Abstract
Currently, clinical practice recommendations regarding patients in need of emergent lumbar puncture who are taking direct oral anticoagulants (DOACs) are based upon expert opinion, as evidence-based guidelines are unavailable. We present the case of an 80-year-old Caucasian lady who underwent diagnostic lumbar puncture for presumed meningitis while on therapeutic apixaban for nonvalvular atrial fibrillation. She was subsequently found to have bilateral subdural hematomas. This case report reviews both the current criteria for computerized tomography brain imaging prior to lumbar puncture as well as the bleeding risks of lumbar puncture while on a DOAC.
Keywords: Anticoagulation, Apixaban, Intracranial hemorrhage, Lumbar puncture
Introduction
There are no evidenced-based guidelines regarding the performance of lumbar puncture (LP) in patients taking direct oral anticoagulants (DOACs). Available data suggests a significantly lower risk of major bleeding complications (and specifically of intracranial bleeding) with the use of DOACs as compared with warfarin [1]. Based on the pharmacokinetic profile of DOACs, expert opinion has suggested that when a diagnostic LP is indicated, physicians should postpone the LP by at least 24 h if possible, but to proceed with the LP without delay if the indication is truly emergent [2, 3]. Stronger guidelines exist for DOAC management in patients undergoing spinal or epidural anesthesia [4]. Here, we present a case of life-threatening intracranial bleeding which was detected following diagnostic LP that occurred in a patient taking apixaban without periprocedural interruption.
Case Presentation
An 80-year-old female with a history of hypertension, hyperlipidemia, hypothyroidism, migraine headaches, and paroxysmal nonvalvular atrial fibrillation presented to our hospital with a 2-day history of new-onset, severe, stabbing headaches over her left frontal scalp. Three days prior to her presentation at our institution, she had presented to an outside Emergency Department (ED) with 24 h of fevers, chills, as well as a low-grade generalized headache. Physical examination at that time revealed a temperature of 100.8°F, a body weight of 72 kg, a stiff neck, and mild photophobia. Initial investigations revealed a white blood cell (WBC) count of 18.1 × 103 cells/μL, platelet count of 235 × 103 cells/μL, creatinine of 0.8 mg/dL, normal urinalysis, normal chest X-ray, negative flu swab, and normal computerized tomography (CT) imaging of the abdomen/pelvis. CT of the head was done, which revealed no signs of stroke, intracranial hemorrhage, intracranial masses, hydrocephalus, or signs of increased intracranial pressure. She had no history of central nervous system disease and did not take any immunosuppressive medication. There was no report of altered consciousness, focal neurological deficits, or papilledema on exam. As other acute causes of headache had been ruled out and due to the concern for meningitis, she immediately underwent an urgent diagnostic LP in the ED. Approximately 12–16 mL of cerebrospinal fluid (CSF) was removed for testing (4 vials of 3–4 mL each). LP was performed without complication and revealed a CSF WBC count of 2, a red blood cell count of 10, and no bacteria on Gram stain. The CSF was negative for herpes simplex virus. The patient was diagnosed with a mild systemic infection, likely viral, and discharged on oral ciprofloxacin 500 mg twice daily for 7 days.
The patient was taking apixaban 5 mg twice daily for stroke prevention and had taken her last dose on the morning of admission, approximately 7 h prior to the LP. This was reflected in the laboratory analysis showing an international normalized ratio (INR) of 1.47, a prothrombin time of 16.3 s, and activated partial thromboplastin time of 26.4 s. Anti-Xa level was not checked. Apixaban was resumed without interruption after her discharge, and she took her evening dose approximately 5 h after the LP.
On the following day (24 h post-LP), she developed a new, severe headache which was different completely in character from the one she had presented with the day prior to the outside ED. She described it as a sharp stabbing pain, located over her left frontal scalp, somewhat relieved when lying flat. She contacted the outside ED by telephone and described her symptoms to them. She was informed that she likely had developed a post-LP headache and was instructed to take acetaminophen for the pain and return to the ED if her symptoms worsened.
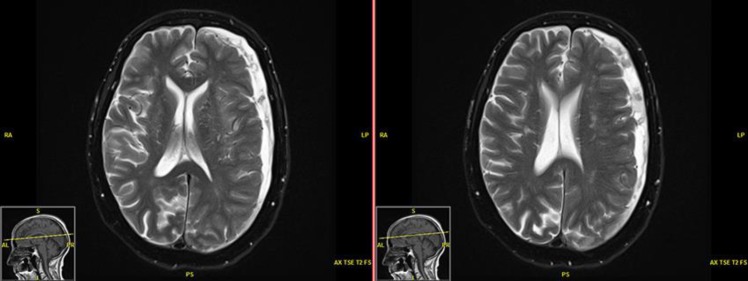
Her headache continued to worsen over the next 48 h. By the time she presented to our ED (72 h post-LP), she was complaining of 10/10 headache as well as interval development of gait instability, loss of balance, generalized weakness, and nausea. Upon admission, vital signs were normal. Physical exam revealed a Glasgow coma scale of 15 and no focal neurologic deficits. Laboratory analysis revealed normal WBC count; her coagulation profile was consistent with the use of apixaban, with an INR of 1.3, prothrombin time of 16.0 s, and activated partial thromboplastin time of 39.8 s. Platelet count at this time was 203 × 103 cells/μL. Creatinine remained stable at 0.8 mg/dL. Noncontrasted CT of the brain revealed bilateral subdural hematomas with features of acute bleeding. The left frontal hematoma measured approximately 14.2 mm, while the right frontal hematoma was about 11.9 mm. These findings were confirmed by MRI (Fig. 1).
Fig. 1.
MRI of the brain demonstrating bilateral subdural hematomas.
Initially, conservative management was attempted, with discontinuation of apixaban and symptomatic treatment with acetaminophen, gabapentin, and ondansetron. However, her headache continued to worsen, and she therefore underwent evacuation of the subdural hematomas via left burr hole on hospital day 3.
Postoperatively, the patient had remarkable improvement in her headache and associated symptoms. Serial CT scan also demonstrated interval improvement. She was discharged home on hospital day 10 with home healthcare for rehabilitation with aspirin 81 mg daily. Her aspirin dose was increased to 325 mg daily 1 month after discharge.
Four months after discharge, her case is still actively being discussed in detail amongst the neurology, cardiology, and neurosurgery services; with specific attention as to whether or not to restart anticoagulation. Ultimately, the deployment of a left atrial appendage closure (WATCHMAN) device was recommended to the patient as the preferred option; however, the patient has thus far deferred this procedure as of the time of this writing. She has a CHADS2VASC score of 4 implying a 5′ annual stroke risk, and a HASBLED score of 3 implying a 5.8′ annual bleeding risk. The current decision is to continue aspirin 325 mg and avoid anticoagulation, although this decision may continue to evolve based upon the patient's preferences.
Discussion
We have presented the case of a woman with nonvalvular atrial fibrillation on therapeutic anticoagulation with apixaban for stroke prevention, who suffered bilateral subdural hematoma after an LP. This case highlights the importance of head imaging prior to LP in patients on anticoagulation in order to rule out intracranial causes of headache, including increased intracranial pressure and intracranial hemorrhage. It also provides an opportunity to review the indications for head CT prior to LP, LP safety in a patient on anticoagulation, and the importance of head imaging when a patient has a change in headache symptoms.
First, the question arises if CT imaging of the head should have been obtained upon initial presentation to the outside ED prior to LP. As our patient was on oral anticoagulation with apixaban and presented with a headache, a head CT without contrast to rule out intracranial hemorrhage was warranted. Although there is evidence that apixaban dosed at 5 mg twice daily does not carry an increased risk of intracranial hemorrhage as compared with aspirin [5], most providers in the emergency setting would agree that intracranial hemorrhage is a possibility and would assess with head imaging. As for the need for head imaging prior to LP in patients not on anticoagulation, the current evidence supports imaging only under certain circumstances. The traditional criteria espoused by the Infectious Disease Society of America (IDSA) for patients with suspected acute bacterial meningitis who require CT of the head before undergoing LP are as follows: immunocompromised, known disease of the central nervous system, new-onset seizure, altered level of consciousness, focal neurologic deficit, or papilledema [6]. The patient had none of these criteria by report of the outside ED. Recently, there have been efforts to even further decrease utilization of CT imaging prior to LP in patients suspected to have bacterial meningitis [6, 7]. This is based largely on data indicating that this sequence of testing significantly delays antibiotic administration, which in turn has been clearly tied to worse outcomes in this disease [6, 7]. In addition, a recent review of the literature sheds doubt on both the age-old premises that an LP increases the risk of brainstem herniation as well as the assumption that a head CT can aptly predict those who are at increased risk of brainstem herniation [6]. This evidence would imply that the use of CT imaging for these indications may be an antiquated practice. With the lack of any of the IDSA criteria for CT and accounting for the significant harm that can be done by delaying antibiotic therapy, one can argue that in this patient's case, it would have been clinically justifiable not to obtain a CT immediately if our patient had not been on anticoagulation.
The second question that arises is focused on the necessity of an immediate LP in this case. Currently, there is a lack of clinical evidence upon which to base management regarding patients on oral anticoagulants who require an urgent LP. However, the American Society of Regional Anesthesia and Pain Medicine recently released evidence-based guidelines regarding the use of regional anesthesia in patients receiving anticoagulation [4]. While these guidelines are directed at spinal blocks and epidural catheters, with the major adverse outcome being spinal hematoma, the authors state that they “may also serve as a resource for […] similar procedures (e.g., […] lumbar puncture)” [4]. These guidelines recommend a delay of 72 h after the last dose of any direct oral anti-factor Xa agent prior to neuraxial puncture [4]. They also suggest that if proceeding with LP before the recommended 72 h window, a calibrated anti-factor Xa assay be obtained to evaluate the degree of anticoagulant effect [4]. This recommendation is largely based on pharmacokinetic data, as there have been no reports of spinal hematoma associated with neuraxial anesthesia in patients treated with apixaban [4].
A recent expert opinion paper from Brazil directly addressed the question of LP in patients on DOACs [3]. While acknowledging the lack of evidence, Domingues et al. [3] suggest that the anticoagulant should be held at least 24 h prior to the LP in patients with normal renal function, and at least 72 h prior in patients with impaired renal function. If an LP is crucial to patient care, providers should consider rapid reversal of the DOAC in emergent situations in order to minimize bleeding risk [8]. Unfortunately, the current cost of andexanet alfa, the direct reversal agent for apixaban, is quite high, running USD 25,000–50,000 per patient treatment [9]. This excessive cost may deter providers from using andexanet alfa prior to LP.
Providers should also consider removing the lowest amount of CSF necessary in order to run their testing. This is because the mechanism of subdural hematoma formation after CSF removal is often subdural vein rupture [10]. The walls of the subdural bridging veins are known to be more fragile than the epidural veins, and the removal of larger volumes of CSF from the subdural space results in stretching and tearing of these veins, resulting in a hematoma [11]. Anticoagulation with DOACs, as is the case with most hematomas, can increase the amount of bleeding in these situations, leading to catastrophic outcomes. Given the available literature, this patient should not have undergone diagnostic LP upon admission while still on therapeutic apixaban. More appropriately, she should have been treated empirically with antibiotics and re-evaluated for potential diagnostic LP at least 24 h after the last dose of apixaban, preferably waiting 72 h if possible.
Providers might be eager to perform LPs in cases of suspected bacterial meningitis in order to increase the yield of CSF cultures to identify an organism. This is because delay of LP greater than 24 h from the time of initiation of antibiotics rarely yields positive culture results [12]. But bacterial cultures of CSF are not the only way to detect bacterial organisms.
Most labs can test for bacteria in CSF using polymerase chain reactions (PCR) and immunochromatographic testing (ICT). Brink et al. [12] found that PCR testing for bacterial meningitis was positive in 89′ of patients on days 1–3, 70′ of patients on days 4–6, and 33′ of patients on days 7–10. The same study shows that ICT for pneumococcal meningitis was positive in 88′ of patients on days 1–3, 90′ of patients on days 4–6, and 75′ of patients on days 7–10 [12]. So, if a delay of LP is necessary due to therapeutic anticoagulation, PCR and ICT can still be very helpful in identifying the bacterial organism long after treatment with i.v. antibiotics has begun.
The final question that arises looks at whether the patient should have been seen immediately by the emergency department the day after her LP when she first developed a worsening headache of different character. If an LP has been performed on a patient treated with a DOAC within 72 h of the last dose, a very high suspicion for intracranial or neuraxial bleeding should be held by the clinician and an urgent CT of the head should be obtained. New or worsening headache, altered mentation, new-onset seizure, focal neurologic deficits, or signs of increased intracranial pressure all would warrant immediate head imaging. Similarly, urgent MRI of the spine should be obtained for new or worsening back pain, leg numbness or weakness, or bowel/bladder dysfunction. When she described worsening of her headache on the day following LP, this should have prompted immediate CT imaging.
Conclusion
This case report highlights the importance of understanding the criteria of CT brain imaging prior to an LP, the optimal time frame to hold a DOAC in order to minimize the risk of procedure-related bleeding, and the vital importance of head imaging when a neuroclinical change in a patient's status occurs under these circumstances.
Statement of Ethics
The patient provided both oral and written informed consent for the publishing of this report.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors did not receive any funding support.
Author Contributions
P.V. contributed to the diagnosis, physical examination, and testing of the patient, wrote the first draft, and worked on the syndromic description. M.J.M. reviewed, edited, and corrected the draft, developed the theoretical time frame, and modified the Discussion. All authors read and approved the final manuscript.
Acknowledgement
We would like to thank Dr. Jeffrey Garland who helped review the initial case and gave us comments and advice.
References
- 1.Gómez-Outes A, Terleira-Fernández AI, Calvo-Rojas G, Suárez-Gea ML, Vargas-Castrillón E. Dabigatran, Rivaroxaban, or Apixaban versus Warfarin in Patients with Nonvalvular Atrial Fibrillation: A Systematic Review and Meta-Analysis of Subgroups. Thrombosis. 2013;2013:640723. doi: 10.1155/2013/640723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baron TH, Kamath PS, McBane RD. Management of antithrombotic therapy in patients undergoing invasive procedures. N Engl J Med. 2013 May;368((22)):2113–24. doi: 10.1056/NEJMra1206531. [DOI] [PubMed] [Google Scholar]
- 3.Domingues R, Bruniera G, Brunale F, Mangueira C, Senne C. Lumbar puncture in patients using anticoagulants and antiplatelet agents. Arq Neuropsiquiatr. 2016 Aug;74((8)):679–86. doi: 10.1590/0004-282X20160098. [DOI] [PubMed] [Google Scholar]
- 4.Horlocker TT, Vandermeuelen E, Kopp SL, et al. Regional Anesthesia in the Patient Receiving Antithrombotic or Thrombolytic Therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Fourth Edition) Reg Anesth Pain Med. 2018;3((43)):263–309. doi: 10.1097/AAP.0000000000000763. [DOI] [PubMed] [Google Scholar]
- 5.Huang WY, Singer DE, Wu YL, Chiang CE, Weng HH, Lee M, et al. Association of Intracranial Hemorrhage Risk With Non-Vitamin K Antagonist Oral Anticoagulant Use vs Aspirin Use: A Systematic Review and Meta-analysis. JAMA Neurol. 2018 Dec;75((12)):1511–8. doi: 10.1001/jamaneurol.2018.2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.April MD, Long B, Koyfman A. Emergency Medicine Myths: Computed Tomography of the Head Prior to Lumbar Puncture in Adults with Suspected Bacterial Meningitis - Due Diligence or Antiquated Practice? J Emerg Med. 2017 Sep;53((3)):313–21. doi: 10.1016/j.jemermed.2017.04.032. [DOI] [PubMed] [Google Scholar]
- 7.Glimaker M, Johansson B, Orjan G, et al. Adult Bacterial Meningitis: Earlier Treatment and Improved Outcome following Guideline Revision prompting Prompt Lumbar Puncture. CID. 2015;8((60)):1162–9. doi: 10.1093/cid/civ011. [DOI] [PubMed] [Google Scholar]
- 8.Steiner T, Weitz JI, Veltkamp R. Anticoagulant-Associated Intracranial Hemorrhage in the Era of Reversal Agents. Stroke. 2017 May;48((5)):1432–7. doi: 10.1161/STROKEAHA.116.013343. [DOI] [PubMed] [Google Scholar]
- 9.Beik N, Reddy P, Sylvester KW, Connell NT, Giugliano RP, Piazza G, et al. Andexanet Alfa (Andexxa) Formulary Review. Crit Pathw Cardiol. 2019 Jun;18((2)):66–71. doi: 10.1097/HPC.0000000000000177. [DOI] [PubMed] [Google Scholar]
- 10.Loo CC, Dahlgren G, Irestedt L. Neurological complications in obstetric regional anaesthesia. Int J Obstet Anesth. 2000 Apr;9((2)):99–124. doi: 10.1054/ijoa.1999.0347. [DOI] [PubMed] [Google Scholar]
- 11.Yamashima T, Friede RL. Why do bridging veins rupture into the virtual subdural space? J Neurol Neurosurg Psychiatry. 1984 Feb;47((2)):121–7. doi: 10.1136/jnnp.47.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brink M, Welinder-Olsson C, Hagberg L. Time window for positive cerebrospinal fluid broad-range bacterial PCR and Streptococcus pneumoniae immunochromatographic test in acute bacterial meningitis. Infect Dis (Lond) 2015;47((12)):869–77. doi: 10.3109/23744235.2015.1078907. [DOI] [PubMed] [Google Scholar]