Abstract
We report the case of a 56-year-old man who presented with dysphagia and weight loss. An esophagoduodenoscopy revealed a severe esophageal stricture in the distal esophagus. After surgical resection, the final pathologic analysis revealed that the tumor was comprised of benign-appearing fibroinflammatory cells with an increase and predominance of IgG4-positive plasma cells. He did not, however, have any other symptoms indicative of systemic autoimmune disease or connective tissue disorders. Histologically, abundant infiltration of IgG4-positive plasma cells and lymphocytes was observed. The patient was diagnosed with IgG4-related disease, definitive, with esophageal involvement.
Keywords: IgG4-related disease, Esophagus, Autoimmune esophagitis
Introduction
Immunoglobulin G4-related disease (IgG4-RD) is an immune-mediated fibroinflammatory condition that can affect multiple organs and lead to tumefactive, tissue-destructive lesions and organ failure [1]. The disease was not recognized as a systemic condition until 2003 when extrapancreatic manifestations were identified in patients with autoimmune pancreatitis [2]. Autoimmune pancreatitis had been linked to elevated serum IgG4 concentrations as early as 2001 [3]. Over the last decade, the disease has become recognized as a unified systemic disorder that links various organ conditions once considered to be unrelated [4]. Recognition of the disease entity is vital due to its frequent misdiagnosis as a malignant tumor, which can result in unnecessary treatment measures. Many organs can be involved in the disease such as the pancreas, biliary tract, salivary glands, lymph nodes, thyroid, kidneys, lung, skin, prostate, and aorta [1, 5]. Involvement of the esophagus is extremely rare [6, 7, 8].
Case Report
Three years ago, A 56-year-old Asian man presented to our clinic with debilitating dysphagia involving solids for several months. The patient had a heavy smoking history (3 packs/day, 30 years), but no alcohol drinking history. He had uncontrolled diabetes mellitus over 10 years, and underwent coronary artery bypass graft surgery 8 years previously.
The patient had previously visited a local clinic with heartburn and dysphagia, where he underwent esophagogastroduodenoscopy (EGD) without a biopsy. EGD revealed esophageal stricture and mucosal abrasion. When initially referred to our clinic, provisional diagnosis included gastroesophageal reflux disease, thus, proton pump inhibitor therapy began at first visit. We planned further evaluations like computed tomography (CT), barium swallow, esophageal manometry, and endoscopic biopsy, but he constantly refused admission or further evaluations and was lost to follow-up for 18 months because of his poor economic status.
As time went by, his dysphagia became aggravated and was associated with weight loss. He revisited the clinic with a body weight loss of 7 kg (47 kg at visit; usual weight 54 kg) and dysphagia involving both solids and liquids; he could barely swallow a liquid diet and had difficulty even in swallowing pills.
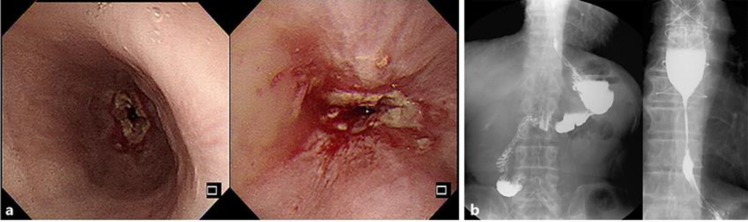
Physical examination revealed no superficial lymph nodes. A blood test showed that complete blood cell counts, creatinine, and liver function tests were normal. EGD showed severe esophageal stricture at 32 cm from incisors and mucosal erosions with exudate (Fig. 1a). Biopsies were performed at erosions (only 2 pieces of tissue). Biopsy results showed necroinflammatory exudate. Barium swallow (Fig. 1b) showed stricture in the mid-to-distal esophagus and delayed contrast passage. CT scan (Fig. 2) demonstrated an esophageal lesion, length about 70 mm, in the lower esophagus with marked luminal narrowing and wall thickening, without enlarged lymph nodes. An abdominopelvic CT scan of the pancreas was performed and showed normal.
Fig. 1.
a Esophagoduodenoscopy showed severe esophageal stricture and mucosal erosions with exudate. The 5-mm-diameter scope could not even pass at the stricture site. b Barium swallow (esophagography) showed about 4-cm-length stricture in the mid-to-distal esophagus and delayed contrast passage at the stricture site.
Fig. 2.
CT scan demonstrated a distal esophageal lesion. The esophageal lesion was in the lower esophagus with marked luminal narrowing and wall thickening without enlarged lymph nodes.
Previous proton pump inhibitor therapy was not effective and the lesion was long. Findings of body weight loss of 7 kg and wall thickening of the esophagus might suggest malignancy, but no lymph node enlargement was revealed on CT scan. There was a previous CT scan a year previously, because of coronary artery bypass graft history. In the previous scan, there was no esophageal wall thickening or enlarged lymph nodes. To evaluate esophageal motility disorders, esophageal manometry was planned but the stricture was too narrow for a catheter to pass.
As the disease showed benign features (benign biopsy, no lymph node enlargement), we suggested esophageal dilatation rather than surgical resection. But the patient wanted immediate resolution of symptoms and refused the step-wise procedure. Thus, the surgical measure Ivor-Lewis esophagectomy was performed. His postoperative course was uneventful, and he was discharged on postoperative day 10. The oral intake of soft diet was tolerable at the time of discharge.
Upon gross examination, the resected specimens showed marked wall thickening and stricture with mucosal erosion in the lower esophagus (Fig. 3a). Histologically (Fig. 3b, c), scattered lymphoid follicles and prominent muscular hypertrophy were observed in the submucosal layer. Dense lymphocyte and plasma cell infiltration was observed in the submucosal layer and the proper muscle layer. Immunohistochemistry (Fig. 3d) revealed IgG4+ plasma cells at a level of >50/HPF and a ratio of >90′ IgG4+/IgG+ plasma cells. Postoperative serum level of IgG was 1,450 mg/dL (normal range: 700–1,600) and IgG4 was 171.0 mg/dL. Based on the comprehensive diagnostic criteria for IgG4-RD [9], He was diagnosed with an IgG4-RD, definitive, with esophageal involvement.
Fig. 3.
a Upon gross examination, the resected specimens showed wall thickening and stricture with mucosal erosion in the lower esophagus. b Scattered lymphoid follicles and muscular hypertrophy were observed in the submucosal layer. c Most of the cells in the infiltrate are plasma cells. d IgG4 stains the majority of the plasma cells in the field. Immunohistochemistry revealed IgG4+ plasma cells at a level of >50/HPF and a ratio of >90′ IgG4+/IgG+ plasma cells. Hematoxylin-eosin. Original magnification, ×40 (b), ×200 (c). IgG, immunoperoxidase. Original magnification, ×200 (d,left). IgG4, immunoperoxidase. Original magnification, ×200 (d,right).
Following achievement of remission by surgical method, the patient received maintenance prednisolone therapy (30 mg/day), which was slowly tapered. His dysphagia improved greatly and he returned to his usual weight (54 kg). After prednisolone therapy, follow-up serum IgG4 level dropped to 48.9 mg/dL and prednisolone therapy was tapered. Serum IgG4 level sustained a similar level (52.1 mg/dL after 6 months; 49.0 mg/dL after 11 months).
Discussion
In this case, preoperative endoscopic biopsies revealed necroinflammatory exudate. It might be that the biopsies were too shallow and few to detect unique pathologic features. if the specialist was suspicious for malignancy, biopsies would involve 5 or more pieces of tissue and would be fairly deep. However, even if we had tried endoscopic dilatation first, due to a high degree of fibrosis as the result of long-standing disease, surgical measures might have been inevitable.
Based on the comprehensive diagnostic criteria for IgG4-RD [9], a diagnosis of IgG4-RD is definitive in patients with organ enlargement or organ dysfunction, mass or nodular lesions, a serum IgG4 level >135 mg/dL, and histopathological findings of >10 IgG4+ cells/HPF and an IgG4+/IgG+ cell ratio >40′. A diagnosis of IgG4-RD is probable in patients with organ involvement and who fulfill the histopathological criteria without increased serum IgG4 levels. IgG4-RD is a systemic disease characterized by specific histopathologic findings of an intense lymphoplasmacytic infiltrate, storiform fibrosis, and obliterative phlebitis in the presence of predominant IgG4-positive plasma cells [10]. Moreover, a confident pathological diagnosis can be made in the presence of two of the three major histological features [11].
IgG-RD occurring in the esophagus is extremely rare. Previous reports revealed that IgG4-RD with esophagus involvement typically affects middle-aged to elderly patients (mean age was 54.7 ± 16.4 years) and is more common in males. Multiorgan disease may be evident at diagnosis but may also evolve metachronously, over months to years [12].
Glucocorticoids are the first-line agent for remission induction in patients with active, untreated IgG4-RD unless contraindications to such treatment are present [13]. A consensus statement in Japan suggested that prednisolone be tapered over a period of 3–6 months to 5 mg/day, and then continued at a dose between 2.5 and 5 mg/day for up to 3 years. Another approach has been to discontinue glucocorticoids entirely within 3 months [14].
The degree of fibrosis within the affected organs is a major determinant of treatment responsiveness. Untreated IgG4-RD often progresses from lymphoplasmacytic inflammation to extensive fibrosis. Patients in whom fibrosis has become well established are less likely to have a response to glucocorticoids and rituximab, but treatment responses have been reported in some patients with apparently widespread fibrosis [15].
Conclusion
Since IgG4-RD is a recently described disorder, it is possible that IgG4-related esophageal disease is an underdiagnosed or misdiagnosed disease entity. Diagnosis remains difficult and is best done through sufficient biopsies and detailed histologic analysis. A high index of suspicion is necessary to accurately make the diagnosis prior to resection.
Statement of Ethics
The published research is compliant with the guidelines for human studies and animal welfare regulations.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
No funding was received for this study.
Author Contributions
Sung Wook Jang and Hyun Deok Shin were involved in the literature review and creation of the manuscript. Min Ho Jeon was involved in editing the manuscript.
References
- 1.Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012 Feb;366((6)):539–51. doi: 10.1056/NEJMra1104650. Available from: http://www.nejm.org/doi/10.1056/NEJMoa1108895. [DOI] [PubMed] [Google Scholar]
- 2.Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003;38((10)):982–4. doi: 10.1007/s00535-003-1175-y. [DOI] [PubMed] [Google Scholar]
- 3.Hamano H, Kawa S, Horiuchi A, Unno H, Furuya N, Akamatsu T, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001 Mar;344((10)):732–8. doi: 10.1056/NEJM200103083441005. [cited 2019 Jun 25] Available from: http://www.nejm.org/doi/abs/10.1056/NEJM200103083441005. [DOI] [PubMed] [Google Scholar]
- 4.Stone JH, Khosroshahi A, Deshpande V, Chan JK, Heathcote JG, Aalberse R, et al. IgG4-Related Disease: Recommendations for the Nomenclature of this Condition and its Individual Organ System Manifestations. Arthritis Rheum. 2012;64((10)):3061. doi: 10.1002/art.34593. [cited 2019 Jun 19] Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5963880/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neild GH, Rodriguez-Justo M, Wall C, Connolly JO. Hyper-IgG4 disease: report and characterisation of a new disease. BMC Med. 2006 Oct;4((1)):23. doi: 10.1186/1741-7015-4-23. [cited 2019 Jun 19] Available from: http://www.ncbi.nlm.nih.gov/pubmed/17026742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mori S, Tahashi Y, Uchida K, Ikeura T, Danbara N, Wakamatsu T, et al. Sclerosing Esophagitis with IgG4-positive Plasma Cell Infiltration. Intern Med. 2017 Nov;56((22)):3023–6. doi: 10.2169/internalmedicine.8095-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Obiorah I, Hussain A, Palese C, Azumi N, Benjamin S, Ozdemirli M. IgG4-related disease involving the esophagus: a clinicopathological study. Dis Esophagus. 2017 Dec;30((12)):1–7. doi: 10.1093/dote/dox091. [cited 2019 Jun 19] Available from: http://academic.oup.com/dote/article/30/12/1/4096643/IgG4related-disease-involving-the-esophagus-a. [DOI] [PubMed] [Google Scholar]
- 8.Yang L, Jin P, Sheng J. Immunoglobulin G4-related disease (IgG4-RD) affecting the esophagus, stomach, and liver. Endoscopy [Internet] 2015 Mar 3;47((S 01)):E96–E97. doi: 10.1055/s-0034-1391252. [cited 2019 Jun 19]. Available from: http://www.thieme-connect.de/DOI/DOI?10.1055/s-0034-1391252. [DOI] [PubMed] [Google Scholar]
- 9.Umehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol. 2012 Feb;22((1)):21–30. doi: 10.1007/s10165-011-0571-z. [cited 2019 Jun 18] Available from: http://link.springer.com/10.1007/s10165-011-0571-z. [DOI] [PubMed] [Google Scholar]
- 10.Weindorf SC, Frederiksen JK. IgG4-related disease: A reminder for practicing pathologists. Arch Pathol Lab Med. 2017 Nov;141((11)):1476–83. doi: 10.5858/arpa.2017-0257-RA. [DOI] [PubMed] [Google Scholar]
- 11.Deshpande V, Zen Y, Chan JK, Yi EE, Sato Y, Yoshino T, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012 Sep;25((9)):1181–92. doi: 10.1038/modpathol.2012.72. [cited 2019 Jun 19] Available from: http://www.ncbi.nlm.nih.gov/pubmed/22596100. [DOI] [PubMed] [Google Scholar]
- 12.Kamisawa T, Shimosegawa T, Okazaki K, Nishino T, Watanabe H, Kanno A, et al. Standard steroid treatment for autoimmune pancreatitis. Gut. 2009 Nov;58((11)):1504–7. doi: 10.1136/gut.2008.172908. [cited 2019 Jun 23] Available from: http://www.ncbi.nlm.nih.gov/pubmed/19398440. [DOI] [PubMed] [Google Scholar]
- 13.Khosroshahi A, Wallace ZS, Crowe JL, Akamizu T, Azumi A, Carruthers MN, et al. Second International Symposium on IgG4-Related Disease International consensus guidance statement on the management and treatment of IgG4-related disease. Arthritis Rheumatol. 2015 Jul;67((7)):1688–99. doi: 10.1002/art.39132. [DOI] [PubMed] [Google Scholar]
- 14.Ghazale A, Chari ST, Zhang L, Smyrk TC, Takahashi N, Levy MJ, et al. Immunoglobulin G4-associated cholangitis: clinical profile and response to therapy. Gastroenterology. 2008 Mar;134((3)):706–15. doi: 10.1053/j.gastro.2007.12.009. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0016508507021701. [DOI] [PubMed] [Google Scholar]
- 15.Raissian Y, Nasr SH, Larsen CP, Colvin RB, Smyrk TC, Takahashi N, et al. Diagnosis of IgG4-related tubulointerstitial nephritis. J Am Soc Nephrol. 2011 Jul;22((7)):1343–52. doi: 10.1681/ASN.2011010062. [cited 2019 Jun 23] Available from: http://www.ncbi.nlm.nih.gov/pubmed/21719792. [DOI] [PMC free article] [PubMed] [Google Scholar]