Abstract
Background
Since a primary watertight dural suture after incidental durotomies has a failure rate of 5–10%, a watertight closure technique of the overlying layers (fascia, subcutis and skin) is essential. The purpose of this cadaveric study was to find the most watertight closure technique for fascia, subcutis and skin.
Methods
Different suturing techniques were tested for each layer in a sheep cadaveric model by measuring the leakage pressure. The specimens were mounted on a pressure chamber connected to a manometer and a water tube system. Subsequently, the leakage was over-sewed with a cross stitch and the experiment was repeated.
Results
Cross stitch suturing [median =180 mbar (43; 660)] performed best compared to continuous [median =16 mbar (6; 52)] (P=0.003) but not to single knot [median =118 mbar (21; 387)] (P=1.0) or locking stitch suturing [median =109 mbar (3; 149)] (P=0.93) for fascia closure. Continuous suture [median =9 mbar (3; 14)] resulted in a higher leakage pressure than single knot [median =1 mbar (1; 6)] (P=0.017) for subcutaneous closure. No significant differences were found between intracutaneous, Donati-continuous, single knot and locking stitch for skin closures (P=0.075). However, the Donati-continuous stitch closure resulted in higher pressures in tendency. Over-sewing increased median leakage pressure from 8.0 to 11.0 mbar (P=0.068) and from 4.0 to 13.0 mbar (P=0.042) for single knot and for locking stitch skin closures, respectively.
Conclusions
Cross stitches for the fascia, continuous suturing technique for the subcutis and Donati-continuous stitch for the skin resulted in the most watertight closure within this experimental setting. If leakage occurs, over-sewing might relevantly improve the watertightness of the wound.
Keywords: Wound closure, suture technique, watertightness, incidental durotomy, lumbar spine
Introduction
The rate of incidental durotomies varies around 1–17% of all lumbar spinal surgeries (1-4), representing one of the most common complications of lumbar spine surgery (5,6). In such a case, the advantage of a primary watertight dural repair is undisputed (3,5,7,8). Previous studies have examined which suturing technique leads to the highest hydrostatic strength for dural closure (9-12). Yet it is not always possible to close the dura completely watertight, for example due to localization and morphology of the tear or a mismatch of the diameter of suture relative to the needle (9). Narotam et al. also showed that a primary watertight suture has a failure rate of 5% to 10% (13) leading to pseudomeningoceles, cerebrospinal fluid (CSF) fistulas, wound infections or intracranial hypotension syndrome. Revision surgeries are often inevitable in such cases.
If the CSF leaks out of the skin, the risk of a persisting CSF fistula and therefore infection exists (14). Thus the most watertight closure technique of lumbar wounds (fascia, subcutis and skin) is desired to reduce the development of CSF fistula after incidental durotomy.
To the best of our knowledge, the watertightness of different suturing techniques to close the fascia, subcutis and skin of the lumbar region has not yet been investigated experimentally. Therefore, the purpose of this cadaveric study was to find the most watertight closure technique for fascia, subcutis and skin of the lumbar spine.
Methods
Specimen preparation
Ovine fascia, subcutis and skin of 6 different sheep were used in this study to prepare fresh pieces of 15 cm × 10 cm. A 6 cm incision was performed midline through all the layers, representing a possible incision length for lumbar multi-level decompression. The following suturing techniques were applied by one senior staff member. For the skin: intracutaneous suture (Monocryl 3-0, Figure 1A), Donati-continuous suture (Ethilon 2-0, Figure 1B), single knot suture (Ethilon 2-0, Figure 1C) and locking stitch suture (Ethilon 2-0, Figure 1D). For the subcutis: continuous suture (Figure 1E) and single knot suture (Figure 1C) (both with Vicryl 3-0). And for the fascia: single knot suture (Figure 1C), cross stitches (Figure 1F), continuous suture (Figure 1E) and locking stitch suture (Figure 1D) (all with Vicryl 1). To standardize the distances of needle penetration, a plastic template was used to draw the entry points. Each suturing technique was performed 5 times per level (fascia, subcutis and skin).
Figure 1.
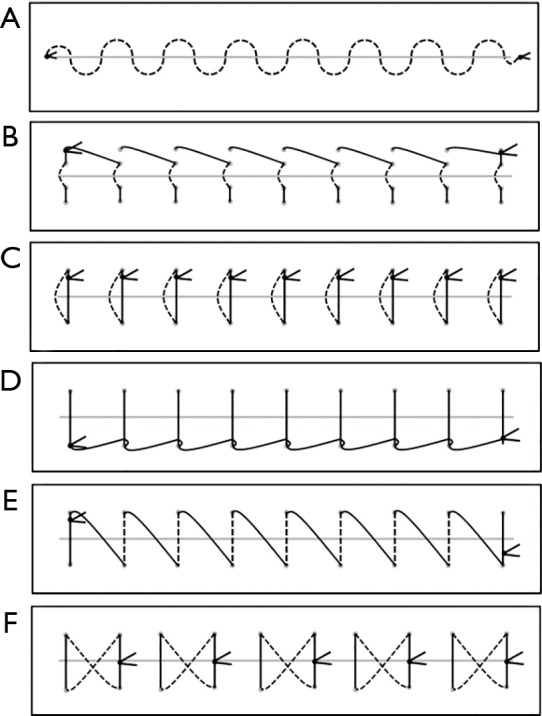
Suture techniques: (A) intracutaneous suture; (B) Donati-continuous suture; (C) single knot suture; (D) locking stitch suture; (E) continuous suture; (F) cross stitch suture.
Experimental setting (Figure 2)
Figure 2.
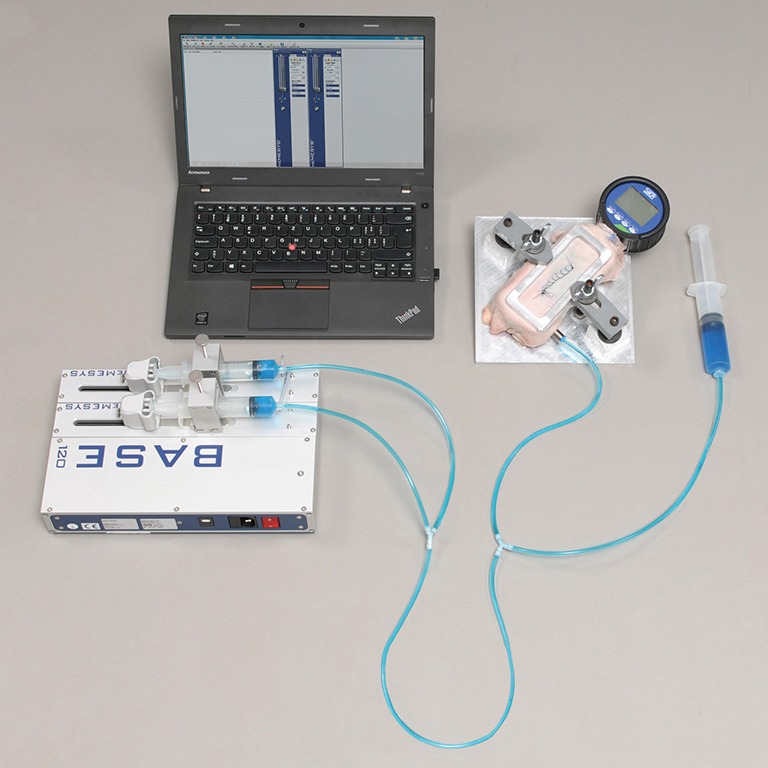
Experimental setting: low-pressure modules with two syringes connected through a flexible tube system with the pressure chamber. Additional syringe on the right to deaerate the system.
A calibrated, digital precision-reference-manometer (SIKA Dr. Soebert & Kühn GmbH & Co. KG, Kaufungen, Germany) with a measuring range of −1 to 3 bar and a resolution of 1 mbar, mounted on a custom made aluminium pressure chamber was used for recording the hydrostatic pressure continuously.
To feed a constant flow of phosphate buffered saline (PBS) solution into the flexible tubes connected system, neMESYS dosing Systems were used (Cetoni GmbH, Korbussen, Germany) consistent of basemodule 120 and two low pressure modules (14:1) controlled by neMESYS Userinterface V.2016.6.14.1 software. Each low-pressure module was equipped with a 30 mL syringe and the whole system was loaded with PBS solution. For better visualization, food coloring was added to the PBS solution. Hereby it was carefully observed, that no air bubbles were introduced within the system and that the chamber was filled to the rim. To minimize the influence of a hydraulic gradient between syringes and chamber, the whole setup was horizontally aligned on the same plane.
After mounting the specimen on the pressure chamber tightly, a constant flow of 1 mL/s was applied into the pressure chamber. Slow-motion videos were used to determine the exact pressure values. Leakage was defined at a maximum pressure value when the first drop of PBS solution was observed. For ten specimens (series with single knot and locking stitch of the skin), the leakage was over-sewed with a cross-stitch and the experiments were repeated to investigate the effect of over-sewing.
Statistical analysis
Statistical analysis was performed using SPSS (IBM Corp. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.). Statistical significance of the effect of suture technique on leakage pressure within the respective subgroup (type of tissue) was investigated using Kruskal-Wallis/Mann-Whitney U tests. For post-hoc analysis, in groups showing a statistically significant effect, the suture technique with the highest median leakage pressure was compared to all other suture techniques. P values were adjusted using Bonferroni correction. Significance was set at α =0.05.
To test for a significant effect of over-sewing on leakage pressure for the subgroup skin, Wilcoxon signed-rank tests were used for the two applied suture techniques.
Results
Skin closure
For skin closure no significant differences were found between the investigated suturing techniques with intracutaneous [median =5 mbar (4; 13)], Donati-continuous [median =20 mbar (6; 55)], single knot [median =10 mbar (3; 21)] and locking stitch suturing [median =8 mbar (5; 23)] [H(3) =6.9, P=0.075]. However, the Donati-continuous stitch closure resulted in higher pressures in tendency (Figure 3).
Figure 3.
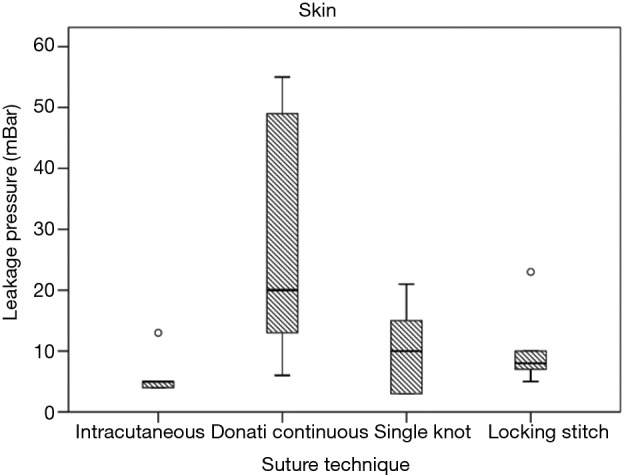
For skin closure no significant differences were found between the investigated suturing techniques (P=0.075). However, the Donati-continuous stitch closure resulted in higher pressures in tendency.
Over-sewing of the skin increased median leakage pressure from 8.0 to 11.0 mbar (Z=−1.826, P=0.068) and from 4.0 to 13.0 mbar (Z=−2.032, P=0.042) for single knot and for locking stitch, respectively. There was a significant increase in leakage pressure following over-sewing for locking stitch (median change: 10 mbar) (Figure 4).
Figure 4.
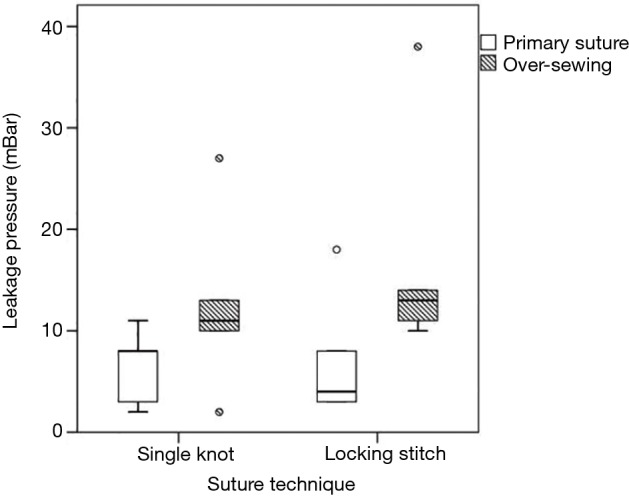
Over-sewing of the skin significantly increased the median leakage pressure from 4.0 to 13.0 mbar (P=0.042) in the locking stich group.
Subcutis closure
For closure of the subcutis, continuous suturing [median =9 mbar (3; 14)] resulted in a significantly higher leakage pressure than single knot suturing [median =1 mbar (1; 6)] (U=2.000, P=0.017, r=0.60) (Figure 5).
Figure 5.
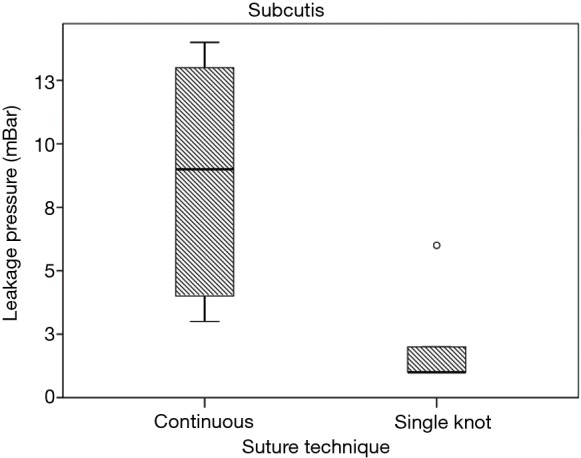
For subcutis closure, continuous suturing (median =9 mbar) resulted in a significantly higher leakage pressure than single knot suturing (median =1 mbar) (P=0.017).
Fascia closure
There was a statistically significant effect of suture technique on leakage pressure for the fascia closure with cross-stitches [H(3) =13.294, P=0.004] (Figure 6).
Figure 6.
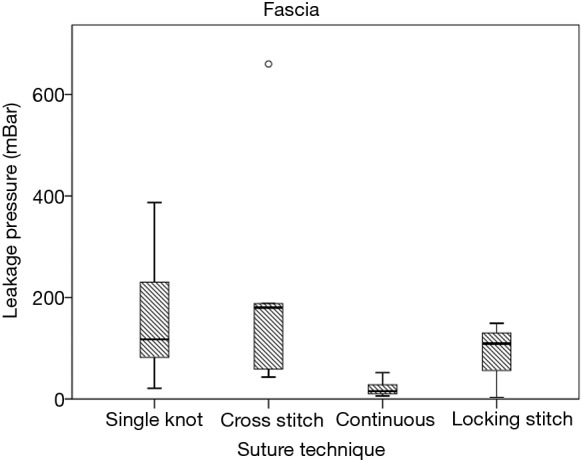
For fascia closure, cross stitch (median =180 mbar) resulted in a significantly higher leakage pressure than continuous (median =16 mbar) (P=0.003) but not than single knot (median =118 mbar) (P=1.0) and locking stitch suture (median =109 mbar) (P=0.93).
Post-hoc comparison revealed cross stitch [median =180 mbar (43; 660)] to be significantly superior to continuous [median =16 mbar (6; 52)] (U=1.0, P=0.003, r=0.76) but not to single knot [median =118 mbar (Jeyn21; 387)] (U=14.0, P=1.0, r=0.05) and locking stitch suturing [median =109 mbar (3; 149)] (U=7.0, P=0.93, r=0.36).
All layers
The spot of leakage occurred in 6 out of 58 sutures at the site of the needle holes. For the other 52 the spot of leakage was in the region of incision.
Discussion
Since primary watertight dural suture after incidental durotomy has a failure rate of 5% to 10% (13), a watertight closure technique of the overlying layers (fascia, subcutis and skin) is essential to reduce the risk of development of CSF fistula, which result in revision surgery (5). Although suturing techniques for a watertight dural repair were compared, such comparison for the overlying layers were lacking up to this series of experiments.
In this study we found that cross stitches for the fascia, continuous suturing technique for the subcutis and Donati-continuous stitch for the skin resulted in the most watertight wound closure combination.
For the fascial closure, statistical significance could be found only in comparing cross stitches with continuous suturing but not with single knot or locking stitch suturing. Nevertheless, a strong tendency was found favoring cross stitches with a median leakage pressure of 180 mbar compared to 118 and 109 mbar in single knot and locking stitches respectively. The lacking statistical significance is most probably explained by the fact that reproducibility of the measured leakage pressures was difficult to achieve due to carcass characteristics which in turn resulted in relatively wide standard deviations. Further investigations should therefore include a greater sample sizes but also human specimens for better external validity. The complexity of our study set-up and the limited supply of cadavers only allowed a relatively small sample size. However, our results implicate that in cases of intraoperative CSF leakage cross stitches should be favored for fascial closure.
Moreover, we observed that the fascial layer provides with a median of 180 mbar leakage pressure the strongest water barrier compared to the subcutis and cutis with 9 mbar and 20 mbar respectively. This is an important information in our view and the clinical consequence is that beside the dural closure, particularly the fascial layer seems mostly important for achieving watertightness.
For the subcutis, continuous sutures showed significantly better leakage pressure than single knot suturing. No statistical significances were found comparing the here investigated skin suture techniques and we are therefore are not able to make strong recommendations for such, although some tendency favoring Donati-continuous stitches can be mentioned. This might be caused due to the characteristics of the Donati- technique which includes a superficial and deep sutured layer compared with the other suture types (intracutaneous, single knot and locking stitches) which only include one layer, respectively.
There is little data about the expected postoperative CSF pressure in case of a lumbar CSF leakage. It is known from lumbar punctures in a sitting position, that CSF opening pressures are around 34.6 cmH2O, which corresponds to about 34 mbar (15). Expected peak pressures while coughing extent from 80 to 125 mmHg, which correspond to about 107 to 167 mbar (16,17). This means that even in a case of an absent dural layer the fascial closure might provide enough watertightness to resist physiological CSF pressure. Nevertheless, our data are based on ovine specimens and should be confirmed with human specimens or even better with in vivo experiments.
In cases of insufficient dural closure but sufficient epidural wound closure a pseudomeningocele might develop. The exact incidence of a pseudomeningocele is difficult to estimate, but assumed to be around 0.07–2% for lumbar laminectomies and discectomies (5,18). Most of these pseudomeningoceles appear to be asymptomatic (19-23). Local swelling might be the sole indicator of a pseudomeningocele. The management remains controversial; While some authors recommend surgical revision (19,22,23), others only recommended a surgical repair in case of a large symptomatic pseudomeningocele, progressive neurological symptoms, fistula, infection or intracranial hypotension (20). However, small pseudomeningoceles (<5 cm) usually resorb spontaneously within 3 months to 3 years (19-21). Therefore, they can often be treated non-operatively.
A further finding in our experiment was that once a cutaneous leakage occurred, reinforcement of the suture by over-sewing the spot of leakage with a cross stitch led up to a three times higher leakage pressure (Figure 4). This is concordant with other results from the literature. Tosun et al. stated, that over-sewing the wound with a gauze pad for 5 days after non-recognized intraoperative dural tears with CSF fistula, represents a reasonable therapy option in patients without neurological impairment (5). Waisman and Schweppe treated eight patients with postoperative CSF leakage conservatively, by reinforcing the skin suture, bed rest in the Trendelenburg position, antibiotic coverage, and repeated drainage of the subcutaneous CSF collection. None of the patient needed a surgical revision for persisting CSF leakage (24). In our own clinical experience, bedside over-sewing of the spot of leakage can be a valuable approach to reduce the rate of revision surgeries in the case of CSF leakage directly during the first postoperative days. However, even if over-sewing relevantly improves the watertightness of the wound experimentally, further research is needed in vivo to verify if it can also reduce rates of surgical revisions.
Further limitations need to be considered when interpreting the reported findings. The herein reported results are based on the biomechanical analysis of fresh ovine cadaver samples. Although we believe that this limitation does not reduce the validity of our assumptions, human tissue studies are needed to verify the results. The contribution of some factors, such as for example the use of absorbable suture material rather than non-absorbable material, can only be evaluated in living tissue. Furthermore, the complexity of the study set-up and the limited supply of cadavers only allowed a relatively small sample size.
Reproducibility of the measured leakage pressures was difficult to achieve due to carcass characteristics and may explain the relatively wide standard deviations. Only the immediate hydrostatic strength of the suture was measured, long-term leakage properties were not assessed in this model.
Conclusions
With respect to mentioned limitations, we conclude that cross stitches for the fascia, continuous suturing technique for the subcutis closure and preferentially Donati-continuous stitch closure for the skin result in the most watertight closure within this experimental setting. The most important epidural barrier against CSF leakage is the fascial closure. Special attention should be given to close this layer properly. Further, in the case of CSF leakage directly during the first postoperative days bedside over-sewing of the spot of leakage might be valuable approach. However, the proposed wound closure technique is only an addition to a watertight dural closure after incidental durotomies.
Acknowledgments
None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All applicable international, national and institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted. This article does not contain any studies with human participants performed by any of the authors.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Hannallah D, Lee J, Khan M, et al. Cerebrospinal fluid leaks following cervical spine surgery. J Bone Joint Surg Am 2008;90:1101-5. 10.2106/JBJS.F.01114 [DOI] [PubMed] [Google Scholar]
- 2.Saxler G, Krämer J, Barden B, et al. The long-term clinical sequelae of incidental durotomy in lumbar disc surgery. Spine (Phila Pa 1976) 2005;30:2298-302. 10.1097/01.brs.0000182131.44670.f7 [DOI] [PubMed] [Google Scholar]
- 3.Cammisa FP, Jr, Girardi FP, Sangani PK, et al. Incidental durotomy in spine surgery. Spine (Phila Pa 1976) 2000;25:2663-7. 10.1097/00007632-200010150-00019 [DOI] [PubMed] [Google Scholar]
- 4.Wang JC, Bohlman HH, Riew KD. Dural tears secondary to operations on the lumbar spine. Management and results after a two-year-minimum follow-up of eighty-eight patients. J Bone Joint Surg Am 1998;80:1728-32. 10.2106/00004623-199812000-00002 [DOI] [PubMed] [Google Scholar]
- 5.Tosun B, Ilbay K, Kim MS, et al. Management of Persistent Cerebrospinal Fluid Leakage Following Thoraco-lumbar Surgery. Asian Spine J 2012;6:157-62. 10.4184/asj.2012.6.3.157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ruban D, O'Toole JE. Management of incidental durotomy in minimally invasive spine surgery. Neurosurg Focus 2011;31:E15. 10.3171/2011.7.FOCUS11122 [DOI] [PubMed] [Google Scholar]
- 7.Guerin P, El Fegoun AB, Obeid I, et al. Incidental durotomy during spine surgery: incidence, management and complications. A retrospective review. Injury 2012;43:397-401. 10.1016/j.injury.2010.12.014 [DOI] [PubMed] [Google Scholar]
- 8.Than KD, Wang AC, Etame AB, et al. Postoperative management of incidental durotomy in minimally invasive lumbar spinal surgery. Minim Invasive Neurosurg 2008;51:263-6. 10.1055/s-0028-1082313 [DOI] [PubMed] [Google Scholar]
- 9.Dafford EE, Anderson PA. Comparison of dural repair techniques. Spine J 2015;15:1099-105. 10.1016/j.spinee.2013.06.044 [DOI] [PubMed] [Google Scholar]
- 10.Ghobrial GM, Maulucci CM, Viereck MJ, et al. Suture Choice in Lumbar Dural Closure Contributes to Variation in Leak Pressures: Experimental Model. Clin Spine Surg 2017;30:272-5. 10.1097/BSD.0000000000000169 [DOI] [PubMed] [Google Scholar]
- 11.Faulkner ND, Finn MA, Anderson PA. Hydrostatic comparison of nonpenetrating titanium clips versus conventional suture for repair of spinal durotomies. Spine (Phila Pa 1976) 2012;37:E535-9. 10.1097/BRS.0b013e31824cf756 [DOI] [PubMed] [Google Scholar]
- 12.Finn MA, Faulkner ND, Hetzel SJ, et al. Spinal duraplasty materials and hydrostasis: a biomechanical study: laboratory investigation. J Neurosurg Spine 2011;15:422-7. 10.3171/2011.5.SPINE10851 [DOI] [PubMed] [Google Scholar]
- 13.Narotam PK, José S, Nathoo N, et al. Collagen matrix (DuraGen) in dural repair: analysis of a new modified technique. Spine (Phila Pa 1976) 2004;29:2861-7; discussion 2868-9. 10.1097/01.brs.0000148049.69541.ad [DOI] [PubMed] [Google Scholar]
- 14.Goodkin R, Laska LL. Unintended "incidental" durotomy during surgery of the lumbar spine: medicolegal implications. Surg Neurol 1995;43:4-12; discussion 12-4. 10.1016/0090-3019(95)80031-B [DOI] [PubMed] [Google Scholar]
- 15.Abualenain J, Ranniger C, Jacob D. Measurement of CSF opening pressure during lumbar puncture in the sitting position in the Emergency Department. Acad Emerg Med 2011;18:244. [Google Scholar]
- 16.Sansur CA, Heiss JD, DeVroom HL, et al. Pathophysiology of headache associated with cough in patients with Chiari I malformation. J Neurosurg 2003;98:453-8. 10.3171/jns.2003.98.3.0453 [DOI] [PubMed] [Google Scholar]
- 17.Williams B. On the pathogenesis of syringomyelia: a review. J R Soc Med 1980;73:798-806. 10.1177/014107688007301109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hawk MW, Kim KD. Review of spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg Focus 2000;9:e5. 10.3171/foc.2000.9.1.5 [DOI] [PubMed] [Google Scholar]
- 19.Couture D, Branch CL., Jr Spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg Focus 2003;15:E6. 10.3171/foc.2003.15.6.6 [DOI] [PubMed] [Google Scholar]
- 20.Solomon P, Sekharappa V, Krishnan V, et al. Spontaneous resolution of postoperative lumbar pseudomeningoceles: A report of four cases. Indian J Orthop 2013;47:417-21. 10.4103/0019-5413.114937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tu A, Tamburrini G, Steinbok P. Management of postoperative pseudomeningoceles: an international survey study. Childs Nerv Syst 2014;30:1791-801. 10.1007/s00381-014-2501-9 [DOI] [PubMed] [Google Scholar]
- 22.Eismont FJ, Wiesel SW, Rothman RH. Treatment of dural tears associated with spinal surgery. J Bone Joint Surg Am 1981;63:1132-6. 10.2106/00004623-198163070-00010 [DOI] [PubMed] [Google Scholar]
- 23.Kotani Y, Abumi K, Ito M, et al. Neurological recovery after surgical treatment of giant cervical pseudomeningoceles extending to lumbar spine associated with previous brachial plexus injury. Eur Spine J 2010;19 Suppl 2:S206-10. 10.1007/s00586-010-1387-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Waisman M, Schweppe Y. Postoperative cerebrospinal fluid leakage after lumbar spine operations. Conservative treatment. Spine (Phila Pa 1976) 1991;16:52-3. 10.1097/00007632-199101000-00010 [DOI] [PubMed] [Google Scholar]


