI] [PubMed] [Google Scholar]
- 23.Edmond JC, Foroozan R. Cortical visual impairment in children. Curr Opin Ophthalmol. 2006;17:509–12. doi: 10.1097/ICU.0b013e3280107bc5. [DOI] [PubMed] [Google Scholar]
- 24.Brooks BP, Simpson JL, Leber SM, Robertson PL, Archer SM. Infantile spasms as a cause of acquired perinatal visual loss. J AAPOS. 2002;6:385–8. doi: 10.1067/mpa.2002.129796. [DOI] [PubMed] [Google Scholar]
- 25.Castano G, Lyons CJ, Jan JE, Connolly M. Cortical visual impairment in children with infantile spasms. J AAPOS. 2000;4:175–8. [PubMed] [Google Scholar]
- 26.Houliston MJ, Taguri AH, Dutton GN, Hajivassiliou C, Young DG. Evidence of cognitive visual problems in children with hydrocephalus: A structured clinical history-taking strategy. Dev Med Child Neurol. 1999;41:298–306. doi: 10.1017/s0012162299000675. [DOI] [PubMed] [Google Scholar]
- 27.Woodward GA. Posttraumatic cortical blindness: Are we missing the diagnosis in children? Pediatr Emerg Care. 1990;6:289–92. doi: 10.1097/00006565-199012000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Ackroyd RS. Cortical blindness following bacterial meningitis: A case report with reassessment of prognosis and aetiology. Dev Med Child Neurol. 1984;26:227–30. doi: 10.1111/j.1469-8749.1984.tb04435.x. [DOI] [PubMed] [Google Scholar]
- 29.Dumoulin SO, Jirsch JD, Bernasconi A. Functional organization of human visual cortex in occipital polymicrogyria. Hum Brain Mapp. 2007;28:1302–12. doi: 10.1002/hbm.20370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bosch DG, Boonstra FN, Reijnders MR, Pfundt R, Cremers FP, de Vries BB. Chromosomal aberrations in cerebral visual impairment. Eur J Paediatr Neurol. 2014;18:677–84. doi: 10.1016/j.ejpn.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 31.Bosch DG, Boonstra FN, de Leeuw N, Pfundt R, Nillesen WM, de Ligt J, et al. Novel genetic causes for cerebral visual impairment. Eur J Hum Genet. 2016;24:660–5. doi: 10.1038/ejhg.2015.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tresidder J, Fielder AR, Nicholson J. Delayed visual maturation: Ophthalmic and neurodevelopmental aspects. Dev Med Child Neurol. 1990;32:872–81. [PubMed] [Google Scholar]
- 33.Harris CM, Kriss A, Shawkat F, Taylor D, Russell-Eggitt I. Delayed visualmaturation in infants: A disorder of figure-ground separation? Brain Res Bull. 1996;40:365–9. doi: 10.1016/0361-9230(96)00128-1. [DOI] [PubMed] [Google Scholar]
- 34.Bianchi PE, Salati R, Cavallini A, Fazzi E. Transient nystagmus in delayed visual maturation. Dev Med Child Neurol. 1998;40:263–5. doi: 10.1111/j.1469-8749.1998.tb15459.x. [DOI] [PubMed] [Google Scholar]
- 35.Saunders KJ, McClelland JF, Richardson PM, Stevenson M. Clinical judgement of near pupil responses provides a useful indicator of focusing ability in children with cerebral palsy. Dev Med Child Neurol. 2008;50:33–7. doi: 10.1111/j.1469-8749.2007.02012.x. [DOI] [PubMed] [Google Scholar]
- 36.Saunders KJ, Little JA, McClelland JF, Jackson AJ. Profile of refractive errors in cerebral palsy: Impact of severity of motor impairment (GMFCS) and CP subtype on refractive outcome. Invest Ophthalmol Vis Sci. 2010;51:2885–90. doi: 10.1167/iovs.09-4670. [DOI] [PubMed] [Google Scholar]
- 37.Fazzi E, Signorini SG, Bova SM, La Piana R, Ondei P, Bertone C, et al. Spectrum of visual disorders in children with cerebral visual impairment. J Child Neurol. 2007;22:294–301. doi: 10.1177/08830738070220030801. [DOI] [PubMed] [Google Scholar]
- 38.Jacobson L, Lundin S, Flodmark O, Ellstrom KG. Periventricular leukomalacia causes visual impairment in preterm children. A study on the aetiologies of visual impairment in a population-based group of preterm children born 1989–95 in the county of Varmland, Sweden. Acta Ophthalmol Scand. 1998;76:593–8. doi: 10.1034/j.1600-0420.1998.760516.x. [DOI] [PubMed] [Google Scholar]
- 39.Zeki SM, Hollman AS, Dutton GN. Neuroradiological features of patients with optic nerve hypoplasia. J PediatrOphthalmol Strabismus. 1992;29:107–12. doi: 10.3928/0191-3913-19920301-11. [DOI] [PubMed] [Google Scholar]
- 40.Jacobson L, Ygge J, Flodmark O. Nystagmus in peri- ventricular leucomalacia. Br J Ophthalmol. 1998;82:1026–32. doi: 10.1136/bjo.82.9.1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dutton GN, Calvert J. Impairment of Cognitive Vision: Its detection and measurement. In: Gordon Dutton, Martin Bax., editors. In Visual Impairment in Children due to Damage to the Brain. London: Wiley-Blackwell publishers; 2010. pp. 125–6. [Google Scholar]
- 42. [Last accessed on 2018 Dec 10]. Available from: htps://www.good-lite.com/Details.cfm?ProdID=44 .
- 43. [Last accessed on 2018 Dec 10]. Available from: http://www.beesneez.co.uk/Puppetface.htm .
- 44. [Last accessed on 2018 Dec 10]. Available from: http://www.chetana.org.in/vision.php .
- 45.Bowman R, McCulloch DL, Law E, Mostyn K, Dutton GN. The ‘mirror test’ for estimating visual acuity in infants. Br J Ophthalmol. 2010;94:882–5. doi: 10.1136/bjo.2009.162750. [DOI] [PubMed] [Google Scholar]
- 46.Vervloed MP, Janssen N, Knoors H. Visual rehabilitation of children with visual impairments. J Dev Behav Pediatr. 2006;27:493–506. doi: 10.1097/00004703-200612000-00008. [DOI] [PubMed] [Google Scholar]
- 47.Jacob N. Enabling learning thought sensory development in children who are deafblind. DBI Review. 2013;50:18–21. [Google Scholar]
- 48.Little S, Dutton GN. Some children with multiple disabilities and cerebral visual impairment can engage when enclosed by a ‘tent’: Is this due to Balint syndrome? Br J Vis Impair. 2014;33:66–73. [Google Scholar]
- 49. [Last accessed on 2018 Dec 10]. Available from: http://www.chetana.org.in/pdf/resourcematerial/Light%20pad%20activities_awareness%20&%20interest.pdf .
- 50.Macaluso E, Frith CD, Driver J. Multisensory stimulation with or without saccades: fMRI evidence for crossmodal effects on sensory-specific cortices that reflect multisensory location-congruence rather than task-relevance. Neuroimage. 2005;26:414–25. doi: 10.1016/j.neuroimage.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 51.Renier LA, Anurova I, De Volder AG, Carlson S, VanMeter J, Rauschecker JP. Preserved functional specialization for spatial processing in the middle occipital gyrus of the early blind. Neuron. 2010;68:138–48. doi: 10.1016/j.neuron.2010.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


