Abstract
Objective:
To verify the effect of adjusting the challenge–skill balance with respect to rehabilitation process.
Design:
A single-blind, two-arm, parallel-group, randomized controlled trial.
Setting:
Recovery rehabilitation unit of Harue Hospital, Japan.
Subjects:
The trial included 72 clients (mean (SD): age, 74.64 (9.51) years; Functional Independence Measure score, 98.26 (15.27)) with cerebral or spinal disease or musculoskeletal disease.
Interventions:
Clients were randomly divided into two groups: the experimental group, who received occupational therapy with adjustment of the challenge–skill balance, and the control group who received conventional occupational therapy. Time from admission to discharge was considered the implementation period; the final evaluation was conducted at three months after discharge.
Main measures:
The primary outcome was subjective quality of life (Ikigai-9). Secondary outcomes were the health-related quality of life (EuroQol–5 Dimensions, Five Levels (EQ-5D-5L)), the Flow State Scale for Occupational Tasks, and the Functional Independence Measure. A cost-effectiveness analysis was conducted using total cost and quality-adjusted life-year based on the EQ-5D-5L.
Results:
Significant differences were observed between the experimental and control groups with respect to the Ikigai-9 score (P = 0.008) and EQ-5D-5L (P = 0.038), and the effect sizes were 0.76 (95% confidence interval [CI]: 0.27–1.24) and 0.62 (95% CI: 0.14–1.10), respectively. No significant between-group differences in other outcomes were observed, for example, the Functional Independence Measure score improved in both experimental and control groups (119.80 (5.50) and 118.84 (6.97), respectively. The incremental cost-effectiveness ratio was US$5518.38.
Conclusions:
Adjusting the challenge–skill balance may be a useful approach to improve the participant’s subjective quality of life in the rehabilitation process.
Keywords: Occupational therapy, rehabilitation interventions, randomized controlled trial, quality of life, psychological factors
Introduction
Client-centered practices aimed at enabling clients to participate in specific activities that are important to them are considered important elements in rehabilitation. Several benefits, such as increased motivation as well as the effectiveness of rehabilitation, have been reported using such practices.1,2 Its success is dependent on the ability of rehabilitation therapists to incorporate clients’ desires to the rehabilitation process. However, numerous rehabilitation therapists focus on their experiences and values or misunderstand the client’s desires, thereby tending to exclude clients from the decision-making process.2–4 Moreover, there exist unequal relationships between therapists and clients owing to differences in expertise regarding illness and disability.5 Reportedly, such relationships may result in the client experiencing negative emotions, such as a lack of self-esteem, and adversely affect the rehabilitation process.6,7
Rehabilitation therapists attempt to include the clients in goal-setting process using the Canadian Occupational Performance Measure8 and Goal Attainment Scaling;9 moreover, they evaluate comprehensive life functions using the International Classification of Functioning Disability and Health.10 However, there is often insufficient confirmation regarding the suitability of various approaches to achieve these goals for the client. A good goal is typically considered to be specific, measurable, achievable, realistic/relevant, and time bound (SMART);11 however, constantly verifying the suitability of the goals or approaches incrementally offered in response to changes in client’s ability is challenging.
Considering these problems, we designed a rehabilitation process that applies flow theory12 to share the various factors of rehabilitation process, including goal-setting, with clients as well as to promote tasks which help clients maintaining positive mental attitude. Flow (also termed “zone”) is defined as “a state in which people are so involved in an activity that nothing else seems to matter; the experience is so enjoyable that people will continue to do it even at great cost, for the sheer sake of doing it.”12 Previous studies have demonstrated that the flow state contributes to happiness, self-esteem, and quality of life.13–15 One of the factors leading to the flow state is the challenge–skill balance for an activity, and considering this, the relationship between flow state and other negative emotions is modeled as a flow model.12 In this model, flow is expected to occur when the challenge–skill balance for a activity is achieved. On the other hand, anxiety is experienced when the challenge exceeds the skill and boredom is experienced when the skill exceeds the challenge. Therefore, in our research, based on this flow model, we have designed an approach termed “adjusting the challenge–skill balance” to balance the challenges and skills in the rehabilitation process and verify its effect.
In our previous research, we conducted occupational therapy with adjusting the challenge–skill balance in older adults using an adult day program and examined the effects of this approach on the health-related quality of life.16 Because only one activity was targeted and the number of interventions was 10, the approach of adjusting the task was short-term and we were unable to verify multiple activities in the rehabilitation process. Therefore, we targeted clients undergoing recovery rehabilitation and decided to repeat the approach of adjusting the challenge–skill balance for multiple activities. Furthermore, we developed a process support tool using information terminals to ensure the consistency and continuity of the approach among the therapists. Based on a protocol designed via preliminary research,17,18 the present study aimed to examine the effect of adding the adjusting the challenge–skill balance to the rehabilitation process on the subjective quality of life as well as on the cost-effectiveness, if any, via a randomized controlled trial.
Methods
Design
The protocol has been published in a peer-reviewed journal.18 This study commenced in October 2017, and the follow-up evaluation was completed in October 2018. The study was conducted according to the standards of Declaration of Helsinki and was approved by the Ethics Review Commit-tee of the Tokyo Metropolitan University (No. 17020) and was registered in the trial registry (UMIN000029505). All clients provided written informed consent.
In this randomized controlled trial, we compared the approaches of adjusting the challenge–skill balance with occupational therapy (experimental group) and conventional occupational therapy (control group) based on the Consolidated Standards of Reporting Trials criteria.19 Outcomes were measured at admission to the recovery rehabilitation unit (“pre” assessment), at discharge (“post” assessment), and at three months after discharge (“follow-up” assessment). The primary outcome was change in subjective quality of life, and the secondary outcomes were changes in health-related quality of life, flow experience, and activities of daily living, as well as the cost-effectiveness.
Clients were recruited at the recovery rehabilitation unit of Harue Hospital, Fukui, Japan. Clients aged <50 years or >100 years on admission to the unit were excluded from the trial. This criterion is based on an age range set to ±2 standard deviations of 75.7 ± 12.3 years, which was the mean age of previously admitted clients. The clients were blinded to the assignment; however, the principal investigator, intervention therapists, and evaluators were not blinded. Because the procedures performed in the experimental group were considered feasible in any rehabilitation processes regardless of the disease, we included patients with cerebral or spinal disease and musculoskeletal diseases, which are the main target diseases of the recovery rehabilitation unit. Moreover, the present study requires communication and comprehension skills to implement client-centered rehabilitation processes in both groups, and the outcomes adopted the client’s self-reported questionnaire. Therefore, we excluded clients with mini mental state exam scores below cut-off point (23 points)20 to secure research credibility. Furthermore, the trial was canceled for the clients who were transferred to another unit or another hospital or died during the research period. Clients were included in this analysis even when meeting the cancelation criteria, because the intention to treat principle was applied to guarantee the comparability of randomized groups.
Randomization
Clients were randomly assigned to the experimental or control group using block randomization. The block size was 4 to reduce the predictability and equalize the two groups. To homogenize the initial data, randomization was performed after division based on the disease group (cerebral or spinal disease or musculoskeletal disease) and the Visual Analog Scale on health included in EuroQol–5 Dimensions (EQ-5D) (EQ-VAS score; high or low based on 50 as the cut-off value).21 In the present study, we focused on the client’s subjective evaluation of outcomes; therefore, we adopted EQ-VAS to homogenize the degree of subjective evaluation of health in the two groups. Thus, stratification was as follows: (1) cerebral or spinal disease and high EQ-VAS; (2) cerebral or spinal disease and low EQ-VAS; (3) musculoskeletal disease and high EQ-VAS; and (4) musculoskeletal disease and low EQ-VAS. Thereafter, clients were randomly allocated using computer software (R. Ver. 3.2.1).
The person allocating the clients was notified regarding the allocation group via email from a central randomization center. Although the statisticians created block random patterns for each of the four layers, information about the group was masked. The chief researcher informed the six occupational therapists responsible for the client regarding treatment assignment but did not inform the client. In the experimental group, a dedicated mobile tablet application was used to support the approach of adjusting the challenge–skill balance but not used in the control group. The possibility of contamination was limited between the groups. The person collecting the outcome data was acquainted with client allocation.
Procedures
Occupational therapy was conducted according to the American Occupational Therapy Association guidelines22 by occupational therapists with experience of client-centered practice (at least 200 work hours). The therapists were trained in the approach of adjusting the challenge–skill balance (at least 50 h). Both groups followed the guidelines and conducted comprehensive assessments and interventions for domains such as occupations (e.g. activities of daily living and instrumental activities of daily living), client factors (e.g. body functions and value), performance skills (e.g. motor and process skills), performance patterns (e.g. habits and routines), and situations and environment (e.g. behavioral standards, educational and residential status, as well as caregivers). The main difference between the two groups was in whether the clients and the therapists quantified and shared the perceptions of task using a common scale, challenge and skill level. Treatments in each group comprised sessions lasting 40–60 min, conducted six times per week. The time from pre- to post-assessment was considered the implementation period. During the follow-up period, each client was instructed to deduce the assigned group in response to the questionnaire prepared for the present study (e.g. Did you know the type of rehabilitation that was provided?). The procedures in the experimental and control groups are summarized in the following sections.
Experimental group
The experimental group was subjected to the approach of adjusting the challenge–skill balance using a dedicated custom application program. In the first session, therapists used the Canadian Occupational Performance Measure8 to evaluate client’s issues with several activities of daily living. In the second session, clients were instructed to perform tasks related to the selected activities, which reflects the assessment by the therapist. In the third session, clients evaluated their activities based on challenge and skill level. Challenge level was defined as the client’s perception of the activity’s difficulty and was evaluated on a seven-point scale from “extremely simple” (1) to “extremely difficult” (7). “Skill level” was defined as the client’s perception of the required skill associated with the activity and was evaluated from “not at all” (1) to “extremely skilled” (7).13,23 Moreover, the clients were instructed to justify their scores by the therapists.
Based on the evaluations by the client and therapist, the factors contributing to difficulties with task performance (“challenge components”; e.g. environmental or physical factors, such as range of movement, time requirement, pain, and fatigue) and improving task performance (“skill components”; e.g. frequency, range, distance, accuracy, and dexterity) were determined. Compensation approaches, such as environmental adjustment or the use of technical aids, were permitted in the experimental group to adjust the challenge level.
Depending on the challenge–skill balance, the therapist judged the necessity to re-adjust the activity. The criterion for this adjustment was a difference of ⩽1 between the challenge and skill levels evaluated by the therapist and client. When the client’s levels were balanced, intervention could be initiated. If there was an imbalance, the activity was re-adjusted until the challenge and skill levels of the activity evaluated by the client meet the above criteria. The challenge and skill components were considered throughout the assessment process. After the client performed the adjusted activity, the client-reported challenge and skill levels were re-evaluated. The evaluation and adjustment processes were repeated at least once a week until the challenge and skill levels were balanced for several activities.
Control group
The first and second sessions were performed similar to those of the experimental group. The control group did not undergo the subjective evaluation of the challenge and skill levels by the client. Therefore, following the third session, the therapist assessed the client and provided therapy based on the general guidelines for occupational therapy practice.22
Outcomes
The primary outcome was the subjective quality of life measured using the Ikigai-9 score.24 The secondary outcomes were measured using the health-related quality of life (EQ-5D-5L),21 the Flow State Scale for Occupational Tasks,25 and the Functional Independence Measure.26 The Ikigai-9 and EQ-5D-5L were measured at the pre-, post-, and follow-up assessments, but the Flow State Scale for Occupational Tasks and the Functional Independence Measure were only measured at the pre- and post-assessments. During the follow-up period, we sent self-evaluation form on outcomes (Ikigai-9 and EQ-5D-5L) to the client’s residence and requested a response.
The Ikigai-9 is a self-filled questionnaire measuring the mental state “reason for living; Ikigai.” Ikigai-9 involves the following three factors: (1) optimistic and positive feelings for life; (2) positive and active attitude toward the future; and (3) recognition of the meaning of self-existence. These three factors were evaluated using three questions each (nine questions in total) and scored using a 5-point Likert-type scale from “strongly disagree” (1 point) to “strongly agree” (5 points), with a total score of 9–45 points (Table 1). The Cronbach’s alpha of Ikigai-9 was 0.87.24
Table 1.
Items of Ikigai-9.
| 1 | I often feel that I am happy |
| 2 | I want to learn something new or start |
| 3 | I think that I am useful for something else or society |
| 4 | I am relaxed mentally |
| 5 | I am interested in various things |
| 6 | I think that my existence is necessary for something or someone else |
| 7 | My life is abundant and fulfilling |
| 8 | I want to extend my possibilities |
| 9 | I think that I am influencing someone |
Author translated the items with the permission of the developer.
Ikigai-9 comprises nine items (three factors). The three factors are as follows: optimistic and positive feelings for life (1, 4, and 7), positive and active attitude toward the future (2, 5, and 8), and recognition of the meaning of self-existence (3, 6, and 9).
The EQ-5D-5L defines health conditions based on five dimensions (e.g. mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) and provides a utility index, which can be used in cost-effectiveness analyses.27 Moreover, we used the EQ-VAS for the self-assessment of health condition from “worst” (0) to “best” (100). Test–retest reliability for EQ-5D-5L was r = 0.90 and that for EQ-VAS was r = 0.86.21
Flow experience was evaluated using the Flow State Scale for Occupational Tasks, which was developed as a measure based on factors that are considered to be components of the flow. It comprises three factors that indicate the “sense of control of the task” (six items), “experience of positive emotion” (four items), and “experience of absorption by concentrating on a task” (four items). The items were measured in a 7-point scale ranging from “strong disagreement” (1) to “strong agreement” (7), with a total score ranging from 14 to 98 points. The high score is considered to indicate the strong flow state in performing a specific task. The Cronbach’s alpha was 0.92.25 The activities of daily living were measured using the Functional Independence Measure, evaluating 18 items on motor and cognitive subscales in seven grades. The total score ranges from 18, indicating the need for full assistance, to 126, indicating full independence. Intraclass correlation coefficient was 0.96.26
Sample size
An a priori power analysis was conducted (G*power, version 3.1.7) based on the effect size of 0.76 for EQ-5D-5L16 and 0.78 for Ikigai-917 in previous research. A sample size of 68 was required to achieve an effect size of 0.7 in the quality of life score, an alpha level of 0.05 (two-sided), and an 80% power to detect the difference.
Statistical analysis
All data were entered into Microsoft Excel 2016 before being exported to IBM SPSS version 24 or R version 3.4.1 for analysis by statisticians who were unaware of group allocation. SPSS was primarily used for outcome analysis and R was used to calculate cost-effectiveness. The baseline characteristics of the groups were analyzed using effect sizes. Moreover, the activities supported by both groups were categorized and compared.
The primary and secondary outcomes were analyzed using a linear mixed model for repeated measures with a maximum likelihood estimate. In this model, group (experimental or control), time (pre-, post-, or follow-up assessment), and the group and time interaction were considered as fixed effects and clients were considered as random effects. Time was considered as a repeated measure. A P-value of <0.05 using type III fixed effects was considered significant. This was reported to be an appropriate statistical method for a longitudinal trial with missing data.28 The magnitude of the between-group effect was determined as the effect size based on Hedges’ g for each outcome,29 calculated by dividing the difference between the means of each group by the pooled standard deviation. According to the standardized criteria from previous studies on effect sizes, 0.2 can be considered as small, 0.5 as medium, and 0.8 as large.29
A cost-effectiveness analysis was conducted using total cost and quality-adjusted life-year based on the utility value of the EQ-5D-5L.27 The incremental cost-effectiveness ratio was calculated based on a comparison of the study groups from discharge to the follow-up assessment. The financial data were calculated according to the rehabilitation cost registered in the electronic medical record. The total cost was converted to US dollars using the average exchange rate at the time of data analysis. The incremental cost-effectiveness ratio was calculated as [CoE − CoC]/[EfE − EfC], where Co is the mean cost, Ef is the mean quality-adjusted life-year, E is the experimental group, and C is the control group. To consider the uncertainty of the incremental cost-effectiveness ratio, the mean was calculated using the bootstrap method (1000 times), which resamples from the observed data and experimentally forms its distribution using these statistics.30
Results
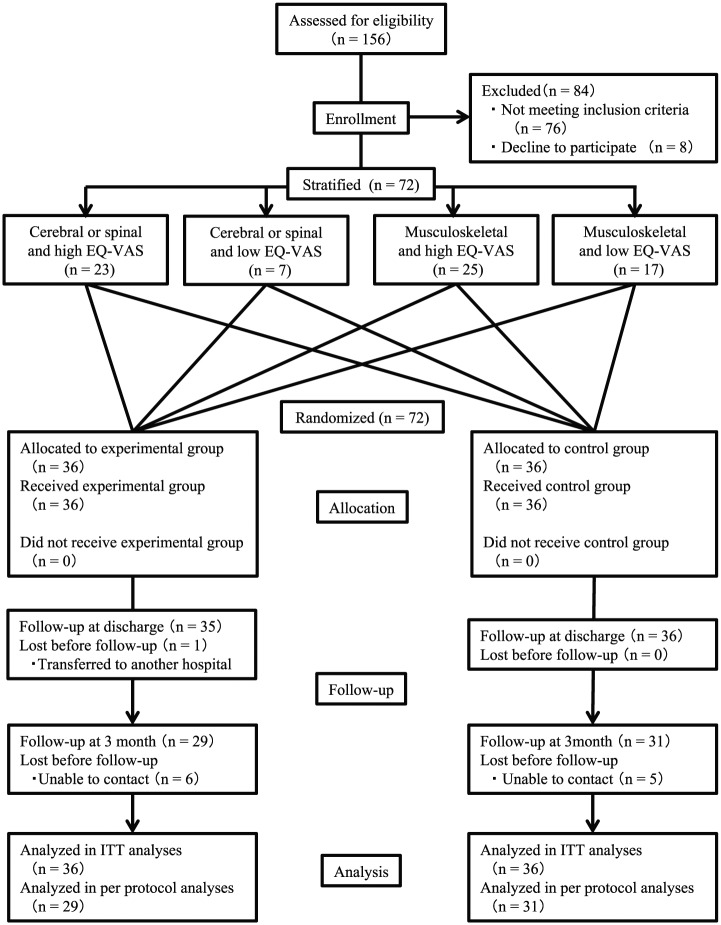
We targeted 72 clients for random assignment (Figure 1). Among them, 60 individuals were able to participate thorough the entire study period up to the follow-up assessment. The characteristics of the clients in the two groups matched satisfactorily at the initial evaluation (Table 2). The occupational therapy provided in the present study was 44.3 ± 36.0 sessions in the experimental group and 43.6 ± 28.2 sessions in the control group (40 min was considered as one session). Targeted activities were comparable between the two groups (Table 3).
Figure 1.
Flow chart of participant allocation.
ITT, intention to treat; High EQ-VAS, EuroQol–5 Dimensions Visual Analog Scale ≧ 50; Low EQ-VAS, EuroQol–5 Dimensions Visual Analog Scale < 50.
Table 2.
Characteristics of the clients at the initial evaluation (n = 72).
| Experimental group |
Control group |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cerebral or spinal and high EQ-VAS (n = 11) | Cerebral or spinal and low EQ-VAS (n = 3) | Musculoskeletal and high EQ-VAS (n = 13) | Musculoskeletal and low EQ-VAS (n = 9) | Total (n = 36) | Cerebral or spinal and high EQ-VAS (n = 12) | Cerebral or spinal and low EQ-VAS (n = 4) | Musculoskeletal and high EQ-VAS (n = 12) | Musculoskeletal and low EQ-VAS (n = 8) | Total (n = 36) | Effect size | |
| Age, mean (SD) | 67.00 (6.43) | 71.67 (4.58) | 71.67 (4.58) | 78.89 (7.67) | 74.11 (9.11) | 72.75 (11.73) | 68.75 (7.63) | 76.50 (9.28) | 79.88 (7.59) | 75.17 (9.99) | g = 0.11 |
| Sex, n | |||||||||||
| Male | 5 | 1 | 3 | 3 | 12 | 8 | 3 | 2 | 2 | 15 | |
| Female | 6 | 2 | 10 | 6 | 24 | 4 | 1 | 10 | 6 | 21 | V = 0.09 |
| Disease, n | |||||||||||
| Cerebral infarction | 7 | 2 | – | – | 9 | 9 | 3 | – | – | 12 | |
| Cerebral hemorrhage | 2 | – | – | – | 2 | 2 | 1 | – | – | 3 | V = 0.06 |
| Subarachnoid hemorrhage | 1 | – | – | – | 1 | 1 | – | – | – | 1 | |
| Spinal cord injury | 1 | 1 | – | – | 2 | – | – | – | – | – | |
| Femoral neck fracture | – | – | 3 | 2 | 5 | – | – | 1 | – | 1 | |
| Intertrochanteric femoral fracture | – | – | 2 | 3 | 5 | – | – | 3 | 2 | 5 | |
| Lumbar compression fracture | – | – | 2 | 3 | 5 | – | – | 1 | 2 | 3 | |
| Pelvic fracture | – | – | – | 1 | 1 | – | – | 2 | 2 | 4 | |
| Lumbar spinal canal stenosis | – | – | – | – | 5 | – | – | – | 1 | 1 | |
| Knee osteoarthritis | – | – | 5 | – | – | – | – | 5 | – | 5 | |
| Hip osteoarthritis | – | – | – | – | – | – | – | – | 1 | 1 | |
| Above knee amputation | – | – | 1 | – | 1 | – | – | – | – | – | |
| Cerebral or spinal and high EQ-VAS (n = 11) | Cerebral or spinal and low EQ-VAS (n = 3) | Musculoskeletal and high EQ-VAS (n = 13) | Musculoskeletal and low EQ-VAS (n = 9) | Total (n = 36) | Cerebral or spinal and high EQ-VAS (n = 12) | Cerebral or spinal and low EQ-VAS (n = 4) | Musculoskeletal and high EQ-VAS (n = 12) | Musculoskeletal and low EQ-VAS (n = 8) | Total (n = 36) | Effect size | |
| Length of stay (day), mean (SD) | 47.82 (30.92) | 87.00 (39.36) | 43.2 (33.70) | 38.67 (26.22) | 49.47 (33.05) | 42.25 (27.54) | 72.75 (39.00) | 36.92 (20.44) | 56.63 (26.61) | 49.53 (27.99) | g = 0.00 |
| Treatment period (day), mean (SD) | 45.33 (31.41) | 84.86 (38.04) | 41.68 (33.24) | 36.59 (27.08) | 47.14 (32.69) | 40.96 (26.73) | 69.98 (38.48) | 34.61 (21.03) | 54.09 (25.67) | 47.06 (27.95) | g = 0.00 |
| MMSE, mean (SD) | 26.73 (2.61) | 29.33 (1.15) | 27.92 (2.36) | 26.56 (2.74) | 27.33 (2.53) | 28.25 (1.71) | 25.25 (1.89) | 27.50 (2.58) | 27.25 (2.38) | 27.36 (2.46) | g = 0.01 |
| EQ-VAS, mean (SD) | 75.64 (11.42) | 30.00 (10.00) | 68.08 (17.14) | 33.89 (11.67) | 58.67 (22.95) | 78.08 (9.07) | 46.25 (11.09) | 72.92 (18.02) | 39.38 (10.16) | 65.33 (20.72) | g = 0.30 |
| Flow state scale for occupational task, mean (SD) | 79.36 (12.73) | 79.33 (6.43) | 80.31 (9.31) | 78.78 (13.21) | 79.56 (10.90) | 75.67 (12.29) | 50.5 (15.93) | 82.5 (12.81) | 77.13 (11.19) | 75.47 (15.32) | g = 0.31 |
| Ikigai-9, mean (SD) | 29.45 (7.35) | 20.33 (4.73) | 29.92 (4.25) | 26.00 (8.44) | 28.00 (6.88) | 26.41 (9.20) | 25.00 (6.37) | 32.33 (6.54) | 30.63 (12.26) | 29.17 (9.06) | g = 0.15 |
| Functional Independence Measure, mean (SD) | |||||||||||
| Motor | 69.18 (13.63) | 58.67 (25.42) | 62.69 (13.93) | 63.22 (12.57) | 64.47 (14.29) | 72.41 (11.22) | 57.00 (23.85) | 67.92 (10.30) | 55.88 (15.96) | 65.53 (14.85) | g = 0.07 |
| Cognitive | 31.27 (3.17) | 34.67 (0.58) | 33.23 (2.83) | 34.00 (1.41) | 32.97 (2.76) | 33.67 (2.02) | 29.00 (4.69) | 34.83 (0.58) | 33.75 (1.83) | 33.56 (2.62) | g = 0.22 |
| Total | 100.45 (14.45) | 93.67 (25.42) | 95.92 (16.07) | 97.22 (12.92) | 97.44 (15.11) | 106.08 (10.40) | 86.00 (25.65) | 102.75 (10.38) | 89.63 (17.00) | 99.08 (15.60) | g = 0.11 |
EQ-VAS, EuroQol–5 Dimensions visual analog scale; High EQ-VAS, EuroQol–5 Dimensions visual analog scale ≧ 50; Low EQ-VAS, EuroQol–5 Dimensions visual analog scale < 50; MMSE, Mini Mental State Examination; effect size g, Hedges’ g; effect size V, Cramer’s V. Effect size of disease calculated Cramer’s V which is a measure of association between two nominal variables (disease: cerebral or spinal disease and musculoskeletal disease, group: experiment and control group).
Table 3.
Activities targeted by the experimental and control groups.
| Activity | Experimental group (n = 36) | Control group (n = 36) | Effect size |
|---|---|---|---|
| Upper limb function | 7 | 7 | V = 0.21 |
| Basic movement | 7 | 8 | |
| Eating | 3 | 0 | |
| Dressing | 7 | 8 | |
| Toilet | 2 | 5 | |
| Bathing | 15 | 21 | |
| Walking | 29 | 27 | |
| Climbing up and down stairs | 12 | 14 | |
| Cleaning up the room | 7 | 9 | |
| Washing clothes | 9 | 7 | |
| Communication | 1 | 2 | |
| Cooking | 10 | 7 | |
| Shopping | 4 | 1 | |
| Driving | 5 | 7 | |
| Hobby | 7 | 7 | |
| Work | 2 | 0 | |
| Total | 127 | 130 |
Effect size calculated Cramer’s V for the association between activity and group.
Overall, 36 clients were assigned to both the experimental and control groups. Both groups were divided based on the disease group (cerebral or spinal disease or musculoskeletal disease) and the Visual Analog Scale on health included in EQ-5D (stratification), and random allocation was performed to achieve homogenization. No significant effect was observed at each initial value.
The activity was selected by the client and the therapist using the Canadian Occupational Performance Measure. The table shows the total number of activities selected. The total number of activities selected in the two groups was similar.
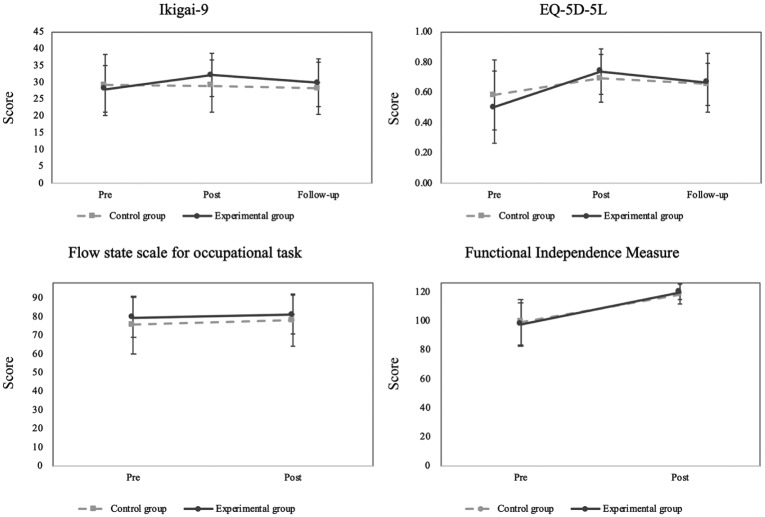
The pre-, post-, and follow-up assessment scores as well as the change scores of each outcome are shown in Table 4. The results of the linear mixed model are shown in Table 5 and Figure 2. As shown, a significant difference was observed between the two groups in the Ikigai-9 score. Regarding the secondary outcomes, there was a significant difference between the two groups in the EQ-5D-5L but not for either the Flow State Scale for Occupational Tasks or the Functional Independence Measure. Furthermore, it appears that for the Ikigai-9 and EQ-5D-5L, the experimental group reported higher scores during the post-assessment period but these decreased during the follow-up period. The effect sizes based on the changes in the pre–post-assessment results were 0.76 (95% confidence interval [CI]: 0.27–1.24), 0.62 (95% CI: 0.14–1.10), −0.09 (95% CI: −0.56 to 0.37), and 0.25 (95% CI: −0.21 to 0.72) for the Ikigai-9, EQ-5D-5L, Flow State Scale for Occupational Tasks, and the Functional Independence Measure, respectively.
Table 4.
The pre-, post-, and follow-up assessment scores and the changes in the scores of Ikigai-9, EQ-5D-5L, Flow State Scale for Occupational Task, and Functional Independence Measure.
| Outcome | Experimental group |
Control group |
Effect size between groups |
||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | Hedge’s g | Lower | Upper | |
| Ikigia-9 | |||||||||
| Pre | 36 | 28.00 | 6.88 | 36 | 29.17 | 9.06 | |||
| Post | 35 | 32.14 | 6.31 | 36 | 28.89 | 7.85 | |||
| Follow-up | 29 | 29.83 | 7.10 | 31 | 28.10 | 7.75 | |||
| Change score (pre-post) | 35 | 4.06 | 6.58 | 36 | –0.28 | 4.63 | 0.76 | 0.27 | 1.24 |
| Change score (pre-follow) | 29 | 1.97 | 6.84 | 31 | –1.61 | 6.55 | 0.53 | 0.01 | 1.04 |
| EQ-5D-5L | |||||||||
| Pre | 36 | 0.50 | 0.24 | 36 | 0.58 | 0.23 | |||
| Post | 35 | 0.74 | 0.15 | 36 | 0.69 | 0.16 | |||
| Follow-up | 28 | 0.66 | 0.20 | 29 | 0.65 | 0.14 | |||
| Change score (pre-post) | 35 | 0.24 | 0.23 | 36 | 0.11 | 0.20 | 0.62 | 0.14 | 1.10 |
| Change score (pre-follow) | 28 | 0.16 | 0.26 | 29 | 0.10 | 0.22 | 0.28 | –0.25 | 0.80 |
| Flow State Scale for Occupational Task | |||||||||
| Pre | 36 | 79.56 | 10.90 | 36 | 75.47 | 15.32 | |||
| Post | 35 | 81.09 | 10.54 | 36 | 78.11 | 14.15 | |||
| Change score | 35 | 1.66 | 10.15 | 36 | 2.64 | 10.33 | –0.09 | –0.56 | 0.37 |
| Functional Independence Measure | |||||||||
| Pre | 36 | 97.44 | 15.11 | 36 | 99.08 | 15.60 | |||
| Post | 35 | 119.80 | 5.50 | 36 | 118.14 | 6.97 | |||
| Change score | 35 | 22.57 | 13.67 | 36 | 19.06 | 13.75 | 0.25 | –0.21 | 0.72 |
Pre = at admission to the recovery rehabilitation unit; Post = at discharge; Follow = at 3 months after discharge; EQ-5D-5L = EuroQol–5 Dimensions, Five Levels.
Table 5.
Linear mixed model with repeated measures comparing the two groups on the Ikigai-9, EQ-5D-5L, Flow State Scale for Occupational Task, and Functional Independence Measure (n = 72).
| Comparison: analysis type | Change over time |
Group×Time interaction |
||
|---|---|---|---|---|
| F(df) | p | F(df) | P | |
| Entire period | ||||
| Ikigai-9 | 4.208 | 0.017 | 4.997 | 0.008 |
| EQ-5D-5L | 24.632 | < 0.001 | 3.342 | 0.038 |
| Flow State Scale for Occupational Task | 3.078 | 0.084 | 0.177 | 0.675 |
| Functional Independence Measure | 163.632 | < 0.001 | 1.08 | 0.302 |
| Pre-post | ||||
| Ikigai-9 | 8.004 | 0.006 | 10.513 | 0.002 |
| EQ-5D-5L | 48.137 | < 0.001 | 6.686 | 0.012 |
| Flow State Scale for Occupational Task | 3.078 | 0.084 | 0.177 | 0.675 |
| Functional Independence Measure | 163.632 | < 0.001 | 1.08 | 0.302 |
| Pre-follow | ||||
| Ikigai-9 | 0.087 | 0.769 | 3.816 | 0.055 |
| EQ-5D-5L | 15.475 | < 0.001 | 1.858 | 0.178 |
| Flow State Scale for Occupational Task | – | – | – | – |
| Functional Independence Measure | – | – | – | – |
| Post-follow | ||||
| Ikigai-9 | 5.478 | 0.023 | 0.763 | 0.386 |
| EQ-5D-5L | 5.565 | 0.021 | 0.696 | 0.407 |
| Flow State Scale for Occupational Task | – | – | – | – |
| Functional Independence Measure | – | – | – | – |
Pre = at admission to the recovery rehabilitation unit; Post = at discharge; Follow = at 3 months after discharge; EQ-5D-5L = EuroQol–5 Dimensions; Change Over Time = difference in scores before and after intervention; Group×Time interaction = difference between the groups in change score before and after intervention.
Figure 2.
Transition of each outcome measures in the experimental and control groups.
Pre = at admission to the recovery rehabilitation unit; Post = at discharge; Follow-up = at 3 months after discharge.
Ikigai-9 and EQ-5D-5L improved during the post-assessment period in the experimental group, but tended to return to the pre-assessment values during the follow-up period. Flow State Scale for Occupational Task and Functional Independence Measure showed similar improvement tendency in the pre–post-assessment values in the two groups.
Among the two groups, the effect size of changed scores (pre–post-assessment) for Ikigai-9 and EQ-5D-5L was moderate, whereas the effect size of Flow State Scale for Occupational Task and Functional Independence Measure was smaller.
As a result of comparing the two groups using linear mixed model analysis, significant differences were found between Ikigai-9 and EQ-5D-5L during the entire period as well as in the pre–post-assessment.
Despite blinding, nine clients (31.0%) in the experimental group and seven (22.6%) in the control group (overall 16 (26.7%)) were aware of their assignment, whereas the remaining clients reported successful blinding.
Regarding the cost-effectiveness analysis, quality-adjusted life-year was calculated based on the EQ-5D-5L data using a US dollar to yen exchange rate of $1 to 111.10 yen. The cost of treatment in the experimental group was $1710.86, whereas that in the control group was $1659.46. This produced quality-adjusted life-year of 0.173 and 0.164 in the experimental and control groups, respectively. The incremental cost-effectiveness ratio, based on the bootstrap method, was $5518.38 per quality-adjusted life-year.
Discussion
In the present study, we examined the effect of using the approach of adjusting the challenge–skill balance in the rehabilitation process and observed that the subjective quality of life (primary outcome (Ikigai-9 score)) and health-related quality of life (secondary outcome (EQ-5D-5L)) improved between admission to discharge, and the effect size of each outcome was moderate. However, there were no significant differences in the groups with respect to changes in flow experience and independence in the activities of daily living. Furthermore, the incremental cost-to-effectiveness ratio of the approach of adjusting the challenge–skill balance, which was calculated using quality-adjusted life-year based on the utility index of EQ-5D-5L, was $5518.38 compared with the standard occupational therapy, indicating that rehabilitation using adjusting the challenge–skill balance was a more cost-effective method than the conventional rehabilitation (occupational therapy).
In the present study, adjusting the challenge–skill balance was designed to share the rehabilitation process with clients and to promote tasks suitable which help clients maintaining positive mental attitude and to confirm the effect of this approach, the subjective quality of life (evaluated using the Ikigai-9 score) was adopted as the primary outcome. Several clients participating in rehabilitation programs have multifactorial and complex issues.31 There exists a concern that if the activity is supported without sufficient reason for the complexity, the activity may be matched to anxiety or boredom in the flow model.12 By adjusting the challenge–skill balance to the activity of the client, the occurrence of negative emotions, such as anxiety and boredom, was suppressed. It has been speculated that this occurrence was relatively involved in enhancing the subjective quality of life (Ikigai-9). In other words, we believe that adjusting the challenge–skill balance contributes to focusing on the task itself and avoiding distraction by the task unrelated thoughts (mind-wandering).32 Although this remains hypothetical, considering the report that mind-wandering is reduced by the state of mindfulness,33 the addition of adjusting the challenge–skill balance in rehabilitation may have led to a state similar to mindfulness. We intend to investigate the relationship between adjusting the challenge–skill balance and mind-warming or mindfulness in the future.
Repeating the approach of adjusting the challenge–skill balance also helps to identify the task which should be set according to the changing skill by the therapy while focusing on achievable goals at that time. The features of this approach are similar to the small-step method.34 Rehabilitation often requires the achievement of its goals within a limited period in current healthcare systems;35 therefore, in cases where the clients’ abilities and life goals are greatly diverse, there exists a concern that this approach cannot achieve the goal. The present study demonstrated no significant difference between the groups with regard to the hospitalization period as well as the improvement of the Functional Independence Measure, whereas the EQ-5D-5L tended to improve in the experimental group, thereby suggesting that rehabilitation using adjusting the challenge–skill balance, which is similar to small steps, increases health-related quality of life without any adverse effects on the activities of daily living performance as well as on the hospitalization period.
Interestingly, there was no difference between the groups with regard to the flow state based on the Flow State Scale for Occupational Tasks, despite the fact that routinely involving the clients in self-assessment could have increased their engagement in the therapeutic process. A possible explanation is that a state of deep flow36 was not achieved, because we aimed to only adjust the challenge–skill balance. Although the approach of adjusting the challenge–skill balance is based on flow model, the wider benefits of this approach may have essentially been obtained from other factors, such as reduction in mind-wandering and employing small-step method.
It appears that for the Ikigai-9 and EQ-5D-5L, the experimental group reported higher scores during the post-assessment period but these returned to almost pre-assessment values at the follow-up assessment. Although the approach of adjusting the balance between the client’s challenge and skill was repeated during hospitalization, it appeared to be difficult for the client to continue the approach on their own at home. Therefore, even if the approach of adjusting the challenge–skill balance is implemented once, the sustained effect in the home life environment without assistance for this approach remains unverified. In the future, it will be beneficial to verify the effectiveness of this approach in the client’s home life environment and establish a system that enables the continuation of this approach of adjusting the challenge–skill balance toward follow-up of home life after discharge.
The present study has several limitations. First, the study was performed at a single facility, which might increase the treatment effect compared with that observed with multicenter randomized controlled trial designs. Second, because the therapists were trained for administering the approach of adjusting the challenge–skill balance, it may have biased the intervention in the two groups. In addition, although the therapists were not blinded and the clients were single-blinded, only 73.3% of the clients were successfully blinded. Despite the potential for bias, we believe that the non-blinded clients (23.7%) did not have a strong impact on the results. Third, the extent to which the approach of adjusting the challenge–skill balance was able to obtain the effects described by the flow model and lead to the flow experience in this study remains unclear. Moreover, we have previously conducted a study at an adult day program, but the present study was only conducted in a recovery rehabilitation unit. Therefore, the effects have not been verified in acute, subacute, outpatient, or home visits as well as in follow-up at home life environment, as described above. These issues should be considered in future research.
In conclusion, we suggested that using the approach of adjusting the challenge–skill balance in rehabilitation improves the subjective quality of life of the client.
Clinical messages.
Using adjusting the challenge–skill balance in the rehabilitation process may improve the client’s subjective quality of life.
Adjusting the challenge–skill balance may be a useful and cost-effective approach for clients in the recovery rehabilitation unit when compared with conventional occupational therapy.
Acknowledgments
We appreciate all the people who cooperated in this research.
Footnotes
Author contributions: I.Y. designed and performed the research. I.Y. and K.H. analyzed data. I.Y. drafted the manuscript. K.H. and R.K. reviewed and modified the manuscript. All authors have read and approved the final manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Japanese Association of Occupational Therapists (Grant Number 2017-04).
ORCID iDs: Ippei Yoshida  https://orcid.org/0000-0003-1888-154X
https://orcid.org/0000-0003-1888-154X
Kazuki Hirao  https://orcid.org/0000-0002-2467-7564
https://orcid.org/0000-0002-2467-7564
References
- 1. Palmadottir G. Client perspectives on occupational therapy in rehabilitation services. Scand J Occup Ther 2003; 10(4): 157–166. [Google Scholar]
- 2. Siegert RJ, McPherson KM, Taylor WJ. Toward a cognitive-affective model of goal-setting in rehabilitation: is self-regulation theory a key step. Disabil Rehabil 2004; 26(20): 1175–1183. [DOI] [PubMed] [Google Scholar]
- 3. Cott CA. Client-centred rehabilitation: client perspectives. Disabil Rehabil 2004; 26(24): 1411–1422. [DOI] [PubMed] [Google Scholar]
- 4. Maitra KK, Erway F. Perception of client-centered practice in occupational therapists and their client. Am J Occup Ther 2006; 60(3): 298–310. [DOI] [PubMed] [Google Scholar]
- 5. Bellner AL. Senses of responsibility: a challenge for occupational and physical therapists in the context of ongoing professionalization. Scand J Caring Sci 1999; 13(1): 55–62. [DOI] [PubMed] [Google Scholar]
- 6. Halstead LS. The power of compassion and caring in rehabilitation healing. Arch Phys Med Rehabil 2001; 82(2): 149–154. [DOI] [PubMed] [Google Scholar]
- 7. Palmadottir G. Client-therapist relationships: experiences of occupational therapy clients in rehabilitation. Br J Occup Ther 2006; 69(9): 394–401. [Google Scholar]
- 8. Boniface G, Fedden T, Hurst H, et al. Using theory to underpin an integrated occupational therapy service through the Canadian model of occupational performance. Br J Occup Ther 2008; 71(12): 531–539. [Google Scholar]
- 9. Wade DT. Goal planning in stroke rehabilitation: evidence. Top Stroke Rehabil 1999; 6(2): 37–42. [Google Scholar]
- 10. World Health Organization. International classification of functioning, disability and health: ICF. Geneva: World Health Organization, 2001. [Google Scholar]
- 11. Schut HA, Stam HJ. Goals in rehabilitation teamwork. Disabil Rehabil 1994; 16(4): 223–226. [DOI] [PubMed] [Google Scholar]
- 12. Csikszentmihalyi M. Flow, the psychology of optimal experience, steps towards enhancing the quality of life. New York: Harper & Row, 1991. [Google Scholar]
- 13. Nielsen K, Cleal B. Predicting flow at work: investigating the activities and job characteristics that predict flow states at work. J Occup Health Psychol 2010; 15(2): 180–190. [DOI] [PubMed] [Google Scholar]
- 14. Engeser S, Rheinberg F. Flow, performance and moderators of challenge-skill balance. Motiv Emot 2008; 32(3): 158–172. [Google Scholar]
- 15. Hirao K, Kobayashi R, Okishima K, et al. Flow experience and health-related quality of life in community dwelling elderly Japanese. Nurs Health Sci 2012; 14(1): 52–57. [DOI] [PubMed] [Google Scholar]
- 16. Yoshida I, Hirao K, Nonaka T. Adjusting challenge-skill balance to improve quality of life in older adults: a randomized controlled trial. Am J Occup Ther 2018; 72(1): 7201205030p1–7201205030p8. [DOI] [PubMed] [Google Scholar]
- 17. Yoshida I, Hirao K, Kobayashi R. Effect of adjusting the challenge-skill balance for occupational therapy in a recovery rehabilitation unit: a pilot study. Asian J Occup Ther 2018; 15(1): 11–18. [Google Scholar]
- 18. Yoshida I, Hirao K, Kobayashi R. Study protocol: adjusting the challenge-skill balance for occupational therapy in a recovery rehabilitation unit: a proposal for a randomized controlled trial. BMJ Open 2018; 8(12): e022438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Med 2010; 8(1): 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Anthony JC, LeResche L, Niaz U, et al. Limits of the mini-mental state as a screening test for dementia and delirium among hospital patients. Psychol Med 1982; 12(2): 397–408. [DOI] [PubMed] [Google Scholar]
- 21. EuroQol Group. EuroQol-a new facility for the measurement of health-related quality of life. Health Policy 1990; 16(3): 199–208. [DOI] [PubMed] [Google Scholar]
- 22. Amini DA, Kannenberg K, Bodison S, et al. Occupational therapy practice framework: domain & process 3rd edition. Am J Occup Ther 2014; 68(Suppl): S1–S48. [Google Scholar]
- 23. Csikszeñtmihaly M, Larson R. Being adolescent: conflict and growth in the teenage years. New York: Basic Books, 1984. [Google Scholar]
- 24. Imai T. The reliability and validity of a new scale for measuring the concept of Ikigai (Ikigai-9). Nihon Koshu Eisei Zasshi 2012; 59(7): 433–439. [PubMed] [Google Scholar]
- 25. Yoshida K, Asakawa K, Yamauchi T, et al. The flow state scale for occupational tasks: development, reliability, and validity. Hong Kong J Occup Ther 2013; 23(2): 54–61. [Google Scholar]
- 26. Granger CV, Hamilton BB, Keith RA, et al. Advances in functional assessment for medical rehabilitation. Top Geriatr Rehabil 1986; 1(3): 59–74. [Google Scholar]
- 27. HernandezAlava M, Wailoo A, Grimm S, et al. EQ-5D-5L versus EQ-5D-3L: the impact on cost effectiveness in the United Kingdom. Value Health 2018; 21(1): 49–56. [DOI] [PubMed] [Google Scholar]
- 28. Shek DTL, Ma CMS. Longitudinal data analyses using linear mixed models in SPSS: concepts, procedures and illustrations. Scientificworldjournal 2011; 11: 42–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hedges LV. Distribution theory for glass’s estimator of effect size and related estimators. J Educ Behav Stat 1981; 6(2): 107–128. [Google Scholar]
- 30. Briggs AH, Wonderling DE, Mooney CZ. Pulling cost-effectiveness analysis up by its bootstraps: a non-parametric approach to confidence interval estimation. Health Econ 1997; 6(4): 327–340. [DOI] [PubMed] [Google Scholar]
- 31. Bovend’Eerdt TJ, Botell RE, Wade DT. Writing SMART rehabilitation goals and achieving goal attainment scaling: a practical guide. Clin Rehabil 2009; 23(4): 352–361. [DOI] [PubMed] [Google Scholar]
- 32. Smallwood J, Schooler JW. The restless mind. Psychol Bull 2006; 132(6): 946–958. [DOI] [PubMed] [Google Scholar]
- 33. Mrazek MD, Smallwood J, Schooler JW. Mindfulness and mind-wandering: finding convergence through opposing constructs. Emotion 2012; 12(3): 442. [DOI] [PubMed] [Google Scholar]
- 34. Skinner BF. The technology of teaching. New York: B.F. Skinner Foundation, 2016. [Google Scholar]
- 35. Redfern J, McKevitt C, Wolfe CDA. Risk management after stroke: the limits of a patient-centred approach. Health Risk Soc 2006; 8(2): 123–141. [Google Scholar]
- 36. Emerson H. Flow and occupation: a review of the literature. Can J Occup Ther 1998; 65(1): 37–44. [Google Scholar]