This section is focused on prioritizing unmet clinical needs that will benefit from novel technologies applied to non-invasive detection and monitoring of active inflammation and assessment of treatment response, mucosal targeted drug delivery systems, and prevention of post-operative septic complications and treatment of fistulizing complications.
Keywords: Crohn’s disease, ulcerative colitis, radiology, non-invasive imaging, drug delivery, surgery, fistula, anastomosis, sepsis
Abstract
Novel technologies is part of five focus areas of the Challenges in IBD research document, which also includes preclinical human IBD mechanisms, environmental triggers, precision medicine and pragmatic clinical research. The Challenges in IBD research document provides a comprehensive overview of current gaps in inflammatory bowel diseases (IBD) research and delivers actionable approaches to address them. It is the result of a multidisciplinary input from scientists, clinicians, patients, and funders, and represents a valuable resource for patient centric research prioritization. In particular, the novel technologies section is focused on prioritizing unmet clinical needs in IBD that will benefit from novel technologies applied to: 1) non-invasive detection and monitoring of active inflammation and assessment of treatment response; 2) mucosal targeted drug delivery systems; and 3) prevention of post-operative septic complications and treatment of fistulizing complications. Proposed approaches include development of multiparametric imaging modalities and biosensors, to enable non invasive or minimally invasive detection of pro-inflammatory signals to monitor disease activity and treatment responses. Additionally, technologies for local drug delivery to control unremitting disease and increase treatment efficacy while decreasing systemic exposure are also proposed. Finally, research on biopolymers and other sealant technologies to promote post-surgical healing; and devices to control anastomotic leakage and prevent post-surgical complications and recurrences are also needed.
Novel technologies is part of five focus areas of the Challenges in IBD Research document, which also includes preclinical human IBD mechanisms,1 environmental triggers,2 precision medicine3 and pragmatic clinical research.4
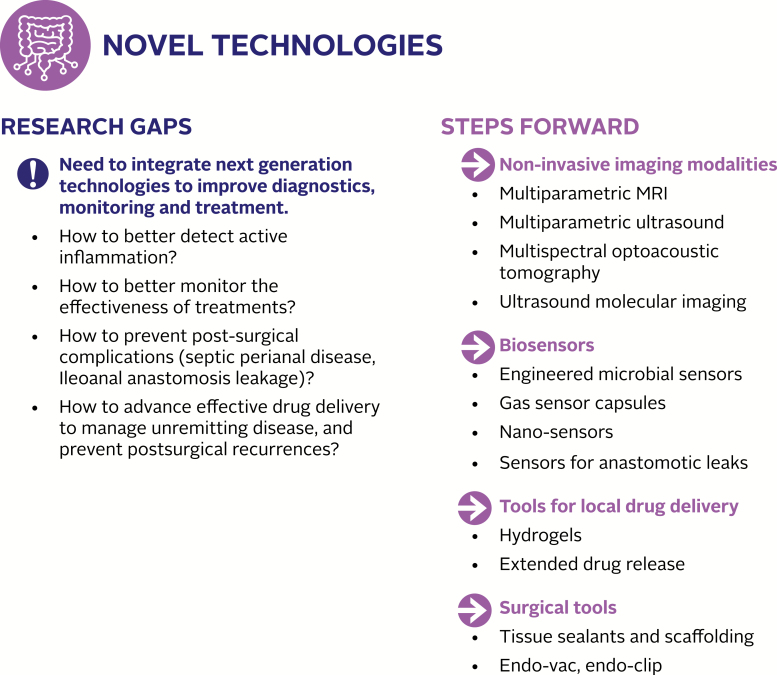
In parallel with the need for advances in understanding the biology of inflammatory bowel diseases (IBD), there is an equally pressing need for new or improved technologies to serve clinical needs in IBD. These advances may be particularly impactful in three areas of need: 1) non-invasive modalities to detect and monitor active inflammation related to IBD and assess treatment response, 2) technologies to enable mucosal targeted drug delivery systems that enhance efficacy and decrease side effects, and 3) surgical and other technologies to prevent post-operative septic complications, treat fistulizing disease and prevent anastomotic failure (Fig. 1).
FIGURE 1.
Novel technologies: current research gaps and steps forward to integrate next generation technologies that address pressing unmet clinical needs in IBD.
NON-INVASIVE DETECTION AND EVALUATION OF ACTIVE INFLAMMATION IN IBD: IMAGING AND SENSING TECHNOLOGIES
Evaluation of Crohn’s disease (CD) activity and treatment response remains a particular challenge. Current clinical assessment of disease activity in adults and children relies heavily on clinical scores such as the Crohn’s Disease Activity Index (CDAI), which is based on patient documentation of symptoms and additional variables over a 7-day period.5 Another scoring system, the Harvey-Bradshaw Index, is an abbreviated clinical scoring system that is based primarily on patient symptoms at the time of evaluation.6 Limitations of these measures include their highly subjective nature and the frequent disconnect between patient symptoms and direct measures of disease activity, such as endoscopic inflammation and histopathology,7 that correlate with long-term outcomes. Circulating biomarkers of inflammation such as erythrocyte sedimentation rate (ESR) and c-reactive protein (CRP), as well as fecal biomarkers, calprotectin and lactoferrin, are used to track disease activity in a quantitative manner but are not specific to IBD-related inflammation and also cannot evaluate changes in inflammation at the bowel segmental level.8 Disease monitoring using non-invasive sensing technologies (devices able to periodically or continuously measure biological signals) able to detect changes in IBD-related clinical parameters (e.g., intestinal inflammation, mucosal healing, changes in microbiome, dysregulation of immune system) could be particularly useful for early recognition of disease activity in asymptomatic patients and for monitoring of response to therapies.
In the absence of optimal non-invasive monitoring technologies, endoscopic measures of disease activity (and treatment response) remain the gold standard for inflammatory activity because of their ability to assess mucosal inflammatory changes in individual bowel segments. Endoscopic improvement, defined as resolution of inflammation observable by endoscopy in a bowel segment following treatment, has emerged as a therapeutic endpoint associated with long-term clinical remission.9 The advantages of endoscopy include: (1) direct visual assessment of disease severity, (2) ability to follow individual bowel segments over time for changes in disease severity, and (3) ability to perform endoscopic mucosal biopsy to obtain microscopic evaluation of disease. However, endoscopy has several limitations; (1) invasiveness including requirement for patient sedation/anesthesia, (2) financial cost, (3) inter-user variability and limited ability to precisely localize the bowel segment being evaluated, (4) lack of established cutoff values to define response/remission,9, 10 (5) the technical challenge associated with reaching remote intestinal segments such as jejunum or proximal ileum or intestine beyond a stricture segment. These limitations constitute major impediments to the frequent use of endoscopy to measure treatment response in routine clinical practice.
Radiological imaging, due to its non-invasiveness, makes a practical modality for the detection and monitoring of CD if other limitations could be overcome. Currently ultrasound (US), Computed Tomography (CT), and Magnetic Resonance Enterography (MRE) are commonly used for CD evaluation. Each technique has advantages and limitations. Conventional US is comparatively inexpensive, does not use ionizing radiation and can be performed in real-time with easy accessibility. Conventional ultrasound has been shown to be very effective in the monitoring of patients with CD, particularly in the pediatric age group. However, US is operator dependent and subject to inter-operator variability. In addition, interpretation is qualitative further increasing operator dependency. However, its application to a disease activity index for CD would require validation, which is currently lacking. Finally, it is difficult for US to evaluate the entire length of large and small bowel as a screening tool and may miss extra-luminal disease complications due to acoustic attenuation from air within the bowel lumen.
CT directly demonstrates bowel wall thickening, mesenteric edema, and lymphadenopathy, as well as inflammatory masses and abscesses. CT is somewhat limited in detecting subtle mucosal inflammation. Furthermore, radiation exposure prevents its frequent use particularly in the pediatric age group. Like CT, MRE has cross-sectional imaging capability that enables it to evaluate extralumenal and extraintestinal disease manifestations of IBD, an important advantage over endolumenal techniques. With the addition of oral contrast distention of the bowel and intravenous contrast delineation of bowel vascularity and inflammation, MRE has been shown to be highly accurate for the detection of active CD in both adults and children.11 Over the past five years, MRE has become the primary imaging modality for disease assessment in patients with Crohn’s disease, although it is important to note that this modality has not been qualified by regulatory agencies as a validated disease activity index in clinical trials. With the recently published “Consensus Recommendations for Evaluation, Interpretation, and Utilization of Computed Tomography and Magnetic Resonance Enterography in Patients With Small Bowel Crohn’s Disease” there is a push for standardization of CT and MRE reporting.12
While the above tests play an important role in current IBD management, there is a need to improve on numerous respective limitations which may include relative invasiveness, cost, ionizing radiation, discomfort, and limitation in the evaluation of the entire gastrointestinal tract. In addition, with the advent of increasing drug options to choose from, there is a need for imaging techniques that can provide validated, early and frequent assessment of treatment response. This would allow a temporal window for dose escalation or addition of combination therapy to maintain clinical remission. Further, early detection of non-responsiveness would help to minimize the toxicity and financial cost associated with non-effective medications.
Another challenge is the evaluation of strictures and the evaluation of the length of bowel involved by CD. Radiological imaging does not perform well for stricture evaluation because imaging signs of active inflammation can obscure underlying fibrosis, while endoscopic imaging and biopsies only sample the mucosa so are not deep enough to detect submucosal and serosal collagen deposition indicative of fibrosis. The length of involved bowel with fibrosis is one prognostic factor to be considered when making decisions as fibrosed bowel mandates surgical treatment, whereas, resecting non-fibrosed wall which requires additional medical therapy as opposed to surgical treatment, may be associated with significant risk of poor outcomes such as short gut syndrome. Current imaging technologies lack a clear distinguishing capability and in particular lack the ability to quantify the amount of fibrosis that is setting in.
TECHNOLOGIES TO ENABLE MUCOSAL TARGETED DRUG DELIVERY SYSTEMS THAT ENHANCE EFFICACY AND DECREASE SIDE EFFECTS
About one-third of IBD patients require surgery within 5–10 years of diagnosis, and two-thirds of patients require surgery over their lifetime.13 Although hospitalization rates have decreased in the biologics era, several publications have shown that rates for surgery have not significantly decreased.14 After surgery, the majority of patients go in remission, but the disease almost always recurs over time, and in general at the surgical anastomosis and in the proximal gut segment. Most studies have reported that endoscopic and histologic recurrence precedes clinical recurrence.15 The early mucosal lesion seen in CD - the aphthous ulcer - can be seen by visualizing the ileum proximal to the anastomosis by colonoscopy within months after surgery. Endoscopic disease has been shown to guide risk for clinical disease and risk of re-operation. It is estimated that 70–90% of patients will have endoscopic disease within 1 year of surgery and this number increases to 80–100% within 3 years. Clinical recurrence is seen in up to 30% of cases in one year. About one-third of the patients will require reoperation in 10 years and 80% in 15 years.15 Risk of reoperation is significant as loss of small bowel is not compatible with healthy lifestyle as it leads to malabsorption and in select cases, short bowel syndrome.
Medication non-adherence remains a barrier to effective treatment in chronic diseases including IBD.16 More infrequent dosing has been demonstrated to increase adherence in chronic conditions.17 In addition, traditional drug delivery formulations may deliver inadequate drug levels at the site of therapeutic action while delivering drug to sites where toxicity may be elicited without therapeutic benefit. To address the need for more effective drug delivery, to achieve reduction of unwanted side effects associated with systemic therapies, and as such to increase treatment adherence, multiple approaches of localized drug delivery and sustained local drug release are currently emerging. Additionally, since it has been observed that recurrent disease occurs in the majority of cases at the site of the anastomosis and in the bowel segment proximal to it, these new approaches to localized and sustained drug release may offer possibilities to intervene locally at the time of surgery or postoperatively with endoscopy in this region. Improved mucosal drug delivery systems targeted to this area of highest recurrence risk could enhance efficacy and decrease side effects.
SURGICAL AND OTHER TECHNOLOGIES TO PREVENT POST-OPERATIVE SEPTIC COMPLICATIONS, TREAT FISTULIZING DISEASE AND PREVENT ANASTOMOTIC FAILURE
Anastomotic Failure
The Achilles heel of IBD surgery is anastomotic failure manifesting as intra-abdominal abscesses and peritonitis. The impact of this complication on the patient and health care resources is enormous. Prolonged hospital stays, reoperations with stoma creation, the development of entero-athmospheric fistula and incisional hernia have profound effect on the quality of life of the patient and cause great disability to take part in normal life.
The cause of anastomotic leakages is multifactorial. Some of the known factors can be corrected (malnutrition, treatment of preoperative septic conditions, weaning of medications associated with a higher risk of anastomotic dehiscences); some strategies can be employed (pre-abilitation or use of staged surgical procedures), but other conditions cannot be modified (male gender, comorbidities, high content of visceral fat, deleterious side effects from chronic use of steroids and biologics).
Despite all efforts, and in the presence of a well vascularized anastomosis, without tension and with a perfect apposition of the two ends providing an “air and water tight” seal, patients still suffer anastomotic dehiscence rates between 2–23%, depending on the site of the anastomosis.18 Why a seemingly perfect anastomosis still can leak is unclear and poorly understood. Improvements are needed in prevention, early detection of leaks and consequently more effective management of dehiscences.
Septic Complications
Septic complications in IBD occur predominantly in patients with a fistulizing phenotype of CD and in patients who have a complicated course after IBD surgery. Both conditions affect the quality of life and disability of the patient and are a great burden on health care resources.19
Fistulizing Crohn’s Disease of the Perineum
Perianal CD affects one out of four patients with Crohn’s disease. To find better solutions to manage perianal fistulas in CD, it is important to understand its pathophysiology. The pathogenesis of perianal fistulas starts with a deep penetrating ulcer responsible for a bowel wall perforation resulting in an abscess, which in turn perforates spontaneously or is drained surgically through the perineal skin. The resulting fistula persists as long as the internal fistulous opening remains patent due to active inflammation and chronic low-grade sepsis along the fistulous tract. The pressure gradient from the diseased anorectum to the perineal skin during defecation aids in the patency of the fistula. Management of the fistula should be directed at healing of the anorectal mucosa, at closure of the internal fistulous opening and at improving the healing environment in the fistulous tract through appropriate drainage of perianal sepsis. Much literature supports this approach.20 Biologics have shown promising results, but their discontinuation is followed by resumption of drainage. Surgical techniques alone aiming at closure of the internal opening, for example, simple closure, mucosal advancement plasty or ligation of the intersphincteric tract have proved to be disappointingly ineffective.
Steps Forward
Non-invasive Technologies for Evaluation of Active Inflammation in IBD
There is a pressing need to use novel imaging or a combination of existing imaging technology to address the gaps noted in detecting and monitoring disease extent and activity. Regarding detection of active disease, multiparametric MRI is one such approach. Newer techniques such as Diffusion-Weighted MRI (DWI) and motility imaging have shown promise. DWI hyperintensity correlates well with endoscopic inflammation in CD, but the correlation is less than that for ulcerative colitis (UC). DWI has an advantage that it can be used in unprepared bowel segments (i.e., no IV or oral preparation), which suggests that it may be used in imaging of patients for whom IV contrast administration is contraindicated or who cannot tolerate oral bowel preparation.21 Motility imaging of the small bowel can be performed with cinematic thick slab steady state free precession sequences, which allow repeated acquisition of images to visualize bowel peristalsis. These sequences allow both qualitative and quantitative assessment of bowel motility. Bowel motility imaging can be very helpful to distinguish under-distended bowel from abnormal bowel in patients with poor oral contrast intake for MRE. In CD, abnormal bowel segments have altered motility.22 In essence, a combination of DWI, motility imaging and MRE performed potentially as low-cost, rapid acquisitions can provide a multiparametric MRI technique that can address some of the need gaps highlighted above.
Multiparametric US is another combination approach that holds promise. While conventional B-mode US has several advantages due to being real-time, it does not provide additional information in terms of early markers of inflammation or fibrosis. Ultrasound Shear-wave Elastography (SWE) is a novel quantitative US imaging technique that allows anatomic mapping of tissue elasticity using shear waves to evaluate underlying tissue stiffness, making evaluation non-operator dependent and quantitative. This technique has shown promise in quantitative assessment of fibrosis in the liver and early studies show that inflammation and fibrosis in the bowel also have a signature.23, 24 Furthermore, extent of inflammation can be quantified using advanced Doppler Techniques and contrast US techniques. These advanced Doppler techniques in combination with contrast enhanced US are recent technological advancements in the field of US imaging. These techniques have several advantages over conventional Doppler imaging: (1) low velocity flow visualization, (2) high resolution, (3) minimal motion artefact, (4) high frame rates. These advantages allow micro-flow detection, the depiction of which is particularly useful for assessment of disease activity as a result of inflammation.25 The combination of conventional US, SWE, contrast US and advanced Doppler techniques offer the possibility of using the low-cost, readily available nature of US imaging to sequentially follow-up patients in remission and identify patients who do not respond to therapy early.23, 24 These methods in combinations hold promise to address the gaps for imaging in CD patients with the caveat that ultrasound due to its inherent limitations of operator dependencey and depth penetration prevent comprehensive bowel evaluation in patients with a diverse body habitus. Robust clinical studies that can evaluate quantitative values differentiating inflammation and assessing grades of fibrosis need to be performed.
There are a number of additional imaging modalities that may be of benefit in the management of IBD. Video Capsule Endoscopy (VCE) has demonstrated advantages over MRE techniques in evaluating the proximal small bowel and has been shown to be highly sensitive for the diagnosis of mucosal lesions. The added advantage of VCE is that it can allow evaluation of both small bowel and the large bowel.26 In addition, it can allow monitoring of patients in remission with very limited side effects. Additional techniques that are newer but hold promise to address the gaps are Multispectral Optoacoustic Tomography and US molecular imaging. Multispectral optoacoustic tomography can be used to image structural features of tissue. Newer approaches that can be performed trans-abdominally and can detect early inflammation can help fill some of the gaps.27, 28 Molecular imaging143 and in particular ultrasound molecular imaging is still in the early phases but early studies show promise as targeted molecular contrast agents can adhere to areas of inflammation and fibrosis.29–32 These can use existing US systems but standardization of signals from contrast agents is still needed.
Development of new sensing technologies (biosensors) and integration of existing sensing technologies are needed to detect and monitor inflammation in the context of IBD, using existing and novel biomarkers. New sensor technologies should be capable to detect the signals related to biological processes regarded to be causative and/or highly correlated with intestinal inflammation in IBD (e.g., cytokine levels, presence of proinflammatory immune cells, proinflammatory mediators, etc.) and should be informative with respect to symptoms (e.g., ability to detect an active ‘flare-up’ prior to observation of severe symptoms, or the ability to distinguish between symptoms caused by inflammation and symptoms occurring in the absence of inflammation).
These biosensors should be non-invasive or minimally invasive (implantable, ingestible, wearable or environmental devices or nano-sensors) and should provide real-time or near-real-time, continuous or periodic, data sampling and reporting, to be recorded together with the corresponding physiological relevant fluctuations in the specific biological signal(s). Such devices would allow routine monitoring of the disease during daily life without the need for a visit to a healthcare facility. Technically novel technologies developed in an experimental setting should be practical and patient-friendly- with high potential for rapid approval for consumer market and cost-effective production. One example is the development of continuous glucose monitoring developed for the study of patients with diabetes.
An example of sensing technology that can be potentially adopted for IBD monitoring is intestinal gas capsule, which can sense variations in the lumenal gas composition,33 particularly changes in hydrogen and hydrogen sulfide (H2 and H2S) that may be associated with exacerbation of IBD. Work is currently being conducted with engineered commensal bacteria and yeast designed to sense various mediators of inflammation. A “sense and respond” version can be envisioned where bacteria not only sense inflammation but are able to deliver an anti-inflammatory signal.
Lastly, newer technologies are being investigated that would allow capsules to sample mucosa or luminal content for “omics” analyses as well as deliver drug to specific targets of the GI tract.34
Targeted Drug Delivery Systems
The observation that recurrent disease frequently occurs at the site of the anastomosis and in the proximal bowel segment after a resection and anastomosis, offers the possibility to intervene locally at the time of surgery or postoperatively with endoscopy on this region. Drug diluting stents could be possibly inserted at the time of surgery or endoscopically at the time of detection of early recurrence. These stents could be “refilled” by oral administration of drugs that are designed to attach on the stent to achieve maximum concentration on the segment at high risk for recurrence.
Another approach is to harness inflammation-targeting drug delivery to achieve high drug concentrations locally at the site of inflammation with minimal exposure of healthy or distant tissues. Inflammation-targeting hydrogel (IT-hydrogel) microfibers, prepared from generally-recognized-as-safe agents, can selectively adhere to the inflamed tissue in the gut and release the encapsulated therapeutic agent on-demand in response to inflammatory enzymes, including matrix metalloproteinases (MMPs) at the target site.35 IT-hydrogel microfibers loaded with dexamethasone (Dex) demonstrated preferential adhesion to inflamed epithelial surfaces in two different mouse colitis models in vivo and to inflamed lesions in colon tissue samples (ex vivo) from patients with ulcerative colitis. Dex-loaded IT-hydrogel enemas administered every other day to mice with colitis resulted in a significant reduction in inflammation and 5-10-fold lower peak serum concentration of drug compared to free Dex enema. In addition to advancing potentially safer steroid based therapies to rapidly achieve remission with reduced systemic side effects, the IT-hydrogel approach is amenable to oral administration for potential treatment of CD and the platform can accommodate a wide spectrum of therapeutic agents including hydrophobic/hydrophilic small molecules and biologics. This technology is currently being tested.
Lastly, gastric resident systems capable of residing safely in the stomach for several weeks and providing extended drug release have been described.36 Further investigation and extensive clinical research are needed to assess the effectiveness of local delivery using existing IBD therapeutics.
Technologies to Prevent and Manage Post-operative Septic Complications, Treat Fistulizing Disease and Prevent Anastomotic Failure
As a first step towards making progress in the treatment of perineal septic complications in CD, there is a need for a proper classification of perianal fistulas that combines characterization of the size, pathology and shape of the tracts, as well as disease activity at the mucosal level. Similarly, to vet the results of different treatment modalities and interventions, it is necessary to identify proper endpoints including the impact of the fistula on the patient’s quality of life.
Technology aiming at surgical closure of the internal opening to transiently reduce inflammation to permit wound healing to occur, as well as technologies for sealing of the fistulous tract should be explored. There may be potential for surgically inserted scaffolds carrying drugs or stem cells that are released in the tract to simultaneously close the internal opening and improve the healing environment.37 The ideal scaffolding fills the tract initially with a material that promotes healing after which it will be fully integrated or dissolved by tissue that replaces it. To address this need scaffolding technology and biocompatible sealants are currently being developed to be used as an enhancement for tissue regeneration at the site of surgery and potentially to be used as a therapeutic option for post-surgical complications and fistulizing disease.38 It is important to note that the above approaches are preliminary in nature given that clinical proof-of-concept evidence is lacking.
In order to make progress in the rate of anastomotic healing, additional studies are needed on the optimal bowel preparation prior to surgery.39 Proper vascularization of bowel ends depends on good surgical technique and experience and is traditionally assessed subjectively. New techniques using fluorescent technology can probably better assess the vascularization of the bowel ends particularly in minimal invasive surgery where imaging is required. Other technology should focus on tissue sealants aiming to reinforce the anastomosis and making it perfectly “air and water tight”. Most of the anastomoses currently are made using mechanical stapling devices. A drawback of the stapling devices is that the staple heights are constant while the tissue thickness varies. There is an unmet need for “smart” stapling devices adapting the staple height to the thickness of the tissue of both bowel ends to have the optimal tissue compression combining a robust adaptation and “air and watertight” seal while preserving vascularization between the staples. New technology should focus on methods to improve and accelerate wound healing at the site of the anastomosis reducing the initial phase of physiological decrease in anastomotic strength because of collagen breakdown and build up. Recently, there has been great interest for the causative role of a collagenase producing microbiome that might be involved in anastomotic leakage.40 New interventions targeted on this microbiome could potentially reduce the rate of anastomotic dehiscences.
It is clear that if a leak is going to happen, the earlier the diagnosis is made the better the outcome of a timelier intervention. The assessment of CRP after surgery has shown great benefit. A low CRP at day 4 has a great negative predictive value and precludes septic complications reliably.41 Early management of anastomotic failure before the development of septic problems is key to preventing the full sequel of events and is the best prevention of worse outcome. Technology focusing on sensing an imminent leak before day four could further improve the management of leakage. Smart sensors might have a role in this.
ACKNOWLEDGMENTS
The authors thank Rosemary Bianculli for design of figures; Orna Ehrlich for coordination with the publisher; Rebecca Kaplan for facilitating public comments; and the following individuals for review and recommendations on the manuscript: Robert Hinton; Douglas Levine; Jeremy Adler; Neil Hyman; Sridhar Mani; Antonina Mikocka-Walus; Chao Li; Carolina Ciacci; Damian Garcia-Olmo; J. Todd Kuenstner; Maria Lia Scribano; Alan Baird; Emina Huang; Giovanni C. Actis; Harris Ahmad; Herbert Van Kruiningen; J.M. Mullin; Pietro Tonelli; Richard M Soll; Simone Saibeni and Ulla Knaus.
Supported by: Crohn’s & Colitis Foundation
REFERENCES
- 1. Pizarro TT, Stappenbeck TS, Rieder F. Challenges in IBD research: preclinical human IBD mechanisms. Inflamm Bowel Dis. 2019;25(Suppl 2):S5–S12. [DOI] [PubMed] [Google Scholar]
- 2. Ho SM, Lewis JD, Mayer EA, et al. . Challenges in IBD research: environmental triggers. Inflamm Bowel Dis. 2019;25(Suppl 2):S13–S23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Denson LA, Curran M, McGovern DPB, et al. . Challenges in IBD research: precision medicine. Inflamm Bowel Dis. 2019;25:S31–S39. [DOI] [PubMed] [Google Scholar]
- 4. Scott FI, Rubin DT, Kugathasan S, et al. . Challenges in IBD research: pragmatic clinical research. Inflamm Bowel Dis. 2019;25(Suppl 2):S40–S47. [DOI] [PubMed] [Google Scholar]
- 5. Best WR, Becktel JM, Singleton JW, et al. . Development of a Crohn’s disease activity index. National cooperative Crohn’s disease study. Gastroenterology. 1976;70:439–444. [PubMed] [Google Scholar]
- 6. Harvey RF, Bradshaw JM. A simple index of Crohn’s-disease activity. Lancet. 1980;1:514. [DOI] [PubMed] [Google Scholar]
- 7. Cellier C, Sahmoud T, Froguel E, et al. . Correlations between clinical activity, endoscopic severity, and biological parameters in colonic or ileocolonic Crohn’s disease. A prospective multicentre study of 121 cases. The groupe d’etudes thérapeutiques des affections inflammatoires digestives. Gut. 1994;35:231–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Røseth AG, Schmidt PN, Fagerhol MK. Correlation between faecal excretion of indium-111-labelled granulocytes and calprotectin, a granulocyte marker protein, in patients with inflammatory bowel disease. Scand J Gastroenterol. 1999;34:50–54. [DOI] [PubMed] [Google Scholar]
- 9. Peyrin-Biroulet L, Sandborn W, Sands BE, et al. . Selecting therapeutic targets in inflammatory bowel disease (STRIDE): determining therapeutic goals for treat-to-target. Am J Gastroenterol. 2015;110:1324–1338. [DOI] [PubMed] [Google Scholar]
- 10. Mahapatra D, Vos FM, Buhmann JM. Active learning based segmentation of Crohns disease from abdominal MRI. Comput Methods Programs Biomed. 2016;128:75–85. [DOI] [PubMed] [Google Scholar]
- 11. Gee MS, Nimkin K, Hsu M, et al. . Prospective evaluation of MR enterography as the primary imaging modality for pediatric Crohn disease assessment. AJR Am J Roentgenol. 2011;197:224–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bruining DH, Zimmermann EM, Loftus EV Jr, et al. ; Society of Abdominal Radiology Crohn’s Disease-Focused Panel Consensus recommendations for evaluation, interpretation, and utilization of computed tomography and magnetic resonance enterography in patients with small bowel Crohn’s disease. Gastroenterology. 2018;154:1172–1194. [DOI] [PubMed] [Google Scholar]
- 13. Cosnes J, Nion-Larmurier I, Beaugerie L, et al. . Impact of the increasing use of immunosuppressants in crohn’s disease on the need for intestinal surgery. Gut. 2005;54:237–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bernstein CN, Loftus EV Jr, Ng SC, et al. ; Epidemiology and Natural History Task Force of the International Organization for the Study of Inflammatory Bowel Disease (IOIBD) Hospitalisations and surgery in Crohn’s disease. Gut. 2012;61:622–629. [DOI] [PubMed] [Google Scholar]
- 15. Olaison G, Smedh K, Sjödahl R. Natural course of Crohn’s disease after ileocolic resection: endoscopically visualised ileal ulcers preceding symptoms. Gut. 1992;33:331–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gilissen LP, Wong DR, Engels LG, et al. . Therapeutic drug monitoring of thiopurine metabolites in adult thiopurine tolerant IBD patients on maintenance therapy. J Crohns Colitis. 2012;6:698–707. [DOI] [PubMed] [Google Scholar]
- 17. Kishimoto H, Maehara M. Compliance and persistence with daily, weekly, and monthly bisphosphonates for osteoporosis in Japan: analysis of data from the CISA. Arch Osteoporos. 2015;10:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hyman N, Manchester TL, Osler T, et al. . Anastomotic leaks after intestinal anastomosis: it’s later than you think. Ann Surg. 2007;245:254–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lo B, Prosberg MV, Gluud LL, et al. . Systematic review and meta-analysis: assessment of factors affecting disability in inflammatory bowel disease and the reliability of the inflammatory bowel disease disability index. Aliment Pharmacol Ther. 2018;47:6–15. [DOI] [PubMed] [Google Scholar]
- 20. de Groof EJ, Sahami S, Lucas C, et al. . Treatment of perianal fistula in Crohn’s disease: a systematic review and meta-analysis comparing seton drainage and anti-tumour necrosis factor treatment. Colorectal Dis. 2016;18:667–675. [DOI] [PubMed] [Google Scholar]
- 21. Oussalah A, Laurent V, Bruot O, et al. . Diffusion-weighted magnetic resonance without bowel preparation for detecting colonic inflammation in inflammatory bowel disease. Gut. 2010;59:1056–1065. [DOI] [PubMed] [Google Scholar]
- 22. Froehlich JM, Waldherr C, Stoupis C, et al. . MR motility imaging in Crohn’s disease improves lesion detection compared with standard MR imaging. Eur Radiol. 2010;20:1945–1951. [DOI] [PubMed] [Google Scholar]
- 23. Quaia E, Gennari AG, Cova MA, et al. . Differentiation of inflammatory from fibrotic ileal strictures among patients with Crohn’s disease based on visual analysis: feasibility study combining conventional B-mode ultrasound, contrast-enhanced ultrasound and strain elastography. Ultrasound Med Biol. 2018;44:762–770. [DOI] [PubMed] [Google Scholar]
- 24. Lu C, Gui X, Chen W, et al. . Ultrasound shear wave elastography and contrast enhancement: effective biomarkers in Crohn’s disease strictures. Inflamm Bowel Dis. 2017;23:421–430. [DOI] [PubMed] [Google Scholar]
- 25. Lu C, Merrill C, Medellin A, et al. . Bowel ultrasound state of the art: grayscale and doppler ultrasound, contrast enhancement, and elastography in Crohn disease. J Ultrasound Med. 2019;38:271–288. [DOI] [PubMed] [Google Scholar]
- 26. Greener T, Klang E, Yablecovitch D, et al. ; Israeli IBD Research Nucleus (IIRN) The impact of magnetic resonance enterography and capsule endoscopy on the re-classification of disease in patients with known Crohn’s disease: A prospective Israeli IBD research nucleus (IIRN) study. J Crohns Colitis. 2016;10:525–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bhutiani N, Grizzle WE, Galandiuk S, et al. . Noninvasive imaging of colitis using multispectral optoacoustic tomography. J Nucl Med. 2017;58:1009–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Knieling F, Neufert C, Hartmann A, et al. . Multispectral optoacoustic tomography for assessment of Crohn’s disease activity. N Engl J Med. 2017;376:1292–1294. [DOI] [PubMed] [Google Scholar]
- 29. Abou-Elkacem L, Bachawal SV, Willmann JK. Ultrasound molecular imaging: moving toward clinical translation. Eur J Radiol. 2015;84:1685–1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wilson KE, Bachawal SV, Abou-Elkacem L, et al. . Spectroscopic photoacoustic molecular imaging of breast cancer using a B7-H3-targeted ICG contrast agent. Theranostics. 2017;7:1463–1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Abou-Elkacem L, Wang H, Chowdhury SM, et al. . Thy1-targeted microbubbles for ultrasound molecular imaging of pancreatic ductal adenocarcinoma. Clin Cancer Res. 2018;24:1574–1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Montesi SB, Désogère P, Fuchs BC, et al. . Molecular imaging of fibrosis: recent advances and future directions. J Clin Invest. 2019;129:24–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kalantar-Zadeh K, Ha N, Ou JZ, et al. . Ingestible sensors. ACS Sens. 2017;2:468–483. [DOI] [PubMed] [Google Scholar]
- 34. Amoako-Tuffour Y, Jones ML, Shalabi N, et al. . Ingestible gastrointestinal sampling devices: state-of-the-art and future directions. Crit Rev Biomed Eng. 2014;42:1–15. [DOI] [PubMed] [Google Scholar]
- 35. Zhang S, Ermann J, Succi MD, et al. . An inflammation-targeting hydrogel for local drug delivery in inflammatory bowel disease. Sci Transl Med. 2015;7:300ra128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bellinger AM, Jafari M, Grant TM, et al. . Oral, ultra-long-lasting drug delivery: application toward malaria elimination goals. Sci Transl Med. 2016;8:365ra157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Panes J. Stem cell therapy for perianal fistulas in Crohn’s disease. Gastroenterol Hepatol (N Y). 2016;12:637–640. [PMC free article] [PubMed] [Google Scholar]
- 38. Bitar KN, Zakhem E. Design strategies of biodegradable scaffolds for tissue regeneration. Biomed Eng Comput Biol. 2014;6:13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bachmann R, Leonard D, Delzenne N, et al. . Novel insight into the role of microbiota in colorectal surgery. Gut. 2017;66:738–749. [DOI] [PubMed] [Google Scholar]
- 40. Shogan BD, Belogortseva N, Luong PM, et al. . Collagen degradation and MMP9 activation by enterococcus faecalis contribute to intestinal anastomotic leak. Sci Transl Med. 2015;7:286ra68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Adamina M, Steffen T, Tarantino I, et al. . Meta-analysis of the predictive value of C-reactive protein for infectious complications in abdominal surgery. Br J Surg. 2015;102:590–598. [DOI] [PubMed] [Google Scholar]