Abstract
Background:
Little is known about the relative harms of edible and inhalable cannabis products.
Objective:
To describe and compare adult emergency department (ED) visits related to edible and inhaled cannabis exposure.
Design:
Chart review of ED visits between 1 January 2012 and 31 December 2016.
Setting:
A large urban academic hospital in Colorado.
Participants:
Adults with ED visits with a cannabis-related International Classification of Diseases, Ninth or 10th Revision, Clinical Modification (ICD-9-CM or ICD-10-CM), code.
Measurements:
Patient demographic characteristics, route of exposure, dose, symptoms, length of stay, disposition, discharge diagnoses, and attribution of visit to cannabis.
Results:
There were 9973 visits with an ICD-9-CM or ICD-10-CM code for cannabis use. Of these, 2567 (25.7%) visits were at least partially attributable to cannabis, and 238 of those (9.3%) were related to edible cannabis. Visits attributable to inhaled cannabis were more likely to be for cannabinoid hyperemesis syndrome (18.0% vs. 8.4%), and visits attributable to edible cannabis were more likely to be due to acute psychiatric symptoms (18.0% vs. 10.9%), intoxication (48% vs. 28%), and cardiovascular symptoms (8.0% vs. 3.1%). Edible products accounted for 10.7% of cannabis-attributable visits between 2014 and 2016 but represented only 0.32% of total cannabis sales in Colorado (in kilograms of tetrahydrocannabinol) during that period.
Limitation:
Retrospective study design, single academic center, self-reported exposure data, and limited availability of dose data.
Conclusion:
Visits attributable to inhaled cannabis are more frequent than those attributable to edible cannabis, although the latter is associated with more acute psychiatric visits and more ED visits than expected.
Primary Funding Source:
Colorado Department of Public Health and Environment.
Colorado saw an increase in cannabis use after liberalization of medical cannabis in 2009 (1) and recreational cannabis in 2014 (2). Increased availability and use of cannabis in Colorado has led to an increase in emergency department (ED) visits associated with the drug (3). In 2014, the Marijuana Enforcement Division began collecting and reporting data on cannabis product sales. Cannabis is most often purchased in flower form for smoking; edible cannabis accounts for only 0.3% of the weight of tetrahydrocannabinol (THC) in total cannabis product sales (4). According to the Colorado Behavioral Risk Factor Surveillance System, 40.4% of marijuana users report smoking cannabis only, whereas 3.6% report using edible cannabis products only (5). The remainder use a combination of the products.
Despite edible cannabis products accounting for a small proportion of the total number of cannabis products sold and used, they frequently contribute to ED visits and may be more toxic than inhalable products. This is supported by increasing numbers of adverse events associated with edible cannabis being reported to poison centers (6), as well as troubling anecdotes of users (7–9). In Colorado, the only deaths definitively associated with cannabis use involved edible products (10–12), which also supports increased toxicity with this route of exposure. However, whether these anecdotal reports by adult users (9) and limited poison center data (13) truly show increased toxicity of edible cannabis compared with inhalable cannabis is unclear. The objective of this study was to describe and compare adult ED visits associated with edible and inhalable cannabis products.
METHODS
Study Design and Population
This was a retrospective observational study based on chart review of patients presenting to the UCHealth University of Colorado Hospital Emergency Department (UCHED). The UCHED serves an urban academic hospital with approximately 100 000 visits per year. More than 97% of patients seen in the UCHED are aged 18 years or older.
All UCHED visits from 1 January 2012 through 31 December 2016 were eligible for inclusion. Visits that contained an International Classification of Diseases, Ninth or 10th Revision, Clinical Modification (ICD-9-CM or ICD-10-CM), code consistent with cannabis exposure were manually reviewed to collect variables of interest (Appendix Table, available at Annals.org). The study protocol was approved by the local institutional review board.
Study Participants and Coding
Adults with an ED visit containing a cannabis-related ICD-9-CM or ICD-10-CM code were included. Assessment of cannabis use is included in the drug use section of the standard nursing assessment questionnaire administered to patients seen at the UCHED and in the clinical notes of the medical providers. A visit was considered at least partially attributable to cannabis if 1 or more of the following criteria were met: 1) the ED provider identified cannabis as likely precipitating or contributing to the condition, 2) the patient was admitted to the hospital and the inpatient provider identified cannabis as likely precipitating or contributing to the condition, or 3) the urine toxicologic screening result was positive and there was a documented temporal relationship (within approximately 24 hours) with cannabis exposure and there was a condition or an event known to be associated with cannabis use (for example, motor vehicle collision or acute panic attack). Patients were considered pregnant if they had a positive urine pregnancy test result or on the basis of clinician note review when no pregnancy test was performed.
Measurements
Visits to the UCHED with cannabis-related ICD-9-CM or ICD-10-CM codes were manually abstracted by 4 trained research assistants who were blinded to the study hypothesis. Research assistants coded whether the visit was at least partially attributable to cannabis, the route of exposure, the dose (when available), the clinical symptoms, and the presenting symptoms. Clinical and presenting symptoms were not mutually exclusive. When the route of exposure was not documented, it was assumed to be inhalation because this is the most common route of exposure in Colorado (5).
The research assistants were trained in chart abstraction using 50 UCHED charts with cannabis-related ICD-9-CM and ICD-10-CM codes selected from the study period. Charts were abstracted by a medical toxicologist and one of the research assistants. Discrepancies in coding were determined with regard to attribution of the visit to cannabis, clinical symptoms, route of exposure, and reported dose. The research assistants were retrained on discrepancies, and an additional 250 charts were then reviewed by the medical toxicologist to determine accuracy. The medical toxicologist abstracted a random sample of 10% of all charts reviewed by the research assistants, and the [H9260] statistic was calculated to determine interrater reliability. Double abstraction was performed on 1111 visits in the ICD code-generated data set. Visits with questionable attribution to cannabis were arbitrated by the medical toxicologist. A sensitivity analysis was performed using 1% of all UCHED charts to ensure adequate capture of cannabis-related visits using the ICD-9-CM and ICD-10-CM code search strategy.
Statistical Analysis
Descriptive statistics were used to characterize categorical variables in the overall population and in the subpopulations with cannabis-attributable and edible cannabis–attributable visits. Differences among the groups were evaluated using a [H9273]2 test. Absolute differences in clinical symptoms (with 95% CIs) were calculated as the percentage in the edible group minus the percentage in the inhalable group. Length of stay was summarized in both groups. Data analysis was performed using SAS, version 9.4 (SAS Institute).
We also compared the proportions of cannabis-attributable visits by route of exposure (edible vs. inhalable) with the corresponding proportions of cannabis sales in the state. For this analysis, we summarized cannabis product sales data for Colorado and converted to kilograms of THC. We assumed THC content of 20% per kilogram of flower sold for inhalable cannabis and 10 mg of THC for each unit sold for edible cannabis. Assuming a 1:9 ratio for edible versus inhaled exposures, we calculated that a sample size of 2000 would provide enough data to reliably estimate a 5-fold increased rate of ED visits for edible versus inhaled exposure.
Role of the Funding Source
The Colorado Department of Public Health and Environment (CDPHE) funded this study through a competitive grant program. The CDPHE was not involved in study design, analysis, data interpretation, or dissemination of these findings.
RESULTS
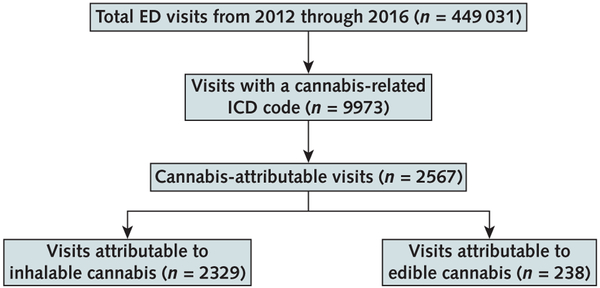
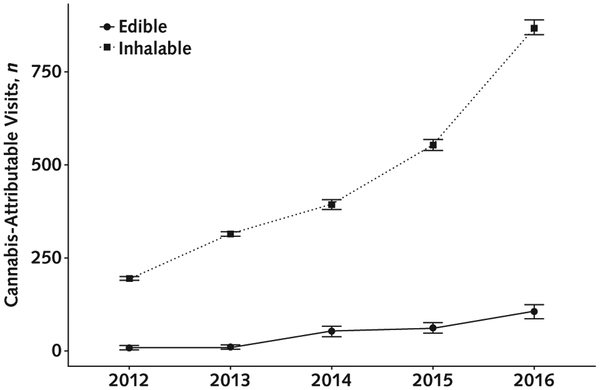
There were 449 031 eligible visits to the UCHED during the study period. Cannabis-related ICD-9-CM or ICD-10-CM codes were present in 9973 visits (Table 1), and 2567 visits (25.7%) were deemed at least partially attributable to cannabis. Among these, the route of exposure was available in 2432 (94.7%). Edible ingestion was reported in 238 visits (9.3%), and exposure in the remainder was considered to be via inhalation (2194 were documented as such, and 135 had insufficient documentation) (Figure 1). The frequency of visits attributable to inhalable and edible cannabis increased each year during the study period (Figure 2). The dose was available in only 130 records (5.1%). Pregnant women accounted for fewer than 2% of patients with a cannabis-attributable visit (n = 46).
Table 1.
Patient Demographic Characteristics*
| Characteristic | All ED Visits (n = 449 031)† | ED Visits With Cannabis-Related ICD Code (n = 9973) | Cannabis-Attributable ED Visits (n = 2567) |
|---|---|---|---|
| Median age (IQR), y | 39(27–54) | 36 (27–48) | 30(24–41) |
| Gender | |||
| Male | 195 485(43.5) | 6247 (62.6) | 1674(65.2) |
| Female | 253 511 (56.5) | 3725 (37.4) | 893 (34.8) |
| Unknown | 35(0.01) | 1 (0) | 0(0) |
| Race | |||
| American Indian/Alaska Native | 2685(0.6) | 65 (0.7) | 9 (0.4) |
| Asian | 12 487 (2.8) | 70 (0.7) | 31 (1.2) |
| Black | 124 462 (27.7) | 3408 (34.2) | 939 (36.6) |
| Multiple | 769(0.17) | 8 (0.08) | 0 (0) |
| Native Hawaiian/other Pacific Islander | 1190(0.27) | 16(0.2) | 4 (0.2) |
| Other | 100 588(22.4) | 1577 (15.8) | 455(17.7) |
| White | 204 249(45.5) | 4778 (47.9) | 1115 (43.4) |
| Missing | 2601 (0.58) | 51 (0.5) | 14 (0.6) |
| Ethnicity | |||
| Hispanic | 100 339(22.4) | 1622 (16.3) | 457 (17.8) |
| Non-Hispanic | 346 422 (77.2) | 8318(83.4) | 2101 (81.9) |
| Missing | 2270(0.5) | 33 (0.33) | 9 (0.35) |
| State of residence | |||
| Colorado | 427 245(95.2) | 9418(94.4) | 2315(90.2) |
| Other | 21 786(4.9) | 555 (5.6) | 252 (9.8) |
| Disposition | |||
| Admitted | 71 537 (15.9) | 4315(43.3) | 810(31.6) |
| Observed in ED | 1790(0.4) | 65 (0.65) | 19(0.74) |
| Died | 393 (0.09) | 0 (0) | 0 (0) |
| Discharged | 358 686(79.9) | 5160(51.7) | 1605(62.5) |
| Admitted to intensive care unit | 11 (0) | 2 (0.02) | 0 (0) |
| Left against medical advice | 1551 (0.4) | 50 (0.50) | 6 (0.23) |
| Left without being seen | 8035(1.8) | 91 (0.91) | 29(1.13) |
| Other | 2779(0.6) | 98 (0.98) | 44(1.71) |
| Transferred to different hospital | 2969 (0.7) | 0 (0) | 0 (0) |
| Transferred to psychiatric facility | 1280(0.3) | 192 (1.93) | 54(2.10) |
| Insurance | |||
| Indigent | 118 059(26.3) | 1719(17.2) | 451 (17.6) |
| Medicaid | 159 674(35.6) | 4225 (48.6) | 1190(50.6) |
| Medicare | 72 832 (16.2) | 1683(19.4) | 361 (15.4) |
| Other | 94 852 (21.1) | 2192 (25.2) | 507 (21.6) |
| Veterans Affairs | 3614(0.8) | 154(1.8) | 58 (2.5) |
ED = emergency department; ICD = International Classification of Diseases; IQR = interquartile range.
Data are numbers (percentages) unless otherwise indicated.
Three visits were missing data on age.
Figure 1. Flow chart of visit selection and review.
ED = emergency department; ICD = International Classification of Diseases.
Figure 2. Exposure to edible and inhalable cannabis products in cannabis-attributable visits at UCHED from 2012 to 2016.
Error bars indicate 95% CIs. UCHED = UCHealth University of Colorado Hospital Emergency Department.
Reasons for Cannabis-Attributable ED Visits
Gastrointestinal symptoms, including cannabinoid hyperemesis syndrome, were the most common reason among patients with cannabis-attributable visits (n = 788 [30.7%]). Specifically, 301 patients presented for 440 visits due to cannabinoid hyperemesis syndrome (range, 1 to 17 visits per patient per year). Intoxication was the second most common reason (n = 762 [29.7%]). Psychiatric symptoms were the third most common (n = 633 [24.7%]); of these, 297 (46.9%) were for acute psychiatric symptoms, such as acute anxiety or acute psychosis; 94 (14.1%) were for acute exacerbations of underlying chronic disease; and 100 (15.8%) were for chronic psychiatric conditions, such as depression, schizophrenia, or psychosis (Table 2).
Table 2.
Most Common Clinical Conditions Associated With Cannabis-Attributable Visits, by Route of Exposure
| Condition | Edible Exposure (n = 238), n (%) | Inhalable Exposure (n = 2329), n (%) | Absolute Difference (Edible — Inhalable) (95% CI), percentage points | Total Visits, n (%) |
|---|---|---|---|---|
| Gastrointestinal symptoms | 36(15.1) | 752 (32.3) | −17.2 (−12.2 to −22.1) | 788 (30.7) |
| Cannabinoid hyperemesis syndrome | 20 (8.4) | 420(18.0) | −9.6 (−5.7 to −13.5) | 440 (17.1) |
| Intoxication | 115(48.3) | 647 (27.8) | 20.5 (13.9 to 27.1) | 762 (29.7) |
| Psychiatric symptoms | 62 (26.1) | 571 (24.5) | 1.6 (−4.2 to 7.4) | 633 (24.7) |
| Acute psychiatric symptoms | 43(18.0) | 254(10.9) | 7.1 (2.1 to 12.1) | 297 (46.9) |
| Acute exacerbation of underlying chronic disease | 1 (0.4) | 93 (4.0) | −3.6 (−2.5 to −4.7) | 94(14.1) |
| Chronic psychiatric condition | 1 (0.4) | 99 (4.3) | −3.9 (−2.8 to −5.0) | 100 (15.8) |
| Cardiovascular symptoms | 19(8.0) | 73(3.1) | 4.9 (1.4 to 8.4) | 92 (3.6) |
Comparison of Visits Attributable to Inhalable Versus Edible Cannabis
Patients with visits attributed to edible cannabis were similar in age to those with visits attributed to inhalable cannabis; however, they were more likely to be female (51.3% vs. 33.1%; P < 0.001), more likely to live outside Colorado (40.8% vs. 6.6%; P < 0.001), and less likely to be admitted to the hospital (18.9% vs. 32.9%; P < 0.001). Length of stay was longer for visits attributable to inhalable cannabis (median, 3 hours [range, 0 to 121 hours] vs. 2 hours [range, 1 to 54 hours]).
Clinical symptoms for cannabis-attributable visits varied between the inhaled and edible exposure groups. Gastrointestinal symptoms were more common in patients exposed to inhalable compared with edible cannabis; 18.0% versus 8.4% had cannabinoid hyperemesis syndrome (mean difference, 9.6 percentage points [95% CI, 5.7 to 13.5 percentage points]; P < 0.001). Although there was no difference in the frequency of overall psychiatric-related visits between groups, visits related to acute psychiatric symptoms were more common in patients with edible exposures (18.0% vs. 10.9%; mean difference, 7.1 percentage points [CI, 2.1 to 12.1 percentage points]; P < 0.001). Visits due to cardiovascular symptoms were also more common in patients exposed to edible products (8.0% vs. 3.1%; P < 0.001). Severe adverse cardiovascular events, including myocardial infarction and ventricular dysrhythmia, occurred in both groups.
Chart Review Sensitivity and Interrater Reliability
We reviewed 4800 random ED records from the 449 031 overall visits from the study period. During 2012 to 2014, there were no records containing a mention of cannabis that were not included in our ICD-9-CM–generated data set. In 2015 and 2016, there were 26 records with a mention of cannabis exposure that were not captured by our search criteria (0.01% of total records). These charts were all in the subset of visits in which ICD-10-CM codes were used and represented polypharmacy ingestion cases with no identified temporal relationship with cannabis use and no urine toxicologic screening. The cannabis references were medical shorthand notation (for example, “+cann” or “+pot”) identified in consulting physician notes, and the exposure was not documented by the primary medical team caring for the patient. None of these cases were considered cannabis-attributable by our definition. The interrater reliability for abstracted data was good ([H9260] = 0.79 [CI, 0.75 to 0.83]).
Colorado Sales Data by Route of Exposure
Sales data showed that the unadjusted quantity of THC sold as both inhalable products and edible products increased between 2014 and 2016 in Colorado (Table 3). There was 309 times more THC sold in flower form, the primary product sold for inhalation, compared with edible products (range, 279 to 325) over this period. During the same period, 219 ED visits were attributable to edible exposure and 1819 to inhaled exposure. Thus, an estimated 10.7% of cannabis-attributable ED visits between 2014 and 2016 were due to edible cannabis.
Table 3.
Cannabis Product Sales Reported to the Colorado Marijuana Enforcement Division in the Recreational Cannabis Period
| Year | Sales ofInhalable Cannabis Products | Sales of Edible Cannabis Products | Inhalable-Edible Ratio (THC Content) | ||
|---|---|---|---|---|---|
| Flower, kg | THC Content, kg* | Units | THC Content, kg† | ||
| 2014 | 67 239 | 13 448 | 4.8 × 106 | 48 | 279 |
| 2015 | 108 507 | 21 701 | 7.0 × 106 | 70 | 310 |
| 2016 | 152 244 | 30 449 | 9.4 × 106 | 94 | 325 |
| Total | 327 990 | 65 598 | 21.2 × 106 | 212 | 309 |
THC = tetrahydrocannabinol.
Based on THC content of 20% per kilogram sold.
Based on 10 mg per unit sold.
DISCUSSION
This study involving nearly 10 000 cannabis-related ED visits with manual reconciliation of the role cannabis played in each visit showed that, although less frequent overall, edible products lead to more acute psychiatric events and cardiovascular symptoms than inhaled exposure. The high frequency of visits and the greater likelihood of hospital admission associated with inhalable products suggest that user education about the adverse health effects of inhalable cannabis may have the greatest effect on public health.
A PubMed literature search using the terms cannabis edible OR cannabis emergency on 8 November 2018 found 446 articles. In addition, we examined the systematic literature review report of the CDPHE’s Retail Marijuana Public Health Advisory Committee, which is updated quarterly, on 22 October 2018. These articles suggest that ED visits associated with cannabis use are increasing (3, 14). Edible products are a major source of unintentional cannabis exposures in children, but the differences in health care visits associated with edible versus inhalable cannabis in adults have not been systematically examined (15–17). It has become clear that cannabis is associated with acute psychiatric illness (18–20), and this has led to more ED visits that are at least partially attributable to cannabis, although these studies did not stratify visits by route of exposure. Similarly, a study that examined the National Inpatient Sample found that admissions associated with cannabis had a high proportion of psychiatric and cardiovascular symptoms, although these visits also were not stratified by route of exposure (21).
The kinetics of absorption, onset, and duration of action of edible products may be well suited for medical indications but are not ideal for recreational use, in which the user hopes to feel the effects rapidly. Inhalable cannabis results in clinical effects within 10 minutes, peak blood concentrations occur within 30 to 90 minutes, and clearance is complete within 4 hours. Oral THC does not reach significant blood concentration until at least 30 minutes, with a peak at approximately 3 hours and clearance approximately 12 hours after ingestion (22). Users report longer-lasting effects with edible products than with smoking or vaping (8); they also report more intense effects and unpleasant psychiatric symptoms (9). These factors may lead to more severe clinical manifestations; death has been associated with use of edible products, as in the cases of a man who jumped from a balcony after consuming an edible product (11), a woman who was killed by her husband after he ingested an edible product (10), and a man who died by suicide at a ski resort after eating an edible product (12).
Hospital admission was more common in the cohort with visits attributable to inhalable cannabis. This seemed to be driven by admission of patients with cannabinoid hyperemesis syndrome, which is far more common among patients with inhaled exposure. The larger proportion of acute psychiatric visits associated with edible exposure is troubling given the capacity of THC to cause or exacerbate psychosis (20, 23–25) and the risk for violent behaviors linked to cannabis-associated psychosis (26, 27). The association of cardiovascular visits with edible exposure is also concerning. Cannabis is now recognized as a risk factor for adverse cardiovascular events (28, 29), and the increased rate of visits associated with edible products seems to have translated to a higher proportion of cardiovascular events in such visits.
Other studies using public health data (30), administrative hospital data sets (19), poison center data (15, 17), and retrospective designs (31, 32) have shown increased ED visits associated with cannabis use. These studies did not use chart review to assess validity of diagnoses or symptoms. Despite its strengths, our study has several important limitations. It used a retrospective design with exposure data captured largely through self-report. There was no comparative community-based exposure cohort. Patients presenting to the ED clearly differ from the overall population of cannabis users, most of whom may use cannabis with no adverse effects. A prospective cohort of users and nonusers is necessary to determine the true rates of cannabis-attributable visits in the user population. We could not verify doses, and ingested doses may have been larger than inhaled doses. However, the dose was documented in 80 visits attributable to edible exposure, and only 19 were 50 mg or higher. We were surprised by the low dose of edible products reported by these patients considering that a typical joint in Colorado contains approximately 100 mg of THC. In addition, route of exposure was captured from the medical record and was presumed to be inhalation when it was not documented. This could have biased the analyses toward greater toxicity in the cohort with inhaled exposure, which further emphasizes our finding that edible products have greater toxicity per unit of cannabis sold. Finally, the UCHED has the second most visits per year in the state and is located in an area with high cannabis availability. These factors likely increase the rates of cannabis-attributable ED visits at this hospital.
Our data suggest an interesting relationship between route of cannabis exposure and ED visits. Although edible cannabis accounted for only 0.32% of total cannabis sales (in kilograms of THC) from 2014 to 2016, 10.7% of cannabis-attributable visits at the UCHED in this period were due to edible cannabis. If inhalable and edible cannabis were equally toxic and resulted in the same number of ED visits, we would expect that 0.3% of cannabis-attributable visits would be due to use of edible products. The observed proportion of cannabis-attributable visits with edible exposure was about 33 times higher than expected (10.7% vs. 0.32%) if both routes of exposure were equally toxic. However, there are limitations in using state-level sales data to infer ED visit rates, and careful interpretation of the results is required. First, we made assumptions about the THC content of the flower and edible products based on the average known THC concentration in Colorado products. Furthermore, we compared chart data from a single hospital with state-level sales data. Our comparisons could not account for cannabis that is cultivated at home or obtained through the black market. However, these methods of procurement are believed to be minor compared with the retail marketplace in Colorado. More than 50% of Colorado cannabis dispensaries are in the Denver metropolitan area, but sales data are not geocoded in Colorado. Geocoding may be beneficial for other regions wishing to examine associations of products and clinical illness.
The increased number of visits attributable to edible products among visitors to Colorado suggests that naive users or tourists are at greater risk. There are many reasons for increased rates of adverse drug events, including inconsistent dosing (33), dose stacking (13), pharmacodynamic variability between routes of exposure (34), unintentional exposure (17), and user naiveness (7, 35). These findings should be considered carefully in states considering legalization of recreational cannabis. Some have argued for stricter state regulations on edible products, with pediatric exposures as the primary supporting evidence (36). It may be best to limit edible products to medical indications in order to minimize pediatric exposures and mitigate the excessive rate of adult ED visits associated with these products. At the very least, users must be educated about the delayed kinetic profile and the increased risk for acute psychiatric and adverse cardiovascular events associated with edible ingestion. As suggested by the American College of Clinical Pharmacology (37), the U.S. Food and Drug Administration should strongly consider increased oversight of these products in order to standardize packaging, dosing, warnings, and user education. Minimization of heavy cannabis use may lead to fewer ED visits and hospital admissions related to cannabinoid hyperemesis syndrome. Education of users about the adverse health effects of cannabis use may have the greatest effect on public health.
In conclusion, inhalable cannabis results in a higher frequency of cannabis-attributable ED visits, although acute psychiatric events and cardiovascular symptoms are more common with edible exposure. Future studies that examine cannabis-attributable ED visits should be stratified by route of exposure and should account for population exposure to inhalable and edible products.
Grant Support:
By a grant entitled “The Adverse Health Effects of Edible Cannabis Products” from the CDPHE. Dr. Monte received support from NIH K23 GM110516, NIH CTSI UL1 TR001082, and CDPHE 17 FHHA 96950.
Disclosures: Dr. Monte reports grants from the Colorado Department of Public Health and Environment during the conduct of the study and also sits on the Colorado Retail Marijuana Public Health Advisory Committee, a group of clinicians and scientists tasked with reviewing the scientific literature related to the public health effects of cannabis use and exposure. Dr. Saben reports grants from the Colorado Department of Public Health and Environment during the conduct of the study. Authors not named here have disclosed no conflicts of interest. Disclosures can also be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M18-2809.
Appendix Table.
ICD Codes Used for Data Pull
| ICD-10-CM marijuana and cannabis codes |
| F12 Cannabis related disorders |
| F12.1 Cannabis abuse |
| F12.10 Cannabis uncomplicated |
| F12.12 Cannabis abuse with intoxication |
| F12.120 Cannabis uncomplicated |
| F12.121 Cannabis delirium |
| F12.122 Cannabis with perceptual disturbance |
| F12.129 Cannabis abuse unspecified |
| F12.15 Cannabis abuse with psychotic disorder |
| F12.150 Cannabis abuse with delusions |
| F12.151 Cannabis abuse with hallucinations |
| F12.159 Cannabis abuse unspecified |
| F12.18 Cannabis abuse with other cannabis-induced disorder |
| F12.180 Cannabis abuse with cannabis-induced anxiety disorder |
| F12.188 Cannabis abuse with other cannabis-induced disorder |
| F12.19 Cannabis abuse with unspecified cannabis-induced disorder |
| F12.2 Cannabis dependence |
| F12.20 Cannabis dependence uncomplicated |
| F12.21 Cannabis dependence in remission |
| F12.22 Cannabis dependence with intoxication |
| F12.220 Cannabis dependence uncomplicated |
| F12.221 Cannabis dependence with delirium |
| F12.222 Cannabis dependence with perceptual disturbance |
| F12.229 Cannabis dependence unspecified |
| F12.25 Cannabis dependence with psychotic disorder |
| F12.250 Cannabis dependence with delusions |
| F12.251 Cannabis dependence with hallucinations |
| F12.259 Cannabis dependence unspecified |
| F12.28 Cannabis dependence with other cannabis-induced disorder |
| F12.280 Cannabis dependence with cannabis-induced anxiety disorder |
| F12.288 Cannabis dependence with other cannabis-induced disorder |
| F12.29 Cannabis dependence with unspecified cannabis-induced disorder |
| F12.9 Cannabis use, unspecified |
| F12.90 Cannabis use uncomplicated |
| F12.92 Cannabis use, unspecified with intoxication |
| F12.920 Cannabis use uncomplicated |
| F12.921 Cannabis use with delirium |
| F12.922 Cannabis use with perceptual disturbance |
| F12.929 Cannabis use unspecified |
| F12.95 Cannabis use, unspecified with psychotic disorder |
| F12.950 Cannabis use with delusions |
| F12.951 Cannabis use with hallucinations |
| F12.959 Cannabis use unspecified |
| F12.98 Cannabis use, unspecified with other cannabis-induced disorder |
| F12.980 Cannabis use, unspecified with anxiety disorder |
| F12.988 Cannabis use, unspecified with other cannabis-induced disorder |
| F12.99 Cannabis with unspecified cannabis-induced disorder |
| T40.7X1A Poisoning by cannabis, accidental/unintentional |
| T40.7 Poisoning by, adverse effect of and underdosing of cannabis (derivatives) |
| T40.7X Poisoning by, adverse effect of and underdosing of cannabis (derivatives) |
| T40.7X1 Poisoning by cannabis (derivatives), accidental (unintentional) |
| T40.7X1A …… initial encounter |
| T40.7X1D …… subsequent encounter |
| T40.7X1S …… sequela |
| T40.7X2 Poisoning by cannabis (derivatives), intentional self-harm |
| T40.7X2A …… initial encounter |
| T40.7X2D …… subsequent encounter |
| T40.7X2S …… sequela |
| T40.7X3 Poisoning by cannabis(derivatives), assault |
| T40.7X3A …… initial encounter |
| T40.7X3D …… subsequent encounter |
| T40.7X3S sequel |
| T40.7X4A Poisoning by cannabis, undetermined |
| ICD-9-CM cannabis codes |
| 305.2 Marijuana/cannabis abuse, nondependent |
| 305.20 Marijuana/cannabis abuse, unspecified |
| 305.21 Marijuana/cannabis abuse, continuous |
| 305.22 Marijuana/cannabis abuse, episodic |
| 305.23 Marijuana/cannabis abuse, in remission |
| 304.3 Marijuana/cannabis dependence |
| 304.31 Marijuana/cannabis dependence unspecified |
| 304.32 Marijuana/cannabis dependence episodic |
| 304.33 Marijuana/cannabis dependence in remission |
| T40.7 Poisoning by cannabis |
ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification; ICD-10-CM = International Classification of Diseases, 10th Revision, Clinical Modification.
Current author addresses and author contributions are available at Annals.org.
Publisher's Disclaimer: Disclaimer: The contents of this work are the sole responsibility of the authors and do not necessarily represent the views of the National Institutes of Health (NIH) or the CDPHE.
Reproducible Research Statement: Study protocol, statistical code, and data set: Available from Dr. Monte (andrew.monte@ucdenver.edu).
References
- 1.Ogden DW. Investigations and Prosecutions in States Authorizing the Medical Use of Marijuana [Memorandum]. Accessed at http://blogs.justice.gov/main/archives/192 on 18 August 2014.
- 2.Colo. Const. amend. LXIV.
- 3.Zhu H, Wu LT. Trends and correlates of cannabis-involved emergency department visits: 2004 to 2011. J Addict Med. 2016;10:429–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Colorado Department of Revenue. Marijuana Sales Reports. Denver: Colorado Department of Revenue; 2018. Accessed at www.colorado.gov/pacific/revenue/colorado-marijuana-sales-reports on 9 July 2018. [Google Scholar]
- 5.Colorado Department of Public Health and Environment. Behavioral Risk Factor Surveillance System and Child Health Survey. Denver: Colorado Department of Public Health and Environment; 2018. Accessed at www.colorado.gov/pacific/cdphe/behaviorsurvey on 7 February 2019. [Google Scholar]
- 6.Cao D, Srisuma S, Bronstein AC, Hoyte CO. Characterization of edible marijuana product exposures reported to United States poison centers. Clin Toxicol (Phila). 2016;54:840–6. [DOI] [PubMed] [Google Scholar]
- 7.Dowd M. Don’t harsh our mellow, dude. The New York Times. 3 June 2014. Accessed at www.nytimes.com/2014/06/04/opinion/dowd-dont-harsh-our-mellow-dude.html on 7 February 2019.
- 8.Giombi KC, Kosa KM, Rains C, Cates SC. Consumers’ perceptions of edible marijuana products for recreational use: likes, dislikes, and reasons for use. Subst Use Misuse. 2018;53:541–7. doi: 10.1080/10826084.2017.1343353 [DOI] [PubMed] [Google Scholar]
- 9.Lamy FR, Daniulaityte R, Sheth A, Nahhas RW, Martins SS, Boyer EW, et al. “Those edibles hit hard”: exploration of Twitter data on cannabis edibles in the U.S. Drug Alcohol Depend. 2016;164:64–70. doi: 10.1016/j.drugalcdep.2016.04.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Phillips N. Trial for Richard Kirk in Observatory Park slaying set for March 2017. The Denver Post. 29 September 2016. Accessed at www.denverpost.com/2016/09/29/richard-kirk-observatory-park-marijuana-killing-wife-insanity-plea/2016 on 7 February 2019.
- 11.Ingold J. Denver coroner: Man fell to death after eating marijuana cookies. The Denver Post. 2 April 2014. Accessed at www.denverpost.com/2014/04/02/denver-coroner-man-fell-to-death-after-eating-marijuana-cookies/2014 on 7 February 2019.
- 12.Third Death in Colorado Linked to Marijuana Edibles. Food Safety News. 27 March 2015. Accessed at www.foodsafetynews.com/2015/03/third-death-in-colorado-linked-to-edible-marijuana/#.WzKfui2ZOjQ on 24 June 2018.
- 13.Monte AA, Zane RD, Heard KJ. The implications of marijuana legalization in Colorado. JAMA. 2015;313:241–2. doi: 10.1001/jama.2014.17057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang GS, Hall K, Vigil D, Banerji S, Monte A, VanDyke M. Marijuana and acute health care contacts in Colorado. Prev Med. 2017; 104:24–30. doi: 10.1016/j.ypmed.2017.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang GS, Le Lait MC, Deakyne SJ, Bronstein AC, Bajaj L, Roosevelt G. Unintentional pediatric exposures to marijuana in Colorado, 2009–2015. JAMA Pediatr. 2016;170:e160971. doi: 10.1001/jamapediatrics.2016.0971 [DOI] [PubMed] [Google Scholar]
- 16.Wang GS, Roosevelt G, Heard K. Pediatric marijuana exposures in a medical marijuana state. JAMA Pediatr. 2013;167:630–3. doi: 10.1001/jamapediatrics.2013.140 [DOI] [PubMed] [Google Scholar]
- 17.Wang GS, Roosevelt G, Le Lait MC, Martinez EM, Bucher-Bartelson B, Bronstein AC, et al. Association of unintentional pediatric exposures with decriminalization of marijuana in the United States. Ann Emerg Med. 2014;63:684–9. doi: 10.1016/j.annemergmed.2014.01.017 [DOI] [PubMed] [Google Scholar]
- 18.Hudak M, Severn D, Nordstrom K. Edible cannabis-induced psychosis: intoxication and beyond [Letter]. Am J Psychiatry. 2015;172: 911–2. doi: 10.1176/appi.ajp.2015.15030358 [DOI] [PubMed] [Google Scholar]
- 19.Hall KE, Monte AA, Chang T, Fox J, Brevik C, Vigil DI, et al. Mental health-related emergency department visits associated with cannabis in Colorado. Acad Emerg Med. 2018;25:526–37. doi: 10.1111/acem.13393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.D’Souza DC, Perry E, MacDougall L, Ammerman Y, Cooper T, Wu YT, et al. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology. 2004;29:1558–72. [DOI] [PubMed] [Google Scholar]
- 21.Desai R, Shamim S, Patel K, Sadolikar A, Kaur VP, Bhivandkar S, et al. Primary causes of hospitalizations and procedures, predictors of in-hospital mortality, and trends in cardiovascular and cerebrovascular events among recreational marijuana users: a five-year nationwide inpatient assessment in the United States. Cureus. 2018;10: e3195. doi: 10.7759/cureus.3195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grotenhermen F. Pharmacokinetics and pharmacodynamics of cannabinoids. Clin Pharmacokinet. 2003;42:327–60. [DOI] [PubMed] [Google Scholar]
- 23.Di Forti M, Marconi A, Carra E, Fraietta S, Trotta A, Bonomo M, et al. Proportion of patients in South London with first-episode psychosis attributable to use of high potency cannabis: a case-control study. Lancet Psychiatry. 2015;2:233–8. doi: 10.1016/S2215-0366(14)00117-5 [DOI] [PubMed] [Google Scholar]
- 24.van Os J, Bak M, Hanssen M, Bijl RV, de Graaf R, Verdoux H. Cannabis use and psychosis: a longitudinal population-based study. Am J Epidemiol. 2002;156:319–27. [DOI] [PubMed] [Google Scholar]
- 25.Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370:2219–27. doi: 10.1056/NEJMra1402309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kylie Lee KS, Sukavatvibul K, Conigrave KM. Cannabis use and violence in three remote Aboriginal Australian communities: analysis of clinic presentations. Transcult Psychiatry. 2015;52:827–39. doi: 10.1177/1363461515589047 [DOI] [PubMed] [Google Scholar]
- 27.Norström T, Rossow I. Cannabis use and violence: is there a link? Scand J Public Health. 2014;42:358–63. doi: 10.1177/1403494814525003 [DOI] [PubMed] [Google Scholar]
- 28.Jouanjus E, Lapeyre-Mestre M, Micallef J; French Association of the Regional Abuse and Dependence Monitoring Centres (CEIP-A) Working Group on Cannabis Complications. Cannabis use: signal of increasing risk of serious cardiovascular disorders. J Am Heart Assoc. 2014;3:e000638. doi: 10.1161/JAHA.113.000638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kalla A, Krishnamoorthy PM, Gopalakrishnan A, Figueredo VM. Cannabis use predicts risks of heart failure and cerebrovascular accidents: results from the National Inpatient Sample. J Cardiovasc Med (Hagerstown). 2018;19:480–4. doi: 10.2459/JCM.0000000000000681 [DOI] [PubMed] [Google Scholar]
- 30.Colorado Department of Public Health and Environment. Monitoring Health Concerns Related to Marijuana in Colorado. Denver: Colorado Department of Public Health and Environment; 2014. Accessed at www.colorado.gov/pacific/cdphe/retail-marijuana-public-health-advisory-committee on 7 February 2019. [Google Scholar]
- 31.Kim HS, Anderson JD, Saghafi O, Heard KJ, Monte AA. Cyclic vomiting presentations following marijuana liberalization in Colorado. Acad Emerg Med. 2015;22:694–9. doi: 10.1111/acem.12655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim HS, Hall KE, Genco EK, Van Dyke M, Barker E, Monte AA. Marijuana tourism and emergency department visits in Colorado [Letter]. N Engl J Med. 2016;374:797–8. doi: 10.1056/NEJMc1515009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vandrey R, Raber JC, Raber ME, Douglass B, Miller C, Bonn-Miller MO. Cannabinoid dose and label accuracy in edible medical cannabis products. JAMA. 2015;313:2491–3. doi: 10.1001/jama.2015.6613 [DOI] [PubMed] [Google Scholar]
- 34.Newmeyer MN, Swortwood MJ, Taylor ME, Abulseoud OA, Woodward TH, Huestis MA. Evaluation of divided attention psychophysical task performance and effects on pupil sizes following smoked, vaporized and oral cannabis administration. J Appl Toxicol. 2017;37:922–32. doi: 10.1002/jat.3440 [DOI] [PubMed] [Google Scholar]
- 35.Allen JA, Davis KC, Duke JC, Nonnemaker JM, Bradfield BR, Farrelly MC. New product trial, use of edibles, and unexpected highs among marijuana and hashish users in Colorado. Drug Alcohol Depend. 2017;176:44–7. doi: 10.1016/j.drugalcdep.2017.03.006 [DOI] [PubMed] [Google Scholar]
- 36.MacCoun RJ, Mello MM. Half-baked—the retail promotion of marijuana edibles. N Engl J Med. 2015;372:989–91. doi: 10.1056/NEJMp1416014 [DOI] [PubMed] [Google Scholar]
- 37.Benjamin DM, Fossler MJ. Edible cannabis products: it is time for FDA oversight. J Clin Pharmacol. 2016;56:1045–7. doi: 10.1002/jcph.778 [DOI] [PubMed] [Google Scholar]