Abstract
Background/Aims
Fecal incontinence (FI) is a common complaint that increases in prevalence with age. Our aim was to determine the prevalence of FI and assess its severity by self-report in a male-predominant Veteran outpatient clinic setting.
Methods
An anonymous 28 item questionnaire was administered to a convenience sample of veterans awaiting appointments. FI was defined as a loss of liquid or solid stool at least monthly. Multivariable logistic and linear models were used to identify predictors of FI prevalence and severity.
Results
One hundred thirty-three gastroenterology (GI) participants and 126 primary care (PC) participants completed the survey. Ninety-four of 259 participants (36.3%, 95% confidence interval [CI]: 30.4–42.5) reported an episode of FI (41.4% GI participants vs 31.0% PC participants; P = 0.078) with 33.6% having FI within the last 30 days (36.8% GI participants vs 30.2% PC participants; P = 0.122). Participants with more bowel movements per week (P = 0.005) and per day (P < 0.001) and with a higher Bristol Stool Scale form (P = 0.010) were more likely to have FI. Of participants with FI, mean Fecal Incontinence Severity Index score was 23.0 ± 9.5 with a significantly higher symptom score in GI participants compared to PC participants (25.2 ± 10.0 vs 20.1 ± 8.2; P = 0.011). Few participants had ever been asked by (35.0%) or evaluated by (18.0%) a doctor for FI symptoms.
Conclusions
FI is a common complaint and under-recognized problem in the male-dominant Veteran population. Despite its prevalence, relatively few participants were asked about FI, with even less being treated. Due to the possible effects and implications on quality of life, more should be done to recognize this condition and arrange treatment.
Keywords: Fecal incontinence, Prevalence, Veterans
Introduction
Fecal incontinence (FI) is a common complaint with serious implications for quality of life. Whitehead et al1 and Ditah et al2 reported that the prevalence of FI in non-institutionalized United States adults to be 8.0%. Alsheik et al found the prevalence to be 12.0% among patients visiting an outpatient gastroenterology clinic.3 FI affects both men and women, and increases in prevalence with age. The average of onset is 49 years of age, with prevalence rates of up to 16.0% for older adults (70 years or older) and as high as 47.0% for patients living in nursing homes.1,2–4
Historically, FI was thought to be more prevalent in women than in men.5–13 For example, Nelson et al14 reported an adjusted odds ratio (OR) of 1.51 (95% confidence interval [CI], 1.10–2.11) for FI in women vs men. However, other studies have suggested that the prevalence of FI may be similar between men and women.1,2,15–17 Both O’Keefe et al16 (8.1% male vs 7.9% female) and Drossman et al15 (7.9% male vs 7.7% female) found a similar prevalence in men compared to women. Data from the National Health and Nutrition Evaluation Survey (NHANES) found a non-significant higher prevalence of FI in women (8.9%) compared to men (7.7%). In evaluating the NHANES data from 2005 to 2010, Ditah et al2 found that women had higher rates of FI only when they had urinary incontinence.2 Conversely, the largest study of community-dwelling Americans demonstrated male gender as significant risk factor for having FI within the last 7 days (OR, 1.23; 95% CI, 1,07–1.41).18
To date, there has been only one study on FI prevalence in men and this was assessing the impact of prostate cancer. There have been no studies screening for the prevalence or frequency of FI in a predominantly male or Veteran population. We hypothesized that FI is a prevalent complaint among Veterans. Therefore, the aim of the study was to determine the prevalence of FI and assess its severity by self-report in a male-predominant Veteran outpatient clinic setting.
Materials and Methods
Study Participants and Recruitment
This survey study was conducted at the Ann Arbor Veterans Affairs (VA) gastroenterology (GI) and primary care (PC) outpatient clinics. With investigational review board approval (VA IRB project 002 10/2017–10/202018), a convenience sample of patients with scheduled appointments were invited to participate in the study upon appointment check-in. Participants aged 18–85 were eligible for participation. Exclusion criteria included the following: participants who were unable to understand or provide written informed consent or unable to read or understand questionnaire. An informational letter was provided to those interested in learning more about the study, and an anonymous questionnaire was given to those willing to participate.
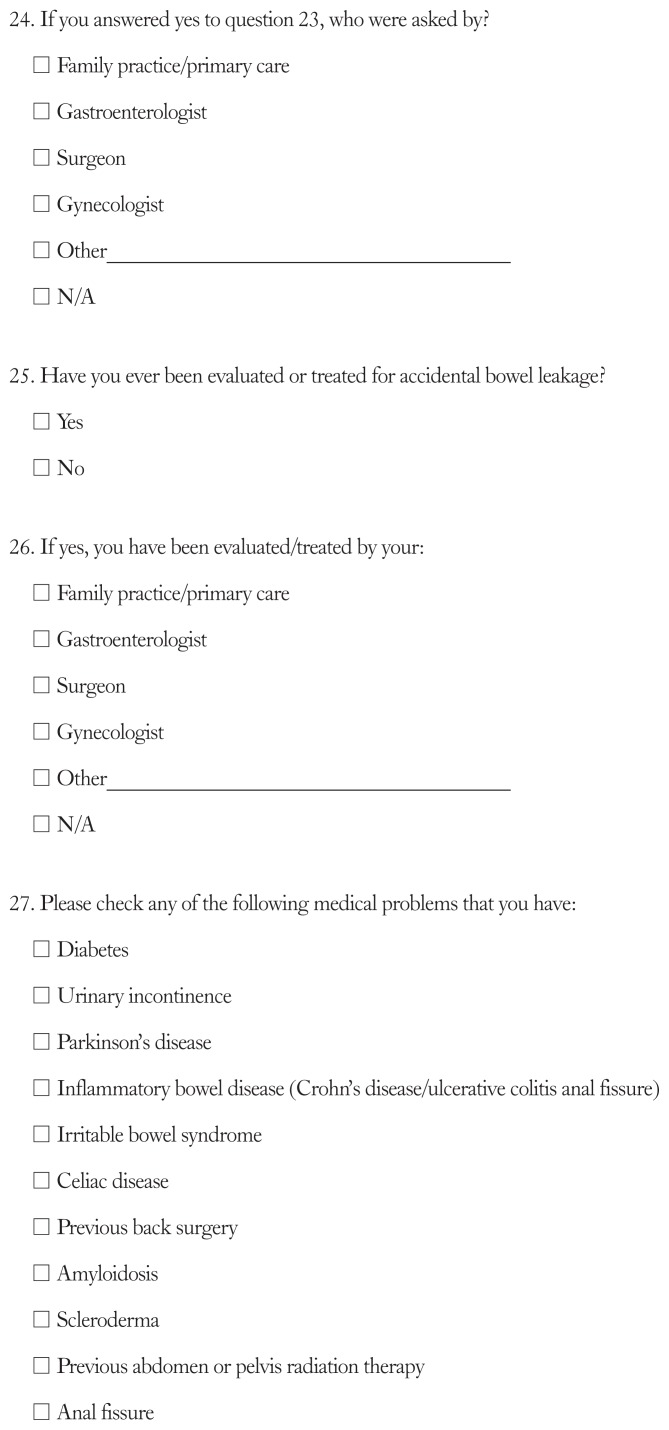
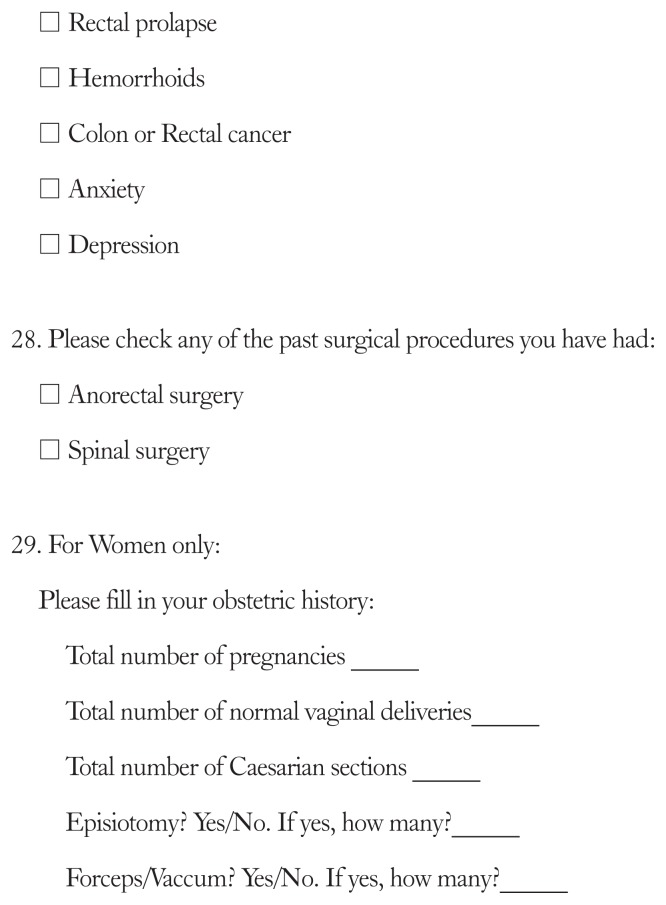
Survey Instrument
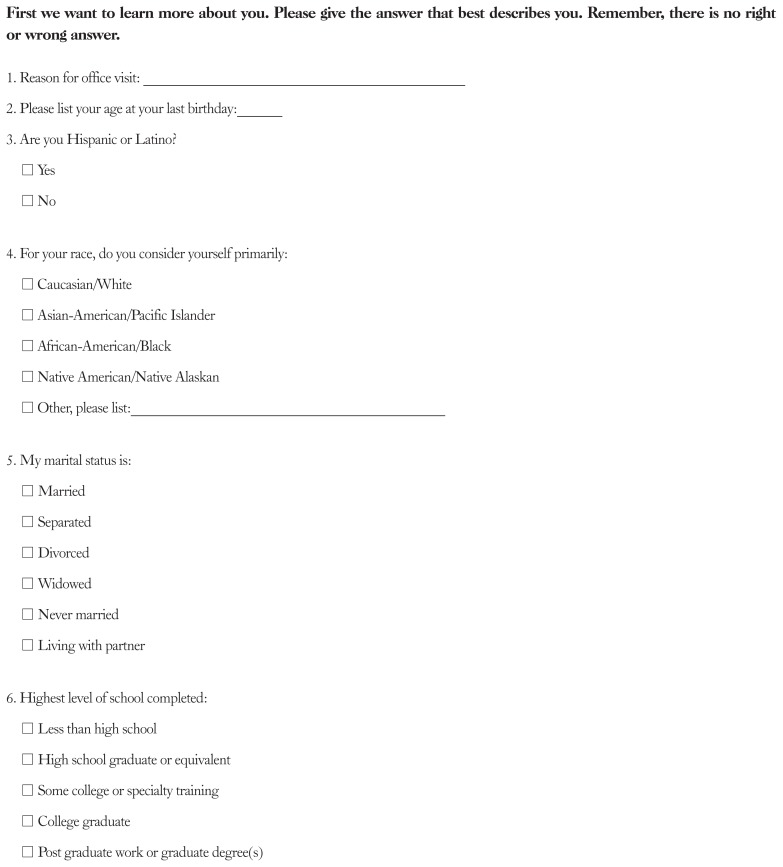
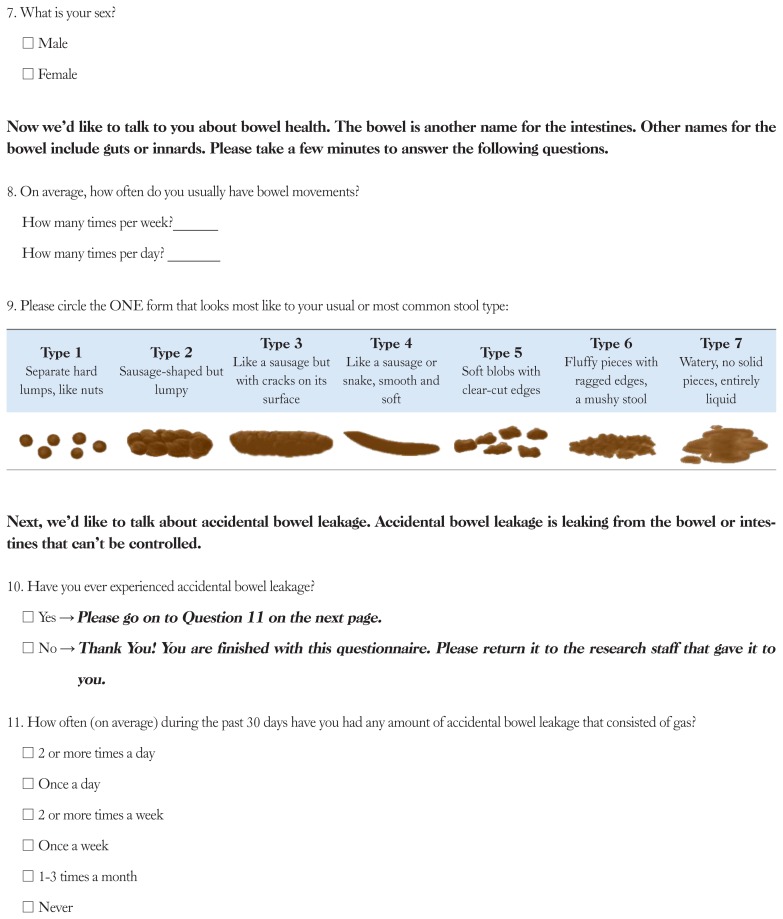
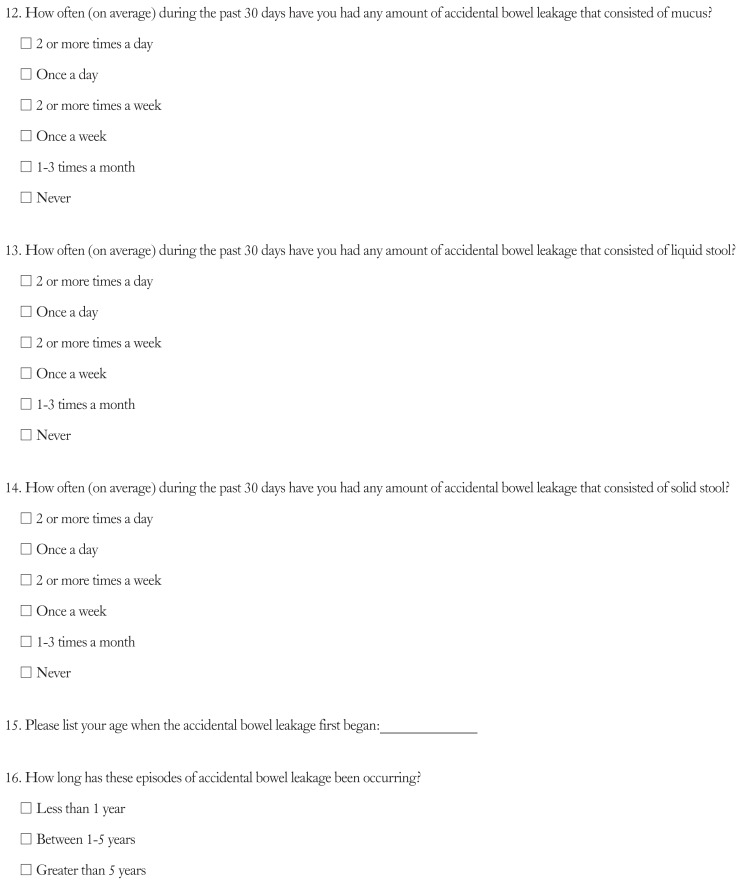
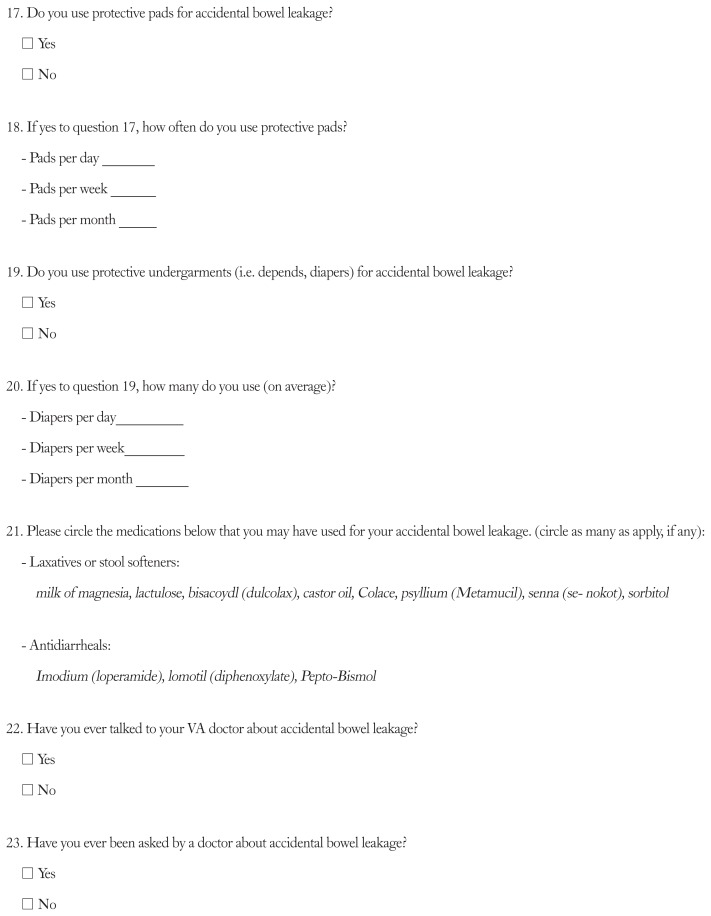
The questionnaire contained 28 items. All participants filled out the first 10 questions that assessed the following: baseline demographics, baseline bowel habits, including frequency and stool consistency by the Bristol stool form scale (BFSF) and history of FI.19 FI was defined as an involuntary loss of liquid or solid stool at least monthly. Similar wording to the NHANES 2009–2010 Bowel Health survey was utilized in this questionnaire.20 To those who answered yes to “Have you ever experienced accidental bowel leakage?” participants responded to an additional 18 questions. Using the validated Fecal Incontinence Severity Index (FISI) both type (gas, mucus, liquid, and solid stool) and severity of symptoms were assessed.21 The FISI measures the severity of FI based on the self-reported frequency of FI symptoms. Additional questions included the willingness to discuss accidental bowel leakage with medical providers, prior evaluation and/or treatment of FI, as well as medical comorbidities (Appendix).
Statistical Methods
Our planned sample size for each clinic was based on the formula by Kish, using an alpha of 0.05 with a 95.0% power to detect a prevalence of 8.0% based on prior studies.1,2,22 Using this formula, the sample size for this study was 113 study participants per clinic. We planned for a 20.0% incomplete survey rate and had allowed for the possibility of recruiting up to 136 subjects from each outpatient setting (total of 272 participants).
Descriptive statistics were calculated for patient characteristics by clinic type and by the presence of leakage. Our primary outcome was the prevalence of FI as defined by liquid or solid stool incontinence within the last 30 days. This was determined by an affirmative answer to the following question “Have you ever experienced accidental bowel leakage” and an affirmative answer to either of the following questions, “How often (on average) during the past 30 days have you had any amount of accidental bowel leakage that consisted of liquid stool” or “How often (on average) during the past 30 days have you had any amount of accidental bowel leakage that consisted of solid stool?” Frequency and type of leakage as well as the FISI was calculated per clinic type. FISI scores > 30 predict a detrimental effect on quality of life.23 Bivariate analyses utilizing chi-square test for categorical variables and the student’s t test for continuous variables were performed to examine associations between patient characteristics and FI prevalence of and symptom severity. Additionally, in subjects who had FI, bivariate analysis to assess associations between patient characteristics by clinic type and symptom severity was performed. Multivariable logistic and linear regression models were used for binary and continuous outcomes, respectively. P-values less than 0.05 were considered significant with the results presented as OR with 95% CI.
Results
A total of 272 participants were approached while awaiting their GI and PC appointments. Overall, 133 participants from GI clinic and 126 participants from PC clinic completed the survey for a 95.2% response rate including the 5 questionnaires that were not completed in entirety and excluded from analysis. The average age in years of the respondents was 59.3 ± 13.9 years old. The population was predominantly male (87.3%) and Caucasian (86.3%). GI participants were more likely to have more bowel movements per week and per day with a mean higher BSFS and loose stool consistency (BSFS type 5, 6, and 7) as compared to PC participants. Further study population characteristics are listed in Table 1.
Table 1.
Overall Study Participant Characteristics by Clinic Visit
| Characteristics | Total (N = 259) | GI participants (n = 133) | PC participants (n = 126) | P-value |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age (yr) | 59.3 ± 13.9 | 57.2 ± 14.4 | 61.6 ± 14.6 | 0.220 |
| Sex (male) | 226 (87.3) | 112 (84.2) | 114 (90.5) | 0.130 |
| White | 220 (86.3) | 110 (82.7) | 110 (87.3) | 0.520 |
| Married/partner | 145 (56.0) | 67 (50.3) | 78 (61.9) | 0.060 |
| ≤ High school education | 75 (16.5) | 35 (26.5) | 38 (30.2) | 0.510 |
| Bowel related measures | ||||
| BMs per week | 13.0 ± 13.4 | 15.1 ± 15.7 | 10.7 ± 10.1 | 0.001 |
| BMs per day | 2.0 ± 1.9 | 2.3 ± 2.3 | 1.8 ± 1.5 | 0.030 |
| BSFS | 4.3 ± 1.5 | 4.6 ± 1.5 | 4.0 ± 1.5 | 0.001 |
| BSFS type 5, 6, and 7 | 103 (39.8) | 65 (48.9) | 38 (30.2) | 0.002 |
| Episode of ABL | 94 (36.3) | 55 (41.4) | 39 (31.0) | 0.080 |
GI, gastroenterolgy; PC, primary care; BM, bowel movement; BSFS, Bristol stool form scale; ABL, accidental bowel movement.
Data are presented as n (%) or mean ± SD.
Of the participants, 36.3% (94/259, 95% CI, 30.4–42.5) reported “ever” having an episode of accidental bowel leakage (41.4% GI [55/133] and 31.0% [39/126] PC participants; P = 0.078) (Table 1). Subjects with more bowel movements per week (P = 0.005) and per day (P < 0.001) and with a higher BSFS (P = 0.010) and loose stool consistency (BSFS type 5, 6, and 7; P = 0.002) were more likely to have “ever” had an episode of accidental bowel leakage (Table 2). No demographic factors were associated with a higher likelihood of FI. When controlling for age and clinic type, only the increased number of bowel movements per day remained significant (P = 0.022) (Table 3).
Table 2.
Overall Study Participant Characteristics by Accidental Bowel Leakage (N = 259)
| Characteristics | No ABL (n = 165) | ABL (n = 94) | P-value |
|---|---|---|---|
| Demographic characteristics | |||
| Age (yr) | 59.4 ± 14.7 | 59.1 ± 12.6 | 0.825 |
| Sex (male) | 146 (88.5) | 80 (85.1) | 0.452 |
| White | 144 (87.8) | 76 (84.4) | 0.521 |
| Married/partner | 93 (56.4) | 52 (55.3) | 0.878 |
| ≤ High school education | 43 (26.2) | 30 (31.9) | 0.327 |
| Bowel related measures | |||
| BMs per week | 11.2 ± 10.2 | 16.0 ± 17.3 | 0.005 |
| BMs per day | 1.7 ± 1.4 | 2.6 ± 2.5 | < 0.01 |
| BSFS | 4.1 ± 1.5 | 4.6 ± 1.5 | 0.010 |
| BSFS type 5, 6, and 7 | 54 (31.4) | 49 (52.1) | 0.002 |
ABL, accidental bowel movement; BM, bowel movement; BSFS, Bristol stool form scale.
Data are presented as n (%) or mean ± SD.
Table 3.
Multivariable Logistic Regression Estimates of Predictors of Having Experienced Fecal Incontinence
| Characteristics | Experienced FI | P-value |
|---|---|---|
| Age | 1.00 (0.98–1.02) | 0.414 |
| GI clinic | 1.52 (0.87–2.65) | 0.132 |
| BMs per day | 2.41 (1.38–4.19) | 0.001 |
| BMs per week | 1.02 (1.00–1.04) | 0.010 |
| BSFS type 5, 6, and 7 | 1.79 (0.98–3.26) | 0.051 |
FI, fecal incontinence; GI, gastroenterology; BM, bowel movement; OR, odds ratio; CI, confidence interval.
Data are presented as OR (95% CI).
Participants With Leakage
Eighty-seven of 259 (33.6%) of all participants reported having FI (either solid and/or liquid stool) within the last 30 days, 36.8% (49/133) GI and 30.2% (38/126) PC participants (P = 0.120). Participant characteristics by clinic type are listed in Table 4. In both populations, there was a high prevalence of depression and anxiety. Participants by clinic type were similar except in following areas. PC participants were more likely to report back pain (P < 0.001) and GI subjects were more likely to have inflammatory bowel disease (IBD) (P = 0.021) or a history of anal fissure (P = 0.013). Gas incontinence was the most common type of leakage reported as shown in Table 5. Thirty-two of 49 (65.3%) and 25/38 (65.7%) of GI and PC participants also reported gas leakage at least once or more a week, respectively. Liquid stool incontinence occurred at least weekly in 47.1% (n = 41/87) of participants, with a slight predominance in GI participants (26/49, 53.1%) as compared to PC participants (15/38, 39.4%). Loss of mucus at least once per week or greater (31.0%, n = 27) was reported less frequently than liquid stool loss but similarly in both clinic populations (17/49 [34.6%] in GP participants vs 10/38 [26.4%] in PC participant; P = 0.094). Solid stool incontinence happened the least in our cohort, with 11.5% (n = 10) of subjects reporting stool loss at least once per week or greater and mainly found in the GI clinic population.
Table 4.
Participant Characteristics With Fecal Incontinence in Last 30 Days by Clinic Type
| Characteristics | GI participants (n = 49) | PC participants (n = 38) | P-value |
|---|---|---|---|
| Demographic characteristics | |||
| Age (yr) | 59.0 ± 10.2 | 58.8 ± 14.7 | 0.924 |
| Sex (male) | 41 (83.7) | 34 (89.7) | 0.282 |
| White | 40 (85.1) | 30 (81.6) | 0.522 |
| Married/partner | 26 (53.1) | 24 (60.5) | 0.498 |
| ≤ High school education | 13 (26.5) | 14 (34.2) | 0.444 |
| Comorbid conditions | |||
| Urinary incontinence | 7 (14.3) | 8 (21.6) | 0.375 |
| Diabetes mellitus | 12 (26.1) | 13 (35.1) | 0.372 |
| Irritable bowel syndrome | 12 (25.5) | 8 (21.6) | 0.683 |
| Inflammatory bowel disease | 6 (13.0) | 0 (0) | 0.022 |
| Previous back injury | 19 (41.3) | 4 (10.8) | < 0.001 |
| Anal fissure | 7 (15.2) | 0 (0) | 0.011 |
| Depression | 23 (50.0) | 20 (54.1) | 0.944 |
| Anxiety | 18 (38.3) | 20 (54.1) | 0.152 |
| Bowel related measures | |||
| BMs per week | 17.1 ± 19.7 | 14.4 ± 14.9 | 0.444 |
| BMs per day | 2.8 ± 2.9 | 2.4 ± 2.2 | 0.478 |
| BSFS | 4.8 ± 1.5 | 4.3 ± 1.6 | 0.092 |
| BSFS type 5,6, and 7 | 29 (59.2) | 17 (44.7) | 0.182 |
| FISI | 25.2 ± 10.0 | 20.1 ± 8.2 | 0.011 |
GI, gastroenterology; PC, primary care; BM, bowel movement; BSFS, Bristol stool form scale; FISI, Fecal Incontinence Severity Index.
Data are presented as n (%) or mean ± SD.
Table 5.
Fecal Incontinence Severity Index in Last 30 Days by Clinic Type
| FI type | GI participants (n = 49) | PC participants (n = 38) | P-value |
|---|---|---|---|
| Gas | |||
| ≥ 1/day | 17 (34.7) | 10 (26.3) | |
| 2–6/wk | 9 (18.4) | 8 (21.0) | 0.892 |
| 1/wk | 6 (12.2) | 7 (18.4) | |
| 1–3/mo | 12 (24.5) | 9 (23.7) | |
| Never | 5 (10.2) | 4 (10.5) | |
| Mucus | |||
| ≥ 1/day | 7 (14.3) | 2 (5.3) | |
| 2–6/wk | 8 (16.3) | 3 (7.9) | 0.093 |
| 1/wk | 2 (4.1) | 5 (13.2) | |
| 1–3/mo | 13 (26.5) | 5 (13.2) | |
| Never | 19 (38.8) | 23 (60.4) | |
| Liquid stool | |||
| ≥ 1/day | 9 (18.4) | 5 (13.2) | |
| 2–6/wk | 8 (16.3) | 2 (5.3) | 0.314 |
| 1/wk | 9 (18.4) | 8 (21.1) | |
| 1–3/mo | 19 (38.8) | 22 (57.9) | |
| Never | 4 (8.2) | 1 (2.6) | |
| Solid stool | |||
| ≥ 1/day | 2 (4.1) | 1 (2.6) | |
| 2–6/wk | 2 (4.1) | 0 (0) | 0.122 |
| 1/wk | 5 (10.2) | 0 (0) | |
| 1–3/mo | 9 (18.4) | 4 (10.3) | |
| Never | 31 (63.3) | 33 (86.8) | |
GI, gastroenterology; PC, primary care; FI, fecal incotinence.
Data are presented as n (%).
In those subjects with FI, we found that participants had a mean onset of symptoms at age 53 with 71.3% having symptoms for greater than 1 year (Table 6). The mean FISI score was 23.0 ± 9.5 with a significantly higher symptom score in GI participants compared to PC participants (25.2 ± 10.0 vs 20.1 ± 8.2, P = 0.011) (Table 4). Fifteen GI participants (30.6%) reported a FISI greater than 30 compared to 4 PC participants (10.5%) (P = 0.024). On bivariate analysis of symptom severity, number of bowel movements per week, and the presence of IBD predicted increased symptom severity. On multivariable linear regression analysis, only the presence of IBD was associated with increasing FI severity (P = 0.031) (Table 7).
Table 6.
Details About Fecal Incontinence in Last 30 Days by Clinic Type
| Characteristic | GI participants (n = 49) | PC participants (n = 38) | P-value |
|---|---|---|---|
| Age of onset (yr) | 53.4 ± 15.3 | 53.9 ± 17.2 | 0.883 |
| Duration of FI in years | |||
| < 1 yr | 15 (30.6) | 10 (26.3) | 0.512 |
| 1–5 yr | 19 (38.8) | 20 (52.6) | |
| > 5 yr | 15 (30.6) | 8 (21.1) | |
| Use of protective pads | 16 (32.7) | 9 (23.7) | 0.522 |
| Per day | 1.3 ± 1.0 | 0.8 ± 0.8 | 0.134 |
| Per week | 8.7 ± 6.2 | 5.0 ± 4.5 | 0.181 |
| Per month | 31.4 ± 23.6 | 19.3 ± 13.4 | 0.220 |
| Use of protective undergarments | 11 (22.4) | 6 (15.8) | 0.573 |
| Per day | 0.9 ± 1.0 | 1.3 ± 1.0 | 0.432 |
| Per week | 5.8 ± 7.2 | 7.2 ± 7.2 | 0.711 |
| Per month | 24.6 ± 29.6 | 28.5 ± 27.7 | 0.792 |
| Ever asked by doctor | 21 (42.9) | 10 (26.3) | 0.214 |
| Evaluated by doctor | 12 (24.5) | 4 (10.5) | 0.129 |
GI, gastroenterology; PC, primary care; FI, fecal incontinence.
Data are presented as mean ± SD or n (%).
Table 7.
Factors Associated With Fecal Incontinence Severity by Multivariable Linear Regression
| Model | |||
|---|---|---|---|
|
| |||
| Variable | Parameter estimate | Standard error | P-value |
| Age (yr) | 0.07 | 0.11 | 0.526 |
| Sex | |||
| Female | reference | --- | --- |
| Male | −4.38 | 3.23 | 0.182 |
| History of urinary incontinence | |||
| No | reference | --- | --- |
| Yes | −1.57 | 2.78 | 0.568 |
| History of diabetes mellitus | |||
| No | reference | --- | --- |
| Yes | −0.15 | 2.61 | 0.951 |
| History of anxiety | |||
| No | reference | --- | --- |
| Yes | 1.29 | 2.52 | 0.614 |
| History of depression | |||
| No | reference | --- | --- |
| Yes | −1.84 | 2.46 | 0.448 |
| History of irritable bowel syndrome | |||
| No | reference | --- | --- |
| Yes | 3.99 | 2.57 | 0.118 |
| History of inflammatory bowel disease | |||
| No | reference | --- | --- |
| Yes | 9.16 | 4.23 | 0.031 |
| Bowel movements per week | 0.19 | 0.21 | 0.362 |
At the clinic visit, none of the subjects listed any symptom consistent with FI as their reason for visit. Few participants had ever been asked by (31/87, 35.6%) or evaluated by a doctor (16/87, 18.4%) for their FI symptoms (Table 6). Gastroenterologists were involved in assessing symptoms in 68.2% of cases (45.5% asked by GI alone), whereas primary care physicians asked in 36.4% of cases.
Discussion
FI is a common complaint among Veterans in this cross-sectional survey of GI and PC participants. More than one-third of our population had FI at least monthly. Stool consistency (higher BSFS) and frequency of bowel movements were significant factors associated with FI prevalence. Additionally, few participants were asked or treated for their leakage symptoms. Our study is unique as it assesses prevalence in a predominantly male population and is the first to assess FI in Veterans. Adolfsson et al24 assessed the prevalence of urinary and bowel symptoms in population-based groups of men with and without prostate cancer. The authors found that the risk of bowel urgency and FI was 1.3–4.5 times that of the controls with a prevalence of FI of 4.0%.24 Lastly, Cohan et al25 characterized 144 men with FI to 897 women who presented to a tertiary medical center and found that men were slightly younger and more likely than women to present with coexistent constipation and less sphincter dysfunction.
One third of participants (36.8% of GI and 30.2% of PC) reported FI within the last 30 days. This finding is at least 3 times higher than most recent monthly estimate of FI prevalence.2 The reasons for increased FI prevalence in our population is likely multifold. Our population is older with a mean age of 59. From prior studies, age is definite risk factor for increasing prevalence of FI.1,2 Additionally in our population, there was high prevalence of diabetes mellitus which is a known risk factor for FI.13,26 The presence of diabetes was noted to be slightly higher in the PC participants compared to the GI participants, but not statistically significant. However, our findings were higher than prior national estimates of Veterans with diabetes, as Reiber et al27 estimated the prevalence in diabetes in male Veterans receiving VA care was 16%. Further reasons for this high rate of FI need to be further studied and these findings confirmed with a population-based survey.
Results from our study show that subjects with more bowel movements per week (P = 0.005) and per day (P < 0.001) and with a higher BSFS (P = 0.010) were more likely to have FI. These findings are congruent with the literature, as FI often occurs in conditions that cause diarrhea.28–30 We found that those with FI were more likely to have loose consistency stools (BSFS type 5, 6, and 7; P = 0.002). Although diarrhea is often a presenting complaint leading to GI clinic evaluation, similar reports of FI were found between GI and PC clinics (P = 0.078). Importantly, there was also no significant difference between type of FI between clinic types, although liquid stool incontinence showed a slight predominance in GI participants (53.1%) as compared to PC participants (39.6%). Therefore, our study emphasizes the critical point that a provider should ask any patient who suffers from diarrhea about episodes of FI.
Using the FISI score, a patient-based scale assessing the degree of FI adapted from Rockwood et al,21 prior work has shown that FISI scores are highly correlated with quality-of-life measures.23 This included measures such as life-style restriction, depression, and embarrassment, with scores greater than 30 predicting a detrimental effect on quality of life. From our study, the mean FISI score was 23.0 ± 9.5 with a significantly higher symptom score in GI participants (25.2 ± 10.0) compared to PC participants (20.1 ± 8.2). Fifteen GI participants (30.6%) reported a FISI greater than 30 compared to 4 PC participants (10.5%) (P = 0.024). Additionally, a sizeable percentage of participants required the use of protective pads (28.7%) or protective undergarments (19.5%), which varied minimally by clinic type. From the work of Rockwood et al21 the use of a pad or accidental leakage was also found to be highly correlated with the FISI score; however, their study revealed only 8% of individuals reported wearing a protective pad.
Our study also demonstrates that FI is a persistently under-recognized problem. FI can be a difficult topic to discuss for some patients due to embarrassment or other social factors and not always reported to their medical provider. A concerning finding from our study was that few participants had ever been asked by or evaluated by a doctor for their leakage symptoms. However, this is consistent with earlier reports in the literature with less than a third of people suffering from this condition having discussed their symptoms with a health care professional.1,31,32 Of those asked about symptoms related to leakage, gastroenterologists were involved in assessing symptoms in 68.2% of cases, whereas primary care physicians asked in 36.4% of cases. In both clinic settings, more needs to be done to recognize this complaint, as FI can have a devastating impact on quality of life.
Our study has several potential limitations. The primary limitation is the cross-section of participants surveyed. Although subjects with scheduled appointments in 2 clinics were included, there may be selection bias and thus may not represent all Veterans. However, given that no significance was found between the report of FI between PC and GI clinics, our results suggest that FI is also a common complaint among those without underlying bowel or digestive health issues. To counter this, an overall high response rate was seen, further strengthening our results and findings. Administering the survey in a population-based study format would address these issues. Overall, the generalizability of our findings to other populations may be limited. Our study also relied on self-report, therefore recall bias may be introduced by the study design.
In conclusion, FI is a common complaint and under-recognized problem among a cross-section of veterans in both GI and PC clinics. Despite its prevalence, relatively few participants were asked about leakage, with even less being treated. Stemming from these findings, a large-scale study among Veterans should be pursued to determine the actual impact and prevalence of this condition in the Veteran population.
Appendix.
Footnotes
Conflicts of interest: None.
Author contributions: Amy E Hosmer: acquisition of data, analysis and interpretation of data, and drafting of the manuscript; Sameer D Saini: analysis and interpretation of data, and critical revision of the manuscript for important intellectual content; and Stacy B Menees: study concept and design, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, and statistical analysis.
Financial support: None.
References
- 1.Whitehead WE, Borrud L, Goode PS, et al. Fecal incontinence in US adults: epidemiology and risk factors. Gastroenterology. 2009;137:512–517. e1–e2. doi: 10.1053/j.gastro.2009.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ditah I, Devaki P, Luma HN, et al. Prevalence, trends, and risk factors for fecal incontinence in United States adults, 2005–2010. Clin Gastroenterol Hepatol. 2014;12:636–643. e1–e2. doi: 10.1016/j.cgh.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 3.Alsheik EH, Coyne T, Hawes SK, et al. Fecal incontinence: prevalence, severity, and quality of life data from an outpatient gastroenterology practice. Gastroenterol Res Pract. 2012;2012 doi: 10.1155/2012/947694. 947694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nelson R, Furner S, Jesudason V. Fecal incontinence in Wisconsin nursing homes: prevalence and associations. Dis Colon Rectum. 1998;41:1226–1229. doi: 10.1007/BF02258218. [DOI] [PubMed] [Google Scholar]
- 5.Halland M, Koloski NA, Jones M, et al. Prevalence correlates and impact of fecal incontinence among older women. Dis Colon Rectum. 2013;56:1080–1086. doi: 10.1097/DCR.0b013e31829203a9. [DOI] [PubMed] [Google Scholar]
- 6.Rømmen K, Schei B, Rydning A, Sultan AH, Mørkved S. Prevalence of anal incontinence among Norwegian women: a cross-sectional study. BMJ Open. doi: 10.1136/bmjopen-2012-001257. Published Online First: 30 Jun 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Botlero R, Bell RJ, Urquhart DM, Davis SR. Prevalence of fecal incontinence and its relationship with urinary incontinence in women living in the community. Menopause. 2011;18:685–689. doi: 10.1097/gme.0b013e3181fee03b. [DOI] [PubMed] [Google Scholar]
- 8.Martins G, Soler ZA, Cordeiro JA, Amaro JL, Moore KN. Prevalence and risk factors for urinary incontinence in healthy pregnant Brazilian women. Int Urogynecol J. 2010;21:1271–1277. doi: 10.1007/s00192-010-1185-2. [DOI] [PubMed] [Google Scholar]
- 9.Bharucha AE, Zinsmeister AR, Locke GR, et al. Prevalence and burden of fecal incontinence: a population-based study in women. Gastroenterology. 2005;129:42–49. doi: 10.1053/j.gastro.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 10.Chen GD, Hu SW, Chen YC, Lin TL, Lin LY. Prevalence and correlations of anal incontinence and constipation in Taiwanese women. Neurourol Urodyn. 2003;22:664–669. doi: 10.1002/nau.10067. [DOI] [PubMed] [Google Scholar]
- 11.Kok AL, Voorhorst FJ, Burger CW, van Houten P, Kenemans P, Janssens J. Urinary and faecal incontinence in community-residing elderly women. Age Ageing. 1992;21:211–215. doi: 10.1093/ageing/21.3.211. [DOI] [PubMed] [Google Scholar]
- 12.Eva UF, Gun W, Preben K. Prevalence of urinary and fecal incontinence and symptoms of genital prolapse in women. Acta Obstet Gynecol Scand. 2003;82:280–286. doi: 10.1034/j.1600-0412.2003.00103.x. [DOI] [PubMed] [Google Scholar]
- 13.Melville JL, Fan MY, Newton K, Fenner D. Fecal incontinence in US women: a population-based study. Am J Obstet Gynecol. 2005;193:2071–2076. doi: 10.1016/j.ajog.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 14.Nelson R, Norton N, Cautley E, Furner S. Community-based prevalence of anal incontinence. JAMA. 1995;274:559–561. doi: 10.1001/jama.1995.03530070057030. [DOI] [PubMed] [Google Scholar]
- 15.Drossman DA, Li Z, Andruzzi E, et al. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38:1569–1580. doi: 10.1007/BF01303162. [DOI] [PubMed] [Google Scholar]
- 16.O’Keefe EA, Talley NJ, Zinsmeister AR, Jacobsen SJ. Bowel disorders impair functional status and quality of life in the elderly: a population-based study. J Gerontol A Biol Sci Med Sci. 1995;50:M184–M189. doi: 10.1093/gerona/50A.4.M184. [DOI] [PubMed] [Google Scholar]
- 17.Kalantar JS, Howell S, Talley NJ. Prevalence of faecal incontinence and associated risk factors; an underdiagnosed problem in the Australian community? Med J Aust. 2002;176:54–57. doi: 10.5694/j.1326-5377.2002.tb04283.x. [DOI] [PubMed] [Google Scholar]
- 18.Menees SB, Almario CV, Spiegel BMR, Chey WD. Prevalence of and factors associated with fecal incontinence: results from a population-based survey. Gastroenterology. 2018;154:1672–1681. e3. doi: 10.1053/j.gastro.2018.01.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroentero. 1997;32:920–924. doi: 10.3109/00365529709011203. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. National health and nutrition examination survey 2009–2010 data documentation, codebook, and frequencies. [accessed 28 September, 2019];Depression Screener 2013. Available from URL: https://www.cdc.gov/nchs/nhanes/index.htm.
- 21.Rockwood TH, Church JM, Fleshman JW, et al. Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: the fecal incontinence severity index. Dis Colon Rectum. 1999;42:1525–1532. doi: 10.1007/BF02236199. [DOI] [PubMed] [Google Scholar]
- 22.Kish L. Survey Sampling. New York: John Wiley and Sons; 1995. [Google Scholar]
- 23.Cavanaugh M, Hyman N, Osler T. Fecal incontinence severity index after fistulotomy: a predictor of quality of life. Dis Colon Rectum. 2002;45:349–353. doi: 10.1007/s10350-004-6181-5. [DOI] [PubMed] [Google Scholar]
- 24.Adolfsson J, Helgason AR, Dickman P, Steineck G. Urinary and bowel symptoms in men with and without prostate cancer: results from an observational study in the Stockholm area. Eur Urol. 1998;33:11–16. doi: 10.1159/000019528. [DOI] [PubMed] [Google Scholar]
- 25.Cohan JN, Chou AB, Varma MG. Faecal incontinence in men referred for specialty care: a cross-sectional study. Colorectal Dis. 2015;17:802–809. doi: 10.1111/codi.12943. [DOI] [PubMed] [Google Scholar]
- 26.Quander CR, Morris MC, Melson J, Bienias JL, Evans DA. Prevalence of and factors associated with fecal incontinence in a large community study of older individuals. Am J Gastroenterol. 2005;100:905–909. doi: 10.1111/j.1572-0241.2005.30511.x. [DOI] [PubMed] [Google Scholar]
- 27.Reiber GE, Koepsell TD, Maynard C, Haas LB, Boyko EJ. Diabetes in nonveterans, veterans, and veterans receiving department of veterans affairs health care. Diabetes Care. 2004;27(suppl 2):B3–B9. doi: 10.2337/diacare.27.suppl_2.B3. [DOI] [PubMed] [Google Scholar]
- 28.Rao SS, Bharucha AE, Chiarioni G, et al. Functional anorectal disorders. Gastroenterology. doi: 10.1053/j.gastro.2016.02.009. Published Online First: 25 Mar 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bharucha AE, Zinsmeister AR, Locke GR, et al. Risk factors for fecal incontinence: a population-based study in women. Am J Gastroenterol. 2006;101:1305–1312. doi: 10.1111/j.1572-0241.2006.00553.x. [DOI] [PubMed] [Google Scholar]
- 30.Bharucha AE, Zinsmeister AR, Schleck CD, Melton LJ., 3rd Bowel disturbances are the most important risk factors for late onset fecal incontinence: a population-based case-control study in women. Gastroenterology. 2010;139:1559–1566. doi: 10.1053/j.gastro.2010.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dunivan GC, Heymen S, Palsson OS, et al. Fecal incontinence in primary care: prevalence, diagnosis, and health care utilization. Am J Obstet Gynecol. 2010;202:493, e1–e6. doi: 10.1016/j.ajog.2010.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johanson JF, Lafferty J. Epidemiology of fecal incontinence: the silent affliction. Am J Gastroenterol. 1996;91:33–36. [PubMed] [Google Scholar]