Abstract
Femtosecond laser-assisted cataract surgery was performed in a patient with high myopia, who had undergone posterior chamber phakic intraocular lens surgery (Implantable Collamer Lens, ICL). During docking the machine erroneously focused the laser on the anterior surface of ICL and laser for lens fragmentation was also defocused, which were correctly positioned before laser delivery. During laser application for capsulotomy, air bubbles were entrapped under the ICL prohibiting lens fragmentation. One must be careful during focusing the laser in eyes with ICL. Additionally, gas bubbles under the ICL may lead to difficulties in completion of nuclear disassembly.
Keywords: Cataract surgery, femtosecond laser, phakic intraocular lens
Femtosecond laser-assisted cataract surgery (FLACS) has been shown to improve safety and efficacy of phacoemulsification and latest iterations in FLACS technology are improving results.[1,2] FLACS is especially useful in challenging scenarios when capsulorhexis and nuclear disassembly is anticipated to be difficult. We report the challenges and outcomes from a case where FLACS was employed to assist phacoemulsification in an eye with high myopia previously implanted with a posterior chamber phakic intraocular lens.
Case Report
A 32-year-old man presented with progressively decreased vision in his right eye for the past 2 years. He was a known case of high myopia and had undergone implantation of a posterior chamber phakic intraocular lens (The Visian® ICL, STAAR Surgical Company, CA, USA) elsewhere 4 years back. On examination, the right eye had a corrected distance visual acuity (CDVA) of 6/18 in Snellen's chart and the left eye had a CDVA of 6/6. Slit lamp examination of both eyes showed the ICL in situ with a patent peripheral iridotomy and normal intraocular pressure. The ICL were not in contact with the lens in both eyes with a normal appearing lens vault. The right eye had nuclear cataract [Fig. 1] and the left eye had a clear lens. The dilated fundus evaluation of both eyes was unremarkable. The biometric evaluation of both eyes is shown in Table 1.
Figure 1.
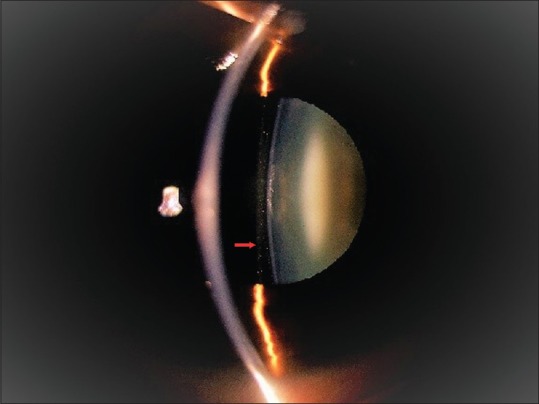
Slit lamp image of right eye showing ICL in situ (arrow) with nuclear cataract
Table 1.
Biometry of both eyes
| Right Eye | Left Eye | |
|---|---|---|
| Axial length | 31.24 mm | 28.30 mm |
| ACD | 2.64 mm | 2.69 mm |
| Lens thickness | 4.74 mm | 4.54 mm |
| K1 | 42.76 D @94 degree | 42.49 D @ 95 degree |
| K2 | 43.80 D @ 4 degree | 43.67 D @ 5 degree |
| Astigmatism | +1.04 D @ 4 degree (ATR) | Astigmatism: +1.18 D @ 5 degree (ATR) |
| IOL Power (SRK/T) | +0.00 D | +7.50 D |
Key: ACD=Anterior chamber depth, K=Keratometry, ATR=Against the Rule
The right eye was taken up for FLACS (Alcon LenSx, Inc., Aliso Viejo, CA, USA) after patient consent. During docking for capsulotomy, we reduced the capsulotomy treatment height (delta up) to 250 microns from the anterior lens capsule as opposed to manufacturer recommendation of 300 microns to avoid excessive laser firing on the undersurface of ICL. We aimed for a 2.8-mm three-planar primary corneal incision, capsulotomy of 4.9 mm, a lens chop diameter of 5.1 mm and lens fragmentation pattern of two chops and three cylinders. However, during docking the machine initially focused the laser on the anterior surface of ICL instead of focusing on anterior lens capsule. Similarly, laser for lens fragmentation was also defocused and shifted superiorly [Fig. 2a]. This was noted before laser delivery and correctly positioned on the anterior lens capsule and center of the lens [Fig. 2b]. However, during femto laser application for capsulotomy, air bubbles were found to be entrapped under the ICL [Fig. 2c] prohibiting lens fragmentation. During phacoemulsification, the ICL was explanted carefully via the temporal corneal tunnel. Close inspection of the undersurface of the ICL showed damage corresponding to the laser application [Fig. 3a]. The capsulotomy was found to be free floating [Fig. 3b] and was removed following which routine phacoemulsification was completed using a direct chop technique with implantation of a three-piece hydrophobic foldable IOL (Sensor AR40M; AMO) in the bag [Fig. 3c and d]. Patient regained uncorrected distant vision of 20/20 at 1 month post cataract surgery.
Figure 2.
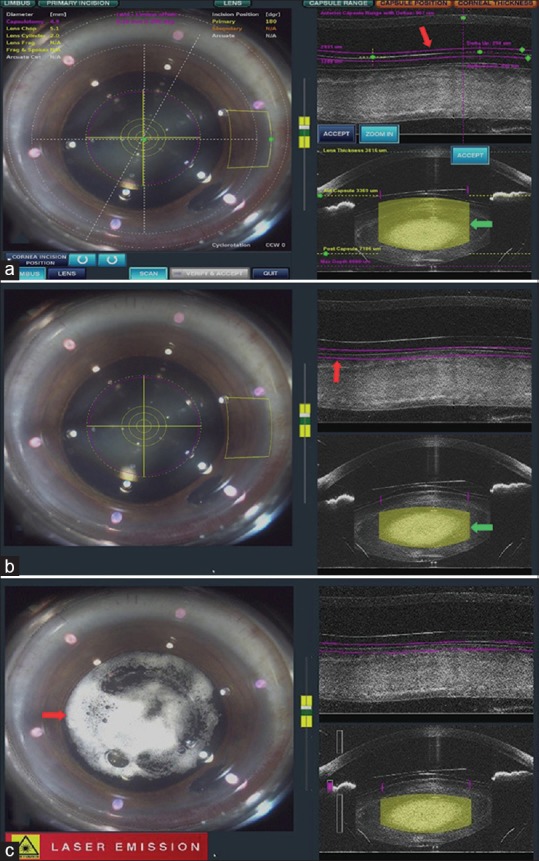
Docking images. (a) Defocused laser beam for capsulotomy (red arrow) and lens fragmentation (blue arrow). (b) Laser focused on anterior lens capsule (red arrow) and lens substance (blue arrow). (c) Docking image showing entrapment of cavitation bubbles (arrow) under the ICL
Figure 3.
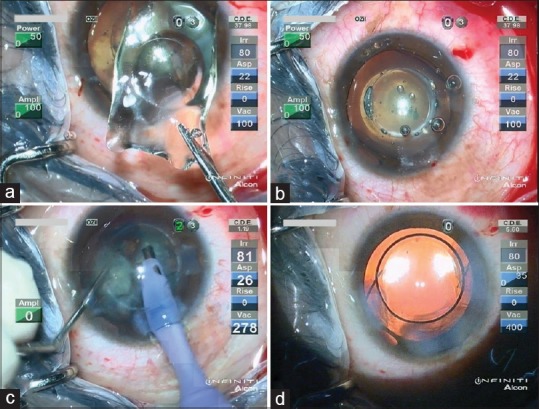
Intraoperative images: (a) Undersurface of the ICL showing damage (arrow) corresponding to the laser application. (b) Free floating capsulotomy (arrow). (c) Phacoemulsification using direct chop technique. (d) Three-piece hydrophobic foldable IOL in the bag
Discussion
We attempted to utilize FLACS for an eye with high myopia with an ICL in situ and found it difficult to perform nuclear fragmentation due to accumulation of bubbles below the ICL. Capsulotomy was found to be free floating but the undersurface of the ICL showed damage inflicted by the femtosecond laser.
In an eye with ICL, there is a moderately high likelihood of errors in the laser beam focus position due to the refractive index of the optical material as well as the refractive power of the ICL as seen in our case. Hence, one must be very careful during the focusing of laser during docking. Another concern is formation of gas bubbles under the ICL which get trapped and lead to difficulties in completion of nuclear disassembly as seen in our case. Several modifications have been suggested to overcome this such as altering the capsulotomy tissue height and increasing vertical spot spacing to reduce bubble formation.[3] Additionally, to avoid complications due to laser focus displacement it is recommended that the safety margin from the anterior and posterior capsule be increased to 1000 microns.[3]
Several authors have described the use of FLACS in eyes with anterior and posterior chamber ICLs.[3,4,5,6,7,8] Anisimova et al. reported bubbles similar to ours which lead to incomplete capsulotomy but did not interfere with nuclear fragmentation.[4] Similarly, Kaur et al. reported incomplete nucleotomy due to bubble entrapment.[5] Diakonis et al. described important modifications in laser settings to improve results in these difficult surgical scenarios.[3] Our case report suggests that docking-related complications are not uncommon in a patient of FLACS with ICL and one should be prepared to deal with the challenges.
In conclusion, entrapment of bubbles below ICL is not unusual following femtosecond capsulotomy. Patients must be informed about this possibility and need for regular ultrasound assisted nuclear disassembly.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Donaldson KE, Braga-Mele R, Cabot F, Davidson R, Dhaliwal DK, Hamilton R, et al. Femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2013;39:1753–63. doi: 10.1016/j.jcrs.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 2.Alio JL, Soria F, Abdou AA. Femtosecond laser assisted cataract surgery followed by coaxial phacoemulsification or microincisional cataract surgery: Differences and advantages. Curr Opin Ophthalmol. 2014;25:81–8. doi: 10.1097/ICU.0000000000000017. [DOI] [PubMed] [Google Scholar]
- 3.Diakonis VF, Yoo SH, Kontadakis GA, El Danasoury AM, Donaldson KE, Culbertson WW. Femtosecond laser-assisted cataract surgery in a patient with posterior chamber phakic intraocular lens. Am J Ophthalmol Case Rep. 2016;1:11–2. doi: 10.1016/j.ajoc.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anisimova N, Malyugin B, Arbisser LB, Sobolev N. Femtosecond laser-assisted cataract surgery in vitrectomized eye with posterior chamber phakic intraocular lens. Digit J Ophthalmol. 2017;23:43–4. doi: 10.5693/djo.02.2017.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaur M, Sahu S, Sharma N, Titiyal JS. Femtosecond laser-assisted cataract surgery in phakic intraocular lens with cataract. J Refract Surg. 2016;32:131–4. doi: 10.3928/1081597X-20160106-01. [DOI] [PubMed] [Google Scholar]
- 6.Kohnen T, Steinwender G. Femtosecond laser-assisted cataract surgery in eyes with foldable anterior or posterior chamber phakic intraocular lenses. J Cataract Refract Surg. 2018;44:124–8. doi: 10.1016/j.jcrs.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 7.Lee CY, Chao SC, Sun CC, Lin HY. Femtosecond laser-assisted cataract surgery in patients with phakic intraocular lenses and low endothelial cell counts: A case report. BMC Ophthalmol. 2017;17:180. doi: 10.1186/s12886-017-0568-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li S, Chen X, Kang Y, Han N. Femtosecond laser-assisted cataract surgery in a cataractous eye with implantable collamer lens in situ. J Refract Surg. 2016;32:270–2. doi: 10.3928/1081597X-20160217-03. [DOI] [PubMed] [Google Scholar]


