Introduction
Chronic diarrhoea is a common problem seen in both primary and secondary care, affecting up to 5% of the general population at any given time.1 Evaluation of chronic diarrhoea poses myriad challenges to the clinician, not in the least because ‘diarrhoea’ means different things to different people (patients and clinicians) but also because it has a diverse aetiology and can be multifactorial in any given individual. Patients relate to loose stool consistency, increased frequency of defaecation, urgency or incontinence (or in combination with one or some of these symptoms) as ‘diarrhoea’ while physicians have traditionally used an increased frequency of defaecation or increased stool weight to define diarrhoea.1
The recent publication of updated British Society of Gastroenterology (BSG) guidelines by Arasaradnam and colleagues addresses this inconsistency, providing a pragmatic definition and approach to the diagnosis and investigation of patients with chronic diarrhoea (figure 1).2 The guidelines define chronic diarrhoea as ‘the persistent alteration from the norm with stool consistency between types 5 and 7 on the Bristol stool chart and increased frequency greater than 4 weeks’ duration’.
Figure 1.
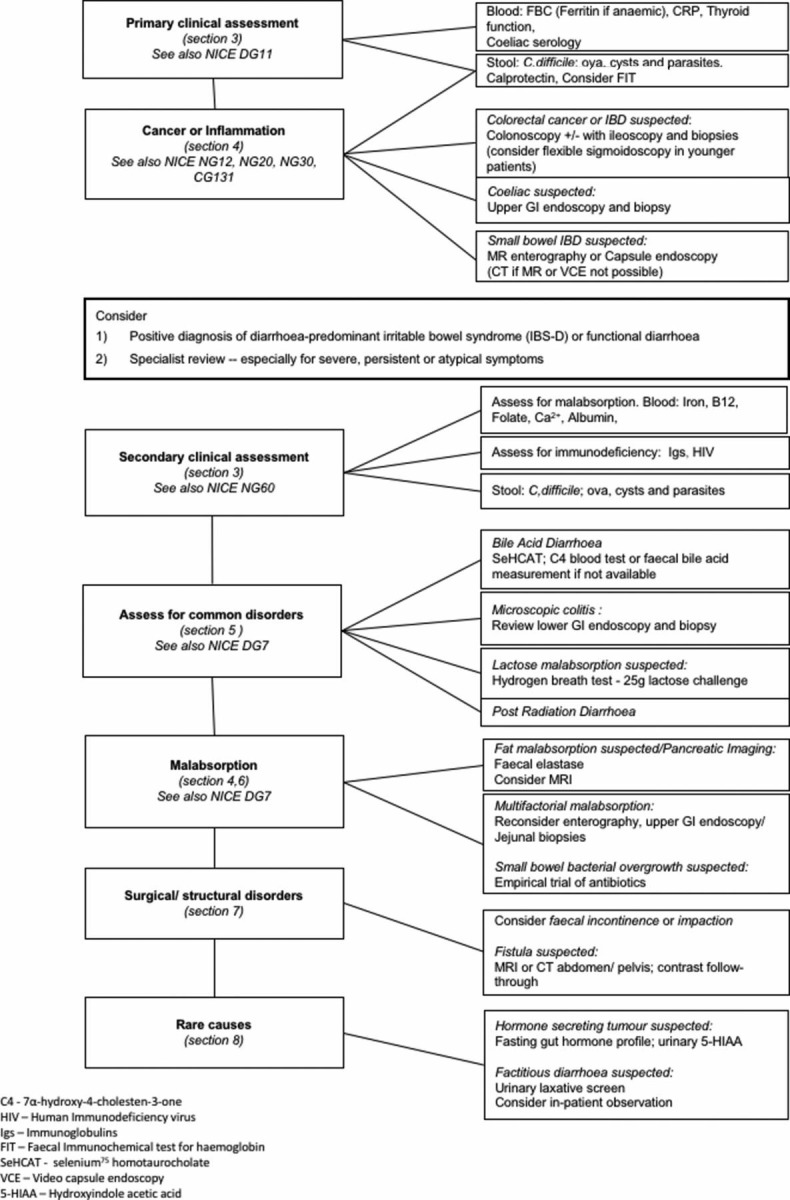
Algorithm for the investigation of chronic diarrhoea based on clinical differential diagnosis. (from Arasaradnam et al, 2018, p. 1381). DG, diagnostics guidance; NG, NICE guideline; NICE, National Institute for Health and Care Excellence.
The challenges presented by the diagnostic workup of chronic diarrhoea are arguably more pronounced in the elderly, wherein diverse aetiologies in the face of multiple potential clinical comorbidities and polypharmacy for these conditions, and additional limitations posed by frailty and resultant inability to undergo recommended investigations need careful consideration. This article aims to offer a pragmatic approach to the assessment of chronic diarrhoea in the elderly (figure 2).
Figure 2.
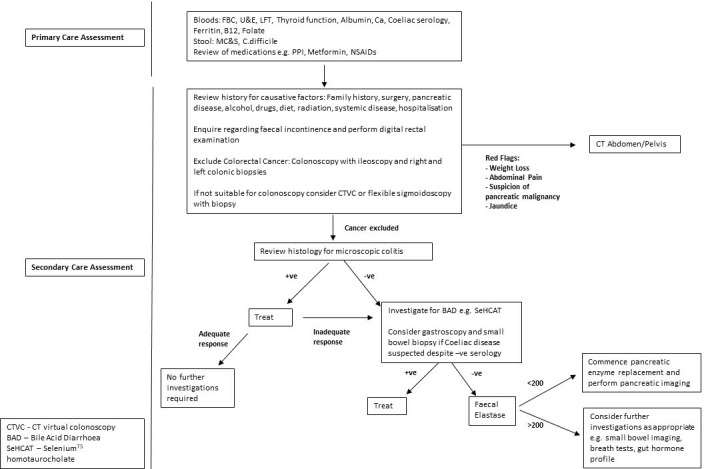
A proposed adapted algorithm for an approach to the assessment of chronic diarrhoea in the elderly. FBC, full blood count; LFT, liver function test; NSAIDs, non-steroidal anti-inflammatory drugs; PPI, proton pump inhibitors; U&E, urea and electrolytes.
Case study
A 73-year-old lady with a history of type 2 diabetes mellitus, controlled hypertension and a previous laparoscopic cholecystectomy is referred urgently to the gastroenterology clinic by her general practitioner (GP). She lives with her husband and is independent with activities of daily living. She reports a 3-month history of a change in bowel habit towards loose, watery stools associated with urgency, frequent nocturnal diarrhoea and occasional episodes of faecal incontinence. Prior to this, she described a normal, formed stool daily. She reports no rectal bleeding, altered blood in the stool or weight loss. She had a recent hospital admission during which she was treated with antibiotics for a community-acquired pneumonia. There has been no recent foreign travel and she denies having used any non-steroidal anti-inflammatory medications recently. Her current medications include metformin, amlodipine, ramipril and omeprazole. There is no relevant family history, she has never smoked and drinks 10 units of alcohol per week with no prior history of excess alcohol intake.
Abdominal examination is unremarkable and a digital rectal examination is normal with no evidence of faecal impaction with normal resting and squeeze anal tone. Blood tests performed by her GP prior to referral including full blood count, vitamin B12, folate and iron studies, serum calcium and albumin, liver chemistry, thyroid function and immunoglobulins are normal. Her IgA transglutaminase antibody for coeliac disease screening is negative. Stool microscopy and culture and Clostridium difficile tests are negative.
Although the widely accepted chronological age of 60 years and over is regarded as ‘elderly’, it must be acknowledged at the outset that potential differences between chronological and biological age must be taken into account in the holistic care of such individuals.3 Thus, a frail patient at any age with comorbid illness and/or limited mobility may be at a higher risk from complications of a medical or surgical intervention as opposed to a much older but physiologically healthy individual. Age-specific concerns such as comorbidity, locomotor and cognitive function and polypharmacy must also be considered carefully.
Chronic diarrhoea may place an elderly patient at risk of dehydration and malnutrition as well as impacting significantly on their quality of life and functional status. The approach to assessment of chronic diarrhoea in the elderly may be complicated by the potential for diarrhoea to be multifactorial as is evident in our patient where there could be a number of factors contributing to her symptoms ranging from diabetes and its treatment (eg, metformin), other medications (eg, omeprazole), cholecystectomy and recent hospitalisation with antibiotic use.4–7 Additional factors to consider in the elderly population are the increased likelihood of colorectal cancer, the second peak of inflammatory bowel disease (IBD) incidence, the potential for polypharmacy contributing to diarrhoea and awareness that faecal incontinence may be more likely in older persons, with or without, associated diarrhoea.
Furthermore, alterations in body composition, as well as hepatic and renal dysfunction are more common in the elderly and may impact on drug pharmacokinetics, with a consequent influence on drug-related chronic diarrhoea and subsequent management.8
While functional bowel disorders clearly exist in the elderly population,9 10 new onset lower gastrointestinal (GI) symptoms should always alert the clinician to the likelihood of an organic pathology and the priority in this age group is to exclude colonic neoplasia.2
Learning outcome 1: New onset gastrointestinal symptoms in the elderly should not be regarded as functional and an organic cause should always be investigated.
Excluding colorectal cancer
The BSG guidelines suggest that faecal immunological testing (FIT) may be used in patients with symptoms suggestive of colorectal cancer without rectal bleeding, as a guide to urgency of referral and prioritisation of investigations.2 The National Institute for Health and Care Excellence have also recommended that FIT could be used in primary care for patients with low-risk symptoms, in the absence of rectal bleeding, who otherwise do not meet the criteria for ‘2-week wait’ (2WW referrals) cancer pathway.11 Elderly patients, newly referred in with chronic diarrhoea, however, would usually be expected to meet 2WW referral guidelines following a documented change in bowel habit or the ‘red flag’ symptom of persistent diarrhoea (>6 weeks) in a person over the age of 60 years.12 The role of FIT does not appear to be fully established in the elderly patient with chronic diarrhoea and it remains to be seen whether it will have a place in secondary care for prioritising patients for colonoscopy.
The exclusion or diagnosis of colorectal cancer relies on colonoscopy. In the elderly population, there are a number of factors that may determine suitability for colonoscopy including comorbidities, frailty, functional baseline and tolerability of bowel preparation.13 14 In patients who are deemed unlikely to tolerate a colonoscopy, a discussion needs to take place between the physician and patient regarding the possible alternatives (flexible sigmoidoscopy, CT virtual colonoscopy (CTVC)) and the suitability of these tests in providing the required diagnostic information.15 16 While a CTVC may be possible in those patients not considered fit for a colonoscopy, the subsequent findings may not be treatable. In such cases, a consideration of the diagnostic utility and prognostic value of such a test in the face of the limits to potential treatment should form an important part of the clinical consultation.
If a colonoscopy is possible, then an ileoscopy should be performed, as also, right-sided and left-sided colonic biopsies with a view to assessing for IBD and particularly for microscopic colitis.2 In those unable to undergo full colonoscopy, a flexible sigmoidoscopy may still allow for assessment and biopsy of the left sided colonic mucosa and thus the potential to diagnose these conditions.
Learning Outcome 2: If deemed fit enough, elderly patients with chronic diarrhoea should undergo colonoscopy with ileoscopy and colonic biopsies.
Colorectal cancer excluded
Following the exclusion of colorectal cancer, decisions focusing on the appropriateness and extent of further investigations should be made in discussion with the patient. If not already done, a thorough review of medications may reveal medication-associated causes of chronic diarrhoea and a considered approach in conjunction with primary care or relevant clinical specialities to consider suitable alternatives if possible.7 A wide range of common medications can cause diarrhoea and a further discussion of drug induced diarrhoea is beyond the scope of this article (box 1).
Box 1. Common causes of drug-induced chronic diarrhoea in the elderly.
PPIs: for example, omeprazole, lansoprazole
H2RAs: for example, ranitidine
NSAIDs: for example, ibuprofen, naproxen, diclofenac
Antibiotics
Biguanides: for example, metformin
Laxatives
Alpha glucosidase inhibitors: for example, acarbose
Motility agents: for example, macrolides, metoclopramide
Cardiac glycosides: for example, digoxin
Chemotherapy agents: for example, epirubicin, 5-flurouracil, methotrexate, cisplatin
Magnesium supplements
ACE inhibitors: for example, ramipril, lisinopril
Colchicine
Thyroid hormones: for example, levothyroxine
SSRIs: for example, sertraline, citalopram
H2RAs, H2 receptor antagonists; NSAIDs, non-steroidal anti-inflammatory drugs; PPIs, proton pump inhibitors; SSRIs, serotonin selective reuptake inhibitors.
Learning Outcome 3: Medications are a common cause of diarrhoea in the elderly and a thorough medications review should be conducted.
Consider faecal incontinence
Faecal incontinence is common and may be mistaken or misrepresented by patients as ‘diarrhoea’.17 It is likely to be an under-reported problem in the elderly population although some studies suggest prevalence rates of around 10%.18 When faecal incontinence is reported, a distinction must be made between incontinence resulting from a structural or neurological condition affecting the anal sphincter complex or symptoms secondary to chronic diarrhoea overwhelming the sphincter. Conditions such as bile acid diarrhoea (BAD) and microscopic colitis which can cause profuse watery diarrhoea frequently cause episodes of faecal incontinence which may improve following appropriate treatment of the underlying condition. It is therefore important to enquire in the initial assessment whether the patient is experiencing symptoms of faecal incontinence as, if the incontinence is judged to be secondary to underlying chronic diarrhoea, the diagnostic workup can focus on identifying the cause of this. The value of an accurate history cannot be over-emphasised.
Faecal loading with subsequent ‘overflow diarrhoea’ and faecal incontinence is not uncommon in the elderly population, in particular those with cognitive or behavioural issues or those with neurological or spinal disease.19 If suspected, faecal impaction should be identified with an anorectal examination and appropriate treatment commenced.20 If faecal incontinence is not felt to be secondary to chronic diarrhoea or faecal impaction, then subsequent investigation may involve dynamic pelvic imaging, endoanal ultrasound, anorectal manometry and onward referral for surgical assessment or biofeedback.17
Faecal incontinence may occur in women as a consequence of childbirth or obstetric complications. In the elderly female population, the formation of a rectocele, secondary to relaxation of the pelvic floor and weakening of the levator ani muscles, may lead to incomplete rectal emptying and subsequent faecal leakage.21 A gynaecological or specialist surgical assessment is often necessary in these situations.
A detailed discussion on the specialist assessment of faecal incontinence, unassociated with diarrhoea, is beyond the scope of this article and is not discussed further but the reader is referred to extensive reviews on this subject for further information.22–24 A range of non-pharmacological techniques ranging from biofeedback therapy and neuromodulation to use of incontinence pads and anal plugs as also dietary modifications may be employed to aid symptom control but will not be helpful if an underlying diarrhoeal disease is the main factor causing incontinence.
Learning Outcome 4: The investigation of faecal incontinence will differ depending on whether it is felt to be caused by chronic diarrhoea or not.
Further assessment of chronic diarrhoea in the elderly
In an elderly patient with profuse, watery, non-bloody, diarrhoea, both microscopic colitis and BAD are frequently misdiagnosed as diarrhoea predominant IBS (IBS-D)25 26 or misattributed to diverticular disease. In the majority of cases, treatment is relatively straightforward and therefore, a positive diagnosis with appropriate treatment can result in significant improvement in quality of life and functional status.
Learning Outcome 5: Chronic diarrhoea secondary to microscopic colitis or bile acid malabsorption is frequently incorrectly labelled as IBS-D in the elderly.
Microscopic colitis
Microscopic colitis, encompassing collagenous colitis and lymphocytic colitis, is more common in women with the mean age of presentation around 60, so will remain common in the elderly population.27 A number of drugs, frequently used in the elderly, are also implicated as potential causes of microscopic colitis including non-steroidal anti-inflammatory drugs, proton pump inhibitors (PPIs) and serotonin selective reuptake inhibitors.28 Among patients diagnosed with IBS-D, up to 10% will have a positive diagnosis of microscopic colitis.26 It typically presents with chronic, non-bloody, secretory diarrhoea, frequently with nocturnal symptoms and episodes of faecal incontinence.28 Macroscopically, the colonic mucosa appears normal at colonoscopy and the diagnosis is made at histological assessment of left and right colonic mucosal biopsies.28 In both forms, histology demonstrates an increase in intraepithelial and lamina propria lymphocytes (>20/100 cells) and the addition of a thickened subepithelial collagen band (>10 um) differentiates collagenous colitis from lymphocytic colitis.29
Following a positive diagnosis of microscopic colitis, controlled release preparations of budesonide are effective in inducing and, if required, maintaining remission. The reader is referred to the American Gastroenterological Association guidelines on the medical management of microscopic colitis for a more comprehensive discussion.30
The relative increased frequency of coeliac disease (around 2%–9%) and BAD (29%–41%) associated with microscopic colitis should prompt further investigation, directed at these conditions, if symptoms fail to settle following commencement of budesonide.27 28 If coeliac serology is negative, it may still be prudent to perform small bowel biopsies if the index of suspicion is high and is essential in any patient with iron deficiency anaemia or weight loss.28 30
Learning Outcome 6: In microscopic colitis, if there is an inadequate response to budesonide, other diagnoses such as bile acid diarrhoea and coeliac disease should be excluded at any age.
Bile acid diarrhoea
BAD may be diagnosed in up to 30% of patients who have been previously diagnosed with IBS-D.25 31 Given its frequency, BAD should be excluded in elderly patients in whom endoscopic procedures and histology have, as yet, failed to identify a cause for their persistent diarrhoea. Cholecystectomy, small bowel resection, ileal disease, pelvic chemoradiotherapy and post-infectious diarrhoea have all been associated with BAD.32 33
Selenium homocholic acid taurine (SeHCAT) testing is the most commonly used investigation for identifying BAD.34 At SeHCAT testing,<5% retention of tauroselcholic (Se) acid at 7 days is considered severe bile acid loss with 10%–15% retention considered mildly abnormal. If confirmed, patients should be commenced on bile acid sequestrants (eg, colestyramine, colesevelam or colestipol)35 and a low-fat diet advised. Therapeutic trials of bile acid sequestrants, in the absence of confirmed BAD, are not recommended in the absence of an obvious aetiology such as ileal resection for Crohn’s disease and a trial should not be considered an adequate diagnostic test.2 36
Learning Outcome 7: Bile acid diarrhoea is an often overlooked aetiology for chronic diarrhoea in the elderly and should be considered if a diagnosis is not evident from endoscopic procedures and subsequent histology.
Pancreatic exocrine insufficiency
Pancreatic exocrine insufficiency, resulting from impairment of pancreatic enzyme and bicarbonate secretion, results in maldigestion and consequently, diarrhoea. Steatorrhoea, secondary to maldigestion of fat, may not be clinically apparent and the appearance of stools is not a reliable marker of its presence.37 While a history of pancreatitis, pancreatic surgery or pancreatic cancer would typically prompt investigation of pancreatic exocrine insufficiency in the elderly, there is also evidence that pancreatic atrophy occurs with advancing age.38 39 Up to 5% and 10% of individuals over the age of 70 and 80 years, respectively, with GI symptoms, will have evidence of pancreatic exocrine insufficiency with consequent risk of malnutrition.39 Furthermore, exocrine pancreatopathy is recognised in patients with diabetes mellitus.40–42
The measurement of human faecal elastase-1 is generally the preferred test of pancreatic function being a sensitive biomarker for moderate to severe but not mild pancreatic insufficiency.43 A faecal elastase value of <200 ug/g should prompt pancreatic enzyme replacement and subsequent investigation for causes of pancreatic exocrine insufficiency. In the elderly, an initial CT scan, if not already performed, will help exclude pancreatic malignancy and other advanced pancreatic disease or age-related atrophy as a cause for exocrine insufficiency. If the CT is unremarkable then clinical judgement should be used in determining the appropriateness of further pancreatic imaging with magnetic resonance cholangiopancreatography and endoscopic ultrasound versus symptomatic management alone with enzyme replacement.2
Learning Outcome 8: Pancreatic exocrine insufficiency is not uncommon in the elderly population and may be easily overlooked. A faecal elastase is a relatively simple, non-invasive investigation that can be used to screen for moderate to severe disease.
Other investigations
Small bowel bacterial overgrowth
Small bowel bacterial overgrowth (SBBO) may be asymptomatic or present with symptoms similar to IBS, presenting with chronic diarrhoea.44 There is marked variance in the quoted prevalence of SBBO in IBS with one meta-analysis suggesting a range of between 4% and 64%.45 Patients with abnormal oro-caecal transit, due to anatomical or functional reasons, are reported to be at increased risk. In the elderly, this may stem from diabetes, previous surgery or intestinal diverticulosis. Furthermore, achlorhydria associated with old age and PPI therapy increases the risk of SBBO and older age is associated with increasing numbers of small intestinal strict anaerobes.44
Hydrogen/methane breath testing shows poor sensitivity and specificity for detection of SBBO and as such, if suspicion is high, BSG guidelines recommend proceeding to an empirical trial of antibiotics.2 In the elderly patient with chronic diarrhoea and symptoms of malabsorption, who may have some of the risk factors for SBBO outlined above and in whom investigations have thus far not revealed a diagnosis, it may be prudent to undergo confirmatory breath testing to avoid potential exposure to repeated empirical courses of antibiotics and their undesirable consequences.2 Given the association between achlorhydria, older age and SBBO, and in the absence of an optimal diagnostic test, it seems plausible that SBBO is under-diagnosed as a cause of chronic diarrhoea in the elderly population. Further research is required here.
Faecal calprotectin
The use of faecal calprotectin is recommended in primary care to aid differentiation between IBS and potential IBD when recent onset lower GI symptoms occur in the younger adult population in whom colorectal cancer is not suspected. It should not be used as a screening test in the elderly.2 46 Elderly patients with a change in bowel habit will automatically meet 2WW referral criteria and as such, a negative faecal calprotectin in primary care, or elsewhere, should not prevent onward referral. A raised calprotectin is non-specific and can occur in IBD, microscopic colitis and colorectal cancer, as well as other GI conditions.47 48 Faecal calprotectin may have a role, should a subsequent diagnosis of IBD be made, when it has the potential to be used as a non-invasive method of monitoring disease activity.49
Small bowel imaging
If small intestinal abnormalities are suspected in elderly patients with chronic diarrhoea, for example following a suspected diagnosis of Crohn’s disease at colonoscopy, then CT or magnetic resonance enterography is the recommended initial investigation of choice for imaging the small bowel.2 50 Video capsule endoscopy may have a role in specific cases depending on findings at initial imaging. However, in the majority of cases of chronic diarrhoea in the elderly, small bowel imaging will not form part of the diagnostic workup.
Neuroendocrine tumours
While the incidence of neuroendocrine tumours (NETs) is on the rise, they remain a rare cause of chronic diarrhoea.51 Unless prior imaging studies, or indeed symptoms and signs, suggest a NET, testing for NETs is not typically a part of the baseline diagnostic workup in the elderly patient with chronic diarrhoea.
Patient outcome
Our patient underwent an ileo-colonoscopy which was normal aside from some hyperplastic rectal polyps. Ileal and colonic biopsies were normal. She underwent a SeHCAT test which revealed severe bile salt malabsorption. Her faecal elastase test was normal. She responded well to a trial of bile salt sequestrants (colesevelam) with normalisation of stool frequency. It was felt that she did not have any clinical indication to continue her PPI and it was discontinued. Metformin was considered in the differential diagnosis of her chronic diarrhoea but as her symptoms resolved with the addition of a bile salt sequestrant (taken 1 hour before her morning medications), it was not felt necessary to consider alternatives.
Conclusions
Chronic diarrhoea is common with potentially serious implications to patients’ health and quality of life. Challenges conferred by the diverse aetiology of chronic diarrhoea itself notwithstanding, inconsistencies in patients’ (and indeed clinicians) interpretation of symptoms, may delay an accurate diagnosis. This is likely more pronounced in the elderly with multiple clinical comorbidities and related therapy. A structured approach based on pathophysiological causes of chronic diarrhoea can facilitate early and often accurate identification of aetiological factors and enable effective therapy where possible. The recently published BSG guidelines offer a pragmatic, evidence-based approach to the assessment of chronic diarrhoea. A logical approach to assessment can positively influence patients’ health-related quality of life, compress clinical morbidity and, in doing so, have wider and positive implications to the health economy.
Footnotes
Correction notice: This article has been corrected since it published Online First. The title has been corrected.
Contributors: BC wrote the initial draft, which was then revised and edited by JM and JL.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Commissioned; externally peer reviewed.
References
- 1. Schiller LR, Pardi DS, Spiller R, et al. Gastro 2013 APDW/WCOG Shanghai Working Party report: chronic diarrhea: definition, classification, diagnosis. J Gastroenterol Hepatol 2014;29:6–25. 10.1111/jgh.12392 [DOI] [PubMed] [Google Scholar]
- 2. Arasaradnam RP, Brown S, Forbes A, et al. Guidelines for the investigation of chronic diarrhoea in adults: British Society of Gastroenterology, 3rd edition. Gut 2018;67:1380–99. 10.1136/gutjnl-2017-315909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Proposed working definition of an older person in Africa for the MDS project, 2002. Available: https://www.who.int/healthinfo/survey/ageingdefnolder/en/
- 4. Ratnaike RN, Jones TE. Mechanisms of drug-induced diarrhoea in the elderly. Drugs Aging 1998;13:245–53. 10.2165/00002512-199813030-00007 [DOI] [PubMed] [Google Scholar]
- 5. Sciarretta G, Furno A, Mazzoni M, et al. Post-cholecystectomy diarrhea: evidence of bile acid malabsorption assessed by SeHCAT test. Am J Gastroenterol 1992;87:1852–4. [PubMed] [Google Scholar]
- 6. Piper MS, Saad RJ. Diabetes mellitus and the colon. Curr Treat Options Gastroenterol 2017;15:460–74. 10.1007/s11938-017-0151-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Philip NA, Ahmed N, Pitchumoni CS. Spectrum of drug-induced chronic diarrhea. J Clin Gastroenterol 2017;51:111–7. 10.1097/MCG.0000000000000752 [DOI] [PubMed] [Google Scholar]
- 8. Klotz U. Pharmacokinetics and drug metabolism in the elderly. Drug Metab Rev 2009;41:67–76. 10.1080/03602530902722679 [DOI] [PubMed] [Google Scholar]
- 9. De Lillo AR, Rose S. Functional bowel disorders in the geriatric patient: constipation, fecal impaction, and fecal incontinence. Am J Gastroenterol 2000;95:901–5. 10.1016/S0002-9270(00)00718-8 [DOI] [PubMed] [Google Scholar]
- 10. Talley NJ, O'Keefe EA, Zinsmeister AR, et al. Prevalence of gastrointestinal symptoms in the elderly: a population-based study. Gastroenterology 1992;102:895–901. 10.1016/0016-5085(92)90175-X [DOI] [PubMed] [Google Scholar]
- 11. Quantitative faecal immunochemical tests to guide referral for colorectal cancer in primary care, 2017. Available: https://www.nice.org.uk/guidance/dg30 [PubMed]
- 12. Suspected cancer: recognition and referral, 2015. Available: https://www.nice.org.uk/guidance/ng12/chapter/1-Recommendations-organised-by-site-of-cancer#lower-gastrointestinal-tract-cancers
- 13. Day LW, Kwon A, Inadomi JM, et al. Adverse events in older patients undergoing colonoscopy: a systematic review and meta-analysis. Gastrointest Endosc 2011;74:885–96. 10.1016/j.gie.2011.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cha JM, Kozarek RA, La Selva D, et al. Risks and benefits of colonoscopy in patients 90 years or older, compared with younger patients. Clin Gastroenterol Hepatol 2016;14:80–6. 10.1016/j.cgh.2015.06.036 [DOI] [PubMed] [Google Scholar]
- 15. Villa NA, Pannala R, Pasha SF, et al. Alternatives to incomplete colonoscopy. Curr Gastroenterol Rep 2015;17 10.1007/s11894-015-0468-7 [DOI] [PubMed] [Google Scholar]
- 16. Leung WCY, Foo DCC, Chan TT, et al. Alternatives to colonoscopy for population-wide colorectal cancer screening. Hong Kong Med J 2016;22:70–7. 10.12809/hkmj154685 [DOI] [PubMed] [Google Scholar]
- 17. Rao SSC. Pathophysiology of adult fecal incontinence. Gastroenterology 2004;126(1 Suppl 1):S14–S22. 10.1053/j.gastro.2003.10.013 [DOI] [PubMed] [Google Scholar]
- 18. Gillibrand W. Management of faecal incontinence in the elderly: current policy and practice. Br J Community Nurs 2016;21:554–6. 10.12968/bjcn.2016.21.11.554 [DOI] [PubMed] [Google Scholar]
- 19. Barrett JA, Brocklehurst JC, Kiff ES, et al. Anal function in geriatric patients with faecal incontinence. Gut 1989;30:1244–51. 10.1136/gut.30.9.1244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rao SSC. Rectal exam: Yes, it can and should be done in a busy practice! Am J Gastroenterol 2018;113:635–8. 10.1038/s41395-018-0006-y [DOI] [PubMed] [Google Scholar]
- 21. Williams KS, Shalom DF, Winkler HA. Faecal incontinence: a narrative review of clinic-based management for the general gynaecologist. J Obstet Gynaecol 2018;38:1–9. 10.1080/01443615.2017.1344204 [DOI] [PubMed] [Google Scholar]
- 22. Faecal incontinence in adults: management, 2007. Available: https://www.nice.org.uk/guidance/cg49
- 23. García Cabrera AM, Jiménez Rodríguez RM, Reyes Díaz ML, et al. Fecal incontinence in older patients. A narrative review. Cir Esp 2018;96:131–7. 10.1016/j.cireng.2017.12.005 [DOI] [PubMed] [Google Scholar]
- 24. Nigam GB, Limdi JK, Vasant DH. Current perspectives on the diagnosis and management of functional anorectal disorders in patients with inflammatory bowel disease. Therap Adv Gastroenterol 2018;11 10.1177/1756284818816956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Smith MJ, Cherian P, Raju GS, et al. Bile acid malabsorption in persistent diarrhoea. J R Coll Physicians Lond 2000;34:448–51. [PMC free article] [PubMed] [Google Scholar]
- 26. Guagnozzi D, Arias Á, Lucendo AJ. Systematic review with meta-analysis: diagnostic overlap of microscopic colitis and functional bowel disorders. Aliment Pharmacol Ther 2016;43:851–62. 10.1111/apt.13573 [DOI] [PubMed] [Google Scholar]
- 27. Rasmussen MA, Munck LK. Systematic review: are lymphocytic colitis and collagenous colitis two subtypes of the same disease - microscopic colitis? Aliment Pharmacol Ther 2012;36:79–90. 10.1111/j.1365-2036.2012.05166.x [DOI] [PubMed] [Google Scholar]
- 28. Pardi DS. Diagnosis and management of microscopic colitis. Am J Gastroenterol 2017;112:78–85. 10.1038/ajg.2016.477 [DOI] [PubMed] [Google Scholar]
- 29. Langner C, Aust D, Ensari A, et al. Histology of microscopic colitis-review with a practical approach for pathologists. Histopathology 2015;66:613–26. 10.1111/his.12592 [DOI] [PubMed] [Google Scholar]
- 30. Nguyen GC, Smalley WE, Vege SS, et al. American gastroenterological association Institute guideline on the medical management of microscopic colitis. Gastroenterology 2016;150:242–6. quiz e17-8 10.1053/j.gastro.2015.11.008 [DOI] [PubMed] [Google Scholar]
- 31. Slattery SA, Niaz O, Aziz Q, et al. Systematic review with meta-analysis: the prevalence of bile acid malabsorption in the irritable bowel syndrome with diarrhoea. Aliment Pharmacol Ther 2015;42:3–11. 10.1111/apt.13227 [DOI] [PubMed] [Google Scholar]
- 32. Barkun AN, Love J, Gould M, et al. Bile acid malabsorption in chronic diarrhea: pathophysiology and treatment. Can J Gastroenterol 2013;27:653–9. 10.1155/2013/485631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Phillips F, Muls ACG, Lalji A, et al. Are bile acid malabsorption and bile acid diarrhoea important causes of loose stool complicating cancer therapy? Colorectal Dis 2015;17:730–4. 10.1111/codi.12932 [DOI] [PubMed] [Google Scholar]
- 34. Mottacki N, Simrén M, Bajor A. Review article: bile acid diarrhoea - pathogenesis, diagnosis and management. Aliment Pharmacol Ther 2016;43:884–98. 10.1111/apt.13570 [DOI] [PubMed] [Google Scholar]
- 35. Wedlake L, A'Hern R, Russell D, et al. Systematic review: the prevalence of idiopathic bile acid malabsorption as diagnosed by SeHCAT scanning in patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther 2009;30:707–17. 10.1111/j.1365-2036.2009.04081.x [DOI] [PubMed] [Google Scholar]
- 36. SeHCAT (tauroselcholic [75 selenium] acid) for the investigation of diarrhoea due to bile acid malabsorption in people with diarrhoea-predominant irritable bowel syndrome (IBS-D) or Crohn's disease without ileal resection, 2012. Available: https://www.nice.org.uk/guidance/dg7
- 37. Lankisch PG, Dröge M, Hofses S, et al. Steatorrhoea: you cannot trust your eyes when it comes to diagnosis. Lancet 1996;347:1620–1. 10.1016/S0140-6736(96)91107-1 [DOI] [PubMed] [Google Scholar]
- 38. Sato T, Ito K, Tamada T, et al. Age-related changes in normal adult pancreas: MR imaging evaluation. Eur J Radiol 2012;81:2093–8. 10.1016/j.ejrad.2011.07.014 [DOI] [PubMed] [Google Scholar]
- 39. Löhr J-M, Panic N, Vujasinovic M, et al. The ageing pancreas: a systematic review of the evidence and analysis of the consequences. J Intern Med 2018;283:446–60. 10.1111/joim.12745 [DOI] [PubMed] [Google Scholar]
- 40. Mohapatra S, Majumder S, Smyrk TC, et al. Diabetes mellitus is associated with an exocrine Pancreatopathy: conclusions from a review of literature. Pancreas 2016;45:1104–10. 10.1097/MPA.0000000000000609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kangrga RN, Ignjatović SD, Dragašević MM, et al. Pancreatic elastase levels in feces as a marker of exocrine pancreatic function in patients with diabetes mellitus. Lab Med 2016;47:140–8. 10.1093/labmed/lmw015 [DOI] [PubMed] [Google Scholar]
- 42. Rathmann W, Haastert B, Icks A, et al. Low faecal elastase 1 concentrations in type 2 diabetes mellitus. Scand J Gastroenterol 2001;36:1056–61. [DOI] [PubMed] [Google Scholar]
- 43. Domínguez-Muñoz JE, D Hardt P, Lerch MM, et al. Potential for screening for pancreatic exocrine insufficiency using the fecal elastase-1 test. Dig Dis Sci 2017;62:1119–30. 10.1007/s10620-017-4524-z [DOI] [PubMed] [Google Scholar]
- 44. Grace E, Shaw C, Whelan K, et al. Review article: small intestinal bacterial overgrowth--prevalence, clinical features, current and developing diagnostic tests, and treatment. Aliment Pharmacol Ther 2013;38:674–88. 10.1111/apt.12456 [DOI] [PubMed] [Google Scholar]
- 45. Ford AC, Spiegel BMR, Talley NJ, et al. Small intestinal bacterial overgrowth in irritable bowel syndrome: systematic review and meta-analysis. Clin Gastroenterol Hepatol 2009;7:1279–86. 10.1016/j.cgh.2009.06.031 [DOI] [PubMed] [Google Scholar]
- 46. The new faecal calprotectin care pathway, 2018. Available: https://www.nice.org.uk/contents/item/display/30916
- 47. Caviglia GP, Ribaldone DG, Rosso C, et al. Fecal calprotectin: beyond intestinal organic diseases. Panminerva Med 2018;60:29–34. 10.23736/S0031-0808.18.03405-5 [DOI] [PubMed] [Google Scholar]
- 48. Alibrahim B, Aljasser MI, Salh B. Fecal calprotectin use in inflammatory bowel disease and beyond: a mini-review. Can J Gastroenterol Hepatol 2015;29:157–63. 10.1155/2015/950286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Mosli MH, Zou G, Garg SK, et al. C-reactive protein, fecal calprotectin, and stool lactoferrin for detection of endoscopic activity in symptomatic inflammatory bowel disease patients: a systematic review and meta-analysis. Am J Gastroenterol 2015;110:802–19. quiz 820 10.1038/ajg.2015.120 [DOI] [PubMed] [Google Scholar]
- 50. Maaser C, et al. ECCO-ESGAR guideline for diagnostic assessment in inflammatory bowel disease. J Crohns Colitis 2018. [Google Scholar]
- 51. Huguet I, Grossman AB, O'Toole D. Changes in the epidemiology of neuroendocrine tumours. Neuroendocrinology 2017;104:105–11. 10.1159/000441897 [DOI] [PubMed] [Google Scholar]


