Abstract
An 84-year-old gentleman underwent uneventful femtolaser-assisted cataract surgery (FLACS) with an arcuate keratotomy (AK) in the left eye. On the 18th post-operative day, a corneal infiltrate developed involving the AK. Staphylococcus epidermidis was the organism isolated on culture. The infiltrate resolved with topical fortified vancomycin and amikacin eyedrops, and the patient regained a visual acuity of 6/6 after 12 weeks. This is the first case from south-east Asia reported in the literature of an infective infiltrate along a femtosecond laser AK. We propose strict peri-operative recommendations to be followed to prevent and treat such infections.
Keywords: Arcuate keratotomy, femtolaser-assisted cataract surgery, infiltration
Arcuate keratotomy (AK) is an efficacious intraoperative procedure for reduction of pre-existing corneal astigmatism between 0.5 and 3.0 D.[1] However, it may also act as an additional route of entry of micro-organisms, increasing the risk of post-operative infection.[2,3,4] The advent of femtosecond laser has made it possible to create highly accurate and well-structured AKs. We report first case of femtosecond laser AK infiltration from south-east Asia, and also propose recommendations for prevention and treatment of these cases.
Case Report
An 84-year-old gentleman underwent femtosecond laser-assisted cataract surgery (FLACS) in the left eye (LE) for grade III nuclear cataract. There was no known history of diabetes mellitus, hypertension, or any immunocompromised state. No evidence of any local or systemic infection was noted. The pre-operative regimen included topical moxifloxacin 0.5% starting three days prior to the surgery. Painting of peri-ocular skin and instillation of 5% povidone iodine drop into the conjunctival cul-de-sac was done prior to the femtolaser procedure as well as phacoemulsification. His corneal curvature revealed astigmatism of 1.0 D (K1 – 44.1 D at 94° and K2 – 45.1 D at 4°). An arcuate keratotomy was planned using the femtolaser platform (Catalys Precision Laser System, Abbott Medical Optics, Inc.) using the Julian Stevens nomogram. An anterior penetrating AK of 80% depth and 30° arc length was created on the steep axis, with a 9 mm optical zone, centered on the limbus. The AK was opened manually at the end of an uneventful surgery.
The post-operative regimen comprised of moxifloxacin 0.5% - dexamethasone 0.1% drop for ten days, followed by prednisolone acetate 1% drop in a tapering dose over 6 weeks. On the first post-operative day (POD), the corrected distance visual acuity (CDVA) was 6/9 in the operated eye, with no significant inflammatory reaction, and complete re-epithelialization of the AK.
On the 18th POD, the patient presented with pain, redness and photophobia in the LE. The CDVA had dropped to 6/18. On slit lamp examination, an infiltrate, 1.5 mm in length, was visible along the AK, involving the margins and full thickness of the incision. Anterior chamber reaction was present (cells+++, flare++++) [Fig. 1a and b]. The intraocular pressure (IOP) was 24 mm Hg. A B-scan ultrasound was performed to look for posterior segment pathology, but no signs of endophthalmitis were seen. The patient did not give any history of trauma, foreign body, or even tap water entering the eyes. The fellow eye examination was unremarkable except for grade II nuclear cataract.
Figure 1.
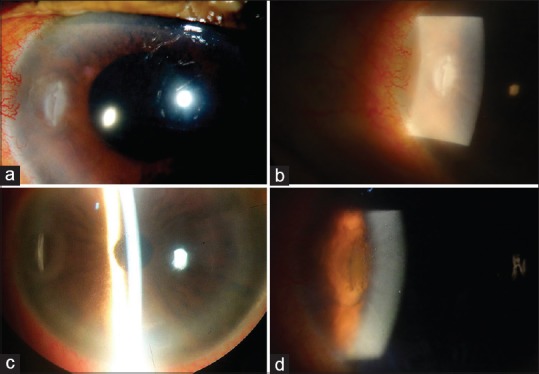
(a and b). Slit lamp photographs of left eye showing infiltrate along arcuate keratotomy incision with vascularization (18th pod). (c). Slit lamp photograph of left eye—4th post operative week, showing resolving infiltrate. (d). Slit lamp photograph of left eye—12th post operative week, showing resolved infiltrate
The patient was started on hourly moxifloxacin 0.5% and tobramycin 0.3% empirically. Prednisolone acetate 1% eyedrop was continued 6 times a day. Betaxolol 0.5% was given twice daily to reduce the IOP.
The response to topical antibiotics was equivocal, and the patient was taken up for scraping from the AK site on the 20th POD. On culture, Staphylococcus epidermidis was the organism found, and it was sensitive to amikacin and vancomycin. The patient was shifted to hourly fortified vancomycin (25 mg/ml), and fortified amikacin (13 mg/ml). He was followed up daily for the next ten days [Fig. 1c]. Over this period, the infiltrate and hypopyon gradually resolved, and the CDVA improved to 6/9. The patient was then followed up weekly, and at last visit (12th post-operative week), the CDVA was recorded as 6/6, with no infiltrate or scarring along the AK [Fig. 1d].
Discussion
To the best of our knowledge, this is the first case to be reported from south-east Asia of an infiltration along the AK created by femtosecond laser, following an uneventful FLACS. Earlier in 2015, Chou et al. from USA had reported a case of femtolaser LRI which showed infiltration due to methicillin-resistant Staphylococcus aureus after an uneventful FLACS.[2] Recently, in 2018, Grillo et al. reported a case of late onset Microsporidial keratitis following an uneventful FLACS with femtosecond laser AK in the USA.[3] In India, Haripriya et al. had reported a case of keratitis and a case of endophthalmitis following manual LRI in phacoemulsification.[4,5]
Arcuate keratotomy may thus act as a double-edged sword, with increased risk of intraocular infection. Multiple factors such as pre-existing local or systemic infection, age of the patient, systemic disorders such as diabetes mellitus or immunocompromised state, increase this risk. These patients should be screened out before planning for an AK. Local infections such as blepharitis, chronic dacryocystitis, conjunctivitis, rhinitis, and sinusitis should be adequately treated prior to surgery.
Intraoperatively, cleaning of the peri-ocular area and instillation of 5% povidone iodine solution drop is of utmost importance. Early onset keratitis following a corneal incision-based procedure is defined as occurring within 30 days from the surgery.[6] These are caused by contamination of the ocular surface by micro-organisms during or immediately after surgery. The organism isolated in our case was Staphylococcus epidermidis, a known inhabitant of the conjunctival flora. Hence, povidone iodine antisepsis is mandatory prior to femtolaser procedure as well as phacoemulsification.
Post-operatively, topical antibiotic coverage for 1 week is of paramount importance in such patients. The anterior penetrating type of AK wounds must be closely followed up for complete re-epithelialization. In case of infiltration, early detection and treatment is the mainstay of therapy. Endophthalmitis must be ruled out with a posterior segment evaluation. Early scraping and microbiological assay help to choose the right antimicrobial drug based on culture sensitivity report. Close follow up to document the progression or remittance of the infiltrate is crucial.
To conclude, femtosecond laser arcuate keratotomy, though a very important tool in the armamentarium of the cataract surgeon, should be used judiciously. The reported cases of infective infiltrate are very few all over the world. Nevertheless, patient selection for this procedure should be meticulous, all necessary peri-operative aseptic and antiseptic measures must be strictly followed, and a close follow-up is essential.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Amesbury EC, Miller KM. Correction of astigmatism at the time of cataract surgery. Curr Opin Ophthalmol. 2009;20:19–24. doi: 10.1097/ICU.0b013e328319c27a. [DOI] [PubMed] [Google Scholar]
- 2.Chou TY, Abazari A, Barash A, Shah S, Kaplowitz K. Early-onset Methicillin-resistant Staphylococcus aureus keratitis and late-onset infectious keratitis in astigmatic keratotomy incision following femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2015;41:1772–7. doi: 10.1016/j.jcrs.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 3.Grillo LM, Epstein IJ, Donnenfeld ED, Perry HD. Late-onset microsporidial keratitis in femtosecond astigmatic keratotomy after laser-assisted phacoemulsification. Cornea. 2018;37:1471–3. doi: 10.1097/ICO.0000000000001743. [DOI] [PubMed] [Google Scholar]
- 4.Haripriya A, Smita A. A case of keratitis associated with limbal relaxing incision. Indian J Ophthalmol. 2016;64:936–7. doi: 10.4103/0301-4738.198862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haripriya A, Syeda TS. A case of endophthalmitis associated with limbal relaxing incision. Indian J Ophthalmol. 2012;60:223–5. doi: 10.4103/0301-4738.95879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heidemann DG, Dunn SP, Chow CYC. Early- versus late onset infectious keratitis after radial and astigmatic keratotomy: Clinical spectrum in a referral practice. J Cataract Refract Surg. 1999;25:1615–9. doi: 10.1016/s0886-3350(99)00285-0. [DOI] [PubMed] [Google Scholar]


