Abstract
The cyberspace plays an important role in improving the quality, equity, and efficiency of health services. Studying people's adoption of online health services, such as online health consultation services (OHCS) can benefit both industry and policy in the health service sector. This paper investigates influencing factors and paths of people's intention of adopting OHCS by employing the extended valence framework, with our new contribution of integrating subjective norm and offline habit into the model. Five hundred forty-three university students participated in the survey. Structural equation models and Sobel-Goodman tests were applied to test the models. The results show that subjective norm (β = 0.077, p = 0.041), trust in providers (β = 0.194, p = 0.002) and perceived benefit (β = 0.463, p < 0.001) positively affect the intention to adopt OHCS, while offline habit (β = −0.111, p = 0.026) has a negative effect. However, the association of perceived risk (β = −0.062, p = 0.315) and adoption is not supported. Moreover, trust in providers plays a mediating role between subjective norm and the intention of adopting, while perceived benefit mediates the relationship between trust in providers and the intention of adopting. This study highlights the importance of trust, subjective norm, perceived benefit, and persisting habits in promoting the adoption of OHCS.
Keywords: online health consultation service, adoption, subjective norm, habit, extended valence framework
Introduction
Information and communication technologies (ICTs) have been widely used to support and to deliver health services recently (1) because ICTs' products [e.g., health information systems (HIS)] can improve the quality, efficiency, and equity of health care services delivery (2). For example, online health services (OHS), as one health information system, comprise online health consultation services (OHCS), information seeking services, and online health forums. OHS can provide health services to anyone with medical demands online at any time (3) and can overcome geographic constraints to provide services for users far away from health institutions (4). Thus, OHS has been deemed as an extension of traditional offline health services (3). With the characteristics of vast territory and inequality of socioeconomic development in China, OHS has been proposed by the Chinese government as an important option of improving the equity and efficiency of health services in China (5, 6). Meanwhile, the OHS industry is emerging and companies, such as “Hao Daifu Zaixian,” “Clove Doctor,” or “Chun Yu Doctor,” have been started, widely advertised, and being noted by the public.
Nevertheless, the public's adoption of OHS is still relatively low in China as compared with more developed countries (7). For example, the 39th Statistical Report on the Development of Chinese Internet Network showed that only 10.8% of Chinese Internet users sought health information online in 2016 (8). In comparison, 72% of U.S. adults who use the internet had searched online for health information in 2012 (9). Furthermore, a study found that less than only one percent of the visitors of the famous Chinese OHS company called “Hao Daifu Zaixian” consulted with doctors online (3). Obviously, there are still shortcomings in Chinese OHS, especially in OHCS. OHCS can provide a new channel to promote the public to obtain more diagnostic information and manage themselves and their families' health, and thereby improve the quality of health care. Meanwhile, growth in OHCS usage can further strengthen the development of the OHS industry. However, the low usage rates of OHCS may make it difficult to exert a significant effect on health services. Therefore, understanding the reasons for such low usage rate will be useful for service providers in formulating strategies aimed at increasing OHCS adoption.
OHS research papers account only for a small proportion of HIS research, based on our literature research in PubMed and Web of Science. Most of the existing literature on HIS focuses on the implementation of HIS, such as Clinical Information System, Computerized Physician Order Entry System, Electronic Health Records or Electronic Medical Record, in health institutions. For example, the determinants of adoption of these HIS haven been examined from the perspective of physicians (10, 11), nurses (2, 12), and medical institutions (13, 14). Some other studies explored how to design a HIS (15, 16) or evaluated the implementation of a HIS (17, 18).
Furthermore, among the OHS literature, research on individuals' adoption of OHCS is very limited. Although some studies have examined the factors that influence consumers to adopt OHS, most of them explored the issue of health information seeking. Trust, perceived risk, perceived usefulness, and perceived health condition are common factors that were found to influence consumers' information seeking behaviors in these studies (4, 19, 20). However, information seeking and online consultations are two related but different behaviors because information seeking is usually unilateral, but online consultation involves interaction between consumers and doctors. Indeed, several articles explored behaviors toward a non-specific comprehensive OHS, which included information seeking, online registration, online consultation, and patient education rather than the information seeking alone (3, 7, 21). No studies that solely concentrated on OHCS were identified in our literature reviews, and thus we developed the present study to contribute to closing this gap.
This study focuses on the adoption of OHCS from the perspective of the decision-making process. OHS is the application of e-commerce in the healthcare context (7), so the adoption of OHCS, as a part of OHS usage, can be considered as an e-commerce behavior. Previous studies have found that perceived benefit and risk, as well as trust are important determinants in consumers' decision-making process of purchase and adoption of online services (19, 22–25). Hence, the extended valence framework (26) including benefit perception, risk perception, and trust was adopted to guide this research. Moreover, using OHCS involves changes in habits of receiving offline medical services (3), and subjective norms are also essential for behavioral change of consumers (27). We this integrated subjective norm and offline habit in the extended valence framework. In short, this paper explores motivational and inhibiting factors of OHCS adoption to improve our current understanding of consumers' decision-making processes regarding OHCS.
Theoretical Foundation and Hypotheses
The Extended Valence Framework
The theoretical foundation of this study is the extended valence framework. The valence framework is a well-established theory deriving from economic and psychological theories in behavioral research (28, 29). Perceived risk and benefit are the two foundational aspects regarding consumers' decision-making and consumers tend to maximize the positive value (perceived benefit) and minimize the negative impacts (perceived risk) of a product or service when they make decision of purchasing it according to the valence framework (30, 31). The valence framework performs well in understanding individual's behavior because by considering both negative and positive attributes in decision-making simultaneously (32).
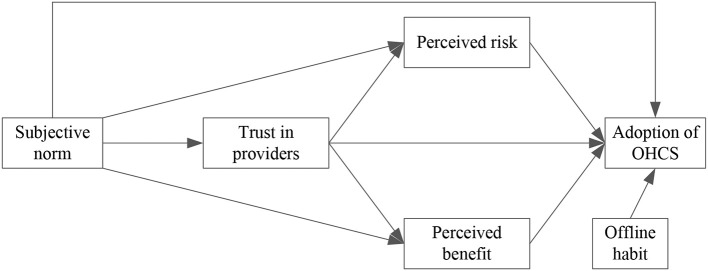
Kim developed the extended valence framework by integrating trust into the valence framework (26). The extended valence framework states that trust, perceived risk and perceived benefit directly affect consumers' purchase intention in one way, and in an indirect way, trust influences the purchase intention through perceived risk and perceived benefit (Figure 1). The extended valence framework has been applied in studies regarding e-commerce, and has been considered a useful and valid theoretical framework to guide our understanding of people's behaviors in the e-commerce context (33), including online health information seeking behavior (4). Moreover, a benefit-risk evaluation may help strategy-planners to make more updated, informed, and effective management decisions (34). Therefore, the extended valence framework is adopted in this paper to promote the understanding of the individual's adoption of OHCS.
Figure 1.
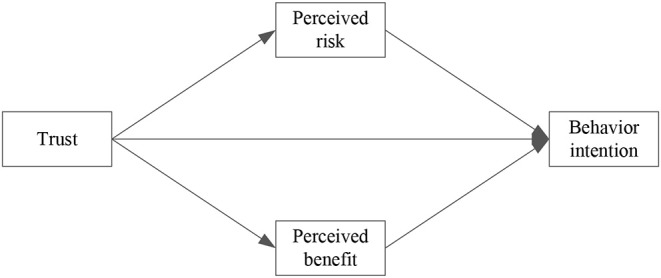
Extended valence framework.
Hypotheses
Perceived Risk
Perceived risk is considered as a salient inhibitor of the adoption of online services, because individuals may experience certain levels of risk due to the uncertainty and uncontrollability of the cyberspace (26). Perceived risk is a multifaceted concept (24) and varies according to types of products or services (35). In the context of this study, perceived risk refers to privacy and security risk concerns. Privacy and security risk involves the collection, use, and disclosure of personal information (36), as well as uncertain consequences of actions based on information and guidance provided by an online doctor (37). Health information technology may aggravate individuals' privacy concerns over the potential misuse of personal health information (38). Empirical findings have shown that there is a negative association between online privacy and security concerns and the use of online health services (21, 39). Thus, we hypothesize:
H1. Perceived risk has a negative effect on the adoption of OHCS.
Perceived Benefit
Perceived benefit is defined as a consumer's belief about the extent to which he/she will become better off through the use of certain online service (31). Evidence from prior studies has shown that perceived benefit exerted a positive and significant effect on customers' behavioral intention (23, 38, 40). OHCS as one of many internet-based services which may bring about potential benefits for consumers, such as cost and time saving (41), which have been identified as relative benefits as compared with traditional offline services (28). Accordingly, if an individual perceived a higher degree of benefits, he/she would be more likely to adopt OHCS. Thus, we hypothesize:
H2. Perceived benefit has a positive effect on the adoption of OHCS.
Trust
Trust either can be defined as one's willingness to rely upon another (42), or as the belief in dependability and honesty (43). In this study, trust refers to the trust in OHCS providers which include both online platform and online doctors. Furthermore, trust in OHCS providers is defined as the individual's confidence in the provider's integrity and dependability (44), and the belief that OHCS providers have attributes that are beneficial to consumers (37). Individuals' trust is considered as one of the most important psychological factors influencing online behaviors (31). Prior studies found that there is a positive association between trust and behavioral intention (22, 26). It's likely that people with a higher degree of trust feel less uncertainty and believe that the service will improve their effectiveness in managing their health (4). Thus, trust can influence consumers' purchase decision making both directly and indirectly through perceived benefits and risks, i.e., trust can have a positive impact on perceived benefits and a negative influence on perceived risks. In sum, trust influences consumers' intention of purchasing in e-commerce both directly and indirectly through perceived risks and benefits (26). Thus, we hypothesize:
H3. Trust in providers has a positive effect on the adoption of OHCS.
H4. Trust in providers has a negative effect on the risk perception of OHCS.
H5. Trust in providers has a positive effect on the benefit perception of OHCS.
Subjective Norm
Subjective norm refers to how an individual thinks he/she should behave and how their behavior would be judged by others in a specific cultural and social environment (45). According to the Theory of Reasoned Action, individual's intention of performing a given behavior is influenced by normative beliefs—the views (whether the individual agrees or not) regarding one behavior developed by important others, such as peers, friends or relatives (46, 47). Thus, people may shape their behavioral intentions based on how they believe significant others will view their behaviors. Previous studies have found that subjective norm affects online health-related behavioral intention positively (19, 48). Therefore, we hypothesize:
H6. Subjective norm has a positive effect on the adoption of OHCS.
In the current study, the subjective norm is also considered to be a determinant of trust, perceived benefit, and perceived risk. Li et al. (49) found that when people do not know a system well, they may rely on the opinions of others significant to them, and then develop trust belief toward the system accordingly (49). Moreover, prior research found that subjective norm directly affects trust (50, 51). Regarding the perceived benefit and perceived risk, few studies in the online health context have simultaneously incorporated the association between subjective norm and perceived benefit, and the association between subjective norm and perceived risk. However, it has been found in other information systems related research that subjective norm influences perceived usefulness positively (52, 53) and motivates users to reveal personal information (54). In other words, subjective norm, to a certain extent, can enhance individual perception of benefits and reduce the risk perception of private information. Therefore, we hypothesize:
H7. Subjective norm has a positive effect on trust in providers.
H8. Subjective norm has a positive effect on perceived benefit.
H9. Subjective norm has a negative effect on perceived risk.
Offline Habit
Habits can shape human's decision process, and are considered as a critical factor influencing people's behavior in the e-commerce context (55). A habit is an individual's repeated, unconscious and automatic behavior (56). Studies have shown that habits may keep individual from switching to new technologies (57). Thus, people's habits of using offline service channels may have a negative effect on their intention to switch to the online service channel (28). Regarding health services, if an individual is used to visiting doctors in hospitals (offline channel), she/he would be more willing to continue to use the offline channel rather than switching to online services. Therefore, we hypothesize:
H10. Offline habit has a negative effect on the adoption of OHCS.
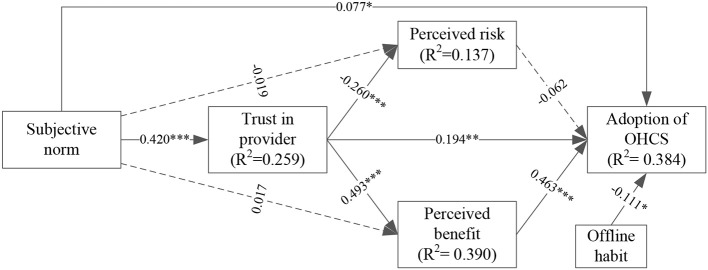
Based on the hypotheses mentioned above, we propose our research model as depicted in Figure 2.
Figure 2.
Research model.
Methods
Participants and Procedures
The participants were university students, which were sampled by convenience. University students represent a large proportion of active online consumers (31), and the younger generation is the most active population participating in online transactions (58). Moreover, students younger than 30 years are the largest group of internet users, representing the majority of Internet users in China (28). Moreover, prior e-service documents including research on OHS also sampled from student populations (19, 28). Here, students from two universities in China were surveyed. We designed a web-based questionnaire, and linkage of the questionnaire was delivered to both undergraduate and graduate students via social network applications (WeChat and QQ). The questionnaire contained instructions and an explanation of the study but did not collect any information that would have made the person identifiable. The participation of each student was completely voluntary, and they could withdraw from the study at any stage. Eventually, 543 valid questionnaires were collected.
Measurements
The adoption of OHCS (AO) was assessed by three items adapted from an instrument created by Venkatesh et al. (59). Similarly, subjective norm (SN) also included three items adapted from Venkatesh et al. (60). Trust in providers (TP) was measured by seven items (four items adapted from Cater and Bélanger (61) and Mou et al. (4) and three self-constructed items). Perceived risk (PR) was assessed by five items adapted from McKnight et al. (62) and Yi et al. (37). Perceived benefit (PB) was measured by six items including four items adapted from Mou et al. (4) and Zhang et al. (7) and two self-developed items. Offline habit (OH) was measured with four items which were adapted from Zhang et al. (7). The items are listed in Table 1. All items were assessed using five-point Likert scales ranging from strongly disagree (1) to strongly agree (5).
Table 1.
Measurement items, factor loading, and characteristics of variables.
| Variables | Items | FL | Mean (SD) | Range |
|---|---|---|---|---|
| Subjective norm | SN1: People who influence my behavior (would think/think) that I should use the OHCS. | 0.875 | 8.39 (2.42) | 3–15 |
| SN2: People who are important to me (would think/think) that I should use the OHCS. | 0.896 | |||
| SN3: People who are in my social circle (would think/think) that I should use the OHCS. | 0.880 | |||
| Trust in providers | TP1: I would characterize OHCS providers as honest. | 0.670 | 22.24 (3.98) | 7–35 |
| TP2: I believe that the health service provided by OHCS platform is useful. | 0.600 | |||
| TP3: The OHCS platform performs its role as health service providers very well. | 0.597 | |||
| TP4: I have confidence in relying on OHCS platforms to complete a health consultation or diagnosis. | 0.681 | |||
| TP5: Doctors on the OHCS platform have medical qualifications. | 0.794 | |||
| TP6: The consultation or diagnosis provided by doctors on OHCS platforms is reliable | 0.769 | |||
| TP7: In my opinion, doctors on the OHCS platform are trustworthy. | 0.806 | |||
| Perceived risk | PR1: Providing personal health information online is unsafe. | 0.576 | 18.36 (3.14) | 5–25 |
| PR2: I think it is risky to provide personal information to OHCS providers. | 0.808 | |||
| PR3: I think it is risky to provide personal health information to doctors on OHCS platforms. | 0.797 | |||
| PR4: I would hesitate to provide my personal information (such as name, address, health condition, bank information, and phone number, etc.) to OHCS platforms. | 0.719 | |||
| PR5: I think it is risky to make a decision (such as taking medicine, controlling diet, etc.) based on the diagnosis provided by the doctors on the OHCS platform. | 0.631 | |||
| Perceived benefit | PB1: Using OHCS can be of benefit to me in managing my health. | 0.793 | 21.35 3.76) | 6–30 |
| PB2: Using OHCS can increase my knowledge of my personal health conditions. | 0.804 | |||
| PB3: Using OHCS can help to relieve stresses about my symptoms or my worries about symptoms. | 0.691 | |||
| PB4: Using OHCS will be useful for my health. | 0.766 | |||
| PB5: Compared with going to the hospital, using OHCS can save time. | 0.706 | |||
| PB6: Compared with going to the hospital, using OHCS can save medical expenses. | 0.666 | |||
| Offline habit | OH1: Whenever I need to see a doctor or have a health consultation, I will choose to go to hospitals or clinics without even being aware of making another choice. | 0.737 | 15.77 (2.50) | 4–20 |
| OH2: Whenever I need to see a doctor or have a health consultation, I unconsciously start going to hospitals or clinics. | 0.879 | |||
| OH3: Choosing to go to hospitals or clinics when I need to see a doctor or have a health consultation is something I do unconsciously. | 0.844 | |||
| OH4: In general, I am accustomed to taking the offline channel (going to hospitals or clinics) for medical treatment or health consultation. | 0.828 | |||
| Adoption of OHCS | AO1: I intend to use OHCS to consult health issues when needed in the future. | 0.811 | 10.27 (2.01) | 3–15 |
| AO2: I predict that I will use OHCS to consult health issues when needed in the future. | 0.862 | |||
| AO3: I plan to use OHCS to consult health issues when needed in the future. | 0.845 |
FL, factor loading; SD, standard deviation.
Statistical Analysis
Before hypotheses testing, we first evaluated the measurement model including composite reliability, convergent validity, and discriminant validity. Then, structural equation modeling (SEM) was conducted to test the hypotheses. Goodness-of-fit indices and the path coefficients with p-values were reported. Based on recommendations of Wang and Lai (63), the ratio of Chi-square values (χ2) to the degrees of freedom (χ2/df) should be <3. The values of the Tucker-Lewis fit index (TLI), comparative fit index (CFI), goodness-of-fit index (GFI), and normalized fit index (NFI) should be higher than 0.9, while root-mean-square residual (RMR) and root-mean-square-error of approximation (RMSEA) should be <0.8. Besides, we conducted a mediation analysis to further examine mediating effects. Sobel-Goodman tests were applied to test the presence of mediation. Amos 21.0 was used for the SEM, and Stata/MP 14.0 was used for all other analyzes.
Result
Descriptive Results
Among the 543 qualified respondents, 64.27% were female; 45.12% were graduate students, and 30.94% were specialized in Medicine. Detailed results are shown in Table 2. Mean values (standard deviations) of AO (adoption of online health consultation service), SN (subjective norm), TP (trust in providers), PR (perceived risk), PB (perceived benefit), and OH (offline habit) were 10.27 (2.01), 8.39 (2.42), 22.24 (3.98), 18.36 (3.14), 21.35 (3.76), and 15.77 (2.50), respectively (Table 1).
Table 2.
Characteristic of respondents.
| Items | Frequency | Percent (%) | |
|---|---|---|---|
| Gender | Female | 349 | 64.27 |
| Male | 194 | 35.73 | |
| Being a graduate student | No | 298 | 54.88 |
| Yes | 245 | 45.12 | |
| Major | Medicine | 168 | 30.94 |
| Else | 375 | 69.06 | |
| Experience of obtaining health information online | No | 189 | 34.81 |
| Yes | 354 | 65.19 | |
| Expense | <1,000 | 100 | 18.42 |
| 1,000–2,000 | 361 | 66.48 | |
| 2,001–3,000 | 55 | 10.13 | |
| More than 3,000 | 27 | 4.97 | |
| Health condition (Frequency of seeing a doctor) | Never | 18 | 3.31 |
| Rarely | 205 | 37.75 | |
| Sometimes | 224 | 41.25 | |
| Usually | 96 | 17.68 | |
Measurement Model Evaluation
The measurement model aims to assess reliability and validity. We used Cronbach's alpha (CA) and composite reliability (CR) to evaluate the construct reliability. The results of all CA test ranged from 0.788 to 0.914, and CR values ranged from 0.835 to 0.915 (Table 3). Since both CA and CR for each construct were higher than the minimum cutoff value of 0.7 (64), construct reliability was supported.
Table 3.
Validity and reliability of variables.
| CA | CR | AVE | SN | TP | PR | PB | OH | AO | |
|---|---|---|---|---|---|---|---|---|---|
| SN | 0.914 | 0.915 | 0.781 | 0.884 | |||||
| TP | 0.907 | 0.874 | 0.500 | 0.467 | 0.707 | ||||
| PR | 0.788 | 0.835 | 0.507 | −0.190 | −0.318 | 0.712 | |||
| PB | 0.887 | 0.878 | 0.547 | 0.326 | 0.620 | −0.170 | 0.740 | ||
| OH | 0.847 | 0.894 | 0.678 | −0.149 | −0.073 | 0.314 | 0.024 | 0.823 | |
| AO | 0.886 | 0.878 | 0.705 | 0.331 | 0.500 | −0.207 | 0.501 | −0.131 | 0.840 |
CA, Cronbach's alpha; CR, composite reliability; AVE, average variance extracted. The bold diagonally are the square root of AVE.
Concerning validity, we assessed both convergent validity and discriminant validity. Convergent validity was assessed by factor loadings and average variance extracted (AVE). The factor loadings and AVE of all constructs were higher than the suggested value of 0.5 (65), indicating a good convergent validity. Additionally, the square root of AVE for each construct was higher than its correlation coefficient with any other construct. Therefore, discriminant validity was acceptable.
Structural Model Evaluation
We first tested the fitness index of the structural model. The result showed that the structural model had a good fit (χ2 = 802.096, χ2/df = 2.416, RMR = 0.040, RMSEA = 0.051, GFI = 0.901, NFI = 0.916, TLI = 0.942, CFI = 0.945). Results of hypotheses testing and the SEM are shown in Table 4 and Figure 3, respectively. Perceived benefit (β = 0.463, p < 0.001) significantly and positively influenced the adoption of OHCS, while the effect of perceived risk (p = 0.315) on the adoption of OHCS was not statistically significant. Trust in providers significantly and positively affected the adoption of OHCS (β = 0.194, p = 0.002) and perceived benefit (β = 0.493, p < 0.001), but negatively affected perceived risk (β = −0.260, p < 0.001). Subjective norm was positively correlated with the adoption of OHCS (β = 0.077, p = 0.041) and trust in providers (β = 0.420, p < 0.001). Nevertheless, none of its effects on perceived benefit (p = 0.593) or on the perceived risk (p = 0.570) was statistically significant. Moreover, offline habit (β = −0.111, p = 0.026) affected the adoption of OHCS negatively. In sum, perceived benefit, trust in providers, subjective norm and offline habit had a significant direct effect on the adoption of OHCS, and the structural model could explain 38.4% of the variation in OHCS adoption (R2 = 0.384).
Table 4.
Path coefficients and the result of hypotheses test.
| Hypotheses | Path coefficients | Sig. | Findings |
|---|---|---|---|
| H1: PR→AO | −0.062 | P = 0.315 | Not supported |
| H2: PB→AO | 0.463 | P < 0.001 | Supported |
| H3: TP→AO | 0.194 | P = 0.002 | Supported |
| H4: TP→PR | −0.260 | P < 0.001 | Supported |
| H5: TP→PB | 0.493 | P < 0.001 | Supported |
| H6: SN→AO | 0.077 | P = 0.041 | Supported |
| H7: SN→TP | 0.420 | P < 0.001 | Supported |
| H8: SN→PB | 0.017 | P = 0.593 | Not supported |
| H9: SN→PR | −0.019 | P = 0.570 | Not supported |
| H10: OH→AO | −0.111 | P = 0.026 | Supported |
Figure 3.
The structural model and R2 values. dashed lines represent unsupported paths. *p < 0.05, **p < 0.01, ***p < 0.001.
Post-hoc Analysis
Based on the result of the structural model, we further conducted a post-hoc analysis to test the mediating effect of trust in providers in the relation between subjective norm and the adoption of OHCS, and to test the mediating effect of perceived benefit in the relation between trust in providers and the adoption of OHCS. We confirmed a significant indirect effect of the subjective norm (β = 0.172, p < 0.001) on adoption through trust in providers, which accounted for 61.6% of the total effect that subjective norm had on adoption (Table 5). Moreover, a significant indirect effect of trust in providers (β = 0.093, p < 0.001) on adoption through perceived benefit was also confirmed, accounting for 36.9% of the total effect.
Table 5.
Mediation result.
| B | S.E. | Sobel z (% of total effect) | ||
|---|---|---|---|---|
| Mediation of TP | Direct effect | |||
| SN | 0.107** | 0.035 | ||
| TP | 0.221*** | 0.021 | ||
| Indirect effect | 7.961 (61.6%) | |||
| SN on AO through TP | 0.172*** | 0.022 | ||
| Mediation of PB | Direct effect | |||
| TP | 0.159*** | 0.023 | ||
| PB | 0.159*** | 0.025 | ||
| Indirect effect | 6.078 (36.9%) | |||
| TP on AO through PB | 0.093*** | 0.015 |
Gender, major, being a graduate student, experience of obtaining health information online, monthly expense and health condition were included in the analysis but not reported in this table.
p < 0.01,
p < 0.001.
Discussion
This study enriches the extended valence framework by integrating subjective norm and offline habit into the extended valence framework in order to investigate the facilitators and barriers of OHCS adoption. To the best of our knowledge, this is the first study about people's decision-making regarding the adoption of OHCS in China. Our results show that trust in providers, perceived benefit, subjective norm, and offline habit significantly affect the adoption of OHCS, while the impact of perceived risk on adoption is not supported. 38.4% variation of the adoption of OHCS is explained by our proposed model, and there are four important findings.
First, the extended valence framework can partly interpret the adoption of OHCS. Perceived benefit, as expected, influences the adoption of OHCS positively—students with a higher degree of perceived benefit are more likely to adopt the OHCS. Also, consistent with existing literature (4, 19), trust in providers has a positive effect on the adoption of OHCS. Moreover, such positive effect is partly mediated by perceived benefit. Therefore, both perceived benefit and trust in providers are critical determinants of OHCS usage.
However, the association between perceived risk and the adoption of OHCS is not significant in this study. Prior studies on OHS have found that perceived risk had a negative effect on behavioral intention toward using health service (7, 39). One possible reason is that online health consultation behavior is different from other OHS behaviors (e.g., health information seeking). Investigations in South Africa and China found that perceived risk plays a role in dampening people's online health information acceptance behavior (4) or intention to use comprehensive OHS (7). The inconsistent results indicate that there is a need to conduct more research specifically focused on OHCS. Another possible explanation could be that the respondents are university students, who have a strong perception of control in online behavior. This makes them believe that they can identify potential risks and avoid risky behavior when they adopt OHCS.
This study confirms a positive associations between subjective norm and the intention of using OHCS, which is consistent with previous findings related to e-services (e.g., e-banking) (27, 66). Compared with other studies that only analyzed the direct relationship between subjective norm and intention of adoption (48, 67), we further found that trust in providers mediated the association of subjective norm and OHCS adoption. In other words, subjective norm directly influences OHCS adoption, but also influences trust in providers first, and then influences OHCS adoption indirectly through trust in providers. Obviously, both direct and indirect effect of subjective norm on the adoption of OHCS show that subjective norm must be taken into account when promoting and implementing OHCS. Unfortunately, associations of subjective norm with perceived benefit and perceived risk are not supported, and such associations deserve to be further explored.
Offline habit is the only negative factor that influences the adoption of OHCS. Habit is considered as an automatic behavioral process, which makes individuals do not evaluate the benefit and cost of their ongoing behavior (68). Hence, habitual behavior causes a lack of motivation to change ongoing behavior (7). Individuals who are used to offline health services were reluctant to transfer to OHS (28). This indicates that the low usage rate of OHCS in China may be due to people's habit of accessing medical services offline. Despite the rapid development of information and communication technology, traditional offline channels (going to hospitals or clinics for medical services) are still the first choice for people to see a doctor. Therefore, OHCS providers should take positive strategies to encourage potential consumers to adopt online services and eliminate the adverse effects of offline habits gradually (28), e.g., by enhancing individual eHealth literacy through educational programs (1).
This study has some limitations. First, the measurement of perceived risk only consisted of privacy and security concerns, while online risk should contain more facets. This implies that H1 can only reflect the non-significant association of privacy and security risk with the adoption of OHCS. Second, the respondents of the present study were only university students, and generalizations to other potential OHCS consumer groups cannot be made. Thus, studies with more representative samples should be conducted in the future. Third, this study studied behavioral intention rather than actual behavior regarding OHCS adoption. It may thus suffer from information bias, since intention and behavior are closely related but not necessarily equivalent.
Conclusion
This study explored factors influencing of the adoption of OHCS by integrating offline habit and subjective norm into the extended valence framework. Subjective norm, trust in providers and perceived benefit were found to play promoting roles regarding individuals' OHCS adoption behavior, while habit had an inhibitory effect. The habit of using offline channels to obtain health services can play an important role in explaining low usage rate of OHCS in China. To promote the adoption of OHCS, the negative effect of offline habit should be considered besides the strengthening of trust, subjective norms and perceived benefits.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Author Contributions
ZG, ZH, XL, CY, and JR have made a direct, intellectual contribution to this study. ZG and ZH designed and wrote most part of the paper and conducted the data analysis. XL, CY, and JR were major contributors of data collection and paper revision. All authors have read and approved the final version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We want to express our acknowledgment to students who finished the questionnaires.
Footnotes
Funding. This is an investigator-initiated study, and no grant funding is obtained.
References
- 1.Kim H, Xie B. Health literacy in the eHealth era: a systematic review of the literature. Patient Educ Couns. (2017) 100:1073–82. 10.1016/j.pec.2017.01.015 [DOI] [PubMed] [Google Scholar]
- 2.Hung S-Y, Tsai JC-A, Chuang C-C. Investigating primary health care nurses' intention to use information technology: an empirical study in Taiwan. Decis Support Syst. (2014) 57:331–42. 10.1016/j.dss.2013.09.016 [DOI] [Google Scholar]
- 3.Zhang X, Guo X, Lai K, Yin C, Meng F. From offline healthcare to online health services: the role of offline healthcare satisfaction and habits. J Electron Commer Res. (2017) 18:138–54. Available online at: http://www.jecr.org/sites/default/files/2017vol18no2_Paper3.pdf [Google Scholar]
- 4.Mou J, Shin D-H, Cohen J. Health beliefs and the valence framework in health information seeking behaviors. Info Technol People. (2016) 29:876–900. 10.1108/ITP-06-2015-0140 [DOI] [Google Scholar]
- 5.State Council of the People's Republic of China Guidance on Promoting the “Internet +” Initiative. (2015) Available online at: http://www.gov.cn/zhengce/content/2015-07/04/content_10002.htm (accessed January 13, 2019)
- 6.Genenal Office of the State Council of the People's Republic of China Opinions on Promoting the Development of “Internet + Medical Health”. (2018) Available online at: http://www.gov.cn/zhengce/content/2018-04/28/content_5286645.htm (accessed January 13, 2019)
- 7.Zhang X, Guo X, Wu Y, Lai K, Vogel D. Exploring the inhibitors of online health service use intention: a status quo bias perspective. Inf Manage. (2017) 54:987–97. 10.1016/j.im.2017.02.001 [DOI] [Google Scholar]
- 8.China Internet Network Information Center The 39th Statistical Report on the Development of Chinese Internet Network. (2017) Available online at: http://www.cac.gov.cn/cnnic39/ (accessed January 13, 2019)
- 9.Fox S, Duggan M. Health Online 2013 | Pew Research Center. (2013) Available online at: http://www.pewinternet.org/2013/01/15/health-online-2013/ (accessed January 13, 2019)
- 10.Kaipio J, Lääveri T, Hyppönen H, Vainiomäki S, Reponen J, Kushniruk A, et al. Usability problems do not heal by themselves: National survey on physicians' experiences with EHRs in Finland. Int J Med Inform. (2017) 97:266–81. 10.1016/j.ijmedinf.2016.10.010 [DOI] [PubMed] [Google Scholar]
- 11.Sidek YH, Martins JT. Perceived critical success factors of electronic health record system implementation in a dental clinic context: an organisational management perspective. Int J Med Inform. (2017) 107:88–100. 10.1016/j.ijmedinf.2017.08.007 [DOI] [PubMed] [Google Scholar]
- 12.Alquraini H, Alhashem AM, Shah MA, Chowdhury RI. Factors influencing nurses' attitudes towards the use of computerized health information systems in Kuwaiti hospitals. J Adv Nursing. (2007) 57:375–81. 10.1111/j.1365-2648.2007.04113.x [DOI] [PubMed] [Google Scholar]
- 13.Wang BB, Wan TTH, Burke DE, Bazzoli GJ, Lin BYJ. Factors influencing health information system adoption in American hospitals. Health Care Manage Rev. (2005) 30:44–51. 10.1097/00004010-200501000-00007 [DOI] [PubMed] [Google Scholar]
- 14.Yoshida Y, Imai T, Ohe K. The trends in EMR and CPOE adoption in Japan under the national strategy. Int J Med Inform. (2013) 82:1004–11. 10.1016/j.ijmedinf.2013.07.004 [DOI] [PubMed] [Google Scholar]
- 15.Urda D, Ribelles N, Subirats JL, Franco L, Alba E, Jerez JM. Addressing critical issues in the development of an oncology information system. Int J Med Inform. (2013) 82:398–407. 10.1016/j.ijmedinf.2012.08.001 [DOI] [PubMed] [Google Scholar]
- 16.Batley NJ, Osman HO, Kazzi AA, Musallam KM. Implementation of an emergency department computer system: design features that users value. J Emerg Med. (2011) 41:693–700. 10.1016/j.jemermed.2010.05.014 [DOI] [PubMed] [Google Scholar]
- 17.Yusof MM, Kuljis J, Papazafeiropoulou A, Stergioulas LK. An evaluation framework for health information systems: human, organization and technology-fit factors (HOT-fit). Int J Med Inform. (2008) 77:386–98. 10.1016/j.ijmedinf.2007.08.011 [DOI] [PubMed] [Google Scholar]
- 18.Petter S, Fruhling A. Evaluating the success of an emergency response medical information system. Int J Med Inform. (2011) 80:480–9. 10.1016/j.ijmedinf.2011.03.010 [DOI] [PubMed] [Google Scholar]
- 19.Mou J, Shin D-H, Cohen J. Understanding trust and perceived usefulness in the consumer acceptance of an e-service: a longitudinal investigation. Behav Inf Technol. (2017) 36:125–39. 10.1080/0144929X.2016.1203024 [DOI] [Google Scholar]
- 20.Xiao N, Sharman R, Rao HR, Upadhyaya S. Factors influencing online health information search: an empirical analysis of a national cancer-related survey. Decis Support Syst. (2014) 57:417–27. 10.1016/j.dss.2012.10.047 [DOI] [Google Scholar]
- 21.Chang J. Privacy and security concerns in online health services. Appl Econ Lett. (2018) 25:1351–4. 10.1080/13504851.2017.1420878 [DOI] [Google Scholar]
- 22.Gefen D, Karahanna E, Straub DW. Trust and TAM in online shopping: an integrated model. MIS Q. (2003) 27:51–90. 10.2307/30036519 [DOI] [Google Scholar]
- 23.Lee M-C. Factors influencing the adoption of internet banking: an integration of TAM and TPB with perceived risk and perceived benefit. Electron Commer Res Appl. (2009) 8:130–41. 10.1016/j.elerap.2008.11.006 [DOI] [Google Scholar]
- 24.Tai Y-M, Ku Y-C. Will stock investors use mobile stock trading? A benefit-risk assessment based on a modified Utaut model. J Electron Commer Res. (2013) 14:67 Available online at: http://www.jecr.org/sites/default/files/14_01_p5.pdf [Google Scholar]
- 25.Choi J, Lee A, Ok C. The effects of consumers' perceived risk and benefit on attitude and behavioral intention: a study of street food. J Travel Tourism Mark. (2013) 30:222–37. 10.1080/10548408.2013.774916 [DOI] [Google Scholar]
- 26.Kim DJ, Ferrin DL, Rao HR. Trust and satisfaction, two stepping stones for successful E-commerce relationships: a longitudinal exploration. Inf Syst Res. (2009) 20:237–57. 10.1287/isre.1080.0188 [DOI] [Google Scholar]
- 27.Liao C, Chen J-L, Yen DC. Theory of planning behavior (TPB) and customer satisfaction in the continued use of e-service: an integrated model. Comput Hum Behav. (2007) 23:2804–22. 10.1016/j.chb.2006.05.006 [DOI] [Google Scholar]
- 28.Lu Y, Cao Y, Wang B, Yang S. A study on factors that affect users' behavioral intention to transfer usage from the offline to the online channel. Comput Hum Behav. (2011) 27:355–64. 10.1016/j.chb.2010.08.013 [DOI] [Google Scholar]
- 29.Ozturk AB, Bilgihan A, Salehi-Esfahani S, Hua N. Understanding the mobile payment technology acceptance based on valence theory: a case of restaurant transactions. Int J Contemp Hospitality Manage. (2017) 29:2027–49. 10.1108/IJCHM-04-2016-0192 [DOI] [Google Scholar]
- 30.Peter JP, Tarpey LX. A comparative analysis of three consumer decision strategies. J Consum Res. (1975) 2:29–37. 10.1086/208613 [DOI] [Google Scholar]
- 31.Kim DJ, Ferrin DL, Rao HR. A trust-based consumer decision-making model in electronic commerce: the role of trust, perceived risk, and their antecedents. Decis Support Syst. (2008) 44:544–64. 10.1016/j.dss.2007.07.001 [DOI] [Google Scholar]
- 32.Lin J, Wang B, Wang N, Lu Y. Understanding the evolution of consumer trust in mobile commerce: a longitudinal study. Inf Technol Manage. (2014) 15:37–49. 10.1007/s10799-013-0172-y [DOI] [Google Scholar]
- 33.Lee ZWY, Chan TKH, Balaji MS, Chong AY-L. Why people participate in the sharing economy: an empirical investigation of Uber. Internet Res. (2018) 28:829–50. 10.1108/IntR-01-2017-0037 [DOI] [Google Scholar]
- 34.Verhagen H, Tijhuis MJ, Gunnlaugsdóttir H, Kalogeras N, Leino O, Luteijn JM, et al. State of the art in benefit–risk analysis: introduction. Food Chem Toxicol. (2012) 50:2–4. 10.1016/j.fct.2011.06.007 [DOI] [PubMed] [Google Scholar]
- 35.Kaplan L, Szybillo G, Jacoby J. Components of perceived risk in product purchase - cross-validation. J Appl Psychol. (1974) 59:287–91. 10.1037/h0036657 [DOI] [Google Scholar]
- 36.Hall JL, McGraw D. For telehealth to succeed, privacy and security risks must be identified and addressed. Health Aff. (2014) 33:216–21. 10.1377/hlthaff.2013.0997 [DOI] [PubMed] [Google Scholar]
- 37.Yi MY, Yoon JJ, Davis JM, Lee T. Untangling the antecedents of initial trust in web-based health information: the roles of argument quality, source expertise, and user perceptions of information quality and risk. Decis Support Syst. (2013) 55:284–95. 10.1016/j.dss.2013.01.029 [DOI] [Google Scholar]
- 38.Li Y. The impact of disposition to privacy, website reputation and website familiarity on information privacy concerns. Decis Support Syst. (2014) 57:343–54. 10.1016/j.dss.2013.09.018 [DOI] [Google Scholar]
- 39.Li H, Wu J, Gao Y, Shi Y. Examining individuals' adoption of healthcare wearable devices: an empirical study from privacy calculus perspective. Int J Med Inform. (2016) 88:8–17. 10.1016/j.ijmedinf.2015.12.010 [DOI] [PubMed] [Google Scholar]
- 40.Ryu H-S. What makes users willing or hesitant to use Fintech?: the moderating effect of user type. Ind Manage Data Syst. (2018) 118:541–69. 10.1108/IMDS-07-2017-0325 [DOI] [Google Scholar]
- 41.Lee M-C. Predicting and explaining the adoption of online trading: an empirical study in Taiwan. Decis Support Syst. (2009) 47:133–42. 10.1016/j.dss.2009.02.003 [DOI] [Google Scholar]
- 42.Doney PM, Cannon JP, Mullen MR. Understanding the influence of national culture on the development of trust. AMR. (1998) 23:601–20. 10.5465/amr.1998.926629 [DOI] [Google Scholar]
- 43.Kumar N. The Power of Trust in Manufacturer-Retailer Relationships. Harvard Business Review. (1996) Available online at: https://hbr.org/1996/11/the-power-of-trust-in-manufacturer-retailer-relationships (accessed January 21, 2019)
- 44.Bhattacherjee A. Individual trust in online firms: scale development and initial test. J Manage Inf Syst. (2002) 19:211–41. 10.1080/07421222.2002.11045715 [DOI] [Google Scholar]
- 45.Venkatesh V, Morris MG. Why don't men ever stop to ask for directions? Gender, social influence, and their role in technology acceptance and usage behavior. MIS Q. (2000) 24:115–39. 10.2307/3250981 [DOI] [Google Scholar]
- 46.Ajzen I. The theory of planned behavior. Org Behav Hum Decis Processes. (1991) 50:179–211. 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- 47.Fishbein M, Ajzen I. Predicting and Changing Behavior. 1st ed. New York, NY;Hove: Routledge; (2015). [Google Scholar]
- 48.Zhao Y, Ni Q, Zhou R. What factors influence the mobile health service adoption? A meta-analysis and the moderating role of age. Int J Inf Manage. (2018) 43:342–50. 10.1016/j.ijinfomgt.2017.08.006 [DOI] [Google Scholar]
- 49.Li X, Hess TJ, Valacich JS. Why do we trust new technology? A study of initial trust formation with organizational information systems. J Strateg Inf Syst. (2008) 17:39–71. 10.1016/j.jsis.2008.01.001 [DOI] [Google Scholar]
- 50.Wu J-H, Shen W-S, Lin L-M, Greenes RA, Bates DW. Testing the technology acceptance model for evaluating healthcare professionals' intention to use an adverse event reporting system. Int J Qual Health Care. (2008) 20:123–9. 10.1093/intqhc/mzm074 [DOI] [PubMed] [Google Scholar]
- 51.Chaouali W, Ben Yahia I, Souiden N. The interplay of counter-conformity motivation, social influence, and trust in customers' intention to adopt Internet banking services: the case of an emerging country. J Retailing Consum Serv. (2016) 28:209–18. 10.1016/j.jretconser.2015.10.007 [DOI] [Google Scholar]
- 52.Venkatesh V, Davis FD. A Theoretical extension of the technology acceptance model: four longitudinal field studies. Manage Sci. (2000) 46:186–204. 10.1287/mnsc.46.2.186.11926 [DOI] [Google Scholar]
- 53.Watjatrakul B. Intention to use a free voluntary service: the effects of social influence, knowledge and perceptions. J Syst Info Tech. (2013) 15:202–20. 10.1108/13287261311328903 [DOI] [Google Scholar]
- 54.Acquisti A, Gross R. Imagined communities: awareness, information sharing, and privacy on the facebook. In: Danezis G, Golle P, editors. Privacy Enhancing Technologies. Berlin: Springer-Verlag Berlin; (2006). p. 36–58. [Google Scholar]
- 55.Liu C, Liao C, Chuang S, Kuo P, To P. Factors influencing the intended use of web portals. Online Inf Rev. (2011) 35:237–54. 10.1108/14684521111128023 [DOI] [Google Scholar]
- 56.Chuang Y-F. Pull-and-suck effects in Taiwan mobile phone subscribers switching intentions. Telecomm Policy. (2011) 35:128–40. 10.1016/j.telpol.2010.12.003 [DOI] [Google Scholar]
- 57.Chen C-F, Chao W-H. Habitual or reasoned? Using the theory of planned behavior, technology acceptance model, and habit to examine switching intentions toward public transit. Transp Res Part F Traffic Psychol Behav. (2011) 14:128–37. 10.1016/j.trf.2010.11.006 [DOI] [Google Scholar]
- 58.Chuan-Chuan Lin J, Lu H. Towards an understanding of the behavioural intention to use a web site. Int J Inf Manage. (2000) 20:197–208. 10.1016/S0268-4012(00)00005-0 [DOI] [Google Scholar]
- 59.Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Q. (2003) 27:425–78. 10.2307/30036540 [DOI] [Google Scholar]
- 60.Venkatesh V, Thong JYL, Chan FKY, Hu PJ-H, Brown SA. Extending the two-stage information systems continuance model: incorporating UTAUT predictors and the role of context. Inf Syst J. (2011) 21:527–55. 10.1111/j.1365-2575.2011.00373.x [DOI] [Google Scholar]
- 61.Carter L, Bélanger F. The utilization of e-government services: citizen trust, innovation and acceptance factors. Inf Syst J. (2005) 15:5–25. 10.1111/j.1365-2575.2005.00183.x [DOI] [Google Scholar]
- 62.McKnight DH, Choudhury V, Kacmar C. The impact of initial consumer trust on intentions to transact with a web site: a trust building model. J Strateg Inf Syst. (2002) 11:297–323. 10.1016/S0963-8687(02)00020-3 [DOI] [Google Scholar]
- 63.Wang W-T, Lai Y-J. Examining the adoption of KMS in organizations from an integrated perspective of technology, individual, and organization. Comput Hum Behav. (2014) 38:55–67. 10.1016/j.chb.2014.05.013 [DOI] [Google Scholar]
- 64.Tang Z, Gong Z, Han X, Peng X. Public interest in continued use of Chinese government portals: a mixed methods study. Telematics Inform. (2018) 35:2312–25. 10.1016/j.tele.2018.09.011 [DOI] [Google Scholar]
- 65.Ogbanufe O, Kim DJ. Comparing fingerprint-based biometrics authentication versus traditional authentication methods for e-payment. Decis Support Syst. (2018) 106:1–14. 10.1016/j.dss.2017.11.003 [DOI] [Google Scholar]
- 66.Chauhan V, Pathak GS, Yadav R. Intention to adopt internet banking in an emerging economy: a perspective of Indian youth. Int J Bank Mar. (2015) 33:530–44. 10.1108/IJBM-06-2014-0075 [DOI] [Google Scholar]
- 67.Hoque MR. An empirical study of mHealth adoption in a developing country: the moderating effect of gender concern. BMC Med Inform Decis Mak. (2016) 16:51. 10.1186/s12911-016-0289-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Polites GL, Karahanna E. Shackled to the status quo: the inhibiting effects of incumbent system habit, switching costs, and inertia on new system acceptance. MIS Q. (2012) 36:21–42. 10.2307/41410404 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.