Abstract
Complete parathyroidectomy (PTx) is essential during total PTx for secondary hyperparathyroidism (SHPT) to prevent recurrent and persistent hyperparathyroidism. Pre-operative imaging evaluations, including computed tomography (CT), ultrasonography (US), and Tc-99m sestamibi (MIBI) scans, are commonly performed. Between June 2009 and January 2016, 291 patients underwent PTx for SHPT after pre-operative evaluations involving CT, US, and MIBI scans, and the diagnostic accuracies of these imaging modalities for identifying the parathyroid glands were evaluated in 177 patients whose intact parathyroid hormone (PTH) levels were <9 pg/mL after the initial PTx. Additional PTx procedures were performed on 7 of 114 patients whose intact PTH levels were >9 ng/mL after PTx, and the diagnostic validities of the imaging modalities for the remnant parathyroid glands were evaluated. A combination of CT, US, and MIBI scans achieved the highest diagnostic accuracy (75%) for locating bilateral upper and lower parathyroid glands before initial PTx. The accuracies of CT, US, and MIBI scans with respect to locating remnant parathyroid glands before additional PTx were 100%, 28.6%, and 100%, respectively. A combination of CT, US, and MIBI scans is useful for initial PTx for SHPT, and CT and MIBI scans are useful imaging modalities for additional PTx procedures.
Subject terms: Parathyroid glands, Parathyroid diseases
Introduction
During end-stage kidney disease, a lack of vitamin D activation in the kidney and phosphorus excretion into the urine causes hypocalcaemia and hyperphosphatemia, resulting in continuous stimulation of the parathyroid glands and causing secondary hyperparathyroidism (SHPT). In SHPT, enlargement (parathyroid dysplasia) of the usual parathyroid glands, i.e. bilateral upper and lower and sometimes the ectopic parathyroid glands, and the supernumerary parathyroid glands is observed. Ectopic parathyroid glands may result from variability or alteration in embryologic development or migration due to the influence of gravity or negative intrathoracic pressure following enlargement1. Supernumerary parathyroid glands may develop from accessory parathyroid fragments arising from the pharyngotracheal duct and are microscopic rests2,3. The incidences of ectopic and supernumerary parathyroid glands reported in operative series of patients with end-stage kidney disease are 39.3% and 6.5–37%, respectively3–7. On the other hand, primary hyperparathyroidism, which is caused by adenoma, hyperplasia, and rarely carcinoma, may show enlargement of the pathological parathyroid glands and usually causes hypercalcemia8,9. The common treatment of primary hyperparathyroidism (except for hyperplasia) is the removal of the pathological parathyroid glands. For pre-operative evaluation of primary hyperparathyroidism, diagnostic imaging studies are necessary to identify the pathological parathyroid glands8,10. However, in SHPT, removing the entire parathyroid gland is required because remnant parathyroid glands are continuously stimulated and can cause persistent and recurrent SHPT3,11. To prevent persistent and recurrent SHPT, pre-operative diagnostic imaging studies are necessary for localizing as many parathyroid glands as possible, including usual, ectopic and supernumerary parathyroid glands. Differences in the purpose of diagnostic imaging studies for primary and secondary hyperparathyroidism may lead to variations in the diagnostic imaging modalities that are employed.
During the initial total parathyroidectomy (PTx) for SHPT, complete PTx, which involves removing the entire parathyroid glands, is necessary to prevent persistent and recurrent SHPT, because PTx such cases can cause recurrent laryngeal nerve injury as a consequence of adhesions12,13. To achieve complete PTx, pre-operative imaging studies are useful for locating the parathyroid glands. Computed tomography (CT), ultrasonography (US), and Tc-99m sestamibi (MIBI) scans are often performed; however, the effectiveness of each modality and their combinations have not been investigated comprehensively in relation to initial and subsequent PTx procedures. Although many reports describe the efficacy of these modalities, either total PTx and transcervical thymectomy were not performed on all of the patients, or the pre-operative and post-operative intact parathyroid hormone (PTH) levels and the incidence of persistent and recurrent SHPT were not considered4,14–16. This implies that any remnant parathyroid glands that may have been present, but could not be identified during surgery, were ignored. Ectopic and supernumerary parathyroid glands are often overlooked, and these cause persistent and recurrent hyperparathyroidism (HPT)17–19. In the present study, the consistency in the localisation of the parathyroid glands, including the bilateral upper and lower, ectopic, and supernumerary parathyroid glands, between the imaging studies and their intra-operative identification was meticulously evaluated in patients whose post-operative intact PTH values had improved after initial PTx. The accuracy of the imaging studies in relation to additional PTx for persistent and recurrent SHPT was also investigated.
Results
Participants
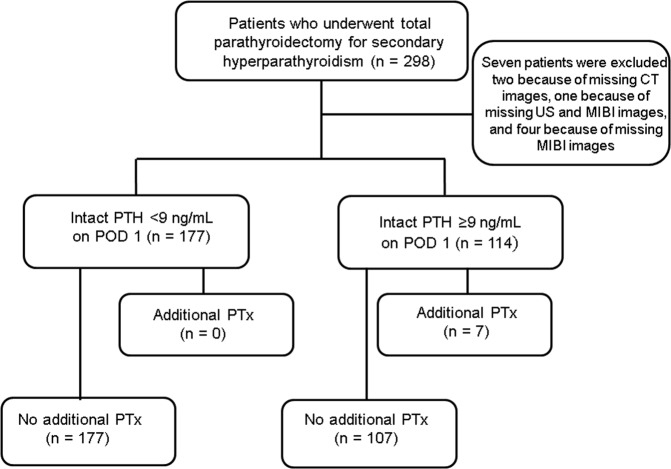
We monitored 298 patients between June 2009 and January 2016 for a mean observation period of 40.8 (standard deviation [SD] 22.2) months, and none of the patients dropped out of the study during this period. Seven patients were excluded from the study because some of their imaging data were missing. Of the 291 patients who were included in this study, 177 had intact PTH levels of <9 pg/mL, which is the lower limit of a normal intact PTH level, on post-operative day (POD) 1, and 114 had intact PTH levels of >9 pg/mL on POD 1 (Fig. 1).
Figure 1.
Patient flow chart. CT, computed tomography; US, ultrasonography; MIBI, Tc-99m sestamibi; PTH, parathyroid hormone; POD, post-operative day; PTx, parathyroidectomy.
Descriptive data
Table 1 summarises the characteristics of the patients who underwent initial PTx stratified according to their intact PTH levels on POD 1. The incidence of additional PTx for persistent and recurrent HPT was significantly lower in patients whose intact PTH levels were <9 pg/mL on POD 1 than in those with levels >9 pg/mL (odds ratio [OR]: 24.77, 95% confidence interval [CI]: 1.400–438.030; P = 0.001) (Table 1). Table 2 shows the number and locations of the parathyroid glands, including ectopic and supernumerary parathyroid glands, that were removed from the 177 patients whose intact PTH levels were <9 pg/mL on POD 1. Of the 177 patients, only 5 (2.8%) had 3 parathyroid glands; 39 (22.0%) had 44 supernumerary parathyroid glands (number of parathyroid glands ≥5), comprising 6 left lower, 2 right lower, 1 carotid sheath, and 35 intrathymic glands; and 65 (36.7%) had 90 ectopic parathyroid glands, comprising 2 intrathyroid, 1 mediastinal, and 87 intrathymic glands. Supplementary Fig. S1 shows an MIBI image of a remnant intrathymic parathyroid gland. Table 3 presents the characteristics of the 7 patients who underwent further PTx for persistent and recurrent SHPT. The mean intact PTH level after initial surgery was 157.1 pg/mL, significantly higher than the 9 pg/mL threshold.
Table 1.
Patient characteristics.
| Intact PTH (POD 1) <9 ng/mL | Intact PTH (POD 1) ≥9 ng/mL | P value | Odds ratio | 95% CI | ||
|---|---|---|---|---|---|---|
| 177 | 114 | |||||
| Male sex (n, %) | 102 (56.7) | 30 (36.1) | 0.006 | 0.502 | 0.311 | 0.811 |
| Mean age (years) (SD) | 56.0 (11.0) | 55.8 (12.4) | 0.732 | −2.267 | 3.222 | |
| Mean hemodialysis vintage (months) (SD) | 140.3 (83.2) | 140.4 (87.1) | 0.907 | |||
| Mean serum calcium level before initial PTx (mg/dL) (SD) | 9.76 (0.91) | 9.62 (0.78) | 0.163 | −0.059 | 0.349 | |
| Mean serum phosphorus level before initial PTx (mg/dL) (SD) | 5.67 (1.70) | 6.00 (1.57) | 0.103 | −0.713 | 0.658 | |
| Mean serum intact PTH level before initial PTx (pg/mL) (SD) | 591.4 (417.7) | 884.9 (708.8) | <0.001 | |||
| Mean serum intact PTH level after initial PTx (pg/mL) (SD) | 4.1 (2.0) | 62.6 (91.0) | <0.001 | |||
| Mean observation period (months) (SD) | 39.5 (21.9) | 42.0 (22.1) | 0.341 | −7.719 | 2.679 | |
| Additional PTx for persistent and recurrent hyperparathyroidism (n [%]) | 0 | 7 (6.1) | 0.001 | 24.77 | 1.400 | 438.030 |
PTH, parathyroid hormone; POD, postoperative day; 95% CI, 95% confidence interval; PTx, parathyroidectomy; SD, standard deviation.
Bold face font denotes statistically significant P-values.
Table 2.
The number and locations of the parathyroid glands.
| Number of parathyroid glands | Number of patients | Number of upper and lower parathyroid glands (ectopic parathyroid glands) | Number of supernumerary parathyroid glands |
|---|---|---|---|
| 177 | 703 (90, comprising 87 intrathymic, 2 intrathyroid, and 1 mediastinal glands) | 44, comprising 6 left lower, 2 right lower, 1 carotid sheath, and 35 intrathymic glands | |
| 3 | 5 | 15 (0) | 0 |
| 4 | 133 | 532 (64, comprising 2 intrathyroid, 1 mediastinal, and 61 intrathymic glands) | 0 |
| 5 | 34 | 136 (22 intrathymic glands) | 34, comprising 4 left lower, 2 right lower, and 28 intrathymic glands |
| 6 | 5 | 20 (4 intrathymic glands) | 10, comprising 1 carotid sheath, 2 left lower, and 7 intrathymic glands |
Table 3.
Characteristics of the patients who underwent additional parathyroidectomies.
| Patient characteristics | |
|---|---|
| 7 | |
| Mean duration until additional PTx (months) (SD) | 30.7 (17.7) |
| Mean serum calcium level before additional PTx (mg/dL) (SD) | 10.1 (0.8) |
| Mean serum phosphorus level before additional PTx (mg/dL) (SD) | 5.2 (0.8) |
| Mean serum intact PTH level after initial operation (pg/mL) (SD) | 157.1 (106.9) |
| Mean serum intact PTH level before additional PTx (pg/mL) (SD) | 409.0 (183.2) |
| Mean serum intact PTH level after additional PTx (pg/mL) (SD) | 41.0 (37.9) |
PTH, parathyroid hormone; PTx, parathyroidectomy; SD, standard deviation.
Diagnostic validity of each imaging modality alone and of their combinations before initial parathyroidectomy
Table 4 shows the diagnostic validity that was calculated from the consistency of the imaging studies of the typical bilateral upper and lower parathyroid glands in the patients who underwent initial PTx procedures. The accuracies of the imaging modalities used alone were significantly lower than their accuracy when used in combination. A combination of CT, US, and MIBI scanning was associated with the greatest diagnostic accuracy (75.1%), a difference that was significant (P < 0.001) (Table 4).
Table 4.
Comparisons of the diagnoses of the upper and lower parathyroid glands.
| Imaging modality | TP | TN | FP | FN | Accuracy | Comparison of accuracy: P value, sign test with Bonferroni correction | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| vs. CT | vs. US | vs. MIBI | vs. CT and US | vs. CT and MIBI | vs. US and MIBI | ||||||
| CT | 422 | 3 | 2 | 281 | 0.600 | ref | — | — | — | — | — |
| US | 402 | 4 | 1 | 301 | 0.573 | 0.999 | ref | — | — | — | — |
| MIBI | 299 | 3 | 2 | 404 | 0.427 | <0.001 | <0.001 | ref | — | — | — |
| CT and US | 514 | 3 | 2 | 189 | 0.730 | <0.001 | <0.001 | <0.001 | ref | — | — |
| CT and MIBI scanning | 465 | 3 | 2 | 238 | 0.661 | <0.001 | <0.001 | <0.001 | <0.001 | ref | — |
| US and MIBI scanning | 463 | 3 | 2 | 240 | 0.658 | <0.001 | <0.001 | <0.001 | <0.001 | 0.999 | ref |
| CT, US, and MIBI scanning | 529 | 3 | 2 | 174 | 0.751 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
TP, True positive; TN, True negative; FP, False positive; FN, False negative; ref, reference; CT, computed tomography; US, ultrasonography; MIBI, Tc—99m sestamibi scan.
Bold face font denotes statistically significant P-values.
Table 5 shows the consistency between the imaging modalities and the diagnostic validity in relation to the ectopic parathyroid glands. CT combined with US and CT combined with US and MIBI scanning were significantly more accurate than any of the imaging modalities used alone. The difference in the diagnostic accuracy of CT and US and CT, US, and MIBI scanning was not significant. None of the supernumerary parathyroid glands were identified pre-operatively in this patient series.
Table 5.
Comparisons of the diagnoses of the ectopic parathyroid glands.
| Imaging modality | TP | TN | FP | FN | Accuracy | Comparison of accuracy: P value, sign test with Bonferroni correction | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| vs. CT | vs. US | vs. MIBI | vs. CT and US | vs. CT and MIBI | vs. US and MIBI | ||||||
| CT | 43 | 0 | 0 | 47 | 0.478 | ref | — | — | — | — | — |
| US | 33 | 0 | 0 | 57 | 0.367 | 0.999 | ref | — | — | — | — |
| MIBI | 27 | 0 | 0 | 63 | 0.300 | 0.210 | 0.999 | ref | — | — | — |
| CT and US | 54 | 0 | 0 | 36 | 0.600 | 0.021 | <0.001 | <0.001 | ref | — | — |
| CT and MIBI | 52 | 0 | 0 | 38 | 0.578 | 0.084 | 0.021 | <0.001 | 0.999 | ref | — |
| US and MIBI | 44 | 0 | 0 | 46 | 0.489 | 0.999 | 0.021 | <0.001 | 0.441 | 0.999 | ref |
| CT, US, and MIBI | 57 | 0 | 0 | 33 | 0.633 | <0.001 | <0.001 | <0.001 | 0.999 | 0.999 | <0.001 |
TP, True positive; TN, True negative; FP, False positive; FN, False negative; ref, reference; CT, computed tomography; US, ultrasonography; MIBI, Tc—99m sestamibi scan.
Bold face font denotes statistically significant P-values.
Diagnostic validity of each imaging modality in relation to additional parathyroidectomy
Seven parathyroid glands were removed during additional PTx procedures. Two ectopic parathyroid glands were located in the thymus. Two supernumerary parathyroid glands were located in the thymus and mediastinum. These ectopic and supernumerary parathyroid glands were not identified pre-operatively with US. All remnant parathyroid glands were identified with CT and MIBI. The diagnostic accuracies for US were 0% (0/4 glands) for the remnant mediastinal and intrathymic parathyroid glands and 66.7% (2/3 glands) for the typical bilateral upper and lower parathyroid glands (Table 6). The accuracies of CT, US, and MIBI scanning were 100%, 28.6%, and 100%, respectively (Table 7).
Table 6.
Additional parathyroidectomy results.
| Patient | Number of resected parathyroid glands at initial operation | Location of undetected parathyroid gland at initial operation | Location of resected parathyroid gland at additional PTx | CT | US | MIBI |
|---|---|---|---|---|---|---|
| 1 | 3 | Right upper | Right upper | Detected | Undetected | Detected |
| 2 | 3 | Right upper | Right upper | Detected | Detected | Detected |
| 3 | 3 | Right lower | Intrathymic | Detected | Undetected | Detected |
| 4 | 3 | Left lower | Intrathymic | Detected | Undetected | Detected |
| 5 | 4 | None | Intrathymic | Detected | Undetected | Detected |
| 6 | 4 | None | Mediastinum | Detected | Undetected | Detected |
| 7 | 4 | Right lower | Right lower | Detected | Detected | Detected |
PTx, parathyroidectomy; CT, computed tomography; US, ultrasonography; MIBI, Tc-99m sestamibi scan.
Table 7.
Diagnoses during additional parathyroidectomy.
| Imaging modality | TP | TN | FP | FN | Accuracy |
|---|---|---|---|---|---|
| CT | 7 | 0 | 0 | 0 | 100% |
| US | 2 | 0 | 0 | 5 | 28.6% |
| MIBI | 7 | 0 | 0 | 0 | 100% |
TP, true positive; TN, true negative; FP, false positive; FN, false negative; CT, computed tomography; US, ultrasonography; MIBI, Tc-99m sestamibi scan.
US shows significantly lower accuracy compared to the other two modalities.
Discussion
SHPT is caused by hypocalcaemia and hyperphosphatemia due to the lack of vitamin D activation in the kidney and phosphorus excretion into the urine following kidney failure. Patients with kidney failure are commonly treated with dialysis to adjust their electrolytes. Despite the adjustment, hypocalcaemia and hyperphosphatemia are often observed and treated with a vitamin D, calcium, and phosphate binder. In this study, although the pre-operative mean serum calcium and phosphorus levels were well controlled with these medications, the long haemodialysis vintage (around 140 months in each group) might have caused SHPT20,21. Complete PTx, which involves removing the entire parathyroid glands, is necessary for patients with SHPT to prevent persistence and recurrence10. However, identifying all of the parathyroid glands is difficult because of their embryology and development of HPT22, and in this study, 7 out of 298 patients (2.3%) underwent additional PTx procedures. Considerable variations in the number and locations of the parathyroid glands cause difficulties in their identification6,22. Of the 177 patients who underwent the successful removal of all their parathyroid glands and did not need additional PTx, only 5 (2.8%) had 3 parathyroid glands, 39 (22.0%) had supernumerary parathyroid glands, and 65 (36.7%) had 90 ectopic parathyroid glands. The percentages of the patients with ectopic (39.3%) and supernumerary (6.5–37%) parathyroid glands were not lower than those reported previously4–7, which indicates that precise PTx procedures were performed in the 177 patients. Undertaking imaging to identify the parathyroid glands before PTx is helpful, because it prevents unsuccessful PTx and unnecessary dissection of tissues that are fragile due to chronic kidney disease23. Some studies have investigated the effectiveness of imaging, but the definitions of the complete removal of the parathyroid glands were not clear. The results may also have overestimated the effectiveness of imaging, because ectopic and supernumerary parathyroid glands were overlooked, and the diagnostic validities associated with imaging ectopic and supernumerary parathyroid glands have been rarely investigated for the same reason16. In this study, the complete removal of the parathyroid glands was clearly defined, and the results were corroborated by the lack of additional PTx procedures required for persistent and recurrent SHPT3.
All the patients in this study underwent CT, US, and MIBI scanning, and the diagnostic validities of the imaging modalities were determined retrospectively. The accuracy of each modality at identifying the standard bilateral upper and lower parathyroid glands was between 42.7% and 60.0%, which was lower than the accuracies of their different combinations. Hence, using one imaging modality is not beneficial for evaluating the location of parathyroid glands, and in particular, the lower diagnostic accuracy of MIBI scans compared with the diagnostic accuracies of CT and US implies that, rather than using MIBI scanning as the main diagnostic imaging modality for pre-operative evaluations of primary HPT, it should be used as an auxiliary imaging modality24. Regarding the assessment of the combinations of imaging modalities, the combination of CT, US, and MIBI scanning showed a significantly higher accuracy than other combinations. This implies that a combination of CT, US, and MIBI scanning is the most beneficial for pre-operative localisation of the upper and lower parathyroid glands.
The diagnostic validities of the imaging modalities used to identify the ectopic parathyroid glands were similar to those of the imaging modalities used to identify the upper and lower parathyroid glands. The mediastinal parathyroid glands were successfully identified pre-operatively and removed from 1 of the 177 patients during the initial PTx procedure. The diagnostic accuracies of CT and US and CT, US, and MIBI scanning for ectopic parathyroid gland identification were higher than those associated with any of the imaging modalities used alone or any of the other imaging modality combinations. However, there was no difference in diagnostic accuracy between CT and US and CT, US, and MIBI scanning.
None of the supernumerary parathyroid glands were identified pre-operatively, and 44 supernumerary parathyroid glands were removed. Nine out of 44 supernumerary parathyroid glands were identified during the procedures. The remaining 35 supernumerary parathyroid glands were identified microscopically and could not be identified during pre-operative imaging or surgery11,18. Since 8 out of 9 supernumerary parathyroid glands were adjacent to the typically located parathyroid glands and 1 supernumerary parathyroid gland was within the carotid sheath, these were overlooked during the pre-operative imaging assessments. Each of the 8 supernumerary parathyroid glands that were adjacent to the typically located parathyroid glands was identified as one parathyroid gland pre-operatively; hence, pre-operative imaging was not useful for identifying supernumerary parathyroid glands.
While it was difficult to identify the supernumerary parathyroid glands, the results from this study regarding the diagnostic validity of imaging for the identification of the typical upper and lower, and ectopic parathyroid glands demonstrated that a combination of CT, US, and MIBI scans was the most appropriate approach for determining the locations of these glands before the initial PTx procedures.
Persistent and recurrent HPT occurs in 5–30% of patients after PTx for SHPT25–27. In our study, 7 out of 291 patients (2.4%) underwent additional PTx procedures for persistent and recurrent HPT. This rate is lower than those reported previously because all the patients underwent total PTx and transcervical thymectomy;28 consequently, 35 supernumerary parathyroid glands that were detected microscopically in the thymus were removed from 177 patients. Although this procedure was effective for initial PTx, patients who required additional PTx were encountered. Determining the locations of the parathyroid glands before additional PTx is necessary. The accuracies of CT and MIBI scans before the additional PTx procedures were 100%, but the accuracy of US was lower than the accuracies of CT and MIBI scanning, which indicates that US is not useful for locating parathyroid glands before additional PTx. US could not identify parathyroid glands in the thymus or mediastinum, and its accuracy at identifying parathyroid glands in the typical upper and lower locations was lower (66.7%) than the accuracies of CT (100%) and MIBI scanning (100%). Hence, CT and MIBI scanning may be useful for locating parathyroid glands before additional PTx procedures, but MIBI scanning cannot detect their locations accurately. CT may be necessary to locate parathyroid glands precisely and to avoid recurrent laryngeal nerve injuries caused by scars and unnecessary dissections. CT and MIBI scanning may be useful to confirm the locations of remnant parathyroid glands29. For the initial and additional PTx procedures, both CT and MIBI scanning were clearly useful. SPECT/CT imaging has recently been reported to improve planar MIBI diagnostic performance, especially in SHPT30. Furthermore, the efficacy of the newest nuclear medicine procedures (i.e. 11C-choline-PET-CT and 18F-choline-PET-CT) have been reported for the pre-operative diagnosis of parathyroid disease31,32. The efficacy of these modalities for pre-operative localisation of parathyroid glands in SHPT remains to be investigated.
One limitation associated with this study is its retrospective design; therefore, future prospective randomised studies of the diagnostic accuracy of pre-operative imaging should be undertaken. In conclusion, CT, US, and MIBI scanning are useful for imaging before initial PTx procedures for SHPT, and CT and MIBI scanning are useful for additional PTx procedures.
Methods
Ethical considerations
This study was approved by the Nagoya Daini Red Cross Hospital’s Institutional Review Board, and conducted in accordance with the principles of the Declaration of Helsinki.
Study design
To investigate the diagnostic accuracies of CT, US, and MIBI scanning used alone and in every combination before initial PTx. Patients with intact PTH values of <9 pg/mL on POD 1 were selected to participate in this study. The locations of the parathyroid glands in these patients had been determined pre-operatively by radiologists using each imaging modality alone and in every combination. Determined locations were compared with the locations of the parathyroid glands determined intra-operatively, and consistency was investigated with respect to the bilateral upper and lower, ectopic, and supernumerary parathyroid glands. The diagnostic validity of each imaging modality was also investigated in the patients who required additional PTx procedures. This retrospective cohort study was conducted according to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines.
Participants
Between June 2009 and January 2016, 298 consecutive patients underwent PTx for SHPT at our hospital. CT, US, and MIBI scanning were performed pre-operatively. One hundred and seventy-seven patients whose intact PTH values were <9 pg/mL on POD 1 participated in an evaluation of the diagnostic validity of the imaging modalities before the initial PTx, and 7 patients participated in an evaluation of the diagnostic validity of the imaging modalities before an additional PTx. The data were collected retrospectively from the patients’ charts and analysed anonymously. As such, the need for informed consent was waived by the relevant institutional review board.
Indications for an initial parathyroidectomy
The clinical practice guidelines for the management of SHPT in chronic dialysis patients were used to determine a patient’s indications for an initial PTx33. Patients who could not continue with calcimimetic agents because of adverse effects were also indicated for initial PTx.
Pre-operative evaluations of the parathyroid glands
The locations of the parathyroid glands in all the patients were determined pre-operatively by radiologists using CT, US, and planar MIBI scanning. Different radiologists assessed the CT, US, and planar MIBI scans.
Surgical procedures and locating the parathyroid glands
PTx and transcervical thymectomy with forearm autograft comprised the initial PTx procedure, which was performed under general anaesthesia in all patients. Four surgeons performed the initial and additional PTx procedures, and they determined the locations of the parathyroid glands during the operations. Pathologists examined frozen and paraffin sections of all the parathyroid glands.
Indications for additional parathyroidectomies
Additional PTx procedures were indicated for patients who were refractory to medication and for patients whose parathyroid glands were identified pre-operatively in the neck or mediastinum using CT, US, or planar MIBI scans33.
Comparisons of the pre-operative imaging evaluations and the intra-operative localisation of the parathyroid glands
The pre-operative imaging evaluations and the intra-operative localisation of the bilateral upper and lower, ectopic, and supernumerary parathyroid glands were compared in relation to the initial PTx. For the additional PTx, the pre-operative imaging evaluations and the intra-operative localisation of the remnant parathyroid glands were compared.
Statistical analyses
The continuous variables were presented as the means (SDs) and the categorical variables were presented as the numbers and percentages. The statistical analyses were performed using the independent sample t-test or the Mann-Whitney U test for the continuous data, and the chi-squared test or Fisher’s exact test for the categorical variables. The patients were categorised as true positive, true negative, false positive, and false negative, and the accuracies of the imaging studies were evaluated. The accuracies of the imaging studies undertaken before the initial PTx were compared using the sign test. The Bonferroni correction was used to adjust for multiplicity. A value of P < 0.05 was considered statistically significant. The statistical analyses were performed using IBM®SPSS® software, for Windows, version 23.0 (IBM Corporation, Armonk, NY, USA).
Supplementary information
Author Contributions
T.H. conceived the study and its design, analysed the data, and drafted the manuscript, T.T., M.O. and K.F. conceived the study and its design, and acquired the data, M.T. interpreted the data, N.G., S.N. and Y.W. critically revised the manuscript for important intellectual content, and Y.T. and T.I. provided final approval of the version to be published.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-51265-y.
References
- 1.Thompson NW, Eckhauser FE, Harness JK. The anatomy of primary hyperparathyroidism. Surgery. 1982;92:814–821. [PubMed] [Google Scholar]
- 2.Henry, J. F. Applied embryology of the thyroid and parathyroid glands. In Surgery of the thyroid and parathyroid glands (ed. Randolph, G. W.) 12–20 (Saunders, 2003).
- 3.Aly A, Douglas M. Embryonic parathyroid rests occur commonly and have implication s in the management of secondary hyperparathyroidism. ANZ J. Surg. 2003;73:284–288. doi: 10.1046/j.1445-2197.2003.t01-1-02620.x. [DOI] [PubMed] [Google Scholar]
- 4.Alkhalili E, et al. The utility of neck ultrasound and sestamibi scans in patients with secondary and tertiary hyperparathyroidism. World J. Surg. 2015;39:701–705. doi: 10.1007/s00268-014-2878-3. [DOI] [PubMed] [Google Scholar]
- 5.Pattou FN, et al. Supernumerary parathyroid glands: frequency and surgical significance in treatment of renal hyperparathyroidism. World J. Surg. 2000;24:1330–1334. doi: 10.1007/s002680010220. [DOI] [PubMed] [Google Scholar]
- 6.Akerström G, Malmaeus J, Bergström R. Surgical anatomy of human parathyroid glands. Surgery. 1984;95:14–21. [PubMed] [Google Scholar]
- 7.Schneider R, et al. Frequency of ectopic and supernumerary intrathymic parathyroid glands in patients with renal hyperparathyroidism: analysis of 461 patients undergoing initial parathyroidectomy with bilateral cervical thymectomy. World J. Surg. 2011;35:1260–1265. doi: 10.1007/s00268-011-1079-6. [DOI] [PubMed] [Google Scholar]
- 8.Silverberg, S. J., & Bilezikian, J. P. Primary hyperparathyroidism: pathophysiology, surgical indications, and preoperative workup. In Surgery of the Thyroid and Parathyroid Glands second edition (ed. Randolph, G. W.) 531–538 (Elsevier Saunders, 2013).
- 9.Campennì A, et al. Parathyroid carcinoma presenting as normocalcemic hyperparathyroidism. J. Bone Miner. Metab. 2012;30:367–372. doi: 10.1007/s00774-011-0344-y. [DOI] [PubMed] [Google Scholar]
- 10.Campennì A, et al. Association of parathyroid carcinoma and thyroid disorders: A clinical review. Endocrine. 2017;56:19–26. doi: 10.1007/s12020-016-1147-7. [DOI] [PubMed] [Google Scholar]
- 11.Hibi Y, et al. Reoperation for renal hyperparathyroidism. World J. Surg. 2002;26:1301–1307. doi: 10.1007/s00268-002-6731-8. [DOI] [PubMed] [Google Scholar]
- 12.Tominaga Y, et al. Re-operation is frequently required when parathyroid glands remain after initial parathyroidectomy for advanced secondary hyperparathyroidism in uraemic patients. Nephrol. Dial. Transplant. 2003;18(Suppl 3):65–70. doi: 10.1093/ndt/gfg1017. [DOI] [PubMed] [Google Scholar]
- 13.Cattan P, et al. Reoperation for secondary uremic hyperparathyroidism: are technical difficulties influenced by initial surgical procedure? Surgery. 2000;127:562–565. doi: 10.1067/msy.2000.105865. [DOI] [PubMed] [Google Scholar]
- 14.Lee JB, Kim WY, Lee YM. The role of preoperative ultrasonography, computed tomography, and sestamibi scintigraphy localization in secondary hyperparathyroidism. Ann. Surg. Treat. Res. 2015;89:300–305. doi: 10.4174/astr.2015.89.6.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yuan LL, Kan Y, Ma DQ, Yang JG. Combined application of ultrasound and SPECT/CT has incremental value in detecting parathyroid tissue in SHPT patients. Diagn. Interv. Imaging. 2016;97:219–225. doi: 10.1016/j.diii.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 16.Andrade JS, et al. Localization of ectopic and supernumerary parathyroid glands in patients with secondary and tertiary hyperparathyroidism: surgical description and correlation with preoperative ultrasonography and Tc99m-Sestamibi scintigraphy. Braz. J. Otorhinolaryngol. 2014;80:29–34. doi: 10.5935/1808-8694.20140008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Okada M, et al. Location frequency of missed parathyroid glands after parathyroidectomy in patients with persistent or recurrent secondary hyperparathyroidism. World J. Surg. 2016;40:595–599. doi: 10.1007/s00268-015-3312-1. [DOI] [PubMed] [Google Scholar]
- 18.Numano M, et al. Surgical significance of supernumerary parathyroid glands in renal hyperparathyroidism. World J. Surg. 1998;22:1098–1102. doi: 10.1007/s002689900524. [DOI] [PubMed] [Google Scholar]
- 19.Schneider R, Bartsch DK, Schlosser K. Relevance of bilateral cervical thymectomy in patients with renal hyperparathyroidism: analysis of 161 patients undergoing reoperative parathyroidectomy. World J. Surg. 2013;37:2155–2161. doi: 10.1007/s00268-013-2091-9. [DOI] [PubMed] [Google Scholar]
- 20.Jäger MD, et al. Risk-factors for nodular hyperplasia of parathyroid glands in sHPT patients. PLoS One. 2017;12:e0186093. doi: 10.1371/journal.pone.0186093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Malberti F, et al. Parathyroidectomy in patients on renal replacement therapy: an epidemiologic study. J. Am. Soc. Nephrol. 2001;12:1242–1248. doi: 10.1681/ASN.V1261242. [DOI] [PubMed] [Google Scholar]
- 22.Agarwal, A., Mishra, A. K., Lombardi, C. P., & Raffaelli, M. Applied embryology of the thyroid and parathyroid glands. In Surgery of the Thyroid and Parathyroid Glands second edition (ed. Randolph, G. W.) 15–24 (Elsevier Saunders, 2013).
- 23.Richards ML, Wormuth J, Bingener J, Sirinek K. Parathyroidectomy in secondary hyperparathyroidism: is there an optimal operative management? Surgery. 2006;139:174–180. doi: 10.1016/j.surg.2005.08.036. [DOI] [PubMed] [Google Scholar]
- 24.Toriie S, et al. Evaluation of the minimally invasive parathyroidectomy in patients with primary hyperparathyroidism: a retrospective cohort study. Ann. Med. Surg. (Lond.). 2016;7:42–47. doi: 10.1016/j.amsu.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weber T, Zeier M, Hinz U, Schilling T, Büchler MW. Impact of intraoperative parathyroid hormone levels on surgical results in patients with renal hyperparathyroidism. World J. Surg. 2005;29:1176–1179. doi: 10.1007/s00268-005-7805-1. [DOI] [PubMed] [Google Scholar]
- 26.Coulston JE, Egan R, Willis E, Morgan JD. Total parathyroidectomy without autotransplantation for renal hyperparathyroidism. Br. J. Surg. 2010;97:1674–1679. doi: 10.1002/bjs.7192. [DOI] [PubMed] [Google Scholar]
- 27.Conzo G, et al. Total parathyroidectomy without autotransplantation in the surgical treatment of secondary hyperparathyroidism of chronic kidney disease. J. Endocrinol. Invest. 2012;35:8–13. doi: 10.3275/7621. [DOI] [PubMed] [Google Scholar]
- 28.Uno N, et al. Incidence of parathyroid glands located in thymus in patients with renal hyperparathyroidism. World J. Surg. 2008;32:2516–2519. doi: 10.1007/s00268-008-9739-x. [DOI] [PubMed] [Google Scholar]
- 29.Yin L, Guo D, Liu J, Yan J. The role of 99mTc-MIBI SPECT-CT in reoperation therapy of persistent hyperparathyroidism patients. Open Med. (Wars.). 2015;10:462–467. doi: 10.1515/med-2015-0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhen L, et al. The application of SPECT/CT for preoperative planning in patients with secondary hyperparathyroidism. Nucl. Med. Commun. 2013;34:439–444. doi: 10.1097/MNM.0b013e32835f9447. [DOI] [PubMed] [Google Scholar]
- 31.Treglia G, et al. Diagnostic performance of choline PET for detection of hyperfunctioning parathyroid glands in hyperparathyroidism: a systematic review and meta-analysis. Eur. J. Nucl. Med. Mol. Imaging. 2019;46:751–765. doi: 10.1007/s00259-018-4123-z. [DOI] [PubMed] [Google Scholar]
- 32.Piccardo A, et al. Additional value of integrated 18F-choline PET/4D contrast-enhanced CT in the localization of hyperfunctioning parathyroid glands and correlation with molecular profile. Eur. J. Nucl. Med. Mol. Imaging. 2019;46:766–775. doi: 10.1007/s00259-018-4147-4. [DOI] [PubMed] [Google Scholar]
- 33.Fukagawa M, et al. Clinical practice guideline for the management of chronic kidney disease-mineral and bone disorder. Ther. Apher. Dial. 2013;17:247–288. doi: 10.1111/1744-9987.12058. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.