Abstract
Environmental triggers is part of five focus areas of the Challenges in IBD research document, which also includes preclinical human IBD mechanisms, novel technologies, precision medicine and pragmatic clinical research. The Challenges in IBD research document provides a comprehensive overview of current gaps in inflammatory bowel diseases (IBD) research and delivers actionable approaches to address them. It is the result of a multidisciplinary input from scientists, clinicians, patients, and funders, and represents a valuable resource for patient centric research prioritization. In particular, the environmental triggers section is focused on the main research gaps in elucidating causality of environmental factors in IBD. Research gaps were identified in: 1) epidemiology of exposures; 2) identification of signatures of biological response to exposures; and 3) mechanisms of how environmental exposures drive IBD. To address these gaps, the implementation of longitudinal prospective studies to determine disease evolution and identify sub-clinical changes in response to exposures is proposed. This can help define critical windows of vulnerability and risk prediction. In addition, systems biology analysis and in silico modeling were proposed as approaches to integrate the IBD exposome for the identification of biological signatures of response to exposures, and to develop prediction models of the effects of environmental factors in driving disease activity and response to therapy. This research could lead to identification of biomarkers of exposures and new modalities for therapeutic intervention. Finally, hypothesis-driven mechanistic studies to understand gene-environment interactions and to validate causality of priority factors should be performed to determine how environment influences clinical outcomes.
Keywords: Crohn’s disease, ulcerative colitis, environment, exposome, smoking, antibiotic, virus, pollutant, diet, epidemiology, in silico modeling
This section is focused on the main research gaps and approaches in elucidating causality of environmental factors in IBD, including epidemiology of exposures, identification of signatures of biological response to exposures, and mechanisms of how environmental exposures drive IBD.
Environmental Triggers is part of five focus areas of the Challenges in IBD research document, which also includes preclinical human IBD mechanisms,1 novel technologies,2 precision medicine3 and pragmatic clinical research.4
The etiology of inflammatory bowel diseases (IBD) has been extensively studied. However, the causative factors are not fully understood. The importance of genetic susceptibility has been established in the last decade and genetic risk variants have been identified, but the lack of complete gene penetrance and the rapid rise of IBD incidence in certain geographic regions suggest that the interaction between genetic and environmental factors contributes to IBD. Several environmental risk factors including exposure to drugs (such as antibiotics), viruses, psychological stress, air pollutants, diet, and chemicals have been explored, but the data are still inconclusive. The main direction in this priority area is to move from association to causation through the following approaches: 1) cohort-based epidemiological studies of exposures; 2) identification and validation of signatures of biological response to exposures; and 3) mechanistic studies of how environmental factors impact disease processes. Finally, it is critical to link these research approaches to clinical outcomes, to conclusively define how environmental exposures affect disease onset, progression and response to therapy. The current knowledge, the research gaps and the potential approaches to address these gaps (Fig. 1) are described below.
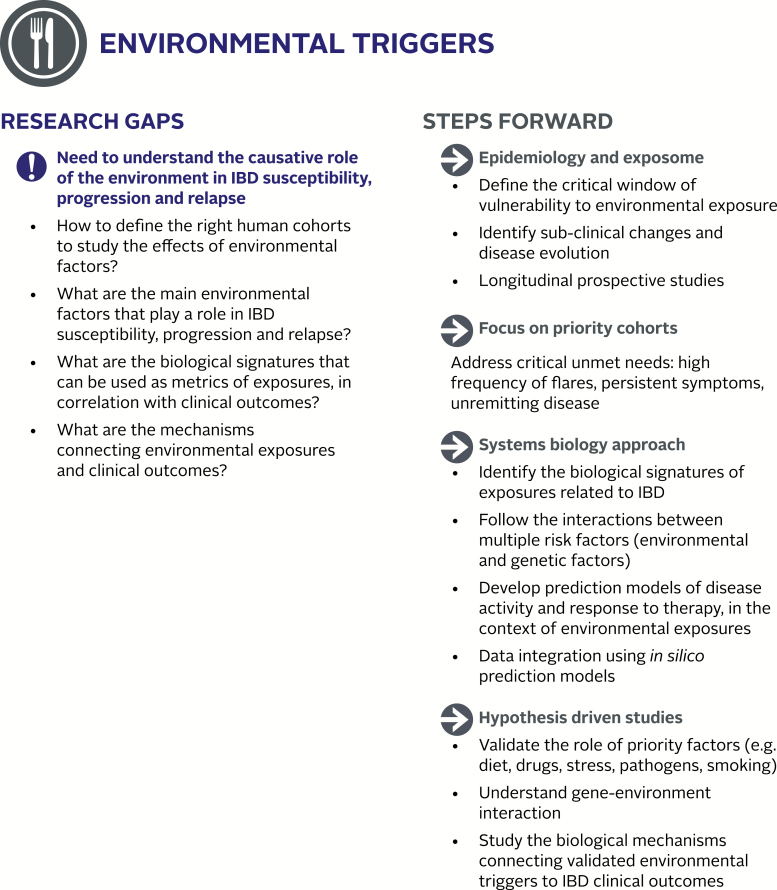
FIGURE 1.
Environmental triggers: current research gaps and proposed steps forward to advance the understanding of the role of environmental factors in IBD.
EPIDEMIOLOGY OF EXPOSURES AND DISEASE EVOLUTION: CONCEPTS IN STUDY DESIGN
Two fundamental questions about Crohn’s disease (CD) and ulcerative colitis (UC) that have yet to be answered are what causes the disease and, once the disease is in remission with medical or surgical therapy, what causes the disease to relapse. In general, IBD is thought to result from one or more environmental exposures in a genetically predisposed host. These environmental triggers allow the genetically predisposed immune dysregulation to cause an aberrant response that ultimately leads to persistent bowel and in some cases extra-intestinal inflammation. More than 200 genetic risk loci have been identified, few of which have a strong association with IBD. Rather, the contribution of the genetic loci is thought to be less than 50% with the effect being greater in CD than UC.5 Indeed, the rapidly increasing incidence of IBD associated with industrialization, first observed in Western societies and now being observed in many Asian countries,6 supports this notion. Thus, there remains great interest in understanding the role of environmental risk factors.
Environmental risk factors of great interest include, but are not limited to, the following: 1) tobacco smoking, the most well-established environmental risk factor for CD and a protective factor in most studies of UC, 2) diet, in part because it has also been used as a therapy, 3) dysbiosis of intestinal resident microorganisms and exposure to pathogens, 4) psychosocial stressors, and 5) medications such as NSAIDs, antibiotics and oral contraceptives.7 To study environmental triggers in IBD in the context of the epidemiology of exposures and disease evolution, observational epidemiology and identification of the critical window of vulnerability is needed to allow properly defining the cohorts, to account for frequency, duration and extent of exposure. The methods of observational epidemiology and reverse-translational research have and will likely continue to be employed in attempting to answer questions about environmental risk factors. Before embarking on such studies, there are a few important issues that investigators need to consider:
Presymptomatic changes leading to IBD: Among important research questions is the question of “Where does health end and illness begin?”. In clinical practice, we define the onset of inflammatory bowel disease as the time when either symptoms start or the time when the physicians first make the diagnosis. However, in most patients there has been an even longer period with the disease before this even happened. For example, Colombel et al observed that abnormal antibody responses to antigens such as S. cerevisiae (ASCA) were detectable long before the disease manifest in military recruits.8 Moreover, given the genetic contribution to the diseases, one might ask if patients are actually born with the disease in a preclinical state, waiting to accumulate environmental exposures and perhaps epigenetic changes.
Critical window of vulnerability: Knowing when disease begins is tightly linked to the question of “What is the critical exposure period for environmental exposures to cause disease?”. This is a critical question in designing studies focusing on the etiology of IBD, the answer to which is not entirely clear today. Indirect evidence from studies of immigrants suggest that early life exposures may be more important than later life exposures.9
Properly defining cohorts to study ET (environmental triggers) in IBD: Similarly, one must think about the population to study to answer the specific research question to account for disease incidence in relationship to the frequency, duration and extent of exposure.
Predicting and following disease activity: Studying disease exacerbations or loss of remission is in some ways easier than studying new onset of disease. However, even this can present technical challenges. It can be difficult to determine when the disease is truly in remission and when it has relapsed. For example, is the patient who has gone from severe symptoms and colonic inflammation to being completely asymptomatic, with a few small colonic ulcers remaining, in remission? Likewise, how many ulcers after surgery does it take to say that the person has active disease? Obviously, if colonoscopy, MRI or CT scan is needed every time we want to determine if a patient has relapsed, that will not be feasible. Therefore, new non-invasive biomarkers that accurately assess disease activity are needed. This would advance the field both clinically and from a research perspective.
Loss of response to therapy: Not all reasons for loss of response are the same. The patient who has developed antibodies to a biologic drug is different from the patient who stops responding to the same biologic drug despite adequate drug levels. Even in the latter case, not all failures are due to the same mechanism. There may be different biological drivers of disease that remain unaffected by a specific therapy, leading to treatment failure. For example, if a primary biological driver of stricture formation in a patient is not affected by anti-TNF therapy, the treatment may fail.
From observational to hypothesis-driven studies: Important research needs in this area include design of hypothesis-driven validation studies to advance from epidemiological observations to validation of potential causal effects of high priority environmental factors. Despite the vast number of association studies, validation and mechanistic studies are lagging.
High priority environmental triggers of IBD: Since the data on the causal effect of environmental triggers in IBD are almost non-existent, one approach is to focus on triggers with previously-established strong associations with IBD to ensure faster return on effort and patient-valued impact in the short-term future. These high priority factors include diet, the gut microbiota, viral exposures, smoking, antibiotics, fungi, and psychosocial stress. Identification of the biological signatures caused by exposure to these factors is needed to direct investigators towards mechanistic studies and development of novel interventions. Below is the description of the research gaps in a few of these areas.
Psychosocial Stress
In the context of IBD, psychosocial stress represents a perturbation of the homeostatic state of brain gut microbiome (BGM) interactions in response to events in the environment. Stress-related perturbations include increased intestinal permeability, immune system modulation and modulation of microbial gene expression and virulence by luminally released norepinephrine.10 Current literature suggests that it is the subjectively “perceived” stress, and not the objective number or severity of stressful events that is related to frequency and severity of disease flares in IBD.11–13 The sensitivity and responsiveness to stress is determined by genetic and epigenetic factors on the stress system and different brain networks the latter including the epigenetic effects within the hypothalamic pituitary (HPA) axis in response to exposure to early adverse life events. There are well-characterized brain networks that play a role in the response to stressful life events, including the salience network (determines the subjective relevance of events for an individual), the stress network, and the central autonomic nervous system (ANS) output. As described above, it is assumed through observations that psychological stress exacerbates IBD flares, but little is known about brain-gut communications and the molecular interplay between intestinal and neuronal molecules that may play a role in IBD and that may represent a biomarker of disease related clinical manifestation.
Diet
There are at least two aspects of diet that may be involved in IBD flares: 1) the proinflammatory effects of a typical Western diet, which is low in fiber and high in animal fat, sugar, emulsifiers and other chemical additives used in processed food. In rodent experiments, such a diet, or its components is associated with gut microbial changes, a reduction of the intestinal mucus layer and resultant increase in intestinal permeability and activation of the gut associated immune system. 2) Modern production practices afford opportunities to change not only the fundamental composition of food but also introduce many understudied additives and pollutants, such as pesticides, polychlorinated biphenyls, preservatives, and heavy metals, which may serve as triggers of IBD.14 This could be changing metabolites generated by gut microbiota in response to alterations in food composition and the introduction of various additives such as artificial sweeteners15 and emulsifiers.16 The impact of dietary factors and pollutants as an environmental trigger of IBD symptoms have been extensively reviewed14, 17, 18 and will only be lightly touched in this section. Since dietary intolerance is a common etiological suspect of symptoms, many patients and physicians have taken food elimination or exclusion to the extreme with only limited evidence-based support, although more promising evidence has begun to emerge more recently.19 An exception to this is the use of elemental and other defined formula diets for CD, with a significant amount of evidence published,19 notably suggesting that exclusive enteral nutrition has similar efficacy as steroids for induction of remission in pediatric CD.20
Intestinal Microbiota and Pathobionts
There is substantial data indicating that the resident gut microbiota (which includes bacteria, viruses, mycobiota, and meiofauna including worms, protists and other organisms) is one aspect of intestinal biology that is influenced by the environment. The microbiome plays a substantial role in controlling normal function of the intestine and contributes to inflammation and systemic disease as well as both CD and UC.21 Much emphasis has been placed on the bacterial microbiome in part due to the ready availability of effective and inexpensive computational tools for analyzing the population structure of complex bacterial communities through analysis of 16S rRNA gene diversity. Computational tools for other components of the microbiome are less well established but are being developed and have been successfully applied. These include analysis of the virome which is altered and has a relationship to the bacterial microbiome in IBD.22 Animal studies provide overwhelming support for the regulation of intestinal inflammation by bacteria, but also show that other components of the microbiome including viruses,23, 24 protists25 and fungi26 fundamentally alter intestinal inflammation. It is very likely that additional associations between components of the microbiome and IBD will be discovered. It is also clear that interactions between different components of the microbiome have significant effects on intestinal biology,27, 28 further underlining the complexity of the relationships between the microbiome and IBD.
Several important factors limit the impact of this area of IBD research. First, most studies have been cross-sectional and merely identify associations between a component of the microbiome and disease; longitudinal studies have not defined associations between the microbiome and disease activity or causation. Second, mechanisms responsible for observed associations are poorly understood, although some information is emerging.29 Lastly, lack of mechanistic insights into the relationship between the environment, the microbiome, and IBD have prevented the development of broadly effective therapeutic interventions that matter to patients.
Dysbiosis of the Gut Microbiota
There has long been interest in single organisms that play a role in the pathogenesis of IBD, such as Mycobacterium paraturberculosis30, 31 and adherent-invasive E. coli recent evidence supports the notion and the overall alteration in the composition of the gut microbiota associated with IBD, known as dysbiosis, may be important in disease pathogenesis. Dysbiosis of the gut microbiota develops in response to the intestinal inflammatory response via the production of alternative electron acceptor facilitating anaerobic respiration with an outgrowth of facultative anaerobes such as Enterobacteriaceae32 or inducing oxidative stress leading to the predominance of aerotolerant bacteria taxa belonging to the Proteobacterium phylum.33 In turn, studies in murine model systems suggests that the dysbiotic microbiota in IBD may play a role in the pathogenesis of disease,34, 35 a notion supported in patients with IBD based on preliminary evidence that fecal microbiota transplantation (FMT) is efficacious in the treatment of ulcerative colitis after multiple inoculations36 and that meaningful clinical responses have been observed in patients with refractory IBD who have received a combination of multiple antibiotics.37 Nevertheless, despite substantial mechanistic data that a dysbiotic microbiota plays a role in murine intestinal inflammation,35, 38 much more evidence is needed to determine if these findings can be reproduced in human IBD. Such evidence may be forthcoming based on ongoing industry sponsored clinical studies testing the safety and efficacy of gut microbiota therapeutics for IBD.
Pathobionts
Bacterial, viral, parasitic infections have been proposed to act as a trigger for the initial clinical presentation of IBD, thereby suggesting a role in the pathogenesis of this disease.39 Such organisms may enter human body through food and contaminated water. Many of these microbial organisms can reside in healthy individuals and elicit no adverse effects and yet, in susceptible populations the impacts are significant.40, 41 hence the term pathobiont. The differential susceptibility can in part be explained by genetics. Alternatively, the mucosal barrier, resident mast cells and other immunological response regulators can be important determinants for disease development, recurrence and progression. However, it is usually difficult to study the mucosal barrier and tissue organization at real-time and over a long period (i.e. a longitudinal approach). For these reasons, the use of surrogate biomarkers for patient stratification (e.g. susceptible versus resistant) are in great need
There is evidence to support a role for the intestinal fungi (the mycobiota) in the pathogenesis of IBD. Glycoprotein cell wall components can activate components of the innate immune system leading to immune signaling via molecules such as CARD9, interleukin 17 (IL17), interleukin 22 (IL22), NF-ĸB, NFAT, and ITAM.42 Evidence in murine model systems supports a functional role for fungi in the pathogenesis of IBD and a comprehensive review on this topic has recently been published.43 For example, CLEC7A knockout mice have increased susceptibility to chemically induced colitis due to their altered responses to indigenous fungi and a variant in the gene encoding dectin-1 is associated with a severe form of UC in humans.26 Observations from mice parallel the role for fungi in the pathogenesis of IBD in humans. Antibodies against Saccharomyces cerevisiae, a marker of CD, react with mannan, a yeast cell wall polysaccharide.44 Multiple studies have shown that patients with IBD have alterations to the gut mycobiota; increases in specific fungal taxa have been associated with bacterial dysbiosis, increased human DNA in feces, and antibiotic use.45 Furthermore, a recent study reported expansion of Candida tropicalis in patients with CD, and that levels correlated with those of anti-S cerevisiae, E coli, and Serratia marcescens; these 3 markers formed enhanced biofilms in mucosal samples patients with CD.46 Finally, there is preliminary evidence that the anti-fungal agent fluconazole reduces inflammation mice with colitis and patients with IBD.47
Pollutants and Toxicants
Our water and air are increasingly polluted by various toxicants that are potential triggers for IBD. This is especially true with introduction of thousands of new chemicals to our environment annually with few being tested thoroughly using animal models. Particulate matter, NO2, SO2 and other related pollutants derived from incomplete fossil fuel combustion smoking can penetrate the GI tract barrier and cause oxidative stress, DNA damage and immune responses leading to IBD.48–51 Drinking water can also contain toxicants including heavy metals,52 and chemicals introduced as a result of hydraulic fracturing.48–51, 53 The high frequency of radiation pollution of food and water sources from failed nuclear plants (Chernobyl and Fukushima) have been added to the long list of unknown, under-characterized, potential environmental triggers of IBD. Epidemiology studies have demonstrated that early-life exposure to radiation may be associated with IBD in children. Many of these environmental agents are thought to have significant impacts on the immune system of vulnerable populations. It is worth noting that high-throughput in vitro models can be used to simultaneously detect the biological response or signatures to thousands of candidate pollutants or toxicants.54–56
Tobacco is one of the sources of toxicants; however, the effect of smoking on IBD is a focus of ongoing investigation. The robust relationship of smoking and IBD has been demonstrated across geographic populations. Moreover, this epidemiologic finding shows opposing effects between CD and UC, with smoking being protective against UC while being a risk for developing CD. Indeed, this may be one of the strongest pathogenic differentiators between CD and UC described. In UC, a systematic review and meta-analysis demonstrated a 3-fold increase in lifetime risk of UC in non-smokers compared to smokers. Ex-smokers also have an increased likelihood of developing UC.57 Smoking is not only a risk factor for the development of CD, but numerous studies confirmed that smokers have increased risk of flares, surgery and postoperative recurrence.58 Likewise, the odds of these complications seem to decrease upon smoking cessation suggesting that this is a disease modifying intervention.59 A recent publication identified 64 SNPs for which the association between the SNP and IBD were modified by smoking behavior. Indeed, functional gene smoking interactions were suggested in two models of experimental colitis where genetic deficiency in IL-10 and NOD2 were also identified as potential human smoking-interaction genes in this study.60 Nonetheless, major knowledge gaps exist in understanding basic mechanisms of smoking effects in terms of gene-smoking-immune system-microbiota interactions, and the opposing epidemiologic findings in CD versus UC.
SIGNATURES OF BIOLOGICAL RESPONSE TO EXPOSURES: THE EXPOSOME
To better understand the link between environmental exposures and disease, we need to identify the signatures of exposure, namely, measurable indicators of biological response to environmental factors, and how they relate to changes in biomarkers of disease onset, disease progression and response to therapy, which also need to be identified and qualified. Currently our knowledge of such metrics, i.e. genetic, epigenetic, metabolic, immunological, microbiological and other molecular signatures is very limited.
Current understanding of complex disease indicates that no single exposure can fully explain the etiology and natural history of a disease. The effects of exposure/triggers are often multifactorial, often occurring as combinations of endogenous triggers and multiple external environmental triggers including diet, chemicals and psychological stress. Unfortunately, the majority of epidemiologic studies in IBD have only examined the impact of a single chemical/trigger on disease development and outcomes.61 This approach does not reflect the real-world relationship between often interacting exposures to multiple factors and disease development. A more accurate descriptor of environmental triggers for disease development is the concept of the exposome,62–65 which can be defined as the cumulative or acute impact of all the exposures of an individual in a lifetime and how these exposures interact with the individual’s genome to elicit or prevent the onset, recurrence and/or progression of a disease. According to this concept, exposures at early-life66 or other windows of vulnerability, as well as exposures to a combination of triggers/agents concurrently or in certain temporal sequences, are crucial determinants of disease onset and outcomes.67, 68 In this regard, the exposome concept goes hand in hand with the notion of genetic heterogeneity in supporting a precision medicine approach to treat and prevent human diseases.62, 63 However, the implementation of such an approach requires significant advancements in our ability to measure accurately multiple exposures as well as all components within the exposome. Methodologies to detect the interactions and to integrate information across the exposome-disease interface are still lacking, particularly for complex diseases and specifically for IBD. In connection to this research gap, identification of multiparametric signatures of exposures is needed to provide a full picture of exposome in IBD. A recent study of primary sclerosing cholangitis, which is comorbid with IBD, has been funded by NIH to explore exposomic and genomic triggers. Another approach to multiparametric analysis can be exemplified by nutrigenomics studies, focused on different phenotypic response to diet, depending on the genotype of each individual.69 In this context, nutrigenetics investigates how genetic susceptibility factors interact with environmental factors, including the diet and gut microbiota, and identifies the signatures of exposures to a nutrient or diet based on comprehensive whole genome analysis and microbiome-based data.70 Moreover, given the interpersonal variability integrating multiple signatures, such as genome sequences, clinical tests, blood metabolome and proteome, fecal microbiome, as described,71 can be used to generate correlation networks and provide stronger evidence of the causal relationship between the exposure and the biological responses.
Given the complexity of the exposure and history of exposure new methods for measuring biological consequences in response to these exposures present a major challenge in the field. As such the challenge is to be able to analyze the massive amount of data coming from multi-omics analyses of target tissues (biopsies) to gain a better understanding of the etiology of the disease as it related to the complex triggers and trigger-trigger interaction. Thus far, only a few classes of endogenous and exogenous triggers related to IBD have been studied.14, 17, 18, 48–51, 72–74 New bioinformatics and statistical methods for studying mixtures are needed to advance the field.
MECHANISMS OF HOW ENVIRONMENTAL EXPOSURES DRIVE IBD
To build the research continuum and advance towards diagnostics and therapeutic interventions, we need to validate the outcomes of the newly identified candidate signatures through investigating of the mechanisms by which environmental exposures can lead to perturbations in biological processes believed to play a role in IBD. For this purpose, we need relevant model systems (animal models or patients).
Multiple models are available to study IBD related molecular networks. These include genetic models such as IL-1 mutants, chemically induced IBD models (DDS) and intestinal organoids, etc. To study the mechanisms that connect environmental triggers and IBD relevant model systems (animal models or patients) should be used to test a specific hypothesis. Studies are needed to establish the mechanisms by which combination of genetic risk factors and environmental triggers lead to disease (computational prediction models and animal models). Development of better animal models is needed to study mechanisms by which environmental exposures could impact remission, disease flares, complications and response to treatment. Finally, a reverse-translation approach, that starts with clinical observations of vulnerability to exposures during disease development or over the course of life, should lead to hypothesis-based studies that can be implemented in the laboratory to identify the underlying biological changes related to disease onset and progression in response to exposures.
STEPS FORWARD TO ADVANCE THE UNDERSTANDING OF ENVIRONMENTAL TRIGGERS IN THE PATHOGENESIS OF IBD
Comprehensive Characterization of the Exposome in IBD
The exposome is defined as the totality of human environmental exposures from conception onwards.62, 63, 75 In this regard, the concept that IBD is yet another complex disease that originates from early-life76 should be considered. In this context, the window of vulnerability can be extended from prenatal77, 78 to pre-conception period79 and other developmental stages including puberty, pregnancy and aging. If new onset IBD in adults is due to exposures that occurred in early childhood, the feasibility of such studies retrospectively will be extremely limited. In the short term, research looking at presymptomatic immune dysregulation, microbiome changes, serology, etc. could help define the presymptomatic latent phase of IBD. To perform these studies, it will be critical to acquire human samples in well-designed epidemiology studies that allow for gene by environmental trigger studies to be performed by taking advantage of technological advances in deep analytics to define new signatures for precision medicine IBD. Such studies may provide much needed new insights into the role that environmental factors play in disease pathogenesis. The broad sharing of data generated from epidemiological, clinical and experimental studies is highly desirable to leverage the IBD communities’ investment in these studies and advance the field of environmental trigger for the disease. Collectively, these new initiatives are aimed at advancing precision medicine-based disease risk assessment, monitoring, prevention and therapies. The overall objectives for the next five years could be accomplished through: 1) expert consultation services in medicine, epidemiology, exposure science, and statistics, 2) sharing resources of cohorts with environmental exposure data and biorepositories, 3) building a core of expertise in analysis of exposure mixtures, 4) informatics tools and, 5) “Integrative Thinking” transdisciplinary workshops that will mesh information from various disciplines for translation to the bedside and precision medicine for IBD.
Since resources are always limited, priorities should focus on the “priority” cohorts to study the signatures of environmental exposures. These may include patients with extreme phenotypes such as high frequency of flares or with persistent symptoms after mucosal healing. It is now well-recognized that chronic low-grade exposure may elicit responses drastically different from those caused by acute exposure; and both might lead to development of common complex diseases. There is mounting evidence indicating that the lag time for disease development, especially for low-dose exposure, could be very long. In some cases, it may extend out several decades, which is the basis for the emerging field known as “Developmental Origins of Health and Disease” (DoHAD).
It is important to realize that individuals or populations are not equally endowed. Marked genetic variations predispose their unique susceptibilities to a particular exposure. Hence, the interplay between genes and exposures, window of susceptibility, life-style or life-stages modifiers, and their complex interactions are all crucial data gaps to be filled. With the completion of the Human Genome Project and twenty years of genome-wide association studies (GWAS) the next challenge resides in defining the influences of specific environmental factors, in particular their effect on the epigenome, in a specific cell/organ, during critical developmental times.
To fill these knowledge gaps, multidisciplinary systems biology approaches using multi-omics platforms on human biospecimens tied to impeccable clinical databases will advance the IBD field. Analyses of these gargantuan data sets require sophisticated informatics and machine learning. Special attention has been paid to early origin of disease, windows of vulnerability (prenatal, in utero, puberty, pregnancy and old age), the interplay between genetics and epigenetics, genetics, epigenetics with other omics (proteomics, metabolomics, metagenomics, and metallomics), the influences of life style modifiers such as diet or stress on epigenetic reprogramming, and finally the data void related to continuous life-long editing of early developmental program.
Ultimately, some future directions for IBD research focused on the exposome include:
Expansion of comparative population-based exposure studies focusing large and ethnically diverse cohorts. For example, an attractive way to assess the impact of stressful life events on IBD outcomes would be to study a large number of patients (1,000+) with frequent online sampling of subjective symptoms (online questionnaires), stool and blood samples for gut microbial metabolites and for stress-related changes. There are now commercial entities that can perform such large-scale studies enrolling patients online almost exclusively relying on the assessment of ambulatory questionnaire and biological information. Out of the collected data, applying machine-learning approaches, it is possible to extract meaningful correlations and causal relationships between stressfully perceived life events and various biological outcomes.
Emphasis on emerging environmental triggers (e.g. nanomaterials, triggers related to climate change related disasters). Untargeted metabolomics and exposomics are a promising strategy to capture information about emerging or unknown environmental triggers.
Development of ambulatory, wearable systems to continuously monitor responses to exposures in real life situation. In terms of stress, there are several reliable wearable devices which can assess the impact of stress on an individual. Approaches that are being evaluated include ambulatory assessment of heart rate variability/vagal tone, ambulatory assessment of skin conductance (sympathetic nervous system activity), sleep patterns, relative time spent in bathroom, physical activity.
The development of novel statistical and bioinformatics methods for analyzing, identifying and mathematically modeling the individual component and/or interactive effects of a multiple exposures. For example, it is now possible based on results from mechanistic studies in animals and large studies in humans to create mathematical (systems biological) models of the circular interactions between the brain, gut, and gut microbes. Feeding biological data into these systems makes it possible to quantitate the impact of life events perceived as stressful by an individual with increased stress responsiveness on biological readouts such as mucosal inflammation, pain and discomfort etc. Multi-omic analysis is being addressed by many research groups. It is critical not to reinvent the wheel for IBD, but rather to partner with collaborators with similar interests. The fundamental challenge of curating, integrating and analyzing large data sets applies to nearly every area of contemporary IBD research discussed in this section and others, as data generation becomes more efficient and expands in scope. Importantly, appropriately designed cohorts with control populations should also give us significant insight into wellness, what makes one patient “mild” or “quiescent” and the appropriate thresholds in different settings, which could be translated into novel lower-risk treatment paradigms.
Emerging new focus on mitochondrial genomics and epigenomics to better understand maternal “inheritance”.
Continued acceleration of application of artificial intelligence to multiparametric analysis of exposome-derived data and related clinical metadata.
Platforms to study single-cell ‘omics’ signatures to uncover mechanisms underlying heterogeneity in cellular and personal responses to environmental perturbations. Collectively, these new initiatives are aimed at advancing IBD trigger research towards precision medicine-based disease risk assessment, monitoring, prevention and therapies.
CONSIDERATIONS OF STUDY COHORT DESIGN FOR THE CHARACTERIZATION OF THE EXPOSOME IN IBD
One can divide populations into those with a high or low incidence of IBD. A potential advantage of a high incidence population is the ability to identify very high incidence subpopulations and follow them prospectively. In contrast, if one is designing a population-based study in a high prevalence region, it is possible that ubiquitous risk factors with small effect sizes have contributed to the high prevalence and the ubiquitous nature of the risk factor will make it difficult to detect the association. In contrast, in areas where the incidence of IBD is just beginning to rise, one could speculate that the key environmental risk factors may also be rising as well and that there would be less universal exposure, therefore increasing the ability to detect the association with new onset IBD. Groups with potential high yield for studying etiologic factors in disease incidence include: 1) children under age 10, which are a population with rising incidence rates even in developing countries,80 because their lives are less experienced and easier to track with parents included to help map what has happened to them, 2) the elderly who like have different phenotypes and different risk factors for IBD than children, 3) individuals living in rapidly industrializing societies such as those in Asia including China and India, and 4) immigrants. For example frameworks for such studies, see Table 1.
Table 1:
Example Framework of Cohort and Case-Control Studies of Risk Factors for IBD
| Study population | Design | Clinical data collected | Biosamples collected | Follow-up period |
|---|---|---|---|---|
| Children of parents with IBD | Prospective cohort study | Diet history; Infections, medications; Mental and physical health information |
Blood and stool collected at birth and serially thereafter | Birth to age 18 |
| Patients over age 65 newly diagnosed with IBD and control patients without IBD | Case-control study | Diet history prior to diagnosis; Other lifestyle factors prior to diagnosis; Medication history prior to diagnosis; Psychological surveys at diagnosis; Infection history; Tobacco use |
Stool and blood samples at diagnosis and index date for controls | Not applicable |
| Immigrants newly diagnosed with IBD and immigrants without IBD | Case-control study | Breastfeeding information from birth (from parents); Infection and medication use including antibiotic use from birth; psychological surveys at diagnosis; Tobacco use; Age at immigration; Region of immigration; Living conditions before and after immigration |
Stool and blood samples at diagnosis and index date for controls | Not applicable |
Studies seeking to understand the role of the environment in underlying biology of IBD through studying relapse of disease need to consider why patients have relapsed. As such, not all patient groups will be equally informative. Here, we propose a few populations that may lend themselves to use in studies of environmental risk factors for disease flare. These include patients who have undergone a surgery for CD, patients only taking mesalamine or diet-based therapies given the non-immunosuppressive nature of these therapies, and those patients in deep and stable remission who elect to discontinue their medical therapy.
There should be an emphasis in studying the interactions between multiple exposures, or the temporal sequences of exposure to major triggers, an approach which traditionally has not been the focus of IBD research which has focused on single types of exposures. For example, psychosocial stress, dietary factors, food additive and pollutants have all been shown in rodent models to affect intestinal permeability, intestinal immune activation and microbial composition and function. In humans, the genetic heterogeneity presumably plays an important role in determining which patient will develop IBD or experience a flare to a single category of these exposures, and in which patients a combination of exposures is required to result in symptoms. The lack of information or study focus is due in part to the lack of methodologies to tease out the individual of combinatorial effects of the exposures and their biological outcomes in animal models or in patients. To identify both the impact of an individual trigger, as well as the potential associations of multiple triggers, and to characterize the interactions, and cumulative effects of multiple triggers, is critically needed to understand the role of environmental triggers in the etiology of IBD.
For example, there are several ways of quantifying the biological response to stress in humans:
Multimodal brain imaging, assessing the engagement of different brain networks to a laboratory stressor, and the altered responsiveness and structure of relevant brain networks.
Measurement of HPA axis and ANS responses to a laboratory stressor
Assessment of gut microbiome and stool metabolite changes in response to stress (reduction of lactobacilli, changes in tryptophan metabolites)
Assessment of intestinal permeability and systemic immune activation in response to chronic stress,
Untargeted metabolomics to capture network level changes in stress-related biochemistry
The traditional target measurements may not be informative for the treatment of patients as individuals. The identification of “fingerprints” or unique signatures associated with exposures which can predict disease development and evolution in vulnerable individuals will advance the field. In this context the use of unbiased multi-omics approaches as read outs will help patient stratification. This requires promotion and fostering of integrative transdisciplinary thinking and approaches in environmental triggers of IBD among clinicians, epidemiologists, and basic scientists. A system biology approach that integrate multiple platforms of signatures including genomics, epigenomics, proteomics, metabolomics and microbiomics with exposomics as readouts of disease states associated with environmental triggers is an opportunity that can individualize patient treatment and management. An important limitation to such data driven approaches is the required sample size (1,000+) and to a lesser degree computing power.
Extensive medical records, dietary recalls, ambulatory stress assessments (using mobile apps), and spectrometry-based exposome measurements81 during different stages of disease evolution are needed to construct a comprehensive platform for integrating the omic-based readouts of environmental triggers for IBD. Significant advancements in qualitative method development including novel statistical and bioinformatics methods, machine learning, data integration and visualization and new tools in clinical informatics will be the absolute necessity for realizing the power of omics signatures for any disease including IBD.
MOVING FROM ASSOCIATION IN THE EXPOSOME TO CAUSATION
From a disease management point of view, it is not always possible to assess the target tissues, hence evidence-based determination of what kind of tissues or cell types could be used as surrogate tissues (e.g. blood cells, buccal cells, fecal cells, urine) for characterizing flares, remissions, and drug responsive and non-responsiveness, with high concordance will forge the field forward. In studying the mechanisms, we need to address what are the cause-and-effect and whether this can be reversed. Understanding these relationships may elucidate the course of biological events that lead to various clinical manifestations and may help to address our challenge of having a heterogeneous cohort. Future studies should focus on the elucidation of how exposures to environmental triggers could lead to alterations in IBD relevant functions and its relation to particular clinical outcomes. Optimally, subsequent to the identification of environmental signatures associated with IBD, studies should optimally be designed to determine the mechanism(s) by which these exposures to play a role in in the pathogenesis of IBD. No doubt that these studies will be challenging to conceptualize, design, and execute in humans. One approach might involve small cohort studies, with high stringency analytics to identify the right computational tool to further study host response mechanisms. Such an approach might be integrative in nature ultimately requiring validation in a larger cohorts. High dimensional and biostatistical approaches, possibly involving deep learning and artificial intelligence, may play a role in helping to connect the mechanism to environmental signatures. For example, such approaches may help integrative analysis combining genetic risk factors and environmental triggers to identify potential cross-talk among the biological pathways affected by both factors. When identifying protective factors studies could involve both human investigation and animal models. Longitudinal sample collection should be performed in animal models and validated in humans to identify the critical windows of vulnerability and the long terms effect of one-time verses persistent exposure. Finally, from a technical standpoint in culture-based and animal model systems, Crispr/Cas9 technology for gene editing performed in existing animal models and in organoid systems may allow to introduce multiple genetic factors and superimpose that with the effects of environmental triggers.
ACKNOWLEDGMENTS
The authors thank Rosemary Bianculli for design of figures; Orna Ehrlich for coordination with the publisher; Rebecca Kaplan for facilitating public comments; and the following individuals for review and recommendations on the manuscript: Robert Hinton; Douglas Levine; Jeremy Adler; Neil Hyman; Sridhar Mani; Antonina Mikocka-Walus; Chao Li; Carolina Ciacci; Damian Garcia-Olmo; J. Todd Kuenstner; Maria Lia Scribano; Alan Baird; Emina Huang; Giovanni C. Actis; Harris Ahmad; Herbert Van Kruiningen; J.M. Mullin; Pietro Tonelli; Richard M Soll; Simone Saibeni and Ulla Knaus.
Supported by: Crohn’s & Colitis Foundation
REFERENCES
- 1. Pizarro TT, Stappenbeck TS, Rieder F et al. Challenges in IBD research: preclinical human IBD Mechanisms. Inflamm Bowel Dis. 2019;25(Suppl 2):S5–S12. [DOI] [PubMed] [Google Scholar]
- 2. Dhyani M, Joshi N, Bemelman WA et al. Challenges in IBD research: novel technologies. Inflamm Bowel Dis. 2019;25(Suppl 2):S24–S30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Denson LA, Curran M, McGovern DPB et al. Challenges in IBD research: precision medicine. Inflamm Bowel Dis. 2019;25(Suppl 2):S31–S39. [DOI] [PubMed] [Google Scholar]
- 4. Scott FI, Rubin DT, Kugathasan S et al. Challenges in IBD research: pragmatic clinical research. Inflamm Bowel Dis. 2019;25(Suppl 2):S40–S47. [DOI] [PubMed] [Google Scholar]
- 5. Ye BD, McGovern DP.. Genetic variation in IBD: progress, clues to pathogenesis and possible clinical utility. Expert Rev Clin Immunol. 2016;12:1091–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ng SC, Bernstein CN, Vatn MH, et al. ; Epidemiology and Natural History Task Force of the International Organization of Inflammatory Bowel Disease (IOIBD) Geographical variability and environmental risk factors in inflammatory bowel disease. Gut. 2013;62:630–649. [DOI] [PubMed] [Google Scholar]
- 7. Ananthakrishnan AN, Bernstein CN, Iliopoulos D, et al. Environmental triggers in IBD: a review of progress and evidence. Nat Rev Gastroenterol Hepatol. 2018;15:39–49. [DOI] [PubMed] [Google Scholar]
- 8. Choung RS, Princen F, Stockfisch TP, et al. ; PREDICTS Study Team Serologic microbial associated markers can predict Crohn’s disease behaviour years before disease diagnosis. Aliment Pharmacol Ther. 2016;43:1300–1310. [DOI] [PubMed] [Google Scholar]
- 9. Li X, Sundquist J, Hemminki K, et al. Risk of inflammatory bowel disease in first- and second-generation immigrants in Sweden: a nationwide follow-up study. Inflamm Bowel Dis. 2011;17:1784–1791. [DOI] [PubMed] [Google Scholar]
- 10. Rhee SH, Pothoulakis C, Mayer EA.. Principles and clinical implications of the brain-gut-enteric microbiota axis. Nat Rev Gastroenterol Hepatol. 2009;6:306–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wintjens DSJ, de Jong MJ, van der Meulen-de Jong AE, et al. Novel perceived stress and life events precede flares of inflammatory bowel disease: a prospective 12-month follow-up study. J Crohns Colitis. 2018. [DOI] [PubMed] [Google Scholar]
- 12. Bernstein CN, Singh S, Graff LA, et al. A prospective population-based study of triggers of symptomatic flares in IBD. Am J Gastroenterol. 2010;105:1994–2002. [DOI] [PubMed] [Google Scholar]
- 13. Singh S, Graff LA, Bernstein CN.. Do NSAIDs, antibiotics, infections, or stress trigger flares in IBD?Am J Gastroenterol. 2009;104:1298–313; quiz 1314. [DOI] [PubMed] [Google Scholar]
- 14. Alvarez PA, Boye JI.. Food production and processing considerations of allergenic food ingredients: a review. J Allergy (Cairo). 2012;2012:746125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Suez J, Korem T, Zeevi D, et al. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature. 2014;514:181–186. [DOI] [PubMed] [Google Scholar]
- 16. Chassaing B, Koren O, Goodrich JK, et al. Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nature. 2015;519:92–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Atkinson W, Sheldon TA, Shaath N, et al. Food elimination based on igg antibodies in irritable bowel syndrome: a randomised controlled trial. Gut. 2004;53:1459–1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Iizuka K. The role of carbohydrate response element binding protein in intestinal and hepatic fructose metabolism. Nutrients. 2017;9:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Albenberg LG, Wu GD.. Diet and the intestinal microbiome: associations, functions, and implications for health and disease. Gastroenterology. 2014;146:1564–1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Narula N, Dhillon A, Zhang D, et al. Enteral nutritional therapy for induction of remission in crohn’s disease. Cochrane Database Syst Rev. 2018;4:CD000542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Stappenbeck TS, Virgin HW.. Accounting for reciprocal host-microbiome interactions in experimental science. Nature. 2016;534:191–199. [DOI] [PubMed] [Google Scholar]
- 22. Norman JM, Handley SA, Baldridge MT, et al. Disease-specific alterations in the enteric virome in inflammatory bowel disease. Cell. 2015;160:447–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kernbauer E, Ding Y, Cadwell K.. An enteric virus can replace the beneficial function of commensal bacteria. Nature. 2014;516:94–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cadwell K, Patel KK, Maloney NS, et al. Virus-plus-susceptibility gene interaction determines Crohn’s disease gene atg16l1 phenotypes in intestine. Cell. 2010;141:1135–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chudnovskiy A, Mortha A, Kana V, et al. Host-protozoan interactions protect from mucosal infections through activation of the inflammasome. Cell. 2016;167:444–456.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Iliev ID, Funari VA, Taylor KD, et al. Interactions between commensal fungi and the C-type lectin receptor dectin-1 influence colitis. Science. 2012;336:1314–1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pfeiffer JK, Virgin HW.. Viral immunity. Transkingdom control of viral infection and immunity in the mammalian intestine. Science. 2016;351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Osborne LC, Monticelli LA, Nice TJ, et al. Coinfection. Virus-helminth coinfection reveals a microbiota-independent mechanism of immunomodulation. Science. 2014;345:578–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kaiko GE, Ryu SH, Koues OI, et al. The colonic crypt protects stem cells from microbiota-derived metabolites. Cell. 2016;165:1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. McNees AL, Markesich D, Zayyani NR, et al. Mycobacterium paratuberculosis as a cause of Crohn’s disease. Expert Rev Gastroenterol Hepatol. 2015;9:1523–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kuenstner JT, Naser S, Chamberlin W, et al. The consensus from the Mycobacterium avium ssp. paratuberculosis (MAP) Conference 2017. Front Public Health 2017;5:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Winter SE, Lopez CA, Bäumler AJ.. The dynamics of gut-associated microbial communities during inflammation. EMBO Rep. 2013;14:319–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Morgan XC, Tickle TL, Sokol H, et al. Dysfunction of the intestinal microbiome in inflammatory bowel disease and treatment. Genome Biol. 2012;13:R79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zhu W, Winter MG, Byndloss MX, et al. Precision editing of the gut microbiota ameliorates colitis. Nature. 2018;553:208–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Furusawa Y, Obata Y, Fukuda S, et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature. 2013;504:446–450. [DOI] [PubMed] [Google Scholar]
- 36. Paramsothy S, Kamm MA, Kaakoush NO, et al. Multidonor intensive faecal microbiota transplantation for active ulcerative colitis: a randomised placebo-controlled trial. Lancet. 2017;389:1218–1228. [DOI] [PubMed] [Google Scholar]
- 37. Turner D, Levine A, Kolho KL, et al. Combination of oral antibiotics may be effective in severe pediatric ulcerative colitis: a preliminary report. J Crohns Colitis. 2014;8:1464–1470. [DOI] [PubMed] [Google Scholar]
- 38. Atarashi K, Honda K.. Microbiota in autoimmunity and tolerance. Curr Opin Immunol. 2011;23:761–768. [DOI] [PubMed] [Google Scholar]
- 39. Beatty JK, Bhargava A, Buret AG.. Post-infectious irritable bowel syndrome: mechanistic insights into chronic disturbances following enteric infection. World J Gastroenterol. 2014;20:3976–3985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Geremia A, Biancheri P, Allan P, et al. Innate and adaptive immunity in inflammatory bowel disease. Autoimmun Rev. 2014;13:3–10. [DOI] [PubMed] [Google Scholar]
- 41. Thomas S, Izard J, Walsh E, et al. The host microbiome regulates and maintains human health: a primer and perspective for non-microbiologists. Cancer Res. 2017;77:1783–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Underhill DM, Iliev ID.. The mycobiota: interactions between commensal fungi and the host immune system. Nat Rev Immunol. 2014;14:405–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Richard ML, Lamas B, Liguori G, et al. Gut fungal microbiota: the Yin and Yang of inflammatory bowel disease. Inflamm Bowel Dis. 2015;21:656–665. [DOI] [PubMed] [Google Scholar]
- 44. Prideaux L, De Cruz P, Ng SC, et al. Serological antibodies in inflammatory bowel disease: a systematic review. Inflamm Bowel Dis. 2012;18:1340–1355. [DOI] [PubMed] [Google Scholar]
- 45. Lewis JD, Scott FI, Brensinger CM, et al. Increased mortality rates with prolonged corticosteroid therapy when compared with antitumor necrosis factor-α-directed therapy for inflammatory bowel disease. Am J Gastroenterol. 2018;113:405–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hoarau G, Mukherjee PK, Gower-Rousseau C, et al. Bacteriome and mycobiome interactions underscore microbial dysbiosis in familial Crohn’s disease. mBio. 2016;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Zwolinska-Wcislo M, Brzozowski T, Budak A, et al. Effect of Candida colonization on human ulcerative colitis and the healing of inflammatory changes of the colon in the experimental model of colitis ulcerosa. J Physiol Pharmacol. 2009;60:107–118. [PubMed] [Google Scholar]
- 48. Kaplan GG, Szyszkowicz M, Fichna J, et al. Non-specific abdominal pain and air pollution: a novel association. PLoS One. 2012;7:e47669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lomer MC, Thompson RP, Powell JJ.. Fine and ultrafine particles of the diet: influence on the mucosal immune response and association with Crohn’s disease. Proc Nutr Soc. 2002;61:123–130. [DOI] [PubMed] [Google Scholar]
- 50. Marynowski M, Likońska A, Zatorski H, et al. Role of environmental pollution in irritable bowel syndrome. World J Gastroenterol. 2015;21:11371–11378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sobczak M, Fabisiak A, Murawska N, et al. Current overview of extrinsic and intrinsic factors in etiology and progression of inflammatory bowel diseases. Pharmacol Rep. 2014;66:766–775. [DOI] [PubMed] [Google Scholar]
- 52. Rehman K, Fatima F, Waheed I, et al. Prevalence of exposure of heavy metals and their impact on health consequences. J Cell Biochem. 2018;119:157–184. [DOI] [PubMed] [Google Scholar]
- 53. Zheng Z, Zhang H, Chen Z, et al. Hydrogeochemical and isotopic indicators of hydraulic fracturing flowback fluids in shallow groundwater and stream water, derived from dameigou shale gas extraction in the northern qaidam basin. Environ Sci Technol. 2017;51:5889–5898. [DOI] [PubMed] [Google Scholar]
- 54. Richard AM, Judson RS, Houck KA, et al. ToxCast chemical landscape: paving the road to 21st century toxicology. Chem Res Toxicol. 2016;29:1225–1251. [DOI] [PubMed] [Google Scholar]
- 55. Sheikh Sajjadieh MR, Kuznetsova LV, Bojenko VB.. Effect of cesium radioisotope on humoral immune status in Ukrainian children with clinical symptoms of irritable bowel syndrome related to chernobyl disaster. Toxicol Ind Health. 2011;27:51–56. [DOI] [PubMed] [Google Scholar]
- 56. Richard AM, Smith D, Shah I, et al. Editor’s highlight: analysis of the effects of cell stress and cytotoxicity on in vitro assay activity across a diverse chemical and assay space. Toxicol Sci. 2016;152:323–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Calkins BM. A meta-analysis of the role of smoking in inflammatory bowel disease. Dig Dis Sci. 1989;34:1841–1854. [DOI] [PubMed] [Google Scholar]
- 58. To N, Gracie DJ, Ford AC.. Systematic review with meta-analysis: the adverse effects of tobacco smoking on the natural history of Crohn’s disease. Aliment Pharmacol Ther. 2016;43:549–561. [DOI] [PubMed] [Google Scholar]
- 59. Cosnes J, Beaugerie L, Carbonnel F, et al. Smoking cessation and the course of Crohn’s disease: an intervention study. Gastroenterology. 2001;120:1093–1099. [DOI] [PubMed] [Google Scholar]
- 60. Yadav P, Ellinghaus D, Rémy G, et al. ; International IBD Genetics Consortium Genetic factors interact with tobacco smoke to modify risk for inflammatory bowel disease in humans and mice. Gastroenterology. 2017;153:550–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Marynowski M, Likońska A, Zatorski H, et al. Role of environmental pollution in irritable bowel syndrome. World J Gastroenterol. 2015;21:11371–11378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Rappaport SM. Implications of the exposome for exposure science. J Expo Sci Environ Epidemiol. 2011;21:5–9. [DOI] [PubMed] [Google Scholar]
- 63. Wild CP. Complementing the genome with an “exposome”: the outstanding challenge of environmental exposure measurement in molecular epidemiology. Cancer Epidemiol Biomarkers Prev. 2005;14:1847–1850. [DOI] [PubMed] [Google Scholar]
- 64. Niedzwiecki MM, Walker DI, Vermeulen R, et al. The exposome: molecules to populations. Annu Rev Pharmacol Toxicol. 2019;59:107–127. [DOI] [PubMed] [Google Scholar]
- 65. Miller GW. The Exposome. Waltham, MA: Elsevier; 2014. [Google Scholar]
- 66. Vrijheid M, Slama R, Robinson O, et al. The human early-life exposome (HELIX): project rationale and design. Environ Health Perspect. 2014;122:535–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Hales CN, Barker DJ.. Type 2 (non-insulin-dependent) diabetes mellitus: the thrifty phenotype hypothesis. Diabetologia. 1992;35:595–601. [DOI] [PubMed] [Google Scholar]
- 68. Ho SM, Cheong A, Adgent MA, et al. Environmental factors, epigenetics, and developmental origin of reproductive disorders. Reprod Toxicol. 2017;68:85–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Corella D, Ordovas JM.. Nutrigenomics in cardiovascular medicine. Circ Cardiovasc Genet. 2009;2:637–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Ordovas JM, Ferguson LR, Tai ES, et al. Personalised nutrition and health. BMJ (Clinical research ed). 2018;361:bmj.k2173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Price ND, Magis AT, Earls JC, et al. A wellness study of 108 individuals using personal, dense, dynamic data clouds. Nat Biotechnol. 2017;35:747–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Bischoff SC. Food allergy and eosinophilic gastroenteritis and colitis. Curr Opin Allergy Clin Immunol. 2010;10:238–245. [DOI] [PubMed] [Google Scholar]
- 73. Camilleri M, Katzka DA.. Irritable bowel syndrome: methods, mechanisms, and pathophysiology. Genetic epidemiology and pharmacogenetics in irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2012;302:G1075–G1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Turnbull JL, Adams HN, Gorard DA.. Review article: the diagnosis and management of food allergy and food intolerances. Aliment Pharmacol Ther. 2015;41:3–25. [DOI] [PubMed] [Google Scholar]
- 75. Miller GW. The Exposome: A Primer. Elsevier Science; 2013. [Google Scholar]
- 76. Örtqvist AK, Lundholm C, Halfvarson J, et al. Fetal and early life antibiotics exposure and very early onset inflammatory bowel disease: a population-based study. Gut. 2019;68:218–225. [DOI] [PubMed] [Google Scholar]
- 77. Gonzalez-Suarez B, Sengupta S, Moss AC.. Impact of inflammatory bowel disease activity and thiopurine therapy on birth weight: a meta-analysis. World J Gastroenterol. 2017;23:8082–8089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Myklebust-Hansen T, Aamodt G, Haugen M, et al. Dietary patterns in women with inflammatory bowel disease and risk of adverse pregnancy outcomes: results from the norwegian mother and child cohort study (moba). Inflamm Bowel Dis. 2017;24:12–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Ren S, Haynes E, Hall E, et al. Periconception exposure to air pollution and risk of congenital malformations. J Pediatr. 2018;193:76–84.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Benchimol EI, Bernstein CN, Bitton A, et al. Trends in epidemiology of pediatric inflammatory bowel disease in Canada: distributed network analysis of multiple population-based provincial health administrative databases. Am J Gastroenterol. 2017;112:1120–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Metz TO, Baker ES, Schymanski EL, et al. Integrating ion mobility spectrometry into mass spectrometry-based exposome measurements: what can it add and how far can it go?Bioanalysis. 2017;9:81–98. [DOI] [PMC free article] [PubMed] [Google Scholar]