Abstract
A 28-year-old male presented to retina clinic with complains of blurring and distortion in right eye for past 1 week. There was history of implantation of phakic intraocular lens (pIOL) bilaterally 4 months back. Ophthalmic examination revealed a full-thickness macular hole in the right eye. Pars plana vitrectomy with inverted internal limiting membrane flap was planned. Post-operatively, patient had a good gain in vision (20/40) with closure of the hole. Macular hole is an unusual complication of pIOL. A detailed pre-operative fundus screening is indispensable. Early presentation and timely intervention can optimize the visual outcome.
Keywords: Autofluorescence, ICL, Implantable collamer lens, macular hole, pars plana vitrectomy
Phakic intraocular lens (pIOL) has gained popularity in the last few decades for correction of high myopia in patients where corneal refractive procedures are contraindicated. While the procedure has the advantages of superior visual outcomes and reversibility, there are reports of various vision-threatening complications like retinal detachment[1] and giant retinal tears.[2] We present a rare occurrence of macular hole (MH) as a complication of pIOL implantation in a high myope. High myopia is an independent risk factor for the development of macular hole and surgical intervention accelerates the changes at the vitreoretinal interface predisposing such eyes to retinal complications.
Case Report
A 28-year-old male presented to our clinic with the chief complaint of blurring of central vision and metamorphopsia OD for past 1 week. There was a history of implantation of phakic intraocular lens (pIOL) (Implantable phakic contact lens, IPCL, Care group, India) for correction of myopia (-13D OD and - 14.5D OS) 4 months back elsewhere following which the patient achieved a vision of 20/20. Presurgical ophthalmic record was non-contributory. There were no obvious retinal or vitreous changes, preoperatively.
On presentation, best corrected visual acuity (BCVA) was 20/125 OD and 20/20 OS. Intraocular pressure was 12 and 14 mmHg in right and left eye, respectively. On slit lamp examination, presence of pIOL was noted in both the eyes [Fig. 1a and b] with adequate vault on ASOCT. Rest of the anterior segment was unremarkable. On dilated fundus examination, presence of early onset incomplete posterior vitreous detachment with peripheral lasered lattices were noted in the right eye. Slit lamp biomicroscopic examination of posterior pole revealed a MH in the affected eye. The fundus in the left eye showed lasered lattice at the supero-temporal periphery. Spectral domain optical coherence tomography (SD-OCT) in the right eye [Fig. 2a] confirmed the presence of full-thickness MH (minimal base diameter of 362 micron, macular hole index = 0.9) with cystic cavities in the walls. Fundus autofluorescence image (FAF) OD [Fig. 3a] showed fundus hyperautofluorescence corresponding to the MH.
Figure 1.
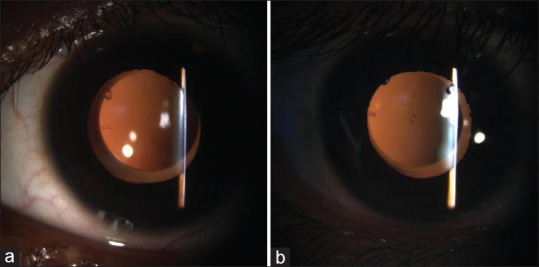
Slit lamp photograph of right and left eye (a and b) in retro illumination mode showing presence of posterior chamber phakic intraocular IOL
Figure 2.
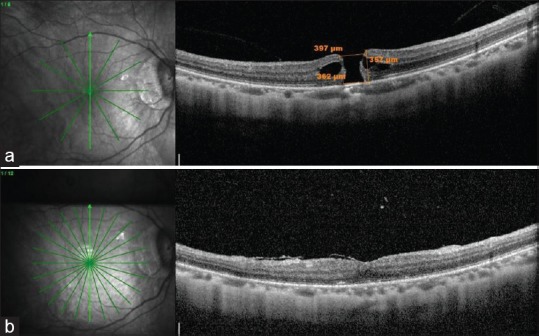
Spectral domain optical coherence tomography (SD-OCT) OD (a) Pre-operatively showing full thickness macular hole with cystic spaces in the wall; (b) Post-operatively at 3 weeks showing anatomical closure of macular hole
Figure 3.
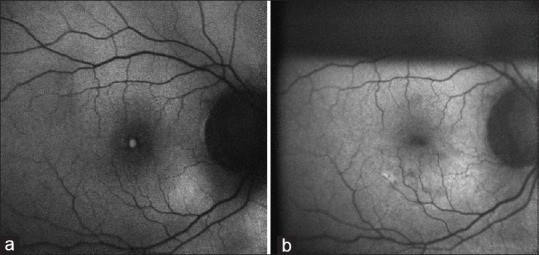
FAF image OD (a) Pre-operatively showing hyperautofluorescence corresponding to the macular hole and a circumferential hypoautofluorescence; (b) Post-operatively at 3 weeks showing decreased foveal hyperautofluorescence after surgery suggesting anatomical closure of the macular hole
23G pars plana vitrectomy was planned. Intraoperatively, brilliant blue G (BBG 0.05% w/v) dye-assisted internal limiting membrane (ILM) peeling with inverted ILM flap followed by fluid-gas exchange for endotamponade (14% SF6 gas) was performed. Prone positioning was advised to the patient for 1 week. Post-operatively at 2 weeks, BCVA improved to 20/40 and the anatomical closure of the macular hole was confirmed on SD-OCT and FAF [Figs. 2b and 3b]. The same is maintained at a follow-up of 6 weeks.
Discussion
Macular hole is mostly idiopathic and commonly seen in elderly females. It has also been seen in association with myopia, trauma, scleral buckling, pneumatic retinopexy, vitrectomy, and rarely following laser-assisted in situ keratomileusis, and cataract surgery.[3] Its occurrence following pIOL is much rarer.[4] Phakic IOL has become one of the most popular options in high myopes who are unsuitable for surface ablative refractive surgeries. However, the surgery entails the risk of vitreoretinal complications like endophthalmitis, retinal tears and detachment, and giant retinal tear.[1,2]
As suggested by Gass, the primary pathology in MH is the progressive antero-posterior and/or tangential traction in the pre-macular vitreous cortex at the retinal interface.[5] Phakic IOL surgery may induce or expediate the changes in vitreomacular interface, which lead to MH formation in myopes. A previous report of two cases of MH following implantation of Implantable collamer lens described several mechanisms of MH formation. According to them, MH could either be pre-existing that was missed pre-operatively, or a part of natural course of high myopic change or induced by the surgery (pIOL implantation).[4] Our patient developed symptoms of metamorphopsia 4 months after pIOL implantation. Therefore, we assume that pIOL implantation might have accelerated the process of vitreous syneresis, posterior vitreous detachment (PVD) and a resultant MH formation in our patient. This case underscores the significance of preoperative fundus screening that must be supplemented with posterior segment OCT, when needed.
Surgical management of MH in patients with phakic IOL is highly challenging.[6] Difficulties and risks vitreoretinal surgery in such cases include:
The plate haptic of pIOL makes the visualisation of retinal periphery difficult with wide angle viewing system, intraoperatively
As the patients of pIOL are generally high myopes with very thin retinas, there is greater risk of iatrogenic retinal break formation during PVD induction. Interface vitrectomy under air for peripheral vitreous removal is very helpful to prevent inadvertent break formation
There is high chance of missing a retinal break owing to severe chorioretinal atrophy and impaired visualisation of the peripheral fundus
Thin ILM, long axial length and presence of posterior staphyloma makes ILM peeling and flap creation highly challenging
There is a risk of pIOL rotation intraoperatively or postoperatively leading to loss of toricity in case of toric lenses, lens touch leading to cataract formation, or iris touch causing uveitis due to up thrust by the gas endo-tamponade.
However, with expertise and good surgical technique these challenges could be overcome successfully to provide optimal anatomical and functional success.
Our case emphasizes the importance of fundus examination before and after IOL implantation to look for vitreoretinal pathology. Albeit, the incidence of this complication remains rare, our case highlights the importance of informing patients about the risk and the symptoms of macular hole that should lead the patient to emergency facilities to be treated as early and as efficiently as possible.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Jiang T, Chang Q, Wang X, Huang X. Retinal detachment after phakic intraocular lens implantation in severe myopic eyes. Graefes Arch Clin Exp Ophthalmol. 2012;250:1725–30. doi: 10.1007/s00417-012-2002-z. [DOI] [PubMed] [Google Scholar]
- 2.Rizzo S, Belting C, Genovesi-Ebert F. Two cases of giant retinal tear after implantation of a phakic intraocular lens. Retina. 2003;23:411–3. doi: 10.1097/00006982-200306000-00024. [DOI] [PubMed] [Google Scholar]
- 3.Arevalo JF, Mendoza AJ, Velez-Vazquez W, Rodriguez FJ, Rodriguez A, Rosales-Meneses JL, et al. Full-thickness macular hole after LASIK for the correction of myopia. Ophthalmology. 2005;112:1207–12. doi: 10.1016/j.ophtha.2005.01.046. [DOI] [PubMed] [Google Scholar]
- 4.Jun JH, Kim YC, Kim KS. Macular hole after phakic intraocular lens implantation: Two cases with divergent manifestations. Semin Ophthalmol. 2014;29:213–7. doi: 10.3109/08820538.2013.835839. [DOI] [PubMed] [Google Scholar]
- 5.Gass JD. Idiopathic senile macular hole. Its early stages and pathogenesis. Arch Ophthalmol. 1988;106:629–39. doi: 10.1001/archopht.1988.01060130683026. [DOI] [PubMed] [Google Scholar]
- 6.Kumar A, Mehta A, Ravani RD, Kakkar P. Management of a case of myopic foveoschisis with phakic intraocular lens (pIOL) in situ: Intraoperative challenges. BMJ Case Rep 2017. 2017 doi: 10.1136/bcr-2016-218224. doi: 10.1136/bcr-2016-218224. [DOI] [PMC free article] [PubMed] [Google Scholar]


