Abstract
Terbinafine has proved to treat numerous fungal infections, including onychomycosis, successfully. Due to its liver metabolization and dependency on the cytochrome P450 enzyme complex, undesirable drug interaction are highly probable. Additionally to drug interactions, the treatment is long, rising the chances of the appearance of side effects and abandonment. Pharmacokinetic data suggest that terbinafine maintains a fungicidal effect within the nail up to 30 weeks after its last administration, which has aroused the possibility of a pulse therapy to reduce the side effects while treating onychomycosis. This study’s goal was to evaluate the effectiveness of three different oral terbinafine regimens in treating onychomycosis due to dermatophytes. Sixty-three patients with onychomycosis were sorted by convenience in three different groups. Patients from group 1 received the conventional terbinafine dose (250 mg per day for 3 months). Group 2 received a monthly week-long pulse-therapy dose (500 mg per day for 7 days a month, for 4 months) and group 3 received a 500 mg/day dose for 7 days every 3 months, totaling four treatments. There were no statistical differences regarding the effectiveness or side effects between the groups. Conclusion: A quarterly terbinafine pulse regimen can be a possible alternative for treating onychomycosis caused by dermatophytes.
Keywords: administration, allylamines/terbinafine, Arthrodermataceae/drug effects, drug compounding, humans, onychomycosis, oral, antifungal agents/administration, dosage/adverse effects/pharmacology
1. Introduction
Onychomycosis due to dermatophytes, yeasts, and non-dermatophyte molds comprises 50% of all cases of nail disease [1]. Known individual risk factors for its development are nail trauma, age, smoking, immunosuppression, obesity, psoriasis, and other causes of onychodystrophy, peripheral arterial disease, and diabetes mellitus [2,3,4,5,6]. Male patients have been reported to have more severe and chronic onychomycosis [7].
The susceptibility to onychomycosis is inherited and it is often observed among family members. Some studies revealed the existence of polymorphisms in genes of the major histocompatibility complex related to higher susceptibility to onychomycosis from dermatophytes, particularly haplotypes HLA-DR8 and HLA-DR1 [8,9,10,11]
The estimated global prevalence of onychomycosis is 5.5% [12]. More than 60% of these infections are caused by dermatophytes, mainly Trichophyton rubrum, Trichophyton mentagrophytes, Epidermophyton floccosum, and Microsporum spp. The remaining infections can be due non-dermatophyte molds, predominantly Scopulariopsis brevicaulis, Aspergillus spp., Acremonium, Fusarium sp.p, Alternaria alternata, and Neoscytalidium spp., or to yeasts, such as Candida albicans [13].
Trauma caused by shoes produces toenail changes, especially in people with orthopedic changes that cause faulty poor adaptation of the feet in shoes, that are identical to some onychomycosis at the time of clinical presentation [14]. Most toenails abnormalities are, in fact, due to the pressure exerted by shoes and not by fungi. It has already been observed that the presence of non-dermatophyte molds in a dystrophic nail could be considered a secondary niche of colonization in a nail previously damaged by trauma, rather than onychomycosis [15].
Aside from the high prevalence, onychomycosis has therapeutic challenges. The available therapeutic arsenal is not vast, and there are high rates of resistance and recurrence, making it a noteworthy public health issue [16,17].
Topical and oral antifungals are the treatment options for onychomycosis. Topical therapy is used in children and adults with mild to moderate onychomycosis or for single affected digits. Ciclopirox and amorolfine are the most used topical agents, and recently, tavaborole and efinaconazole have been introduced in North America [18,19,20].
FDA-approved oral treatment for onychomycosis includes terbinafine and itraconazole, and fluconazole is used off-label. Due to fewer collateral effects and higher cure rates, terbinafine is usually preferred over itraconazole [21]. The standard dosage is 250 mg per day for 6 weeks for fingernails or 12 weeks for toenails. [22]. Some pharmacokinetic studies have shown that terbinafine can be detected in the nail plate in concentrations above the minimal inhibitory concentrations for dermatophytes and other fungi 36 weeks post-treatment [23,24,25]. Pulse regimens have been proposed to reduce the side effects and risks of interaction with other medication. Most studies have shown a superior efficacy of terbinafine compared to itraconazole pulse regimens and similar efficacy compared to a conventional terbinafine dose [26,27].
The standard dose for a terbinafine pulse regimen is 500 mg per day for 7 days a month, twice or three times for fingernails and three to four times for toenails [28].
Zaias and Rebell [29] have described considerable terbinafine efficacy utilizing a quarterly pulse therapy regimen for the treatment of distal subungual onychomycosis (DSO) caused by T. rubrum.
We performed an open non-randomized study in which standard terbinafine regimens were compared with a pulse terbinafine regimen of 500 mg/day for 7 days every 3 months to treat onychomycosis caused by dermatophytes.
2. Materials and Methods
2.1. Patients
In total, we included 63 patients (34 women, 29 men) aged between 24 and 70 years who had visited the Dermatology Outpatient’s Clinic at Santa Casa de Curitiba Hospital between August 2013 and July 2016. Those aged 18 years or older and diagnosed with dermatophyte onychomycosis based on clinical manifestations and confirmed using mycological culture were eligible to participate. Patients with less than 25% of the nail affected by the disease, liver or kidney impairment, pregnant or lactating were excluded. All participants signed an informed consent term.
Two measurements were taken of infected nails before, during the appointments, and at the end of each group treatment. The first one was the length of the nail plate from the free edge to the proximal nail fold, and the second one was the length of the visible fungal-infected portion. The percentage of the compromised nail was then calculated.
Data concerning age, sex, occupation, sport activities, comorbidities, and concomitant use of medications were recorded. Patients were divided into three groups, according to their order of attendance.
In Group 1, 20 patients received continuous 250 mg terbinafine for 3 months. In Group 2, 21 patients received a terbinafine 500 mg monthly pulse regimen, for 4 months. In Group 3, 22 patients received terbinafine 500 mg/day for 7 days, every 3 months and completed four pulse regimens.
Patients of Group 1 were asked to attend the hospital monthly. Patients of Group 2 had appointments every 2 months. Patients of Group 3 attended the hospital every 3 months. During the appointments, all patients were examined, questioned concerning any possible side effects, and received a new supply of terbinafine containing 28 tablets.
Mycological cultures were provided for all patients who completed the study.
2.2. Evaluation of Therapeutic Response
The degrees of improvement were classified as follows: total cure (TC), clinical disease-free nail and a negative mycological culture; mycological cure (MC), <25% of nail impairment and a negative mycological culture; clinical improvement (CI), <25% of nail impairment and a positive mycological culture; therapeutic failure (TF), unchanged clinical examination or worsening and a positive mycological culture.
2.3. Statistical Methodology
For the quantitative variables, a comparison between treatments was undertaken using a Kruskal–Wallis non-parametric test, suitable for the analysis of independent samples and variables with interval measurements without normal distribution [30]. For the group comparisons, in relation to the categorical variables, a non-parametric chi-square test was applied. In all tests, a p value of 5% was considered statistically significant.
2.4. Demographic Characteristics
Table 1 shows the patients’ demographic characteristics. A possible occupational relationship refers to occupations that may lead to greater exposure to fungi on the feet or hands, such as those requiring the use of safety shoes and those in which patients had been exposed to humidity, heat, or trauma. Sport activities were also considered, as trauma is a relevant factor in the speed of growth of a nail plate and, therefore, in the recovery of infected nails. Gender, age, previous treatments, which are also relevant factors in a treatment response, were evaluated, as was the concomitant use of other medications that can interact with terbinafine [31].
Table 1.
Demographic characteristics (n = 63).
| Demographic Characteristics | Group 1 | Group 2 | Group 3 | Total |
|---|---|---|---|---|
| 1. Age | ||||
| Average | 47 | 48 | 48.27 | 47.78 |
| n | 20 | 21 | 22 | 63 |
| Minimum | 26 | 27 | 24 | 24 |
| Maximum | 67 | 70 | 70 | 70 |
| 2. Sex | ||||
| Female (%) | 12 (60.00%) | 12 (57.14%) | 10 (45.45%) | 34 |
| Male (%) | 8 (40.00%) | 9 (42.86%) | 12 (54.55%) | 29 |
| Total | 20 | 21 | 22 | 63 |
| 3. Occupation (%) | ||||
| Possible occupational relationship | 6 (30.00%) | 9 (42.86%) | 5 (22.73%) | 20 |
| No possible occupational relationship | 14 (70.00%) | 12 (57.14%) | 17 (77.72%) | 43 |
| Total | 20 | 21 | 22 | 63 |
| 4. Previous Treatment | ||||
| No (%) | 18 (90.00%) | 19 (90.48%) | 22 (100%) | 59 |
| Yes (%) | 2 (10.00%) | 2 (9.52%) | 0 (0.00%) | 4 |
| Total | 20 | 21 | 22 | 63 |
| 5. Sports Activities (%) | ||||
| None (%) | 9 (45.00%) | 17 (80.95%) | 17 (77.27%) | 43 |
| Effect on the feet (%) | 2 (10.00%) | 2 (9.52%) | 0 (0.00%) | 4 |
| No effect on the feet (%) | 9 (45.00%) | 2 (9.52%) | 5 (22.73%) | 16 |
| Total | 20 | 21 | 22 | 63 |
| 6. Use of Medicines | ||||
| No interaction (%) | 14 (70.00%) | 19 (90.48%) | 18 (81.82%) | 51 |
| Antidepressants (%) | 4 (20.00%) | 1 (4.76%) | 1 (4.55%) | 6 |
| Beta-blockers (%) | 1 (5.00%) | 0 (0.00%) | 1 (4.55%) | 2 |
| Immunosuppressants (%) | 1 (5.00%) | 0 (0.00%) | 0 (0.00%) | 1 |
| >1 Possible interaction (%) | 0 (0.00%) | 1 (4.76%) | 2 (9.09%) | 3 |
| Total | 20 | 21 | 22 | 63 |
| 7. Comorbidities | ||||
| None (%) | 13 (65.00%) | 15 (71.43%) | 16 (72.73%) | 44 |
| Diabetes (%) | 0 (0.00%) | 0 (0.00%) | 1 (4.55%) | 1 |
| Obesity (%) | 1 (5.00%) | 1 (4.76%) | 1 (4.55%) | 3 |
| Hypothyroidism (%) | 2 (10.00%) | 1 (4.76%) | 0 (0.00%) | 3 |
| Depression (%) | 2 (10.00%) | 3 (14.29%) | 1 (4.55%) | 6 |
| Immunodeficiency (%) | 1 (5.00%) | 1 (4.76%) | 1 (4.55%) | 3 |
| >1 Comorbidities (%) | 1 (5.00%) | 0 (0.00%) | 2 (9.09%) | 3 |
| Total | 20 | 21 | 22 | 63 |
The isolated fungi in the mycological cultures were Trichophyton sp, T. rubrum, T. mentagrophytes, and Microsporum gypseum (Table 2).
Table 2.
Isolated fungi (n = 63).
| Fungus | Group 1 | Group 2 | Group 3 | Total |
|---|---|---|---|---|
| Trichophyton sp (n, %) | 15 (75.00%) | 13 (61.90%) | 12 (54.55%) | 40 |
| Trichophyton mentagrophytes (n, %) | 2 (10.00%) | 4 (19.05%) | 5 (22.73%) | 11 |
| Trichophyton rubrum (n, %) | 3 (15.00%) | 4 (19.05%) | 4 (18.18%) | 11 |
| Microsporum gypseum (n, %) | 0 (0.00%) | 0 (0.00%) | 1 (4.55%) | 1 |
| Total | 20 | 21 | 22 | 63 |
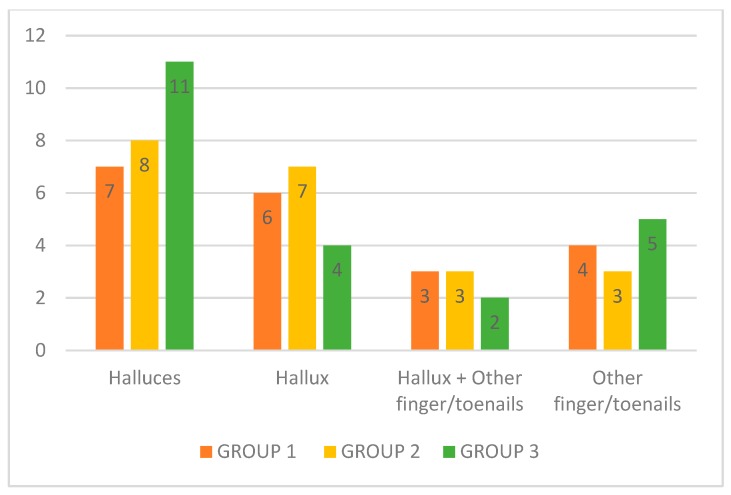
The hallux was the most affected nail (n = 43) in all three groups, followed by the 4th, 5th, and 3rd toenail and the thumbnail (n = 20). There was no significant difference among the groups regarding the distribution of affected fingers or toenails (Figure 1).
Figure 1.
Toenails and fingernails affected (n = 63). Nail disease distribution according to groups before the treatment.
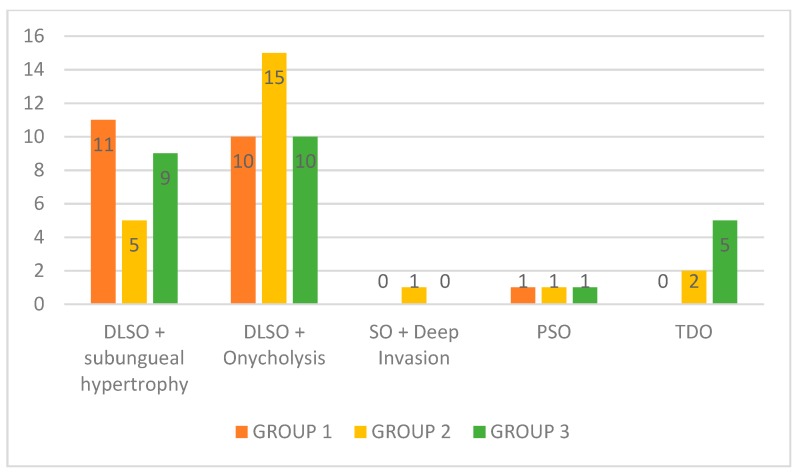
According to the clinical classification proposed by Baran and Hay [32], most patients were identified with a distal lateral subungual onychomycosis (DLSO) with subungual onycholysis (n = 35), followed by DLSO with subungual hypertrophy (n = 25), total dystrophic onychomycosis (TDO) (n = 7), proximal subungual onychomycosis (PSO) (n = 3), and superficial onychomycosis (SO) with deep invasion (n = 1). Nine patients had more than one nail type of onychomycosis in different nails; therefore, for the clinical classification, the sample included 71 affected nails (Figure 2).
Figure 2.
Clinical classification according to groups (n = 71). Clinical classification according to groups before the treatment. DLSO + subungual hypertrophy: distal lateral subungual onychomycosis with subungual hypertrophy; DLSO + Onycholysis: distal lateral subungual onychomycosis with onycholysis; SO + Deep Invasion: superficial onychomycosis with deep invasion; PSO: proximal subungual onychomycosis; TDO: total dystrophic onychomycosis.
3. Results
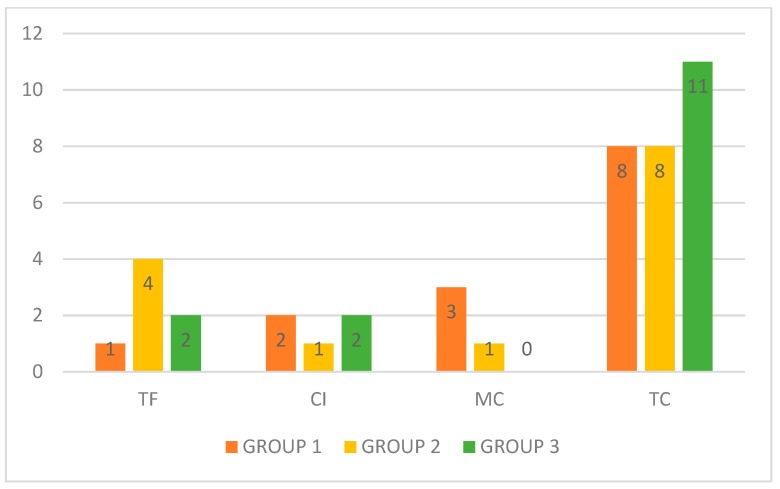
In total, 43 patients completed the study comprising 14, 14, and 15 patients in Groups 1, 2, and 3, respectively. Thirteen (92.86%), 10 (71.43%), and 13 (86.67%) patients from groups 1, 2, and 3, respectively, presented with TC, MC, or CI (Figure 3).
Figure 3.
Response to terbinafine (n = 43). TF: therapeutic failure; CI: clinical improvement; MC: mycological cure; TC: total cure.
After applying the chi-square test, no significant difference was observed between the groups (p = 0.280) concerning the response to terbinafine. However, among the patients who finished the study, the majority (83.72%, p = 0.001) showed at least one degree of improvement (TC, MC, or CI).
3.1. Relationship between Treatment Results, Affected Nails, Clinical Classification, Presence of Comorbidities, Use of Medications, and Isolated Fungi
Table 3 shows clinical and microbiological data, such as treatment results, affected nails, clinical classification, presence of comorbidities, use of medications, and isolated fungi for all participants that finished the study.
Table 3.
Treatment results, affected nails, clinical classification, comorbidities, use of medications, and isolated fungi. TC: total cure, MC: mycological cure, CI: clinical improvement, TF: therapeutic failure.
| Result | Fingernails/Toenails | Clinical Calssification | Comorbidities | Medications | Isolated Fungi |
|---|---|---|---|---|---|
| TC | Right hallux | DLSO + onycholysis | 0 | 0 | Trichophyton sp |
| TC | Right hallux | DLSO + hypertrophy | 0 | 0 | Trichophyton sp |
| TC | Right hallux + 4rth left toenail | DLSO + hypertrophy | 0 | 0 | Trichophyton sp |
| TC | Halluces | DLSO + hypertrophy | depression | antidepressant | Trichophyton sp |
| TC | Right hallux | DLSO + hypertrophy | depression | antidepressant | Trichophyton sp |
| TC | Halluces | DLSO + onycholysis | 0 | 0 | T. rubrum |
| TC | Right hallux | DLSO + hypertrophy | 0 | 0 | T. mentagrophytes |
| TC | Left hallux | DLSO + onycholysis | hypothyroidism | 0 | T. rubrum |
| MC | Halluces | DLSO + onycholysis | obesity + depression | antidepressant | Trichophyton sp |
| MC | Right hallux | DLSO + onycholysis | 0 | 0 | T. mentagrophytes |
| MC | Halluces | DLSO + onycholysis | 0 | 0 | Trichophyton sp |
| CI | Halluces | DLSO + onycholysis | 0 | 0 | Trichophyton sp |
| CI | Halluces | DLSO + onycholysis | 0 | 0 | Trichophyton rubrum |
| TF | Right hallux | DLSO + hypertrophy | hypothyroidism | 0 | T. rubrum |
| TC | Right hallux | DLSO + onycholysis | depression | 0 | T. mentagrophytes |
| TC | Right hallux | DLSO + onycholysis | hypothyroidism | 0 | Trichophyton sp |
| TC | 4rth Right fingernail | DLSO + onycholysis | 0 | 0 | Trichophyton sp |
| TC | Halluces | DLSO + hypertrophy | 0 | 0 | Trichophyton sp |
| TC | Halluces | DLSO + onycholysis | 0 | 0 | T. rubrum |
| TC | Halluces | DLSO + onycholysis | depression | antidepressant | Trichophyton sp |
| TC | Left hallux | DLSO + hypertrophy | 0 | 0 | Trichophyton sp |
| TC | Right hallux | DLSO + onycholysis | HIV | antiretrovirals | Trichophyton sp |
| MC | Left hallux | DLSO + onycholysis | 0 | 0 | Trichophyton sp |
| CI | Halluces | DLSO + onycholysis | 0 | 0 | T. mentagrophytes |
| TF | Right hallux + 2nd left toenail | DLSO + onycholysis | 0 | 0 | T. rubrum |
| TF | Halluces | PSO + SO | 0 | 0 | Trichophyton sp |
| TF | Halluces | DLSO + hypertrophy | 0 | 0 | T. mentagrophytes |
| TF | Halluces | DLSO + hypertrophy + DLSO + onycholysis | 0 | 0 | Trichophyton sp |
| TC | Right hallux + 3rd left toenail | DLSO + hypertrophy | depression | antidepressant | T. mentagrophytes |
| TC | 2nd right + 3rd left toenails | TDO | 0 | 0 | Trichophyton sp |
| TC | Right hallux | TDO | obesity | 0 | Trichophyton sp |
| TC | Right hallux | DLSO + onycholysis | 0 | 0 | Trichophyton sp |
| TC | 2nd right toenail | DLSO + onycholysis + TDO | obesity + depression | antidepressant | T. rubrum |
| TC | Left hallux | DLSO + hypertrophy | 0 | 0 | Trichophyton sp |
| TC | Left hallux | DLSO + onycholysis + TDO | diabetes | o | Trichophyton sp |
| TC | Right hallux | DLSO + onycholysis | 0 | 0 | Trichophyton sp |
| TC | Halluces | DLSO + onycholysis | 0 | 0 | T. rubrum |
| TC | 2nd right + 2nd left toenails | TDO | 0 | 0 | Trichophyton sp |
| TC | 2nd right toenail | DLSO + hypertrophy | 0 | 0 | Trichophyton mentagrophytes |
| CI | Halluces | DLSO + onycholysis | 0 | 0 | Trichophyton sp |
| CI | 3rd right + 3rd left toenail | DLSO + hypertrophy | 0 | 0 | T. mentagrophytes |
| TF | Halluces | DLSO + onycholysis | 0 | 0 | Trichophyton sp |
| TF | Halluces | DLSO + onycholysis | 0 | 0 | T. mentagrophytes |
There was no significant difference in the treatment results concerning the affected nails (p = 0.750), clinical classification (p = 0.580), presence of comorbidities (p = 0.730), use of medications (p = 0.660), and the isolated fungi (p = 0.770).
3.2. Dropouts and Side Effects
Twenty patients did not complete the study, five (7.93%) of them because of side effects. The other 15 (23.90%) patients dropped out for personal reasons.
The most observed side effects were gastralgia (Group 2, n = 4, Group 3, n = 1) and cutaneous rash (Group 1, n = 1). None of these patients had comorbidities or used medications that could interact with terbinafine. (Table 4).
Table 4.
Dropouts and side effects.
| Side Effects/Dropout | Group 1 | Group 2 | Group 3 | Total |
|---|---|---|---|---|
| None | 14 (70.00%) | 14 (66.67%) | 15 (68.18%) | 43 |
| Gastralgia | 0 (0.00%) | 3 (14.28%) | 1 (4.55%) | 4 |
| Cutaneous rash | 1 (5.00%) | 0 (0.00%) | 0 (0.00%) | 1 |
| Did not complete (personal reasons) |
5 (25.00%) | 4 (19.05%) | 6 (27.27%) | 15 |
| Total | 20 | 21 | 22 | 63 |
4. Discussion
Since its introduction, terbinafine has been considered more effective than other antifungals available to treat dermatophytosis [33,34,35,36].
Undesirable side effects have been associated with terbinafine use, especially during a long treatment period, including gastrointestinal side effects, cutaneous rash, headache, myalgia, and, rarely, hepatotoxicity, drug-induced lupus erythematosus, Sjogren’s syndrome, Stevens–Johnson syndrome, toxic epidermal necrolysis, alopecia, and psoriasis [37,38,39,40].
Terbinafine is metabolized in part by the cytochrome P450 isoenzymes, particularly CYP2D6, which explains the lower rates of drug interactions in comparison with other anti-fungal agents [41,42]. Terbinafine is contraindicated in patients with allergy to terbinafine or in patients with liver dysfunction and it may be used with caution with selective serotonin reuptake inhibitors, C1 antiarrhythmics, and monoaminoxidase inhibitors [43,44]. Seven patients that completed this study used antidepressants, six of them presented with TC, and one with MC.
Some studies have shown terbinafine presence in nails in concentrations above the minimal inhibitory concentrations of 0.0015–0.01 mg/ml for dermatophytes and 0.06–0.025 mg/ml for other fungi, e.g., Aspergillus species, for more than 36 weeks post-treatment and high plasmatic levels 12 weeks after the beginning of treatment [16,20,25,33,45]. The use of terbinafine for onychomycosis has been compared with that of other anti-fungal agents, especially itraconazole, or even with terbinafine itself in different types of regimens associated or not with a topical treatment. Most studies have focused on the administration of terbinafine doses between 250 and 500 mg per day for 3 or 4 months or on intermittent therapy involving 4 weeks of terbinafine followed by a 4-week period off terbinafine, and then additional 4 weeks of terbinafine treatment [46,47].
This study aimed to determine whether a longer drug interval period could result in effectiveness rates similar to or higher than those described for other regimens (of approximately 57%) in previous studies [48,49] and also if the proposed regimen can be more economical. The demographic variables in our study were similar to those in other terbinafine comparative studies [7,28,50]. The three groups showed similar TC, MC, and CI rates.
Compared to the Zaias and Rebell’s study [29], which described efficacy using a 250 mg quarterly terbinafine regimen pulse for onychomycosis caused by T. rubrum, in our study, two patients of Group 3 (13.33%) had TC and one patient (6.66%) had clinical improvement of onychomycosis caused by T. mentagrophytes. We opted for the 500 mg quarterly dose in order to compare the efficacy with that of the standard 500 mg monthly dose used in most of the published studies based on pulse regimens. In addition, this is the terbinafine dose of pulse regimen utilized in Brazil. Further studies with a more significant number of participants are necessary to compare the effectiveness of the trimester schemes of oral terbinafine in the treatment of all types of dermatophyte onychomycosis.
Treatment outcomes for onychomycosis can also vary according to age, clinical presentation, comorbidities, and the use of medications that may interact with antifungal treatments [32,51,52]. DLSO with hypertrophy with or without dermatophytoma, PSO, and TDO can be more resistant to treatment. SO may be difficult to treat if associated with immunodeficiency [53,54]. This study did not reveal significant differences between the outcomes and the clinical presentation, the presence of comorbidities, or the concomitant use of medications, probably because of the limited number of participants.
The asymmetric gait nail unit syndrome (AGNUS), firstly described by Zaias et al. in 2012, is caused by repetitive toe trauma in a closed shoe in patients with asymmetric walking due to orthopedic abnormalities. The resulting nail changes can undoubtedly be clinically identical to onychomycosis [55]. In our study, the possible orthopedic abnormalities were not evaluated, but cultures were performed before and after the treatment, confirming that all participants had onychomycosis. In future onychomycosis studies, the evaluation of the concomitant presence of AGNUS can be useful, since it can change the clinical classification and the cure criteria.
As life expectancy is increasing globally, it is common for patients with onychomycosis to present with comorbidities and take more than one long-term medication [36,56,57,58,59]. As the speed of nail growth decreases with age, terbinafine is a good treatment option because it can enhance the speed of growth in the nail plate; therefore, the portion of compromised nail plate grows faster to the free edge and can be eliminated through cutting [58,60,61]. All groups in this study comprised some patients with comorbidities. The most common were depression (n = 7), obesity (n = 5), hypothyroidism (n = 3), diabetes (n = 1), and HIV active infection (n = 1). Only one patient with a comorbidity, who had hypothyroidism, presented with TF.
The pulse regimen therapy (groups 2 and 3) had the lowest cost of treatment. Group 1 used a total of 84 tablets, while groups 2 and 3 used 56 tablets each. The quarterly pulse regimen had the same cost compared to the conventional terbinafine pulse regimen but might be more financially appealing since patients are required to purchase a second terbinafine supply only six months after the start of treatment [48,62,63].
The long drug rest interval may compromise adherence to treatment due to patients forgetting the quarterly dose, which is an issue that can be addressed through counseling patients, family members responsible for them, or, eventually, caregivers of elderly persons using a simple reminder message recorded on their cell phone [64].
5. Conclusions
Despite the limited sample, a pulse therapy regimen using terbinafine 500 mg per day for a week every three months was found to be a potentially useful alternative in the treatment of onychomycosis by dermatophytes. Further studies involving a more significant number of patients are necessary to confirm the effectiveness of this treatment regimen.
Acknowledgments
We sincerely thank Nardo Zaias for kindly providing essential references and suggestions for the preparation of this manuscript.
Abbreviations
| CI | clinical improvement |
| DLSO | distal lateral subungual onychomycosis |
| MC | mycological cure |
| SO | superficial onychomycosis |
| TC | total cure |
| TDO | total dystrophic onychomycosis |
| TF | therapeutic failure |
| AGNUS | asymmetric gait nail unit syndrome |
Author Contributions
Conceptualization, Methodology, Validation, Resources: A.B.S.; Data Curation, Original Draft Preparation and Writing: A.B.S. and F.S.; Writing, Review & Editing: A.B.S., K.S.M.P., F.S., and F.Q.-T.; Supervision: K.S.M.P. and Flavio de F.Q.-T.
Funding
The Terbinafine used in this study was donated by Cristália Pharmaceutical Chemical Ltd. This company had no role in the design, execution, interpretation, or writing of the study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Smith E.B. History of antifungals. J. Am. Acad. Dermatol. 1990;23:776–778. doi: 10.1016/0190-9622(90)70286-Q. [DOI] [PubMed] [Google Scholar]
- 2.Neumann H.A. Oral treatment of onychomycosis of the toe nails; comparison of cost effectiveness of griseofulvin, itraconazole, ketoconazole and terbinafine. Ned. Tijdschr. Geneeskd. 1995;139:1350–1351. [PubMed] [Google Scholar]
- 3.Purim K.S., Bordignon G.P., Queiroz-Telles F. Fungal infection of the feet in soccer players and non-athlete individuals. Rev. Iberoam. Micol. 2005;22:34–38. doi: 10.1016/S1130-1406(05)70004-8. [DOI] [PubMed] [Google Scholar]
- 4.Purim K.S., de Freitas C.F., Leite N. Feet dermatophytosis in soccer player. An. Braz. Dermatol. 2009;84:550–552. doi: 10.1590/S0365-05962009000500020. [DOI] [PubMed] [Google Scholar]
- 5.Gupta A.K., Versteeg S.G., Shear N.H. Onychomycosis in the 21st Century: An Update on Diagnosis, Epidemiology, and Treatment. J. Cutan. Med. Surg. 2017;21:525–539. doi: 10.1177/1203475417716362. [DOI] [PubMed] [Google Scholar]
- 6.Ha S.J., Han K.D., Song Y., Lee J.H. Weight change and risk of onychomycosis: A nationwide cohort study in Korea. J. Am. Acad. Dermatol. 2018;78:613–614. doi: 10.1016/j.jaad.2017.09.030. [DOI] [PubMed] [Google Scholar]
- 7.Gupta A.K., Daigle D., Foley K.A. Network Meta-Analysis of Onychomycosis Treatments. Skin Appendage Disord. 2015;1:74–81. doi: 10.1159/000433473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garcia-Romero M.T., Granados J., Vega-Memije M.E., Arenas R. Analysis of genetic polymorphism of the HLA-B and HLA-DR loci in patients with dermatophytic onychomycosis and in their first-degree relatives. Actas Dermosifiliogr. 2012;103:59–62. doi: 10.1016/j.adengl.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 9.Carrillo-Meléndrez H., Ortega-Hernández E., Granados J., Arroyo S., Barquera R., Arenas R. Role of HLA-DR Alleles to Increase Genetic Susceptibility to Onychomycosis in Nail Psoriasis. Skin Appendage Disord. 2016;2:22–25. doi: 10.1159/000446444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abdel-Rahman S.M. Genetic Predictors of Susceptibility to Dermatophytoses. Mycopathologia. 2017;182:67–76. doi: 10.1007/s11046-016-0046-z. [DOI] [PubMed] [Google Scholar]
- 11.Gupta A.K., Carviel J., Shear N.H. Onychomycosis and Chronic Fungal Disease: Exploiting a Commensal Disguise to Stage a Covert Invasion. J. Cutan. Med. Surg. 2018;22:318–322. doi: 10.1177/1203475417745827. [DOI] [PubMed] [Google Scholar]
- 12.Vlahovic T.C. Onychomycosis: Evaluation, Treatment Options, Managing Recurrence, and Patient Outcomes. Clin. Podiatr. Med. Surg. 2016;33:305–318. doi: 10.1016/j.cpm.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 13.Lipner S.R., Scher R.K. Part I: Onychomycosis: Clinical Overview and Diagnosis. J. Am. Acad. Dermatol. 2019 doi: 10.1016/j.jaad.2018.03.062. [DOI] [PubMed] [Google Scholar]
- 14.Zaias N., Rebell G., Casal G., Appel J. The asymmetric gait toenail unit sign. Skinmed. 2012;10:213–217. [PubMed] [Google Scholar]
- 15.Zaias N., Rebell G., Escovar S. Asymmetric gait nail unit syndrome: The most common worldwide toenail abnormality and onychomycosis. Skinmed. 2014;12:217–223. [PubMed] [Google Scholar]
- 16.Peres N.T., Maranhão F.C., Rossi A., Martinez-Rossi N.M. Dermatophytes- Host-pathogen interaction and antifungal resistance. An. Braz. Dermatol. 2010;85:657–667. doi: 10.1590/S0365-05962010000500009. [DOI] [PubMed] [Google Scholar]
- 17.Gupta A.K., Foley K.A., Mays R.R., Shear N.H., Piguet V. Monotherapy for toenail onychomycosis: A systematic review and network meta-analysis. Br. J. Dermatol. 2019 doi: 10.1111/bjd.18155. [DOI] [PubMed] [Google Scholar]
- 18.Gupta A.K., Foley K.A., Versteeg S.G. New Antifungal Agents and New Formulations Against Dermatophytes. Mycopathologia. 2017;182:127–141. doi: 10.1007/s11046-016-0045-0. [DOI] [PubMed] [Google Scholar]
- 19.Gupta A.K., Mays R.R., Versteeg S.G., Shear N.H., Friedlander S.F. Onychomycosis in children: Safety and efficacy of antifungal agents. Pediatr. Dermatol. 2018;35:552–559. doi: 10.1111/pde.13561. [DOI] [PubMed] [Google Scholar]
- 20.Kreijkamp-Kaspers S., Hawke K.L., van Driel M.L. Oral Medications to Treat Toenail Fungal Infection. JAMA. 2018;319:397–398. doi: 10.1001/jama.2017.20160. [DOI] [PubMed] [Google Scholar]
- 21.Dias M.F.R.G., Bernardes-Filho F., Quaresma-Santos M.V.P., Amorim A.G.D.F., Schechtman R.C., Azulay D.R. Treatment of superficial mycoses: Review. Part II. An. Braz. Dermatol. 2013;88:937–944. doi: 10.1590/abd1806-4841.20132018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salo H., Pekurinen M. Cost effectiveness of oral terbinafine (Lamisil) compared with oral fluconazole (Diflucan) in the treatment of patients with toenail onychomycosis. Pharmacoeconomics. 2002;20:319–324. doi: 10.2165/00019053-200220050-00003. [DOI] [PubMed] [Google Scholar]
- 23.Jensen J.C. Clinical pharmacokinetics of terbinafine (Lamisil) Clin. Exp. Dermatol. 1989;14:110–113. doi: 10.1111/j.1365-2230.1989.tb00904.x. [DOI] [PubMed] [Google Scholar]
- 24.Schatz F., Bräutigam M., Dobrowolski E., Effendy I., Haberl H., Mensing H., Weidinger G., Stütz A. Nail incorporation kinetics of terbinafine in onychomycosis patients. Clin. Exp. Dermatol. 1995;20:377–383. doi: 10.1111/j.1365-2230.1995.tb01353.x. [DOI] [PubMed] [Google Scholar]
- 25.Leyden J. Pharmacokinetics and pharmacology of terbinafine and itraconazole. J. Am. Acad. Dermatol. 1998;38:42–47. doi: 10.1016/S0190-9622(98)70483-9. [DOI] [PubMed] [Google Scholar]
- 26.Warshaw E.M., Fett D.D., Bloomfield H.E., Grill J.P., Nelson D.B., Quintero V., Carver S.M., Zielke G.R., Lederle F.A. Pulse versus continuous terbinafine for onychomycosis: A randomized, double-blind, controlled trial. J. Am. Acad. Dermatol. 2005;53:578–584. doi: 10.1016/j.jaad.2005.04.055. [DOI] [PubMed] [Google Scholar]
- 27.Takahata Y., Hiruma M., Shiraki Y., Tokuhisa Y., Sugita T., Muto M. Treatment of dermatophyte onychomycosis with three pulses of terbinafine (500 mg day for a week) Mycoses. 2009;52:72–76. doi: 10.1111/j.1439-0507.2008.01531.x. [DOI] [PubMed] [Google Scholar]
- 28.Mishra M., Panda P., Tripathy S., Sengupta S., Mishra K. An open randomized comparative study of oral itraconazole pulse and terbinafine pulse in the treatment of onychomycosis. Indian J. Dermatol. Venereol. Leprol. 2005;71:262–266. doi: 10.4103/0378-6323.16619. [DOI] [PubMed] [Google Scholar]
- 29.Zaias N., Rebell G. The successful treatment of Trichophyton rubrum nail bed (distal subungual) onychomycosis with intermittent pulse-dosed terbinafine. Arch. Dermatol. 2004;140:691–695. doi: 10.1001/archderm.140.6.691. [DOI] [PubMed] [Google Scholar]
- 30.Guo S., Zhong S., Zhang A. Privacy-preserving Kruskal-Wallis test. Comput. Methods Programs Biomed. 2013;112:135–145. doi: 10.1016/j.cmpb.2013.05.023. [DOI] [PubMed] [Google Scholar]
- 31.Gupta A.K., Stec N. Recent advances in therapies for onychomycosis and its management. F1000Research. 2019;8 doi: 10.12688/f1000research.18646.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baran R., Hay R.J. New clinical classification for onychomycoses. J. Mycol. Med. 2014;24:247–260. doi: 10.1016/j.mycmed.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 33.Villars V., Jones T.C. Clinical efficacy and tolerability of terbinafine (Lamisil)—A new topical and systemic fungicidal drug for treatment of dermatomycoses. Clin. Exp. Dermatol. 1989;14:124–127. doi: 10.1111/j.1365-2230.1989.tb00908.x. [DOI] [PubMed] [Google Scholar]
- 34.Gupta A.K., Paquet M., Simpson F.C. Therapies for the treatment of onychomycosis. Clin. Dermatol. 2013;31:544–554. doi: 10.1016/j.clindermatol.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 35.Hanna S., Andriessen A., Beecker J., Gilbert M., Goldstein E., Kalia S., King A., Kraft J., Lynde C., Singh D., et al. Clinical Insights About Onychomycosis and Its Treatment: A Consensus. J. Drugs Dermatol. 2018;17:253–262. [PubMed] [Google Scholar]
- 36.Gupta A.K., Mays R.R., Versteeg S.G., Piraccini B.M., Takwale A., Shemer A., Babaev M., Grover C., Di Chiacchio N.G., Taborda P.R.O., et al. Global perspectives for the management of onychomycosis. Int. J. Dermatol. 2018:1–12. doi: 10.1111/ijd.14346. [DOI] [PubMed] [Google Scholar]
- 37.Bonsmann G., Schiller M., Luger T.A., Stander S. Terbinafine-induced subacute cutaneous lupus erythematosus. J. Am. Acad. Dermatol. 2001;44:925–931. doi: 10.1067/mjd.2001.114565. [DOI] [PubMed] [Google Scholar]
- 38.Cerci F., Carvalho M., Nihi F. Erythrodermic psoriasis following terbinafine use. J. Am. Acad. Dermatol. 2016;74 doi: 10.1016/j.jaad.2016.02.971. [DOI] [Google Scholar]
- 39.Branisteanu D.E., Ianosi S.L., Dimitriu A., Stoleriu G., Oanta A., Branisteanu D.C. Drug-induced Rowell syndrome, a rare and difficult to manage disease: A case report. Exp. Ther. Med. 2018;15:785–788. doi: 10.3892/etm.2017.5557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ross C.L., Shevchenko A., Mollanazar N.K., Hsu S., Motaparthi K. Acute generalized exanthematous pustulosis due to terbinafine. Dermatol. Ther. 2018;31:e12617. doi: 10.1111/dth.12617. [DOI] [PubMed] [Google Scholar]
- 41.Shapiro L.E. SNH Drug interactions: Proteins, pumps, and P-450s. J. Am. Acad. Dermatol. 2002;47:467–484. doi: 10.1067/mjd.2002.126823. [DOI] [PubMed] [Google Scholar]
- 42.Nicoletti P., Aithal G.P., Bjornsson E.S., Andrade R.J., Sawle A., Arrese M., Barnhart H.X., Bondon-Guitton E., Hayashi P.H., Bessone F., et al. Association of Liver Injury From Specific Drugs, or Groups of Drugs, With Polymorphisms in HLA and Other Genes in a Genome-Wide Association Study. Gastroenterology. 2017;152:1078–1089. doi: 10.1053/j.gastro.2016.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schmitt J.V., Bombonatto G., Trierweiler S.M., Fabri A.B. General aspects of drug interactions with systemic antifungals in a retrospective study sample. An. Braz. Dermatol. 2013;88:476–479. doi: 10.1590/abd1806-4841.20131781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gupta A.K., Versteeg S.G., Shear N.H. Common drug-drug interactions in antifungal treatments for superficial fungal infections. Expert Opin. Drug Metab. Toxicol. 2018;14:387–398. doi: 10.1080/17425255.2018.1461834. [DOI] [PubMed] [Google Scholar]
- 45.Monod M., Mehul B. Recent Findings in Onychomycosis and Their Application for Appropriate Treatment. J. Fungi. 2019;5:20. doi: 10.3390/jof5010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gupta A.K., Lynch L.E., Kogan N., Cooper E.A. The use of an intermittent terbinafine regimen for the treatment of dermatophyte toenail onychomycosis. J. Eur. Acad. Dermatol. Venereol. 2009;23:256–262. doi: 10.1111/j.1468-3083.2008.03036.x. [DOI] [PubMed] [Google Scholar]
- 47.Christenson J., Peterson G., Naunton M., Bushell M., Kosari S., Baby K., Thomas J. Challenges and Opportunities in the Management of Onychomycosis. J. Fungi. 2018;4:87. doi: 10.3390/jof4030087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jansen R., Redekop W.K., Rutten F.F. Cost effectiveness of continuous terbinafine compared with intermittent itraconazole in the treatment of dermatophyte toenail onychomycosis: An analysis of based on results from the L.I.ON. study. Lamisil versus Itraconazole in Onychomycosis. Pharmacoeconomics. 2001;19:401–410. doi: 10.2165/00019053-200119040-00007. [DOI] [PubMed] [Google Scholar]
- 49.Elewski B., Pollak R., Ashton S., Rich P., Schlessinger J., Tavakkol A. A randomized, placebo- and active-controlled, parallel-group, multicentre, investigator-blinded study of four treatment regimens of posaconazole in adults with toenail onychomycosis. Br. J. Dermatol. 2012;166:389–398. doi: 10.1111/j.1365-2133.2011.10660.x. [DOI] [PubMed] [Google Scholar]
- 50.Scher R.K., Rich P., Pariser D., Elewski B. The Epidemiology, Etiology, and Pathophysiology of Onychomycosis. Semin. Cutan. Med. Surg. 2013;32:S2–S4. doi: 10.12788/j.sder.0014. [DOI] [PubMed] [Google Scholar]
- 51.Hay R.J., Baran R. Onychomycosis: A proposed revision of the clinical classification. J. Am. Acad. Dermatol. 2011;65:1219–1227. doi: 10.1016/j.jaad.2010.09.730. [DOI] [PubMed] [Google Scholar]
- 52.Lipner S.R., Scher R.K. Part II: Onychomycosis: Treatment and Prevention of Recurrence. J. Am. Acad. Dermatol. 2019;80:853–867. doi: 10.1016/j.jaad.2018.05.1260. [DOI] [PubMed] [Google Scholar]
- 53.Gupta A.K., Foley K.A. Evidence for biofilms in onychomycosis. Giornale Italiano di Dermatologia e Venereologia. 2019;154:50–55. doi: 10.23736/S0392-0488.18.06001-7. [DOI] [PubMed] [Google Scholar]
- 54.Finch J.J., Warshaw E.M. Toenail onychomycosis: Current and future treatment options. Dermatol. Ther. 2007;20:31–46. doi: 10.1111/j.1529-8019.2007.00109.x. [DOI] [PubMed] [Google Scholar]
- 55.Zaias N.E.A. Dermatophyte Onychomycosis: The Active Invasion of a Normal Nail Unit versus the Colonization of an Existing Abnormal Nail Unit by Environmental Fungus. SKINmed. 2019;X:1–5. [PubMed] [Google Scholar]
- 56.World Health Organization . Life Spectancy Situation. World Health Organization; Geneva, Swtizerland: 2019. [(accessed on 31 July 2019)]. Available online: https://www.who.int/gho/mortality_burden_disease/life_tables/situation_trends_text/en/ [Google Scholar]
- 57.Piraccini B., Alessandrini A. Onychomycosis: A Review. J. Fungi. 2015;1:30. doi: 10.3390/jof1010030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Maddy A.J., Tosti A. Hair and nail diseases in the mature patient. Clin. Dermatol. 2018;36:159–166. doi: 10.1016/j.clindermatol.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 59.Gupta A.K., Versteeg S.G., Shear N.H., Piguet V., Tosti A., Piraccini B.M. A Practical Guide to Curing Onychomycosis: How to Maximize Cure at the Patient, Organism, Treatment, and Environmental Level. Am. J. Clin. Dermatol. 2019;20:123–133. doi: 10.1007/s40257-018-0403-4. [DOI] [PubMed] [Google Scholar]
- 60.Geyer A.S., Onumah N., Uyttendaele H., Scher R.K. Modulation of linear nail growth to treat diseases of the nail. J. Am. Acad. Dermatol. 2004;50:229–234. doi: 10.1016/j.jaad.2003.07.011. [DOI] [PubMed] [Google Scholar]
- 61.Finlay A.Y., Lever L., Thomas R., Dykes P.J. Nail Matrix Kinetics of Oral Terbinafine in Onychomycosis and Normal Cells. J. Dermatol. Treat. 1990;1:51–53. doi: 10.3109/09546639009089035. [DOI] [Google Scholar]
- 62.Baran R., Sigurgeirsson B., de Berker D., Kaufmann R., Lecha M., Faergemann J., Kerrouche N., Sidou F. A multicentre, randomized, controlled study of the efficacy, safety and cost-effectiveness of a combination therapy with amorolfine nail lacquer and oral terbinafine compared with oral terbinafine alone for the treatment of onychomycosis with matrix involvement. Br. J. Dermatol. 2007;157:149–157. doi: 10.1111/j.1365-2133.2007.07974.x. [DOI] [PubMed] [Google Scholar]
- 63.Yang E.J., Lipner S.R. Pharmacy Costs of Medications for the Treatment of Onychomycosis in the United States. J. Am. Acad. Dermatol. 2019;81:276–278. doi: 10.1016/j.jaad.2019.01.032. [DOI] [PubMed] [Google Scholar]
- 64.Lin K., Lipner S.R. Mobile Phone Reminders for Onychomycosis Medication Adherence. J. Am. Acad. Dermatol. 2018;80:e105–e107. doi: 10.1016/j.jaad.2018.11.010. [DOI] [PubMed] [Google Scholar]