Abstract
Although policies and programs exist to promote safe motherhood in sub-Saharan Africa, maternal health has not improved and may be deteriorating in some countries. Part of the explanation may be the adverse effects of HIV/AIDS on maternity care. We conducted a study in Kisumu, Kenya to explore how fears related to HIV/AIDS affect women’s uptake and health workers’ provision of labor and delivery services. In-depth qualitative interviews with 17 maternity workers, 14 pregnant or postpartum women, four male partners and two traditional birth attendants; as well as structured observations of 22 births; were conducted at four health facilities. Participants reported that fears of HIV testing; fears of involuntary disclosure of HIV status to others, including spouses; and HIV/AIDS stigma are among the reasons that women avoid delivering in health facilities. Maternity workers now have to take into account the HIV status of the women they serve (as well as their own fears of becoming infected and stigmatized) but do not seem to be adequately prepared to handle issues related to consent, confidentiality and disclosure. Importantly, it appeared that women of unknown HIV status during labor and delivery were likely to be targets of stigma and discriminatory practices and that these women were not receiving needed counseling services. The findings suggest that increasing infection control precautions will not be enough to address the challenges faced by maternity care providers in caring for women in high-HIV-prevalence settings. Maternity workers need enhanced culturally sensitive training regarding consent, confidentiality and disclosure. Furthermore, this study points to the necessity of paying more attention to the care of women of unknown HIV-serostatus during labor and delivery. Such interventions may improve the quality of maternity care, increase utilization and contribute to overall improvements in maternal health, while also enhancing prevention of mother-to-child-transmission and HIV care.
Keywords: maternal health, HIV/AIDS, safe motherhood, prevention of mother-to-child transmission, Kenya
Introduction
In sub-Saharan Africa, women comprise approximately 60% of adults living with HIV and young women aged 15–24 are at least three times more likely to be HIV-positive than young men (UNAIDS, 2005). African women also suffer from high levels of unsafe pregnancy and childbirth – the estimated maternal mortality ratio for sub-Saharan Africa was 920 per 100,000 live births in 2000 (WHO, UNICEF, & UNFPA, 2004). Thus, HIV/AIDS and maternal mortality have been referred to as “intersecting epidemics” in sub-Saharan Africa (McIntyre, 2003). Basic maternity services – antenatal care (ANC), skilled delivery attendance and postpartum care – are key interventions for improving maternal health (WHO, 2005) and are especially important for HIV-positive women who may be at greater risk for complications (Gray & McIntyre, 2007).
A recent review of maternal mortality (Graham & Hussein, 2003) recommended assessing the effects of HIV/AIDS on the uptake of maternal health services. In high-HIV-prevalence areas, where HIV testing and prevention of mother-to-child transmission (PMTCT) interventions are standard components of maternity care, women might avoid health facilities for maternity care because of HIV-related fears. Findings from studies in Africa (Etiebet, Fransman, Forsyth, Coetzee, & Hussey, 2004) suggest that pregnant women may be avoiding ANC clinics because of fears of compulsory HIV testing and unwanted disclosure. However, few studies have examined the impact of these fears on women’s decisions regarding where to deliver.
Further, there are indications that HIV/AIDS adversely affects the provision and quality of maternity and other health services in sub-Saharan Africa (Dovlo, 2005; Gerein, Green, & Pearson, 2006). Health workers’ fears of HIV infection and their related discriminatory practices have been identified as a continuing problem in many countries (Ortega, Bicaldo, Sobritchea, & Tan, 2005; Reidpath & Chan, 2005; Reis et al., 2005). Labor and delivery services are especially vulnerable to these problems since they involve exposure to bodily fluids, must be available 24 hours a day and include emergency care (Mathole, Lindmark, & Ahlberg, 2006). Discrimination against HIV-positive pregnant women has been reported in maternity services in diverse settings (Bain Brickley, Hahn, Nguyet, Giang, & Sohn, 2006; Bond, Chase, & Aggleton, 2002; Misiri, Tadesse, & Muula, 2004; PlusNews, 2006).
To better understand the relationship between HIV/AIDS and maternity services in a high-HIV-prevalence setting, we conducted a qualitative study using in-depth interviews and structured observations of childbirth services in Kisumu, Kenya during July–August 2006. This paper focuses on how HIV-related fears may affect where women deliver and on the difficulties maternity workers face caring for HIV-positive women and women with unknown HIV status.
Methods
Sites
This study was conducted in four maternity care facilities: a provincial hospital, a district hospital, a municipal health center and a small private hospital serving lower-middle income clients in Kisumu, Nyanza Province, Kenya. Nyanza Province has the highest HIV prevalence in Kenya; 18.3% of women and 11.6% of men aged 15–49 were estimated to be infected in 2003 (National AIDS and STI Control Programme of the Ministry of Health [Kenya], 2005). HIV prevalence has ranged from 26–35% among ANC attendees at the provincial hospital in recent years (Van’t Hoog et al., 2005). In Nyanza Province, 85% of women receive at least some ANC from a health professional, but only 36% of women deliver in a health facility (Central Bureau of Statistics [Kenya], Ministry of Health [Kenya], & ORC Macro, 2004). Approval for this study was obtained from the institutional review boards of the Kenya Medical Research Institute (KEMRI) and the University of California, San Francisco, as well as from the participating facilities.
In-depth interviews
Thirty-eight in-depth interviews were conducted to explore provider and client perspectives on HIV/AIDS and maternity services. Participants included administrators, facility-based maternity care workers, traditional birth attendants (TBAs), pregnant or postpartum women and male partners of pregnant or postpartum women (See Table 1). Interviews were conducted in English, Dholuo or Kiswahili by a Kenyan nurse-midwife and a male Kenyan social scientist. Following an informed consent process, interviews were conducted in a private room at the participating health facilities or a nearby location where privacy could be maintained. Interviewers used open-ended discussion guides and the interviews were audio-recorded. Potential maternity-worker participants were purposively selected to include different viewpoints by profession, duties, gender and years of experience. Traditional birth attendants were identified from those known to local health workers at the study health facilities as having high-volume home birth practices. Pregnant and postpartum women attending maternity services were recruited at the study health facilities. In order to assure confidentiality, male partners were partners of women receiving maternity services at the same facilities, but were not partners of women being interviewed for the study. Due to the sensitivity of the subject of HIV/AIDS and the stigma and discrimination that could be associated with disclosure, interviewers found that participants were most responsive to questions about the effects of HIV/AIDS on women in their community in general, rather than personal questions.
Table 1.
Characteristics of participants in in-depth interviews (n = 38).
| Number of participants | |
|---|---|
| Type | |
| Pregnant woman | 7 |
| Postpartum woman | 7 (2 home delivery, 5 health facility delivery) |
| Male partner | 4 |
| Health administrator | 5 (4 physicians, 1 nurse) |
| Non-administrator nurse | 11 |
| Non-administrator physician | 2 |
| Traditional birth attendant | 2 |
| Place of recruitment | |
| Health center | 15 |
| District hospital | 10 |
| Provincial hospital | 7 |
| Private maternity hospital | 6 |
| Gender | |
| Female | 31 |
| Male | 7 |
| Age | |
| < 30 years of age | 12 |
| 30–39 years of age | 15 |
| > =40 years of age | 11 |
| Education | |
| Less than secondary | 5 (all of them pregnant women) |
| Secondary | 22 |
| More than secondary | 11 (10 health workers, 1 male partner) |
| Marital status | |
| Unmarried | 5 |
| Married | 30 |
| Widowed | 3 |
| HIV status disclosed to the interviewer | |
| Yes, HIV-positive | 12 |
| Yes, HIV-negative | 3 |
| No | 23 |
Structured observations
Twenty-two observations (See Table 2) of labor, delivery and postpartum care were conducted by a Kenyan nurse-midwife (eight births at each of the larger hospitals, four at the health center and two at the private maternity hospital). She observed the care of individual women, from admission to the maternity ward until discharge or the end of her 12-hour shift. She used a checklist to record observations including condition on arrival; determination of HIV status; counseling; treatment by maternity workers; type of delivery; maternal and infant outcomes; disclosure of HIV status to others and receipt of PMTCT interventions. Some data were also obtained from the woman’s medical chart. Verbal consent for the observations was obtained from maternity workers and individual consent for the observation and abstraction of information from medical records was obtained from each woman observed.
Table 2.
Complete birth observations (n = 22).
| Number of HIV-positive women (n = 5) | Number of HIV-negative women (n = 12) | Number of HIV status unknown women (n = 5) | |
|---|---|---|---|
| Health facility | |||
| Health center | 1 | 3 | 0 |
| District hospital | 1 | 4 | 3 |
| Private hospital | 0 | 1 | 1 |
| Provincial hospital | 3 | 4 | 1 |
| ≤ 18 years of age | 1 | 1 | 3 |
| No antenatal care | 0 | 0 | 1 |
| Arrived in advanced 2nd stage of labor | 1 | 2 | 4 |
| Experienced complication | 0 | 4 | 2 |
| Maternal or infant death | 0 | 0 | 2 |
| Received infant feeding counseling | 4 | 0 | 1 |
| Received family planning counseling | 4 | 1 | 1 |
| Received HIV prevention counseling | 4 | 3 | 1 |
Analytical methods
Recordings from the in-depth interviews were transcribed and translated by a Kenyan social scientist fluent in all three languages. Qualitative data from in-depth interview transcripts and observation notes were coded and analyzed using the Atlas.ti program (Muhr, 2004) using a thematic analysis approach (Braun & Clarke, 2006). Initial coding of the transcripts was conducted according to major topics from the interview guides, but new codes and themes were developed based on the data. Quotations, observations and memos regarding each topic were brought together and evaluated to identify common themes and variant views. Quantitative data from the observations were entered into a database and descriptive analyses were conducted. Measures to ensure validity of the interview findings included triangulation with the observation data and discussion of preliminary results with Kisumu maternity care workers.
Results
HIV/AIDS and decisions about where to deliver
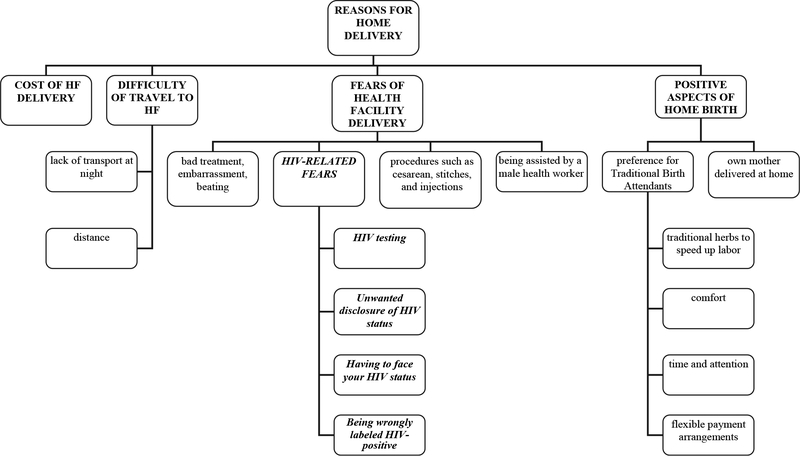
Before discussing HIV/AIDS, participants were asked why many women in Kisumu give birth at home. The main explanations fell under the major themes of: (1) costs of health facility delivery (almost always mentioned first and as the main factor); (2) difficulties traveling to the health facility; (3) positive aspects of home delivery; and (4) fears of health facility delivery (see Figure 1). Participants also talked about fears related to HIV as discouraging health facility delivery, including fears of being tested for HIV, fears of being wrongly labeled HIV-positive, fears of facing one’s HIV-positive status and fears of unwanted disclosure and resultant stigma. Fears of becoming infected with HIV while on the maternity ward did not emerge from the interviews.
Figure 1.
Diagram of reasons given for home delivery versus health facility (HF) delivery in in-depth interviews.
Fears of being tested for HIV during maternity care
Several participants described women’s fears of being forced to test for HIV or being tested without their consent. Many mentioned fear of the stress and shock that would come with an HIV-positive test result and explained that this stress could cause an HIV-positive person to become depressed, commit suicide or die sooner. Some participants suggested that women may wish to deny even the possibility that they could be HIV-positive since both partners are faithful. Others spoke about fears that they would get a “wrong” test result and be incorrectly labeled as HIV-positive. Participants explained how these fears may affect decisions regarding where to deliver in the following quotations:
“They think that if they go to the hospital at times they might be tested and turn out to be positive, so they fear that many people will know their status, so they opt to go to TBAs.”
(HIV-positive, postpartum woman, health center)
“Another thing that they say is that they are forced to admit that they are positive yet they know they are not. That makes them feel ashamed and fear going to the hospital because what they were told to do, they are not doing. So they come to me and say, ‘We were just put into a group and taken aside and they started counseling us telling us that we are positive, but I am not positive’. They say ‘I am annoyed and I can’t go there’.”
(Traditional birth attendant)
Fears of unwanted disclosure of HIV-positive status during maternity care
Participants explained that women often meet other people from their community (health workers and clients) at the maternity unit and described a lack of trust in confidentiality at health facilities that causes some women to choose to deliver at home.
Frequently emphasized was the impact of fears of unwanted disclosure of an HIV-positive result to a male partner and his negative reactions, such as shock, denial and problems in the marriage (quarrels, blame and accusations of promiscuity) that in some cases led to violence. Other participants described women’s fears of economic consequences for herself and her children, such as separation or divorce, abandonment, being “chased away” or “sent packing”, refusal to pay for delivery costs and refusal of economic support:
“There is a friend of mine who recently went for the test and was sent to go call the husband and the husband beat her up and broke her arm and asked why she went to be tested. He came to attack me saying that I am the one who advised her to go and test.”
(Pregnant woman, public hospital, HIV-positive)
Although, negative reactions of male partners were most often mentioned, several HIV-positive women described support from their partners, especially if both partners were HIV-positive.
Avoiding HIV testing/disclosure in maternity services
Strategies used to avoid HIV testing and unwanted disclosure included disposing of an ANC card with a HIV-positive test result and/or switching to another health facility, where the woman could decline to be tested. Women who can afford the cost might deliver at a private hospital where there is less pressure for testing. Another common strategy was to deliver at home with a TBA. As one TBA explained:
“You see some come with lies … Once she knows that she is positive she tears the card and she waits until she starts having labor pains. If her labor pains start in the morning she just keeps quiet because she does not want to go to the hospital … She waits until it is middle of the night … At midnight she knocks at my door … and the first thing that I ask for is the clinic card. ‘Where is your card?’ And she will say that she was at home and forgot the card there. She usually has a lot of fear.”
(Traditional birth attendant)
HIV/AIDS and provision of facility-based maternity services
Health administrators and workers noted some positive effects of HIV/AIDS on maternity service provision, such as new skills acquired at HIV/AIDS training programs and improved infection-control practices. More frequently noted were negative effects, including deaths and illness of maternity workers and increased workloads due to providing PMTCT services. Here we focus on the difficulties and fears health workers described caring for HIV-positive women and women with unknown HIV status.
Fears of HIV infection
Despite describing improved infection-control precautions, most of the maternity workers interviewed reported fears of contracting HIV at work:
“There is that fear that you may contract it. In case there is an accident, for instance in the operating theatre. It is just that you work with a lot of fear. The problem here is that you can get infected because of the nature of our work, but nobody will understand that you got it because something pricked you. People will only see the promiscuity in you.”
(Nurse, maternity unit, public hospital)
Access to post-exposure prophylaxis (PEP) for health workers was limited and differed by workplace; those working at the provincial hospital reported the easiest access, while those at the private hospital reported that they would have to go to another health facility and pay for PEP themselves.
Difficulties dealing with confidentiality and disclosure during maternity care
Many maternity workers discussed difficulties protecting patients’ confidentiality and knowing how – and to whom – to disclose patients’ HIV status. Workers described challenges to assuring privacy and confidentiality in crowded maternity units. Especially in the large hospitals, maternity units were so overcrowded that often two or more women had to share a bed. This situation made it difficult to provide PMTCT services to HIV-positive women without revealing their status to others in the unit.
Maternity workers spoke about HIV-positive women’s reluctance to disclose their status to their male partners and difficulties with responding to male partners’ negative reactions. Even when a pregnant woman specified that she did not want the husband to know her status, her husband might find out when he came to the maternity unit – by seeing the ARV drugs given to the baby, by learning about complications that occurred or because health workers told him directly. The workers recognized the importance of HIV counseling and testing for the male partner and felt frustrated when women and/or men did not cooperate:
“This problem of a mother being HIV-positive and the husband is not aware is a problem to us because it is really difficult to start telling the husband, ‘Your wife has come to deliver here and she is positive. We have given her medicine.’ It becomes difficult to explain … When she is asked she says, ‘My husband is not aware and I don’t want him to know.’ So it becomes difficult for us to explain to the husbands because if you say it maybe the husband can react, even might decide to leave her here.”
(Nurse, maternity unit, health center)
Differential treatment of HIV-positive women
Maternity workers had been trained to treat HIV-positive women the same as other patients and wanted to emphasize that there is no discrimination on their unit. No health workers reported segregating HIV-positive women, not providing medical care or any other directly discriminatory practices. Several workers did admit to handling a woman with “extra care” and being anxious if they know or suspect the woman is HIV-positive. Others suggested that discrimination related to HIV/AIDS status had occurred in the past or might still occur at other maternity hospitals, including behaviors such as fewer vaginal examinations (VEs) and avoidance or delays in performing necessary procedures. These things were described as happening especially in situations where sufficient gloves were not available:
“During my training, you found that people tended to fear. Like in the maternity, you would find that if a mother is HIV-positive, no one would want to be near, to help her deliver.”
(Nurse, private maternity hospital)
“You know this person is HIV-positive and you know that gloves are not a hundred percent protective and yet you are washing your hands literally in that blood. It is not safe. I would imagine that even the number of VEs would be controlled just by the fear; the sheer fact that that person is HIV-positive.”
(Physician-administrator, public hospital)
Treatment of women with unknown HIV status during labor and delivery
Participants explained that the HIV status of some delivering women is unknown. These are women who either have had no ANC, refused testing during ANC or have not brought their ANC card. If the women’s labor is not too advanced, she is offered HIV testing. However, many women arrive in advanced second stage labor. Women with unknown HIV status appeared to cause health workers considerable anxiety. Some health workers were convinced that women who declined HIV testing knew they were HIV-positive and were concealing their status. A few maternity workers talked about conducting Diagnostic Testing and Counseling (DTC) without the women’s consent:
“What we’ve realized is that some of them do know their status. So when they come to our clinic they are like, ‘No. I’ll decide. I don’t want [an HIV test].’ But they know their status. We confirmed this. We did this on three mothers. We did DTC. Where now we take the blood and we test without really going through the other procedures and we realized they were positive so it was like they knew their status but they didn’t want us to know about it.”
(Nurse, maternity unit, public hospital)
The observations on the maternity wards provided additional insights into conditions and treatment of women with unknown HIV status. Of the five women of unknown status observed during labor and delivery (total n = 22), three were ≤18 years of age, one had no ANC (the only one among the women observed), four were admitted in advanced second stage labor and two experienced serious complications (one resulting in maternal death and the other in infant death). Observations on the postpartum ward revealed that most women with unknown status received no counseling on infant feeding, family planning or HIV prevention, whereas most HIV-positive women did (See Table 2).
Discussion
Results of this study indicate that the effects of HIV/AIDS on maternity services in high-HIV-prevalence settings merit more attention. It appears that fears about HIV/AIDS held by both clients and health workers adversely affect both uptake of facility-based labor and delivery services and the quality of care provided on maternity units.
Our findings suggest that fears of HIV/AIDS testing and disclosure have now been added to the list of factors that discourage health facility delivery. A recent study in a district near Kisumu found that the primary barriers to health facility delivery were long distances to health facilities, lack of transport, poor quality of care and financial constraints (Family Care International & Blancroft Research International LLC, 2005). These same factors also discourage health facility delivery in Kisumu, but our findings suggest that fears related to HIV/AIDS also play a role. In order to improve maternal and infant health in settings where skilled delivery attendance is low, all contributing factors need to be recognized and addressed.
Maternity workers also suffer from fears of HIV/AIDS stigma and discrimination and this adversely affects their working conditions and the care they give patients. Although infection control practices and use of universal precautions have improved, Kenyan maternity workers sometimes lack adequate infection control supplies and may not have access to PEP (National Coordinating Agency for Population and Development [Kenya], Ministry of Health [Kenya], Central Bureau of Statistics [Kenya], & ORC Macro, 2005). Thus, they do not feel fully protected. They see contracting HIV as a double injury – not only the physical effects of the disease, but also being labeled as promiscuous. It is not surprising that maternity workers suffer from similar fears of HIV/AIDS stigma and discrimination as their clients, as they are all part of the same community.
Lack of confidentiality on the maternity unit was identified as an important problem. As word of mouth about this situation circulates, it affects not only the quality of care, but also discourages some women from ever using the services. Maintaining confidentiality is not only related to inadequate private space, but also to different cultural norms about individual rights and confidentiality (Airhihenbuwa, 2007). Although in the West it is accepted that a patient’s medical information is confidential and would not be shared without the patient’s consent, the interviews conducted for this study suggested that many health workers find it inconceivable that a husband would not be informed of his wife’s HIV status. Because a pregnant woman is often the first person to be tested in a family due to her contact with the ANC clinic, she is particularly vulnerable to potential adverse consequences of disclosure (Mathole, Lindmark, & Ahlberg, 2006; Medley, Garcia-Moreno, McGill, & Maman, 2004).
An important finding of this study is that the biggest risks may be faced by pregnant women of unknown HIV status and those who are afraid of the consequences of disclosing their HIV-positive status to health workers. Despite the fact that these women may have many obstetric high risk factors, such as young age and no ANC, they may avoid delivering in health facilities because of their HIV-related fears. If they do go to health facilities for delivery, they may be treated poorly and may even be tested for HIV or have their HIV status disclosed without their consent. Maternity workers in this setting experienced discomfort and anxiety caring for women whose HIV status was unknown, as was also found in a study in Zimbabwe (Mathole, Lindmark, & Ahlberg, 2006).
The practice of HIV testing without consent reflects maternity workers’ frustration with a situation where they want to protect themselves and others from infection but do not feel that they have the necessary information to do so. Although the adoption of routine “opt-out” testing in maternity services may solve some of these problems for health workers, the implications of this strategy for women (including stigma and spousal violence) and potential effects on their use of maternity services need to be examined (Perez, Zvandaziva, Engelsmann, & Dabis, 2006).
Importantly, it appears that women of unknown HIV status, who could be either HIV-positive or at risk of becoming infected with HIV, may not receive needed information, counseling and services. We observed that HIV-positive women who have disclosed their status to maternity workers – and thus are seen as being cooperative – were more likely to benefit from skilled delivery attendance and receive better treatment on maternity units than women of unknown HIV status.
This study has certain limitations. First, because study recruitment was conducted through health facilities, we were not able to learn directly about the experiences of women who never utilize health facilities. This fact, combined with the stigma associated with HIV/AIDS, meant that participants talked more about how HIV/AIDS discourages other women in their community from using maternity services, rather than their personal experiences. However, a few women who gave birth at home but used post-natal services, as well as two TBAs, were included in the in-depth interviews. Second, only a small number of interviews were conducted with male partners due to the difficulties faced finding and recruiting them through maternity services. Third, there were few structured observations and health workers may have changed their behavior because they were being observed. Lastly, Kisumu may be different than other places in sub-Saharan Africa. Due to the high HIV prevalence, Kisumu has become an important center for HIV/AIDS research, education and services and maternity workers in Kisumu may have more experience with and sensitivity to this topic than those elsewhere.
Findings of this exploratory study suggest a need to develop interventions to address the concerns noted. Certainly, further improvements should be made in the availability of infection control supplies and training in universal precautions for maternity units. However, our findings suggest that this will not solve the problems with unwanted disclosure, confidentiality and stigma. Maternity workers need enhanced culturally sensitive training on confidentiality, disclosure and helping women to deal with positive test results, as well as space in which to provide confidential services. Interventions to reduce stigma and discrimination experienced by HIV-positive pregnant women and maternity workers are also needed. Lastly, this study points to the need to pay more attention to the needs of women of unknown HIV serostatus in maternity services, especially provision of culturally sensitive and confidential HIV testing services and helpful counseling and support for those who decline testing. It is possible that such interventions could increase utilization of skilled delivery services and contribute to overall improvements in maternal health, while also contributing to PMTCT and HIV care for women and their families.
Acknowledgements
We thank the Kenyan women and men who participated in the study and shared their experiences with us. We acknowledge the important logistical support of the KEM-RI-UCSF Collaborative Group and especially Kisumu FACES. We thank Gaudencia Mittow, Douglas Okelloh and Maria Jarkowiec for their diligent work in collecting and processing the data. We gratefully acknowledge Dr. Koech, the Director of KEMRI and Dr. Wamae, the Director of KEMRI’s Centre for Microbiology, for their support in conducting this research. Training related to this study was carried out with financial assistance from the UC Berkeley/UCSF AIDS International Training and Research Program (Fogarty AITRP # 1 D43 TW00003). Janet Molzan Turan’s work on this article was also supported, in part, by grant # T32 MH-19105–17 from the US National Institute of Mental Health.
Footnotes
Publisher's Disclaimer: The publisher does not give any warranty express or implied or make any representation that the contents will be complete or accurate or up to date. The accuracy of any instructions, formulae and drug doses should be independently verified with primary sources. The publisher shall not be liable for any loss, actions, claims, proceedings, demand or costs or damages whatsoever or howsoever caused arising directly or indirectly in connection with or arising out of the use of this material.
References
- Airhihenbuwa CO (2007). On being comfortable with being uncomfortable: Centering an Africanist vision in our gateway to global health. Health Education and Behavior, 34, 31–42. [DOI] [PubMed] [Google Scholar]
- Bain Brickley D, Hahn DLD, Nguyet LT, Giang LT, & Sohn A (2006). Qualitative study of the challenges to seeking health care among HIV-positive pregnant women in Ho Chi Minh City. Paper presented at the XVI International AIDS Conference, Toronto, Canada. [Google Scholar]
- Bond V, Chase E, & Aggleton P (2002). Stigma, HIV/AIDS and prevention of mother-to-child transmission in Zambia. Evaluation and Program Planning, 25, 347–356. [Google Scholar]
- Braun V, & Clarke V (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101. [Google Scholar]
- Central Bureau of Statistics (Kenya), Ministry of Health (Kenya), & ORC Macro. (2004). Kenya demographic and health survey 2003. Calverton, MD: Author. [Google Scholar]
- Dovlo D (2005). Wastage in the health workforce: Some perspectives from African countries. Human Resources for Health, 3, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etiebet MA, Fransman D, Forsyth B, Coetzee N, & Hussey G (2004). Integrating prevention of mother-to-child HIV transmission into antenatal care: Learning from the experiences of women in South Africa. AIDS Care, 16, 37–46. [DOI] [PubMed] [Google Scholar]
- Family Care International & Blancroft Research International LLC. (2005). Patterns in seeking skilled care at delivery: Household survey findings from Burkina Faso, Kenya, and Tanzania. New York: FCI, The Skilled Care Initiative. [Google Scholar]
- Gerein N, Green A, & Pearson S (2006). The implications of shortages of health professionals for maternal health in sub-saharan Africa. Reproductive Health Matters, 14, 40–50. [DOI] [PubMed] [Google Scholar]
- Graham W, & Hussein J (2003). Measuring and estimating maternal mortality in the era of HIV/AIDS (No. UN/POP/MORT/2003/8). New York: Population Division, Department of Economic and Social Affairs, United Nations Secretariat. [Google Scholar]
- Gray GE, & McIntyre JA (2007). HIV and pregnancy. British Medical Journal, 334, 950–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathole T, Lindmark G, & Ahlberg BM (2006). Knowing but not knowing: Providing maternity care in the context of HIV/AIDS in rural Zimbabwe. African Journal of AIDS Research, 5, 133–139. [DOI] [PubMed] [Google Scholar]
- McIntyre J (2003). Mothers infected with HIV. British Medical Bulletin, 67, 127–135. [DOI] [PubMed] [Google Scholar]
- Medley A, Garcia-Moreno C, McGill S, & Maman S (2004). Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: Implications for prevention of mother-to-child transmission programmes. Bulletin of the World Health Organization, 82, 299–307. [PMC free article] [PubMed] [Google Scholar]
- Misiri HE, Tadesse E, & Muula AS (2004). Are public antenatal clinics in Blantyre, Malawi, ready to offer services for the prevention of vertical transmission of HIV? African Journal of Reproductive Health, 8, 64–70. [PubMed] [Google Scholar]
- Muhr T (2004). Atlas-ti (Version 5.2.9). Berlin, Germany: Atlas-ti Scientific Software Development GmbH. [Google Scholar]
- National AIDS and STI Control Programme of the Ministry of Health (Kenya). (2005). AIDS in Kenya (7th ed). Nairobi, Kenya: NASCOP. [Google Scholar]
- National Coordinating Agency for Population and Development (Kenya), Ministry of Health [Kenya], Central Bureau of Statistics (Kenya), & ORC Macro. (2005). Kenya service provision assessment survey 2004. Nairobi, Kenya: Author. [Google Scholar]
- Ortega NL, Bicaldo BF, Sobritchea C, & Tan ML (2005). Exploring the realities of HIV/AIDS-related discrimination in Manila, Philippines. AIDS Care, 17(Suppl. 2), S153–S164. [DOI] [PubMed] [Google Scholar]
- Perez F, Zvandaziva C, Engelsmann B, & Dabis F (2006). Acceptability of routine HIV testing (“opt-out”) in antenatal services in two rural districts of Zimbabwe. Journal of Acquired Immune Deficiency Syndromes, 41, 514–520. [DOI] [PubMed] [Google Scholar]
- PlusNews. (2006). Uganda: HIV-positive women stigmatized by major hospital [Electronic Version]. IRIN PlusNews, 2007. Retrieved March 31, 2007 from http://www.plusnews.org/Report.aspx?ReportId=39465 [Google Scholar]
- Reidpath DD, & Chan KY (2005). HIV discrimination: Integrating the results from a six-country situational analysis in the Asia Pacific. AIDS Care, 17(Suppl. 2), S195–S204. [DOI] [PubMed] [Google Scholar]
- Reis C, Heisler M, Amowitz LL, Moreland RS, Mafeni JO, Anyamele C, et al. (2005). Discriminatory attitudes and practices by health workers toward patients with HIV/AIDS in Nigeria . PLoS Medicine, 2, e246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. (2005). The female AIDS epidemic: 2005. Geneva, Switzerland: UNAIDS, Global Coalition on Women and AIDS. [Google Scholar]
- Van’t Hoog AH, Mbori-Ngacha DA, Marum LH, Otieno JA, Misore AO, Nganga LW, et al. (2005). Preventing mother-to-child transmission of HIV in western Kenya: Operational issues. Journal of Acquired Immune Deficiency Syndromes, 40, 344–349. [DOI] [PubMed] [Google Scholar]
- WHO. (2005). Word health report 2005: Make every mother and child count. Geneva, Switzerland: Author. [Google Scholar]
- WHO, UNICEF, & UNFPA. (2004). Maternal mortality in 2000: Estimates developed by WHO, UNICEF and UNFPA. Geneva, Switzerland: Author. [Google Scholar]