Abstract
Cardiovascular disease affects 1 in 3 patients and remains the leading cause of death in the United States.1 Severe elevation of low-density lipoprotein cholesterol (LDL-C) levels is a modifiable risk factor for developing premature cardiovascular disease, and elevation levels of 190 mg/dL or greater (to convert LDL-C values to millimoles per liter, multiply by 0.0259) may indicate a monogenic etiology such as familial hypercholesterolemia.2 Treatment with 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors or statins is recommended (class IA) for all adults 21 years or older with an LDL-C of 190 mg/dL or greater. Statin treatment appears to reduce mortality and result in cost savings for health systems.3,4 Therefore, we sought to examine rates of statin prescription in patients screened for dyslipidemia to identify treatment gaps in a real-world contemporary setting.
Keywords: dyslipidemia, statin use, disparities
Methods
For our analysis, we used a deidentified, cloud-based national clinical registry called Explorys (Explorys Inc) that encompasses data from inpatient and outpatient encounters from 360 medical centers in all 50 states. Use of the Explory registry has been deemed exempt from institutional review board approval by University Hospitals Cleveland Medical Center. We included all patients between age 20 and 75 years who had both LDL-C and pharmacy records reported between July 1, 2013, and July 31, 2016. We identified patients with 1 or more statin indications and analyzed them according to groups defined in the 2016 update to the report Heart Disease and Stroke Statistics1: patients with LDL-C of 190 mg/dL or greater,2 patients with diabetes and LDL-C greater than 70 mg/dL,3 and patients with atherosclerotic cardiovascular disease (ASCVD). We did not analyze patients whose sole statin indication was a 10-year cardiovascular risk greater than 7.5%. Statin use was declared for patients prescribed any statin at any dose within the study period (from July 1, 2013, to July 31, 2016). Logistic regression was performed using IBM SPSS Statistics, version 21 (IBM) to model the effect of age, sex, race, and insurance status on statin prescription.
Results
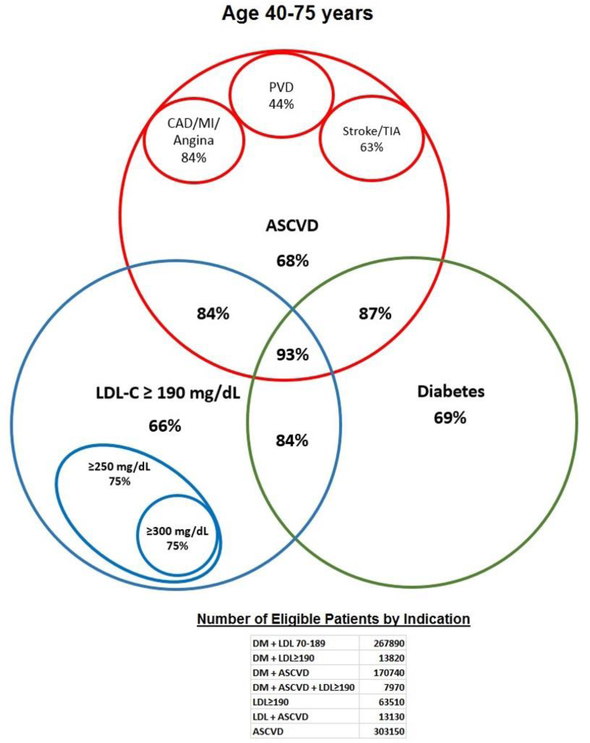
Of the 2 884 260 patients with a qualifying lipid analysis, 109 980 (3.8%) had an LDL-C of 190 mg/dL or greater. The statin prescription rate for patients with severe dyslipidemia but without diabetes or established ASCVD was 66% (41 750) and was comparable with the rates for others with single indications: 69% (183 740) for patients with diabetes but without ASCVD and 68% (207 050) for patients with ASCVD but without diabetes. Even with more severe elevations in LDL-C levels (LDL-C>250 mg/dL and LDL-C>300 mg/dL), 25% (1250) of patients were not prescribed a statin. However, the statin prescription rate for patients (aged 40–75 years) with LDL-C levels of 190 mg/dL or greater was higher if patients had additional statin indications (Figure 1). The prescription rate for patients with LDL-C levels of 190 mg/dL or greater and diabetes or established ASCVD improved to 84% (22 610) and then to 93% (7380) when all 3 conditions coexisted.
Figure 1:
Statin Prescription Rate for Patients 40 to 75 Years, by Indication. Patients aged 40 to 75 years were selected on the basis of having 1 or more indication for a 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitor or statin and were then analyzed within group for statin prescription rates. Statin prescription rates tended to improve when multiple indications were present. ASCVD indicates atherosclerotic cardiovascular disease; CAD, coronary artery disease; DM, diabetes mellitus; LDL-C, low-density lipoprotein cholesterol; MI, myocardial infarction; PVD, peripheral vascular disease; TIA, transient ischemic attack. To convert LDL-C values to millimoles per liter, multiply by 0.0259.
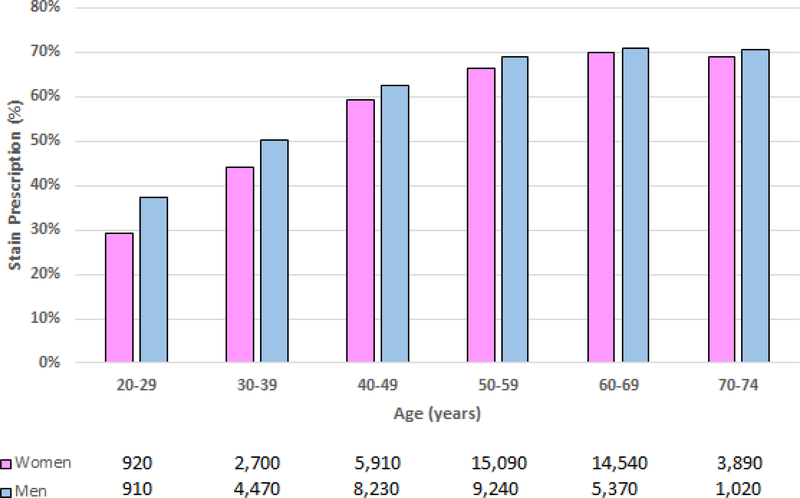
Notably, statin prescription rates for patients with severe dyslipidemia varied sharply by age, with significantly lower rates in younger patients (Figure 2). For instance, statins were prescribed in only 32% (610), 47% (3440), and 61% (8650) of patients in their 30s, 40s, and 50s, respectively. Among patients with an LDL-C level of 190 mg/dL or greater, a multivariable logistic regression model showed that age was by far the most important predictor of statin prescription (age, ≥40 years; adjusted odds ratio [AOR], 2.87; 95% CI, 2.76–2.99; P < .001). Other independent predictors included male sex (AOR, 1.08; 95% CI, 1.05–1.11; P < .001), nonwhite race (AOR, 1.10; 95% CI, 1.07–1.14; P < .001), and self-pay status (AOR, 1.16; 95% CI, 1.10–1.23; P < .001).
Figure 2:
Statin Prescription Rate for Patients With Low-Density Lipoprotein Levels of 190 mg/dL or Greater, by Age Group
Patients with low-density lipoprotein (LDL-C) levels of 190 mg/dL or greater (to convert LDL-C values to millimoles per liter, multiply by 0.0259) were analyzed on the basis of whether a 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitor or statin was prescribed and were then stratified by age group and sex. Younger patients were less likely to be prescribed a statin.
Discussion
We sought to assess statin prescription rates among patients with severe dyslipidemia to identify barriers to ASCVD prevention. The prescription rate for patients with a documented LDL-C level of 190 mg/dL or greater was 66% without ASCVD, but it was 84% for patients with severe dyslipidemia in a secondary prevention setting and 93% for patients with coexisting severe dyslipidemia, diabetes, and ASCVD. Furthermore, prescription rates were highly dependent on age (even after adjusting for other demographics), with less than 45% of patients younger than 40 years receiving a statin prescription. This finding has particular relevance given the early onset of ASCVD and cardiovascular death observed in familial hypercholesterolemia studies from the pre-statin era.5 For this reason, for patients with primary LDL-C elevation level of 190 mg/dL or greater and who are 21 years or older, current guidelines recommend against the use of an ASCVD risk calculation, which could inappropriately lead to deferral of statin therapy for these high-risk patients.6 Specific interventions that optimize the follow up of younger patients after lipid screening may be needed to realize the potential for improved survival and cost reduction associated with the treatment of severe dyslipidemia.
Acknowledgments
Sources of Funding
This work was funded by the Clinical and Translational Science Collaborative of Cleveland grant KL2TR000440 from the National Center for Advancing Translational Sciences component of the National Institutes of Health (NIH) and the NIH Roadmap for Medical Research. The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Disclosures: The authors have no conflict of interest related to the contents of this work.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–360. [DOI] [PubMed] [Google Scholar]
- 2.Austin MA, Hutter CM, Zimmern RL, Humphries SE. Genetic causes of monogenic heterozygous familial hypercholesterolemia: a HuGE prevalence review. Am J Epidemiol. 2004;160(5):407–420. [DOI] [PubMed] [Google Scholar]
- 3.Lazar LD, Pletcher MJ, Coxson PG, Bibbins-Domingo K, Goldman L. Cost-effectiveness of statin therapy for primary prevention in a low-cost statin era. Circulation. 2011;124(2):146–153. [DOI] [PubMed] [Google Scholar]
- 4.Kazi DS, Moran AE, Coxson PG, et al. Cost-effectiveness of PCSK9 inhibitor therapy in patients with heterozygous familial hypercholesterolemia or atherosclerotic cardiovascular disease. JAMA. 2016;316(7):743–753. [DOI] [PubMed] [Google Scholar]
- 5.Stone NJ, Levy RI, Fredrickson DS, Verter J. Coronary artery disease in 116 kindred with familial type II hyperlipoproteinemia. Circulation. 1974;49(3):476–488. [DOI] [PubMed] [Google Scholar]
- 6.Knowles JW, Stone NJ, Ballantyne CM. Familial hypercholesterolemia and the 2013 American College of Cardiology/American Heart Association guidelines: myths, oversimplification, and misinterpretation versus facts. Am J Cardiol. 2015;116(3):481–484. [DOI] [PubMed] [Google Scholar]