Abstract
Purpose:
To know the pattern of presentations and management outcome of steroid induced glaucoma in vernal keratoconjunctivitis (VKC).
Methods:
Children of VKC using steroid with two of the following criteria were enrolled: Intraocular pressure (IOP) >21 mm Hg, glaucomatous optic disc and visual field defects. Misused topical steroids were classified in 4 groups; A- Highly potent drugs (dexamethasone, betamethasone), B- Moderate (prednisolone), C- Weak (loteprednol, fluorometholone), D- Unknown drugs. Active/conservative interventions were done to control IOP. Corrected distance visual acuity (CDVA), IOP, anterior segment and fundus examinations were noted. One-way ANOVA test and post hoc Tukey HSD test were used to compare the groups.
Results:
Out of 1423 VKC patients, 240 were using topical steroid without prescriptions. 92 eyes of 47 patients had steroid induced glaucoma. Hence prevalence of this complication was 3.30% in this study population. Mean age was 14.1 ± 3.8 years. Mean IOP was 38 ± 12 mm of Hg and mean vertical cup disc ratio was 0.67 ± 0.25. IOP was controlled by withdrawal of steroids (9 eyes), with antiglaucoma medications (27), trabeculectomy (57) and glaucoma drainage device (1). Mean CDVA at presentation was better in group C (0.23 log MAR). Mean IOP was highest in group A (43.1 mm Hg) followed by group D (40.5 mm Hg). At presentation 17 were blind (CDVA <3/60). Post treatment marginal improvement in CDVA was found (P = 0.46). However, statistically significantly improvement was noticed in IOP (P < 0.00001).
Conclusion:
Injudicious use of steroids leads to vision threatening complications like ocular hypertension and glaucoma in children of VKC. Weak steroids like loteprednol or fluorometholone should be used instead of higher potency drugs. Vision and IOP should be monitored fortnightly in children using topical steroids to detect steroid responders at the earliest.
Keywords: Steroid induced glaucoma, steroid misuse, vernal keratoconjunctivitis
Vernal keratoconjunctivitis (VKC) is a bilateral, chronic, external ocular inflammatory disorder; mainly affecting subjects in their first or second decade mostly in temperate climate.[1,2,3] It is a type 1 IgE mediated hypersensitivity reaction.[4,5,6,7,8] It causes intense ocular itching, tearing, mucous stringy discharge, photophobia, blepharospasm and foreign body sensation.[9,10]
The treatment of VKC includes cold compresses, artificial tears, avoidance of specific/nonspecific triggers, and application of topical ophthalmic preparations ranging from anti-histamines and mast cell stabilizers to periodic use of topical corticosteroids.[10] Up to 85% of subjects require corticosteroids at some point during the course of their illness.[11,12] The more severe the disease process is, the more symptomatically devastating it is and the more potent the treatment must be to alleviate symptoms and achieve disease quiescence.[11] Often mild steroids have to be prescribed for a longer duration due to severe and chronic nature of disease. Due to its potency, high effectiveness and early symptomatic relief, corticosteroids are abused without the knowledge of its vision threatening complications, mainly cataract and glaucoma.[13,14,15]
In our clinical practice, we come across patients with VKC with rise of IOP due to steroid use and these steroids are either prescribed by pharmacy, quacks or general practitioners.[16] In our hospital, we have observed that patients of VKC are unaware of side effects of steroid medications and are in the habit of using them because of quick action and relief of symptoms. Many have studied steroid induced glaucoma in the past, but no study has been exclusively done in children of VKC with ocular hypertension, which has public health importance. Therefore, the aim of this study is to know the pattern of presentation and management outcome of steroid induced glaucoma in children with VKC.
Methods
This is a retrospective and descriptive analytical study. After approval of institutional review board, medical records of patients (less than 18 years of age) who presented for the first time and were already taking treatment elsewhere for VKC were analysed from January 2016 to December 2017. The study followed the tenets of declaration of Helsinki. Those patients of VKC using topical steroid or systemic steroids, who had at least two of the following three criteria, were recruited for the study: IOP more than 21 mm Hg on more than two occasions (ocular hypertension), glaucomatous optic nerve head changes/neuropathy and glaucomatous visual field defects on Humphrey automated perimeter (24-2 or 10-2). Children with angle anomaly, history of congenital or developmental glaucoma, trauma, and uveitis were excluded from the study.
Detailed demographic data with patient's complaints and history of steroid use were noted including drug name, duration and frequency. Ophthalmic examination included uncorrected and corrected distance visual acuity (UDVA and CDVA) using Snellen's chart, anterior segment slit lamp examination, fundus examination by slit lamp biomicroscopy, Goldman applanation tonometry, gonioscopy (in cooperative patients), and Humphrey (24-2 or 10-2) automated perimetry whenever possible.
Topical steroids which were commonly abused were classified in 3 categories depending upon their potency and IOP raising potential. Dexamethasone and betamethasone were included in high potency group (group A). Prednisolone was considered having moderate potency (group B) while loteprednol and fluorometholone were included in weak potency group (group C).[17] In some patients, exact name of the steroids/details were not known, old case registry and old eye drops were not available and further investigation to trace the drugs were unsuccessful, were included in unknown group (group D). Only on basis of history of drug use for allergy and coexisting presentation of ocular hypertension, we have presumed that it might be steroid for Group D.
Type of VKC was classified as ‘palpebral’ if papillae were predominantly on the upper tarsal conjunctiva, ‘limbal’ if papillae or gelatinous deposits were at the limbus with minimal papillae on the upper tarsus, and ‘mixed’ if both were present.[12] Vision reducing and threatening complications[18,19,20] like shield ulcer, cataractous changes, keratoconus etc., were also noted. Signs of glaucomatous disc changes in the form of increased cupping, thinning of neuroretinal rim, and retinal nerve fibre loss were examined. A glaucomatous optic neuropathy was considered when a vertical cup disc ratio of at least 0.8:1 was seen with neuroretinal rim thinning and or asymmetry of inter eye cupping greater than 0.2.[21] A cup disc ratio of 0.9 or greater was considered as severe cupping.
All the steroid medications or unknown drugs instillation were stopped and patients were managed initially conservatively with antiglaucoma medications depending on IOP, cupping and age of the patients. Protocol of treatment is depicted in the flow chart [Fig. 1]. The surgery of choice was trabeculectomy with or without adjuvant topical mitomycin-C (0.4 milligram/ml for 2 minutes). The patients with failed trabeculectomy were managed either with needling or repeat trabeculectomy with mitomycin-C. Failure of repeat filtration surgeries warranted use of Glaucoma Drainage Device (GDD). Cyclophotocoagulation was considered as the last option for uncontrolled IOP in eyes without visual prognosis.
Figure 1.
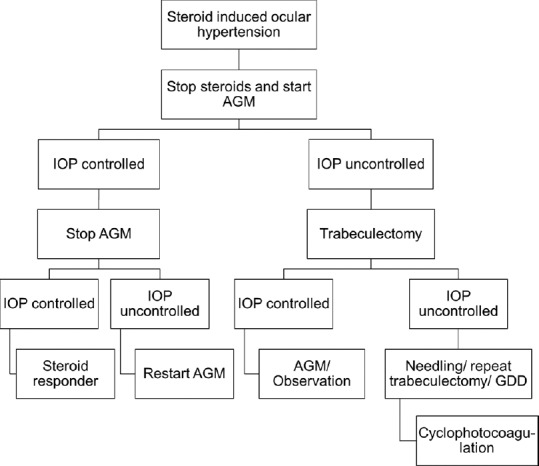
Protocol of treatment in flow chart in cases of steroid induced glaucoma
Steroid responder patients were prescribed initially mast cell stabilisers and antihistaminic eye drops after cessation of steroid drops. Topical cyclosporine (0.05%) or tacrolimus (0. 03%) was also started in those showing poor response. During each follow up visits; visual acuity, IOP, anterior segment and fundus examinations were noted. Outcome analyses of management were done and considered successful if IOP was <20 mm Hg with or without antiglaucoma medications at the last follow up.
Statistical analysis
Statistical analysis was done using IBM SPSS software version 24.0.0.0. Mean, median, standard deviation, ranges were evaluated for continuous variables while for categorical variables, frequency and percentages were recorded. Independent t-test was used to compare mean between the two groups (pre-treatment versus post treatment, right eye versus left eye). Chi square test and fisher exact test were used to compare frequency more than 5 and less than 5 respectively. One-way ANOVA test was performed to compare means between four steroid groups and post hoc Tukey HSD test was performed to find any intra group statistically significant result. P value of less than 0.05 within 95% CI was considered statistically significant.
Results
Total 1423 patients of VKC visited the hospital during the study period. Out of those, 240 patients were already using topical steroid preparations prescribed from elsewhere. We found 92 eyes of 47 patients of VKC having steroid induced ocular hypertension during the study period. About 34 patients were males while thirteen were females. Ocular hypertension was found bilateral in 45 patients and unilateral in rest 2 patients. Mean age of the patients was 14.1 ± 3.8 years [Table 1].
Table 1.
Demographic and pre management details of all patients as a single cohort
| Total patients | 47 (92 eyes) |
| Prevalence of Steroid responders/glaucoma | 19.1% |
| Male/Female | 34 (72%)/13 (28%) |
| Mean age (years±SD) | 14.1±3.8 (range 5-18) |
| Laterality (Right/Left) | 46/46 |
| Mean visual acuity (log MAR) | |
| UDVA | 0.65±0.77 |
| CDVA | 0.50±0.79 |
| Mean IOP on presentation (mm of Hg)* | 38±12 |
| Medically managed cases | 34.2±8.6 |
| Surgically managed cases | 38.9±13.8 |
| Mean vertical cupping on presentation** | 0.67±0.25 |
| Medically managed cases | 0.32±0.09 |
| Surgically managed cases | 0.81±0.17 |
| Associated anterior segment complicating conditions, n (%) Cataract Keratoconus Shield ulcer |
35 (37.2%) 6 (6.3%) 2 (2.1%) |
| No. of eyes required filtration surgery | 57 (61%) |
| No. of eyes underwent cataract surgery | 15 (16%) |
T test is used to compare IOP and cupping on presentation between medically and surgically managed cases. *P=0.12, **P<0.00001
The most frequent complaint was redness and itching in all the patients followed by burning and watering in 39 patients. About 15 patients presented with headache, nausea with or without vomiting suggestive of raised intraocular pressure. Notably only 6 patients complained of diminution of vision despite 0.50 (Snellen equivalent 6/18) ± 0.79 of mean CDVA at presentation. Most common form of VKC in our study was the mixed type (49%) followed by palpebral (32%) and limbal (19%). Associated anterior segment complicating conditions included cataract in 35 (37.2%) eyes, keratoconus in 6 (6.3%) and shield ulcer in 2 (2.1%) eyes.
Mean IOP at presentation was 38 ± 12 mm of Hg and mean vertical cup disc ratio was 0.67 ± 0.25. Total 36 (38%) eyes presented with severe cupping (>0.9). Visual field was reliably performed in 42 (44.6%) eyes; results were suggestive of glaucomatous field defects in 36 eyes and borderline in rest 6 eyes. Gonioscopy revealed open angles in all eyes.
After confirmation of diagnosis, IOP was controlled by withdrawal of steroids alone in 9 eyes. Antiglaucoma medications were able to control IOP in 27 eyes. In 57 eyes, trabeculectomy was required to control IOP. We implanted glaucoma drainage device (Ahmed glaucoma valve) in 1 patient due to inadequate IOP control even after multiple filtration surgeries. We did not require cyclophotocoagulation in any patient as glaucoma was adequately managed by one of the above treatment modalities.
We also compared patients using different steroid medications [Table 2]. The most common drugs instilled by patients were dexamethasone/betamethasone (group A-36 eyes, 38%) or some unknown medications (group D-38 eyes, 40%). Mean CDVA at presentation was better in group C (0.23 log MAR) compared to other groups. Mean IOP was highest in patients using group A drugs (43.1 mm Hg) followed by group D drugs (40.5 mm Hg). ANOVA test showed statistically significant result (P = 0.03) for this parameter and post HOC analysis showed significantly higher IOP in group A compared to group C (P = 0.04).
Table 2.
Comparison of patients according to different types of steroids use
| Parameters | Number (%) | ||||
|---|---|---|---|---|---|
| Group A | Group B | Group C | Group D | Total | |
| Type of VKC | |||||
| Limbal | 8 | 0 | 2 | 8 | 18 (19) |
| Palpebral | 12 | 0 | 4 | 14 | 30 (32) |
| Mixed | 16 | 8 | 6 | 16 | 46 (49) |
| Mean Days of usage | 795 | 570 | 420 | 634 | 639 |
| IOP Mean±SD* | 43.1±10.2 | 33.1±9.9 | 32.3±7.5 | 40.5±15.1 | 39.8±12.9 |
| IOP <30 | 3 (8) | 3 (38) | 4 (33) | 8 (21) | 26 |
| 30-40 | 7 (20) | 1 (12) | 5 (42) | 8 (21) | 15 |
| >40 | 26 (72) | 4 (50) | 3 (25) | 22 (58) | 53 |
| Mean cupping* | 0.70 | 0.65 | 0.5 | 0.69 | 0.67±0.25 |
| Advanced cupping | 16 (44) | 2 (25) | 2 (17) | 16 (42) | 36 (38) |
| Mean BCVA | 0.50 | 0.66 | 0.23 | 0.46 | 0.48 |
| Drugs | 11 (31) | 4 (50) | 8 (67) | 14 (37) | 37 (39) |
| Surgery | 25 (69) | 4 (50) | 4 (33) | 24 (63) | 57 (61) |
| Optic atrophy | 1 | 0 | 0 | 2 | 3 |
| Total number | 36 (38) | 8 (9) | 12 (13) | 38 (40) | 94 |
*ANOVA with post Hoc analysis - overall P=0.03 (group A versus C - 0.04)
Total 26 (72%) patients had IOP greater than 40 in group A which was highest among all groups. Similarly mean cupping was also noted higher in group A (0.7 cupping). Advanced cupping was seen in 16 eyes each in group A and D. Surgical treatment was required to control IOP in more eyes in group A (25 [69%]) and group D (24 [63%]) compared to others. Glaucomatous optic atrophy on presentation was found in 3 eyes (one using dexamethasone and 2 eyes using unknown steroids).
Interestingly we found that the mean UDVA (P = 0.05) and CDVA (P = 0.03) was significantly worse in left eyes and so was IOP (P = 0.02). Mean cupping was also found to be higher in left eyes (0.69) compared to right (0.65) but this was not statistically significant. Moreover, 34 left eyes required surgical approach for glaucoma as compared to 23 right eyes (P = 0.01) [Table 3].
Table 3.
Comparison of right eyes versus left eyes
| Parameters | RIGHT (n=46) | LEFT (n=46) | P |
|---|---|---|---|
| Mean UDVA | 0.52±0.59 | 0.79±0.93 | 0.05 |
| Mean CDVA | 0.34±0.55 | 0.66±0.95 | 0.03 |
| Mean IOP | 35.8±12.2 | 40.2±12.8 | 0.02 |
| Mean cupping | 6.5±2.5 | 6.9±2.5 | 0.15 |
| No. of eyes with advanced cupping | 15 (35%) | 21 (46%) | 0.28 |
| No. of eyes required surgery for glaucoma | 23 (50%) | 34 (74%) | 0.01 |
At presentation 17 patients were blind according to WHO criteria (CDVA worse than 3/60 or visual field less than 10 degrees in better eye). Post treatment marginal improvement in CDVA was found but was not statistically significant (P = 0.46). However, there was statistically significant reduction in IOP (13.8 mm Hg post treatment versus 39.8 mm Hg pre-treatment, P < 0.00001). Small reversal of cupping was also noticed (0.65 ± 0.26 post treatment versus 0.67 ± 0.25 pre-treatment, P = 0.28) [Table 4].
Table 4.
Comparison of patients before and after treatment
| Parameter | Pre-treatment (mean±SD) | Post treatment (mean±SD) | P |
|---|---|---|---|
| UDVA | 0.65±0.77 | 0.67±0.73 | 0.48 |
| CDVA | 0.50±0.79 | 0.48±0.79 | 0.46 |
| IOP | 39.8±12 | 13.8±3.9 | <0.00001 |
| CUPPING | 0.67±0.25 | 0.65±0.26 | 0.28 |
Discussion
This study highlights the visual disability caused by inadvertent use of steroids in children in Indian rural population. We studied patients of VKC with raised IOP who were using topical steroids prescribed elsewhere. These topical steroids were prescribed without counselling the parents or patients about the disease or asymptomatic complications associated with steroid use. The patients continued to use the steroids, because of the quick relief in symptoms of VKC.[22] Injudicious use of steroids and inadequate monitoring led to steroid induced complications like ocular hypertension, glaucoma and cataract affecting vision markedly.
Vision loss resulting from cataract is reversible and relatively easy to manage but glaucoma is often recognised late leaving patients with permanent visual impairment.
About 47 patients were found to have steroid induced glaucoma during the study period and majority (34 [72%]) of them were males. Greater outdoor activities in males result in greater exposure to allergens and subsequently increase the chances of VKC.[12,20,23,24] Male preponderance of approximately 3:1 has been reported in multiple studies.[18,20]
Most of the patients had reduction in CDVA due to cataract and advanced glaucoma. However, only 6 patients complained of diminished vision. Rest were unaware of poor vision perhaps due to unequal involvement of lens and visual field. Itching was present in all the patients in our study followed by redness in 40 (87%) patients. Bonini et al.[20] also noted the major complaints of patients in VKC are itching followed by redness, photophobia and mucous discharge. Saboo et al.[25] in demographic study of VKC patient found itching (88%) as the most common symptom. Relief from itching and redness is perhaps most important for children and their families, which steroids can immediately provide. Hence patients continue to use steroids and ignore minor visual disturbances. This underscores the importance of vigorous assessment of vision and IOP in children using steroids.
Similar to other studies,[12,23] we also noted that the mixed form (49%) of VKC was most commonly associated with steroid-induced glaucoma, followed by the palpebral form (32%), and least with the limbal variety (19%). This could be due to greater severity of disease in mixed VKC requiring more potent steroids for achieving remission.
Mean duration of steroid usage was 21.3 months in our study which was higher than reported in some other studies. Shikha Gupta et al.[26] and Marcus Ang et al.[12] noted 18 months and 10.4 months of mean steroid use respectively. Longer duration of steroid use is associated with more severe forms of glaucoma requiring surgery (trabeculectomy) to control IOP. This was also evidenced as 62% patients in our study required surgery compared to 45% and 16% patients in two above mentioned studies.
Most of the patients in our study were using either high potency steroids (36 [38%]) or some unknown medications (38 [40%]). Shikha Gupta et al. also found that dexamethasone drops were prescribed in majority of cases (26 of 51).[26] Dexamethasone is cheap and easily available as its maximal retail price is capped by Government of India. This was also reflected in the sale of topical steroid units for ophthalmic use in India, which was found to be almost twice that of China and 20 times that of the USA in 2014.[26]
Mean IOP (38.9 versus 34.2 mm Hg) and cupping (0.81 versus 0.32) was higher in the patients on presentation who required surgery than those managed with medications only. Our result corroborates with study done by Sihota et al.[23] In their study of 34 patients of steroid induced glaucoma, they observed mean baseline IOP in eyes requiring surgery was 49.67 mmHg and in eyes managed medically, 30.36 mmHg (P = 0.002). The vertical cup-disc ratio in surgically treated patient was 0.87 as compared to 0.71 (P = 0.012) in the medically treated group.
We divided the patients of VKC into 4 groups according to the type of steroid used. As noted earlier, majority of the patients belonged to group A and D. Patients in these groups also used steroids for greater duration of time compared to group B and C. Higher potency and greater duration of use resulted in more severe glaucoma as mean IOP and cupping was higher in group A and D. Subsequently more patients required trabeculectomy to control IOP in group A (69%) and D (63%). On the other hand, mean CDVA was found to be better in group C (0.23 log MAR) compared to others. Due to similar clinical profile between group A and D, we may conclude that many patients of group D may also have used dexamethasone or betamethasone.
One incidental finding we noted in our study was more severe involvement of left eyes in the patients. Mean CDVA (0.66 versus 0.34 log MAR) was significantly worse (P = 0.03) and IOP (40.2 versus 35.8 mm Hg) was significantly higher (P = 0.02) in left eyes. Though statistically insignificant, left eyes also had higher mean cupping and advanced cupping than right eyes. Nearly 3 out of 4 left eyes (74%) required trabeculectomy compared to 50% of right eyes (P = 0.01). No other study previously reported such difference between eyes. One hypothesis could be greater instillation of medications in left eye. Parents or patients usually instil an eye drop first in the right eye, which causes some stingy sensation. Then it becomes slightly difficult to instil eye drop in the left eye. Some spill over of medication thus may occur and to counter balance that, parents might instil medication multiple times effectively increasing the dosage in left eye. Because of the retrospective analysis of data, we were not able to confirm this hypothesis. However, some genetic or anatomical difference may be responsible in this region producing greater steroid response in left eyes.
IOP could be controlled in all patients with medical or surgical therapy by the end of the study. Slight cup reversal was seen post treatment (0.65 versus 0.67) but not statistically significant. Reversal of cupping is commonly seen in children post treatment but that does not signify neuronal recovery. Mean CDVA only marginally improved to 0.48 from 0.50 logMAR (P = 0.46) indicating permanent glaucomatous vision loss. Cyclophotocoagualtion was not required in any of the patients. At the end of 6 months, 23 of 47 patients (48.9%) were off treatment and rest required continued antiglaucoma medications.
Though our study highlights a major public health issue of children with comprehensive data collection, it has some limitations; it is a retrospective hospital based study so it may not reflect the real problem at community level. Further community based studies are warranted to know the exact prevalence and severity of disease process. In future studies, emphasis should be given to trace the unknown drugs that we classified as Group-D and to investigate the cause of more severe disease presentation in left eye.
Steroids are often only agents providing relief in severe VKC. We recommend at least fortnightly vision and IOP evaluation of children using topical steroids so as to detect steroid responders at the earliest. Weak steroids like loteprednol or fluorometholone should be used instead of higher potency drugs. Use of irrational antibiotic and steroid combinations should be discouraged for simpler ocular ailments. More stringent laws should be enforced to prevent sale of such medications without valid prescriptions. Steroid dependant or responder patients should be prescribed topical cyclosporine (0.05%) or tacrolimus (0. 03%). Non-medical measures like avoidance of possible allergen and cold compresses are equally important. There is a need to individually and collectively educate the public about topical steroids, their advantages and their adverse reactions when abused and when bought without an ophthalmologist's prescription. Electronic media including television may be used for awareness campaigns.
Conclusion
To conclude, 19% of patients using steroids without supervision developed steroid induced glaucoma. Among steroid responders, cataract developed in 37% eyes and 62% required surgery to control IOP. Glaucoma was severe as high potency steroids were used for very long duration causing permanent visual impairment. More than one third (36%) of children were blind (WHO criteria) at presentation. These children will live with visual impairment for years and there will be financial burden to treat complications. Therefore, measures need to be taken collectively by patients, ophthalmologists and the government to prevent steroid misuse.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.De Smedt S, Wildner G, Kestelyn P. Vernal keratoconjunctivitis: An update. Br J Ophthalmol. 2013;97:9–14. doi: 10.1136/bjophthalmol-2011-301376. [DOI] [PubMed] [Google Scholar]
- 2.Khan MD, Kundi N, Saeed N, Gulab A, Nazeer AF. A study of 530 cases of vernal conjunctivitis from the North West Frontier Province of Pakistan. Pak J Ophthalmol. 1986;2:111–4. [Google Scholar]
- 3.Resnikoff S, Cornand G, Filliard G, Hugard L. Limbal vernal conjunctivitis in the tropics. Rev Int Trachome. 1988;65:53–71. [PubMed] [Google Scholar]
- 4.Bangal VS, Bankar SM, Bhandari AJ, Kalkote PR. Bilateral steroid induced glaucoma in vernal keratoconjunctivitis. Int J Med Res Heath Sci. 2015;4:226–8. [Google Scholar]
- 5.Abelson MB, Schaefer K. Conjunctivitis of allergic origin: Immunologic mechanisms and current approaches to therapy [review] Surv Ophthalmol. 1993;38(Suppl):115–32. doi: 10.1016/0039-6257(93)90036-7. [DOI] [PubMed] [Google Scholar]
- 6.Bielory L, Frohman LP. Allergic and immunologic disorders of the eye. J Allergy Clin Immunol. 1992;89:1–15. doi: 10.1016/s0091-6749(05)80033-8. [DOI] [PubMed] [Google Scholar]
- 7.Allansmith MR. St. Louis: The CV Mosby Co; 1982. The Eye and Immunology; pp. 118–30. [Google Scholar]
- 8.Friedlaender MH. 2nd ed. New York: Raven Press; 1993. Allergy and Immunology of the Eye; pp. 193–6. [Google Scholar]
- 9.Vichyanond P, Pacharn P, Pleyer U, Leonardi A. Vernal keratoconjunctivitis: A severe allergic eye disease with remodeling changes. Pediatr Allergy Immunol. 2014;25:314–22. doi: 10.1111/pai.12197. [DOI] [PubMed] [Google Scholar]
- 10.Addis H, Jeng BH. Vernal keratoconjunctivitis. Clin Ophthalmol (Auckland, N.Z.) 2018;12:119–23. doi: 10.2147/OPTH.S129552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mithal S, Sood AK, Maini AK. Management of vernal conjunctivitis with steroid induced glaucoma - a comparative study. Indian J Ophthalmol. 1987;35:298–301. [PubMed] [Google Scholar]
- 12.Ang M, Ti SE, Loh R, Farzavandi S, Zhang R, Tan D, et al. Steroid-induced ocular hypertension in Asian children with severe vernal keratoconjunctivitis. Clin Ophthalmol. 2012;6:1253–8. doi: 10.2147/OPTH.S32936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Munjal VP, Dhir SP, Jain IS. Steroid induced glaucoma. Indian J Ophthalmol. 1982;30:379–82. [PubMed] [Google Scholar]
- 14.Farooq S, Malik A. Evaluation and management of steroid induced glaucoma in vernal keratoconjunctivitis patients. Pak J Ophthalmol. 2007;23:1–4. [Google Scholar]
- 15.Skuta GL, Morgan RK. Corticosteroid-induced glaucoma. In: Ritch R, Shields MB, Krupin T, editors. The Glaucoma. 2nd ed. II. St Louis: Mosby; 1996. pp. 1177–88. [Google Scholar]
- 16. [Last accessed on 2018 Nov 02]. Available from: https://www.aao.org/eyenet/article/steroid-overuse-in-india .
- 17.Cantrill HL, Palmberg PF, Zink HA, Waltman SR, Podos SM, Becker B. Comparison of in vitro potency of corticosteroids with ability to raise intraocular pressure. Am J Ophthalmol. 1975;79:1012–7. doi: 10.1016/0002-9394(75)90687-x. [DOI] [PubMed] [Google Scholar]
- 18.Leonardi A, Busca F, Motterle L, Cavarzeran F, Fregona IA, Plebani M, et al. Case series of 406 vernal keratoconjunctivitis patients: A demographic and epidemiological study. Acta Ophthalmol Scand. 2006;84:406–10. doi: 10.1111/j.1600-0420.2005.00622.x. [DOI] [PubMed] [Google Scholar]
- 19.Tabbara KF. Ocular complications of vernal keratoconjunctivitis. Can J Ophthalmol. 1999;34:88–92. [PubMed] [Google Scholar]
- 20.Bonini S, Bonini S, Lambiase A, Marchi S, Pasqualetti P, Zuccaro O, et al. Vernal keratoconjunctivitis revisited: A case series of 195 patients with long-term follow up. Ophthalmology. 2000;107:1157–63. doi: 10.1016/s0161-6420(00)00092-0. [DOI] [PubMed] [Google Scholar]
- 21. [Last accessed on 2018 Dec 20]. Available from: https://www.reviewofophthalmology.com/article/how-to-evaluate-the-suspicious-optic-disc .
- 22.Phulke S, Kaushik S, Kaur S, Pandav SS. Steroid-induced glaucoma: An avoidable irreversible blindness. J Curr Glaucoma Pract. 2017;11:67–72. doi: 10.5005/jp-journals-l0028-1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sihota R, Sood NN, Agarwal HC. Juvenile secondary glaucomas. J Glaucoma. 1993;15:80–4. [Google Scholar]
- 24.Kaur S, Dhiman I, Kaushik S, Raj S, Pandav SS. Outcome of ocular steroid hypertensive response in children. J Glaucoma. 2016;25:343–7. doi: 10.1097/IJG.0000000000000209. [DOI] [PubMed] [Google Scholar]
- 25.Saboo US, Jain M, Reddy JC, Sangwan VS. Demographic and clinical profile of vernal keratoconjunctivitis at a tertiary eye care centre in India. Indian J Ophthalmol. 2013;61:486–9. doi: 10.4103/0301-4738.119431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gupta S, Shah P, Grewal S, Chaurasia AK, Gupta V. Steroid-induced glaucoma and childhood blindness. Br J Ophthalmol. 2015;99:1454–6. doi: 10.1136/bjophthalmol-2014-306557. [DOI] [PubMed] [Google Scholar]


