Abstract
The aim of our study was to compare early and long-term outcome of patients undergoing either on-pump or off-pump coronary artery bypass grafting with special focus on impairment of renal function. Five hundred ninety-three consecutive patients undergoing coronary artery bypass grafting were retrospectively analyzed. They were assigned either to on-pump (n = 281) or to off-pump (n = 312) group. Early and long-term outcomes were analyzed with special focus on renal function. Basic demographics and preoperative characteristics did not differ between groups (p>0.05) as well as postoperative renal parameters (p>0.05). Postoperative odds ratios (OR) of off-pump group in comparison to on-pump group were higher without reaching significance in terms of incidence of gastrointestinal complications and pneumonia (OR = 2.23 and 1.61, respectively) as well as hazard ratios (HR) on long-term follow-up for mortality and incidence of myocardial infarction (HR = 1.50 and 2.29, respectively). Kaplan-Meier estimation analysis also revealed similar results for both groups in terms of mid- and long-term survival (Breslow p = 0.062 and Log-Rank p = 0.064, respectively) and for incidence of myocardial infarction (Breslow p = 0.102 and Log-Rank p = 0.103, respectively). Our study suggests that use or not use of coronary artery bypass did not influence postoperative renal function. Odds of early outcomes were similar in both groups as well as incidence of myocardial infarction and mortality in long-term follow-up.
Introduction
Cardiac surgery with coronary artery bypass grafting is one of the most frequently applied surgeries world-wide. Numerous studies have been performed in order to compare outcomes of coronary artery bypass grafting (CABG) without (OPCAB) and with use of heart-lung machine (HLM) [1–4]. The conflicting results remain a source of debate. Some studies reported favourable outcomes associated with off-pump surgery [4–9].
Large-scale prospective randomized trials have shown trends towards reduced early risks after off-pump surgery. However these early benefits could not be confirmed in terms of long-term follow-up [3, 10, 11]. Also, worse outcomes of off-pump in comparison to on-pump CABG surgery have been reported concerning graft patency as well as for greater need for coronary reintervention up to one year after surgery [12].
Impairment of renal failure is known to be an important risk factor for increased postoperative mortality of patients after on-pump CABG [13–15]. On-pump surgery may be associated with accelerated growth of atherosclerosis plaques and cardiac calcification which increases operative risk. Becoming an established and feasible technique, OPCAB studies provided a greater benefit in patients with risk for development of renal failure after surgery [16, 17]. It is also known that renal failure can lead to advanced atherosclerotic burden due to changes in calcium metabolism. OPCAB may be a better alternative because of decreased blood loss, and shorter hospital stay [1, 18]. Previously published studies comparing the effect of off-pump versus on-pump CABG on clinical end-points with respect to renal impairment have yielded conflicting results [9, 19, 20].
Therefore, to shed further light on this issue, we performed a retrospective analysis to compare early and long-term outcomes of patients undergoing either on-pump or off-pump coronary artery revascularization with special focus on renal impairment.
Materials and methods
Patients (n = 593) with coronary artery disease were scheduled to undergo coronary artery bypass grafting from January 2009 to October 2012 in our institution and were retrospectively analyzed. Exclusion criteria were as follows: associated valve surgery procedures, supra-aortic vessel diseases and contraindications to aortic cross-clamping. Decisions about the type of treatment were taken according to local practices and patients were assigned to off-pump or to on-pump surgery group. Three hundred and twelve patients received off-pump and 281 patients underwent on-pump surgery.
This study has been carried out in accordance with the Declaration of Helsinki. The study design was a retrospective review of collected registry data. The Ethics Committee waived both the need for ethics approval and informed consent from patients.CABG technique has been previously described [21]. Off-pump surgery was defined as coronary artery bypass grafting (CABG) without use of heart-lung machine (OPCAB) and on-pump surgery was defined as CABG with use of heart-lung machine.
Statistical analysis
Statistic was performed using Student’s t-Test or Mann-Whitney-U Test depending if continuous variables are normally distributed or not and Chi-Square Test was applied for categorical variables. Fisher’s exact Test was performed when the minimum expected count of cells was <5. Univariate regression analysis [Odds ratio (OR)] and Cox regression analysis [Hazard Ratio (HR)] were performed to address predictors for early and long-term outcomes. Kaplan-Meier survival estimation analysis was used to address mid- and long-term survival. A p-value <0.05 was considered significant. All statistical analysis was performed using SPSS Version 25.0 (IBM Corp, Chicago, IL, USA).
Results
Basic demographics and preoperative variables did not significantly differ between both groups (p>0.05) (Table 1). Median age at surgery was 69 years in OPCAB group versus 68 years in on-pump group (p = 0.584). Also, gender, weight and urgency of surgery revealed similar results for both groups (p>0.05). In terms of number of comorbidities, incidence of diabetes, hyperlipidemia, arterial hypertension also similar results were found for both groups (p>0.05). Further, incidence of preoperative apoplexy and carotid artery stenosis did not reveal significant differences.
Table 1. Demographic and preoperative variables of patients undergoing coronary artery bypass surgery.
| OPCAB | HLM | p-value | |
|---|---|---|---|
| Age | 69 (58.25;74) | 68 (59;74) | 0.584 |
| BMI | 27 (25;30) | 28 (25;30) | 0.584 |
| Female | 84 (26.9%) | 70 (24.9%) | 0.577 |
| LVEF (%) | 67 (54;70) | 59.5 (46;70) | <0.001 |
| Vessel CHD | 2 (2;3) | 3 (3;3) | <0.001 |
| Left main stenosis | 60 (19.3%) | 80 (28.5%) | 0.009 |
| Number of bypasses | <0.001 | ||
| 1 | 101 (32.4%) | 5 (1.8%) | |
| 2 | 131 (42.0%) | 54 (19.2%) | |
| 3 | 76 (24.4%) | 137 (48.8%) | |
| 4 | 4 (1.3%) | 69 (24.6%) | |
| 5 | 0 (0.0%) | 16 (5.7%) | |
| Urgency of surgery | 0.209 | ||
| Emergency | 33 (10.6%) | 34 (12.3%) | |
| Urgent | 36 (11.5%) | 44 (15.9%) | |
| Elective | 243 (77.9%) | 199 (71.8%) | |
| Comorbidities | |||
| Diabetes mellitus | 102 (32.7%) | 100 (35.6%) | 0.389 |
| Hyperlipidemia | 217 (68.6%) | 205 (73.0%) | 0.361 |
| Arterial Hypertension | 296 (94.9%) | 269 (95.7%) | 0.623 |
| COPD | 33 (10.6%) | 32 (11.4%) | 0.763 |
| PAOD | 45 (14.4%) | 40 (14.2%) | 0.948 |
| Apoplex | 21 (6.7%) | 19 (6.8%) | 0.988 |
| Renal insufficiency | 48 (15.4%) | 34 (12.1%) | 0.247 |
| IABP preoperative | 1 (0.3%) | 3 (0.7%) | 1.000 |
| Carotid artery stenosis | 33 (10.6%) | 38 (13.5%) | 0.270 |
| Rhythm | 0.977 | ||
| Sinus rhythm | 280 (90.3%) | 254 (90.4%) | |
| Atrial fibrillation | 30 (9.7%) | 27 (9.6%) | |
| Smoker | 73 (23.4%) | 76 (27.0%) | 0.371 |
| Laboratory parameters | |||
| Haemoglobin (g/dL) | 13.8 (12.2;14.7) | 13.8 (12.7;14.9) | 0.232 |
| Hematocrit (%) | 40 (37;43) | 41 (38;43) | 0.307 |
| Creatinine (mg/dL) | 0.92 (0.78;1.08) | 0.94 (0.79;1.08) | 0.897 |
| Urea (mg/dL) | 38 (31;47.25) | 38 (31;46.25) | 0.893 |
| Creatine kinase- MB (U/L) | 15 (11;20) | 14 (11;20) | 0.739 |
| Thrombocytes x 109/L | 229 (191;276) | 243 (199;283) | 0.027 |
| Quick (%) | 99 (91;106) | 99 (89;105) | 0.269 |
| aPTT (sec) | 26 (24;28) | 26 (24;28) | 0.354 |
| Medication | |||
| Digitalis | 4 (1.3%) | 3 (1.1%) | 1.000 |
| ACE- inhibitors | 190 (60.9%) | 169 (60.1%) | 0.851 |
| Beta- blockers | 235 (75.3%) | 211 (75.1%) | 0.948 |
| Calcium channel blocker | 66 (21.3%) | 49 (17.9) | 0.301 |
| Diuretics | 109 (35.2%) | 97 (35.4%) | 0.952 |
| Statins | 229 (73.9%) | 187 (68.2%) | 0.189 |
| Antidiabetics | 94 (30.3%) | 68 (24.8%) | 0.067 |
| Aspirin | 238 (76.8%) | 234 (85.1%) | 0.011 |
BMI, Body mass index; LVEF, left ventricular ejection fraction; CHD, coronary heart disease; CABG, coronary artery bypass graft; COPD, chronic obstructive pulmonary disease; PAOD, peripheral artery occlusion disease; IABP, intraaortic balloon pump; creatinine kinase MB, creatine kinase muscle brain; aPTT, activated thromboplastin time.
Number of bypasses significantly differed between groups (p<0.001). Off-pump surgery group mostly comprised integration of one or two bypass grafts, whereas on-pump surgery group comprised three to five grafts.
Laboratory parameters were similarly distributed between both groups, such as hemoglobin (p = 0.232) and anticoagulation parameters (p = 0.269). Median of preoperative creatinine value was 0.92 (mg/dL) in OPCAB group versus 0.94 (mg/dL) in on-pump group revealing no statistical significance (p = 0.897). Also, urea did not preoperatively differ between groups (p = 0.893).
Intra- and postoperative variables of patients undergoing coronary artery bypass grafting with and without use of heart-lung machine are presented in Table 2.
Table 2. Intraoperative and early postoperative variables of patients undergoing coronary artery bypass surgery.
| OPCAB | HLM | p-value | |
|---|---|---|---|
| Cross-clamp time(min) | 0 | 43 (34;51.5) | <0.001 |
| Duration of surgery (min) | 130 (109;165) | 180 (157;210) | <0.001 |
| Cardiopulmonary bypass time (min) | 0 | 79 (64;94.5) | <0.001 |
| IABP intraoperative | 6 (1.9%) | 13 (14.7%) | 0.057 |
| IABP perioperative | 12 (3.9%) | 14 (5.1%) | 0.464 |
| Catecholamines | 0.251 | ||
| Catecholamines <24h | 249 (80.0%) | 205 (75.4%) | |
| Catecholamines 24h- 48h | 28 (9.1%) | 29 (10.7%) | |
| Catecholamines >48h | 31(10.1%) | 38 (14.0%) | |
| ICU stay (days) | 2 (1;3) | 2 (1;4) | 0.050 |
| Time for intubation (hours) | 14 (11;19) | 16 (12;21) | 0.002 |
| Drainage output over 24h (ml) | 700 (520;1010) | 750 (530;1135) | 0.082 |
| IABP postoperative | 6 (1.9%) | 1 (0.4%) | 0.081 |
| Re-thoracotomy | 17 (5.4%) | 13 (4.7%) | 0.685 |
| Gastrointestinal complications | 5 (1.6%) | 2 (0.7%) | 0.457 |
| Infection | 18 (5.8%) | 18 (6.5%) | 0.704 |
| Pneumonia | 9 (2.9%) | 5 (1.8%) | 0.394 |
| Dialysis postoperative | 13 (4.2%) | 6 (2.2%) | 0.178 |
| In- hospital stay (days) | 12 (10;14) | 13 (11;16) | <0.001 |
| Follow-up (7-year) | |||
| Re-thoracotomy | 0 (0%) | 4 (1.4%) | 0.038 |
| Apoplexy | 8 (2.6%) | 10 (3.6%) | 0.327 |
| Myocardial infarction | 14 (4.5%) | 5 (1.8%) | 0.085 |
| Mortality | 60 (19.2%) | 31 (11.0%) | 0.044 |
| Laboratory parameters | |||
| Creatinine 1. Day (mg/dL) | 1.0 (0.83;1.22) | 1.02 (0.83;1.27) | 0.505 |
| Creatinine 3. Day (mg/dL) | 1.04 (0.86;1.5) | 1.06 (0.81;1.57) | 0.916 |
| Urea 1. Day (mg/dL) | 38 (30;48) | 38 (30;49) | 0.809 |
| Urea 3. Day (mg(dL) | 49 (37;72.25) | 54 (42;72) | 0.160 |
| Creatine kinase- MB 1. Day (U/L) | 18 (14;29) | 30 (24;41) | <0.001 |
| Creatine kinase- MB 3. Day (U/L) | 16 (12;22) | 17 (13;24) | 0.131 |
| Lactate 1. Day | 1.7 (1.3;2.6) | 2.1 (1.5;3) | <0.001 |
| Lactate 3. Day | 1.5 (1.1;2.0) | 1.8 (1.3;2.28) | 0.016 |
IABP, intra-aortic balloon pump; ICU, intensive care unit.
Cross-clamp and cardiopulmonary bypass time significantly differed between groups (p<0.001)—per definitionem—as expected due to categorization. Duration of surgery revealed significant differences between the groups (p<0.001).
ICU stay was similarly distributed between both groups as well as need for catecholamines (p = 0.251). In terms of development of complications, such as incidence of gastrointestinal complications (p = 0.478) or incidence of pneumonia (p = 0.394) no significant differences could be detected. Patients in OPCAB group stayed 12 days in hospital and patients in on-pump group 13 days.
Survival of 7-year long-term follow-up was similar between both groups (p = 0.061). Incidence of development of postoperative apoplexy and myocardial infarction was similarly distributed between the groups (p = 0.323 and p = 0.137, respectively).
In terms of postoperative laboratory renal function parameters creatinine values did not significantly differ on postoperative day 1 and day 3 (p = 0.505 and p = 0.916). Also, no significant differences were found for urea values between the groups (p = 0.809).
Odds ratios (OR) for early outcomes and hazard ratios (HR) for long-term outcomes are depicted in Table 3. Patients in OPCAB group revealed higher odds for gastrointestinal complications and pneumonia in comparison to on-pump surgery group without reaching significance (OR = 2.23 and 1.61; both p>0.05). During long-term follow-up incidence for myocardial infarction was 2.3-fold and for mortality 1.5-fold higher in OPCAB group than in on-pump group (HR = 2.29 and 1.50, respectively; both p>0.05), whereas vice versa incidence of apoplexy was 37% reduced (HR = 0.63, p>0.05). All variables did not reach significance.
Table 3. Odds ratios (OR) and hazard ratios (HR), 95% confidence intervals (95%-CI) and p-values of selected outcome variables of patients undergoing coronary artery bypass surgery.
| OR | 95%-CI | p-value | |
| Re-thoracotomy | 1.17 | 0.56–2.45 | 0.685 |
| Gastrointestinal complications | 2.23 | 0.43–11.60 | 0.340 |
| Infection | 0.88 | 0.45–1.72 | 0.704 |
| Pneumonia | 1.61 | 0.53–4.86 | 0.399 |
| Dialysis postoperative | 1.94 | 0.73–5.18 | 0.185 |
| HR | 95%-CI | p-value | |
| Re-thoracotomy | 0.01 | 0.00–40.44 | 0.285 |
| Apoplexy | 0.63 | 0.25–1.60 | 0.329 |
| Myocardial infarction | 2.29 | 0.82–6.34 | 0.113 |
| Mortality | 1.50 | 0.98–2.38 | 0.066 |
OR and HR in favour of OPCAB in comparison to HLM.
Kaplan-Meier survival estimation analysis depicts mid- (Breslow) and long-term (Log-Rank) survival for up to 7-year follow-up of patients requiring coronary artery bypass surgery with and without use of heart-lung machine revealing similar results between groups (Breslow p = 0.062; Log-Rank p = 0.064) (Fig 1) as well as for incidence of myocardial infarction (Table 4).
Fig 1. Kaplan-Meier survival estimation plot of coronary artery bypass graft surgery with and without use of heart-lung machine (HLM).
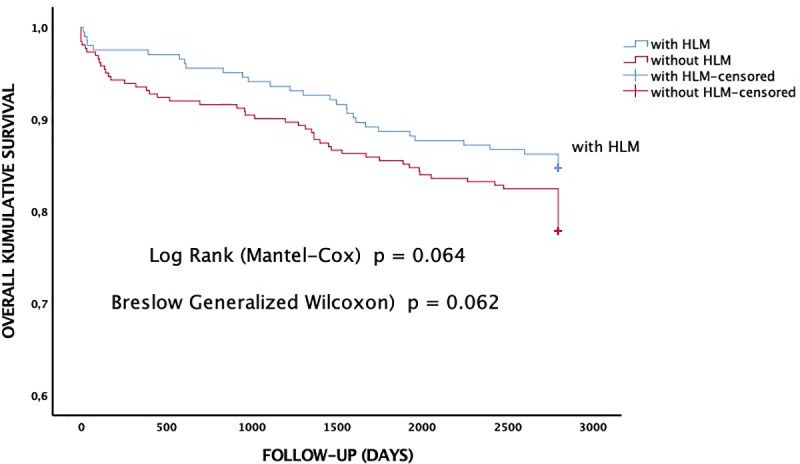
Table 4. p-values of Kaplan-Meier mid-term (Breslow) and long-term (Log-Rank) estimation analysis up to 7-year follow-up.
| Kaplan-Meier | Breslow | Log-Rank | |
|---|---|---|---|
| Survival | a | 0.062 | 0.064 |
| Re-thoracotomy | b | 0.199 | 0.197 |
| Myocardial infarction | a | 0.102 | 0.103 |
| Apoplexy | b | 0.321 | 0.324 |
a in favour of HLM; b in favour of OPCAB.
Discussion
Coronary artery bypass grafting is one of the most often performed surgeries world-wide with an increasing demand. Many studies revealed that use of heart-lung machine provokes inflammation leading to organ dysfunction and increased mortality [4, 22, 23].
Cardiac surgery with use of cardiopulmonary bypass support initiates a systemic inflammatory response presumably caused by contact of blood components with the artificial surface of the extracorporeal circuit, associated with postoperative morbidity and mortality [22, 24, 25]. In this regard, many studies demonstrated increased inflammatory markers, such as TNF-α, IL-6, IL-8 after cardiac surgery with cardiopulmonary bypass (CPB) inducing organ failure [26]. Massive activation of leukocytes, e.g. neutrophils, and different biochemical pathways may result in microthrombosis, microemboli and depletion of coagulation factors [22]. These factors contribute to tissue injury and endothelial dysfunction, to predisposing patients to organ injury and to increasing perivascular edema [22, 27]. Renal dysfunction can be a common complication after coronary artery bypass surgery with use of heart-lung machine [4, 9]. The inflammatory reaction is induced by use of the heart-lung machine. Some studies revealed a correlation in terms of duration of heart-lung machine with kidney injury [22]. One aim of this study was to evaluate early outcomes with respect to renal function comparing OPCAB with on-pump surgery. Studies revealed controversial results in this field [1, 28, 29]. It has been speculated that coronary artery bypass surgery without use of extracorporeal circulation might positively influence incidence and seriousness of acute renal failure [30]. Li et al. described an incidence of AKI of 37.1% after off-pump surgery [31]. Our study reported similar rates of occurrence of renal failure between groups, confirming the findings of other trials showing that off-pump surgery is not associated with decreased rates or reduced severity of acute renal failure [10, 11]. We also found that impairment of renal function did not differ between groups. Singh et al. measured creatinine up to 4 days postoperatively and the results were similar compared with preoperative levels. They found no statistically significant rise in creatinine in either of the two groups corroborating our results [32]. Thus, they concluded that renal function is not affected by the technique of coronary artery bypass surgery whether with or without cardiopulmonary bypass in spite of the theoretical expected advantage of off-pump surgery [32].
Medved et al. also found no difference in postoperative creatine kinase MB after first day and stay on ICU corroborating our results [20]. Additionally, they revealed similar results in early mortality, whereas we found of a 1.5-fold higher risk for OPCAB group in long-term follow-up (HR = 1.50; p = 0.066) without reaching significance between groups. Also Kaplan-Meier estimation analysis showed similar results between groups (Log-Rank p = 0.064). In our study the number of grafts was similar to the results by Lycops et al. [19]. Interestingly, in terms of 5-year survival Lycops et al. revealed 78% in OPCAB group and 68% in on-pump group, whereas we found a 7-year follow-up survival rate of 81% in OPCAB surgery and 89% in on-pump group. Also, Nicolini et al. found out that on-pump surgery is associated with a lower 5-year mortality than OPCAB group corroborating our results [4]. They also found no differences in terms of incidence of myocardial infarction or stroke affirming our findings. Additionally preoperative statin use does not influence development of postoperative AKI [33].
Conclusion
Regarding postoperative renal impairment we did not find any differences between patients’ groups undergoing off- or on-pump surgery. Also, odds of early outcomes were similar in both groups as well as incidence of myocardial infarction and mortality in long-term follow-up.
Study limitations
This study is limited by its retrospective nature, heterogeneity of patient population and relatively small number of patients from a single hospital center. Also, the retrospective nature of this study may introduce confounders and bias of patient selection.
Supporting information
(SAV)
Acknowledgments
We thank Mohamed Zeriouh and Anton Sabashnikov, both former residents at cardiothoracic surgery in Harefield Hospital, London, UK, for reading and editing the manuscript.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Puskas JD, Williams WH, Duke PG, Staples JR, Glas KE, Marshall JJ, et al. Off-pump coronary artery bypass grafting provides complete revascularization with reduced myocardial injury, transfusion requirements, and length of stay: a prospective randomized comparison of two hundred unselected patients undergoing off-pump versus conventional coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125(4):797–808. 10.1067/mtc.2003.324 [DOI] [PubMed] [Google Scholar]
- 2.Sedrakyan A, Wu AW, Parashar A, Bass EB, Treasure T. Off-pump surgery is associated with reduced occurrence of stroke and other morbidity as compared with traditional coronary artery bypass grafting: a meta-analysis of systematically reviewed trials. Stroke. 2006;37(11):2759–69. 10.1161/01.STR.0000245081.52877.f2 [DOI] [PubMed] [Google Scholar]
- 3.Lamy A, Devereaux PJ, Prabhakaran D, Taggart DP, Hu S, Straka Z, et al. Five-Year Outcomes after Off-Pump or On-Pump Coronary-Artery Bypass Grafting. N Engl J Med. 2016;375(24):2359–68. 10.1056/NEJMoa1601564 [DOI] [PubMed] [Google Scholar]
- 4.Nicolini F, Fortuna D, Contini GA, Pacini D, Gabbieri D, Zussa C, et al. Comparison between off- and on-pump coronary artery bypass grafting: long-term results of a real-world registry. Eur J Cardiothorac Surg. 2016;50(3):528–35. 10.1093/ejcts/ezw128 [DOI] [PubMed] [Google Scholar]
- 5.Staton GW, Williams WH, Mahoney EM, Hu J, Chu H, Duke PG, et al. Pulmonary outcomes of off-pump vs on-pump coronary artery bypass surgery in a randomized trial. Chest. 2005;127(3):892–901. 10.1378/chest.127.3.892 [DOI] [PubMed] [Google Scholar]
- 6.Puskas JD, Williams WH, Mahoney EM, Huber PR, Block PC, Duke PG, et al. Off-pump vs conventional coronary artery bypass grafting: early and 1-year graft patency, cost, and quality-of-life outcomes: a randomized trial. JAMA. 2004;291(15):1841–9. 10.1001/jama.291.15.1841 [DOI] [PubMed] [Google Scholar]
- 7.Takagi H, Tanabashi T, Kawai N, Umemoto T. Off-pump surgery does not reduce stroke, compared with results of on-pump coronary artery bypass grafting: a meta-analysis of randomized clinical trials. J Thorac Cardiovasc Surg. 2007;134(4):1059–60. 10.1016/j.jtcvs.2007.07.006 [DOI] [PubMed] [Google Scholar]
- 8.Bakaeen FG, Chu D, Kelly RF, Ward HB, Jessen ME, Chen GJ, et al. Performing coronary artery bypass grafting off-pump may compromise long-term survival in a veteran population. Ann Thorac Surg. 2013;95(6):1952–8; discussion 9–60. 10.1016/j.athoracsur.2013.02.064 [DOI] [PubMed] [Google Scholar]
- 9.Wang Y, Zhu S, Gao P, Zhou J, Zhang Q. Off-pump versus on-pump coronary surgery in patients with chronic kidney disease: a meta-analysis. Clin Exp Nephrol. 2018;22(1):99–109. 10.1007/s10157-017-1432-7 [DOI] [PubMed] [Google Scholar]
- 10.Lamy A, Devereaux PJ, Prabhakaran D, Taggart DP, Hu S, Paolasso E, et al. Effects of off-pump and on-pump coronary-artery bypass grafting at 1 year. N Engl J Med. 2013;368(13):1179–88. 10.1056/NEJMoa1301228 [DOI] [PubMed] [Google Scholar]
- 11.Diegeler A, Reents W, Zacher M. Off-pump or on-pump coronary-artery bypass grafting. N Engl J Med. 2013;369(2):196–7. [DOI] [PubMed] [Google Scholar]
- 12.Houlind K, Fenger-Gron M, Holme SJ, Kjeldsen BJ, Madsen SN, Rasmussen BS, et al. Graft patency after off-pump coronary artery bypass surgery is inferior even with identical heparinization protocols: results from the Danish On-pump Versus Off-pump Randomization Study (DOORS). J Thorac Cardiovasc Surg. 2014;148(5):1812–9 e2. 10.1016/j.jtcvs.2014.02.024 [DOI] [PubMed] [Google Scholar]
- 13.Magee MJ, Coombs LP, Peterson ED, Mack MJ. Patient selection and current practice strategy for off-pump coronary artery bypass surgery. Circulation. 2003;108 Suppl 1:II9–14. [DOI] [PubMed] [Google Scholar]
- 14.Spina S, Lei C, Pinciroli R, Berra L. Hemolysis and Kidney Injury in Cardiac Surgery: The Protective Role of Nitric Oxide Therapy. Semin Nephrol. 2019;39(5):484–95. 10.1016/j.semnephrol.2019.06.008 [DOI] [PubMed] [Google Scholar]
- 15.Zaouter C, Potvin J, Bats ML, Beauvieux MC, Remy A, Ouattara A. A combined approach for the early recognition of acute kidney injury after adult cardiac surgery. Anaesth Crit Care Pain Med. 2018;37(4):335–41. 10.1016/j.accpm.2018.05.001 [DOI] [PubMed] [Google Scholar]
- 16.Boyd WD, Desai ND, Del Rizzo DF, Novick RJ, McKenzie FN, Menkis AH. Off-pump surgery decreases postoperative complications and resource utilization in the elderly. Ann Thorac Surg. 1999;68(4):1490–3. 10.1016/s0003-4975(99)00951-0 [DOI] [PubMed] [Google Scholar]
- 17.Kim HJ, Chung JE, Jung JS, Kim IS, Son HS. Current Status of Off-pump Coronary Artery Bypass Grafting in Patients with Multiple Coronary Artery Disease Compared with On-pump Coronary Artery Bypass Grafting: The Korean National Cohort Study. Thorac Cardiovasc Surg. 2018;66(6):470–6. 10.1055/s-0038-1651516 [DOI] [PubMed] [Google Scholar]
- 18.Dai Z, Chu H, Wang S, Liang Y. The effect of tranexamic acid to reduce blood loss and transfusion on off-pump coronary artery bypass surgery: A systematic review and cumulative meta-analysis. J Clin Anesth. 2018;44:23–31. 10.1016/j.jclinane.2017.10.004 [DOI] [PubMed] [Google Scholar]
- 19.Lycops A, Wever C, Vandekerkhof J, Mees U, Hendrikx M. Midterm follow-up after off-pump versus on-pump coronary artery bypass grafting. Results from a case-matched study. Acta Cardiol. 2005;60(3):311–7. 10.2143/AC.60.3.2005010 [DOI] [PubMed] [Google Scholar]
- 20.Medved I, Anic D, Zrnic B, Ostric M, Saftic I. Off-pump versus on-pump—intermittent aortic cross clamping—myocardial revascularisation: single center expirience. Coll Antropol. 2008;32(2):381–4. [PubMed] [Google Scholar]
- 21.Fortuna D, Nicolini F, Guastaroba P, De Palma R, Di Bartolomeo S, Saia F, et al. Coronary artery bypass grafting vs percutaneous coronary intervention in a 'real-world' setting: a comparative effectiveness study based on propensity score-matched cohorts. Eur J Cardiothorac Surg. 2013;44(1):e16–24. 10.1093/ejcts/ezt197 [DOI] [PubMed] [Google Scholar]
- 22.Paunel-Gorgulu A, Wacker M, El Aita M, Hassan S, Schlachtenberger G, Deppe A, et al. cfDNA correlates with endothelial damage after cardiac surgery with prolonged cardiopulmonary bypass and amplifies NETosis in an intracellular TLR9-independent manner. Sci Rep. 2017;7(1):17421 10.1038/s41598-017-17561-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Merkle J, Daka A, Deppe AC, Wahlers T, Paunel-Gorgulu A. High levels of cell-free DNA accurately predict late acute kidney injury in patients after cardiac surgery. PLoS One. 2019;14(6):e0218548 10.1371/journal.pone.0218548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Caputo M, Mokhtari A, Miceli A, Ghorbel MT, Angelini GD, Parry AJ, et al. Controlled reoxygenation during cardiopulmonary bypass decreases markers of organ damage, inflammation, and oxidative stress in single-ventricle patients undergoing pediatric heart surgery. J Thorac Cardiovasc Surg. 2014;148(3):792–801 e8; discussion 0–1. 10.1016/j.jtcvs.2014.06.001 [DOI] [PubMed] [Google Scholar]
- 25.Li Z, Fan G, Zheng X, Gong X, Chen T, Liu X, et al. Risk factors and clinical significance of acute kidney injury after on-pump or off-pump coronary artery bypass grafting: a propensity score-matched study. Interact Cardiovasc Thorac Surg. 2019;28(6):893–9. 10.1093/icvts/ivy353 [DOI] [PubMed] [Google Scholar]
- 26.Sander M, von Heymann C, von Dossow V, Spaethe C, Konertz WF, Jain U, et al. Increased interleukin-6 after cardiac surgery predicts infection. Anesth Analg. 2006;102(6):1623–9. 10.1213/01.ane.0000215998.21739.48 [DOI] [PubMed] [Google Scholar]
- 27.Amini S, Najafi MN, Karrari SP, Mashhadi ME, Mirzaei S, Tashnizi MA, et al. Risk Factors and Outcome of Acute Kidney Injury after Isolated CABG Surgery: a Prospective Cohort Study. Braz J Cardiovasc Surg. 2019;34(1):70–5. 10.21470/1678-9741-2017-0209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Puskas JD, Kilgo PD, Lattouf OM, Thourani VH, Cooper WA, Vassiliades TA, et al. Off-pump coronary bypass provides reduced mortality and morbidity and equivalent 10-year survival. Ann Thorac Surg. 2008;86(4):1139–46; discussion 46. 10.1016/j.athoracsur.2008.05.073 [DOI] [PubMed] [Google Scholar]
- 29.Chu D, Bakaeen FG, Dao TK, LeMaire SA, Coselli JS, Huh J. On-pump versus off-pump coronary artery bypass grafting in a cohort of 63,000 patients. Ann Thorac Surg. 2009;87(6):1820–6; discussion 6–7. 10.1016/j.athoracsur.2009.03.052 [DOI] [PubMed] [Google Scholar]
- 30.Bucerius J, Gummert JF, Walther T, Borger MA, Doll N, Falk V, et al. Impact of off-pump coronary bypass grafting on the prevalence of adverse perioperative outcome in women undergoing coronary artery bypass grafting surgery. Ann Thorac Surg. 2005;79(3):807–12; discussion 12–3. 10.1016/j.athoracsur.2004.06.013 [DOI] [PubMed] [Google Scholar]
- 31.Li XH, Xiao F, Zhang SY. [Investigation of risk factors of acute kidney injury after off-pump coronary artery bypass grafting and 3 years' follow-up]. Beijing Da Xue Xue Bao Yi Xue Ban. 2017;49(1):131–6. [PubMed] [Google Scholar]
- 32.Singh RS, Thingnam SKS, Mishra AK, Verma I, Kumar V. Renal function after off-pump versus on-pump coronary artery bypass grafting. Asian Cardiovasc Thorac Ann. 2017;25(7–8):504–8. 10.1177/0218492317730256 [DOI] [PubMed] [Google Scholar]
- 33.Park J, Lee JH, Kim KA, Lee SH, Lee YT, Kim WS, et al. Effects of Preoperative Statin on Acute Kidney Injury After Off-Pump Coronary Artery Bypass Grafting. J Am Heart Assoc. 2019;8(7):e010892 10.1161/JAHA.118.010892 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(SAV)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.


