Abstract
Patient: Female, 8
Final Diagnosis: Cerebral palsy
Symptoms: Gait abnormality
Medication: —
Clinical Procedure: —
Specialty: Rehabilitation
Objective:
Congenital defects/diseases
Background:
The purpose of this study was to compare gait abilities in a child with spastic diplegia according to different dorsiflexion angles on hinged ankle-foot orthosis (hinged AFO).
Case Report:
This study is a case report of a child who was diagnosed with spastic diplegia and ambulated independently with the use of a hinged AFO. For gait analysis, the GAITRite® was used under 3 different conditions including barefoot, wearing regular of hinged AFO, and wearing a dorsiflexion 10° hinged AFO. The gait velocity and cadence were collected as temporal parameters, while step length, stride length, and single and double leg support time were collected as temporal spatial parameters. As a result, when a regular hinged AFO was worn on the barefoot, the gait velocity and cadence per minute were increased, whereas the step length and stride length, the single and double leg support time decreased. The gait velocity, cadence, step length, and stride length were significantly increased when dorsiflexion 10° hinged AFO was applied compared to barefoot. The gait velocity, cadence, step length, and stride length increased with dorsiflexion 10° hinged AFO compared to regular hinged AFO.
Conclusions:
The results of this study demonstrated that wearing a dorsiflexion 10° hinged AFO would have a positive effect on improving gait ability of a child with cerebral palsy rather than wearing a bare foot and a general hinged AFO.
MeSH Keywords: Cerebral Palsy, Foot Orthoses, Gait
Background
Cerebral palsy is a non-progressive disease that causes dysfunctions of movement and postural control due to immature brain development and is one of the most common causes of childhood disorders [1]. About 70% to 80% of children with cerebral palsy are typically spastic [2]. Children with spastic diplegia show characteristics such as decreased proprioception, reduced range of motion, coordination disorder, and asymmetric body alignment, which are expressed in gait patterns such as decreased gait velocity, cadence, and single support time [3]. Thus, mobility is related to independence in function and participation in society so effective and efficient walking is one of the important goals for a child with cerebral palsy [4]. Orthosis is a one of the treatment options for correcting gait and posture, and it is also frequently used in general rehabilitation programs to children with cerebral palsy. A variety of orthosis devices are used to change abnormal movement patterns to normalize movement patterns and improve gait ability in children with spastic cerebral palsy [5]. Use of an ankle foot orthosis to restore a positioning peripheral joints, can reduce pathological reflex patterns and movements, and produce normal gait patterns [5]. A variety of ankle foot orthosis are used in clinical interventions, and are characterized by design, materials, stiffness, and ankle control.
Hinged ankle-foot orthosis (hinged AFO) is used to stabilize the foot and ankle so that the child with spastic cerebral palsy can perform functional gait [6]. Most children with cerebral palsy exhibit hyperextension in the extensors of the lower extremity, and the use of hinged AFO helps reduce spasticity in the triceps surae muscle by assisting dorsiflexion and inducing stretching of the Achilles tendon [7]. In addition, it has been reported that the use of hinged AFO controls excessive plantar flexion during the swing phase of walking by correcting the preposition of the foot required for initial contact [8], and thereby increases the range of motion (ROM) in the ankle joint from reduced knee moment during the stance phase of walking, enabling symmetrical weight shift [9,10]. Balaban et al. (2007) reported that 11 children with spastic hemiplegic cerebral palsy who wore hinged AFOs, had reduced dynamic equinus performance and energy expenditure of gait [9]. Radtka et al. (2005) compared walking in 12 children with spastic diplegic cerebral palsy child who wore solid AFO and hinged AFO and found that both orthoses increased the stride length, reduced abnormal ankle plantar flexion during initial contact, midstance, and terminal stance, and increased ankle plantar flex-or moments closer to normal during terminal stance. Hinged AFOs increased ankle dorsiflexion at terminal stance and increased ankle power generation during pre-swing as compared to solid AFO. The hinged AFO would be recommended to produce more normal dorsiflexion during terminal stance and increased ankle power generation during pre-swing in children with spastic diplegic cerebral palsy [7].
The talocrural joint is a hinge joint with 1° of freedom. While normal walking requires at least 10° of dorsiflexion, movements such as going downstairs and squatting require larger degrees of dorsiflexion [11]. Thus, the ROM of dorsiflexion should meet at least 10° of motion to perform functional movements [12]. However, the hinged AFOs commonly used in clinical setting generally set to a neutral ankle position (0°). In addition, there have been no studies that have investigated the effects from different dorsiflexion angles on hinged AFOs.
Thus, the present study aimed to compare the spatiotemporal gait parameters depending on gait the use a regular hinged AFO (with dorsiflexion angle 0°) and a dorsiflexion 10° hinged AFO in a child with spastic diplegia.
Case Report
Patient history and systems review
The patient was an 8-year-old female with spastic diplegia who was receiving treatment at S Rehabilitation Center. In terms of physical characteristics, she was 125 cm in height and weighed 27 kg. She was born naturally at 35-week gestational age weighing 2.7 kg. The magnetic renounce imaging (MRI) results at birth had shown no abnormalities, but the patient exhibited development delays.
Examination
The patient did not have difficulties conducting independent activities including functional movements that use large muscles, such as running or jumping, but was classified as level 1 according to the Gross Motor Function Classification System (GMFCS) because her velocity, balance, and coordination in performing tasks were limited. The patient was also classified as level 1 according to the Manual Ability Classification System since she did not have difficulties in performing tasks using hands and was not limited in conducting activities of daily living (ADL) at the necessary speed and accuracy. Based on the Communication Classification System, the patient was classified as level I because she could adequately communicate with others regardless of the conversation partner.
In this study, a gait analysis system was used to measure the patient’s gait ability. Before measuring, a 5-minute adaptation time was given respectively for 3 conditions; barefoot, wearing a regular hinged AFO and wearing a dorsiflexion 10° hinged AFO. The starting signal was given verbally but after having the patient stand in an upright position looking forward with her elbows fully extended. The measurements were taken 9 times in total, 3 times respectively under t3 conditions; barefoot, wearing a regular hinged AFO and a dorsiflexion 10° hinged AFO.
The spatio-temporal gait parameters of the patient were collected using gait analysis system (GAITRite® Electronic Walkway, CIR System, Inc., NJ, USA). GAITRite® is an electronic walkway that is about 4 m-long and 0.89 m-wide and has pressure sensors (a sensor 1 cm in diameter spaced at intervals of 1.27 cm). Gait parameters are automatically calculated on the computer when pressure generated from the foot contacting the mat is registered through the attached sensors at sampling frequency of 80 Hz [14]. Velocity and cadence were collected as temporal parameters, and step length, stride length, single support time, and double support time as temporal spatial parameters. This tool has been found to have excellent test-retest reliability (ICC=0.91) [15].
Clinical impression
The gait velocity was 110 cm/seconds and the cadence was 176.7 steps/minute. The right step length was 38.5 cm and the left side 36.2 cm. The right stride length was 74.7 cm and the left side 75.3 cm. The single leg support time was 0.3 seconds on the right side and 0.2 seconds on the left side. The double leg support time was 0.1 seconds on the right and 0.2 seconds on the left.
Intervention (hinged ankle-foot orthosis)
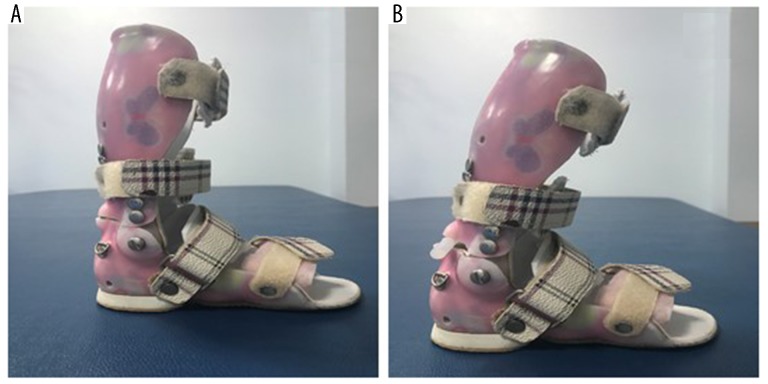
In this study, the hinged AFOs (E-care Medical Center, Seoul, Korea) (Figure 1) were custom-made according to the physical characteristics of the patient. The hinged AFOs were made of a 4.8 mm thick polyester material, which was shaped to support the foot and ankle starting from the bottom of the toes, cover the medial edge of the foot, and extend along the rear calf up to the point 2.5 to 5 cm under then knee [16]. The hinged AFOs were designed so that the position of the hinge forming the joint of the hinged AFO was aligned to the distal end of the malleolus of each patient to allow free dorsiflexion, and that planter flexion does not occur beyond dorsiflexion at 0° [17].
Figure 1.
Hinged ankle-foot orthosis used in this study. (A) Hinged ankle-foot orthosis, (B) dorsiflexion 10° hinged ankle-foot orthosis.
Data analysis
The measurements taken at barefoot, wearing regular hinged AFO, and wearing dorsiflexion 10° hinged AFO were compared using descriptive statistics.
Results
The gait velocity increased from 64.7 cm/second to 67.1 cm/second, which was 2.4 cm/second when walking with a general hinged AFO compared to barefoot, the cadence showed an increase of 9.4 steps/minute from 112.3 steps/minute to 121.7 steps/minute. The right step length decreased from 36.28 cm to 31.27 cm by 5.01 cm and the left step length increased from 32.78 cm to 35.17 cm by 2.39 cm. The right stride length was decreased from 69.96 cm to 66.83 cm (3.13 cm), and the left stride length decreased from 69.7 cm to 66.68 cm (3.02 cm). The right single leg support time decreased by 0.02 seconds from 0.35 seconds to 0.33 seconds, and the left single leg support time decreased by 0.04 seconds from 0.40 seconds to 0.36 seconds. The double leg support time of right side was 0.28 seconds each, and the left double leg support time was decreased from 0.29 seconds to 0.28 seconds by 0.01 seconds.
In comparison with the barefoot, the velocity increased from 64.7 cm/second to 84.6 cm/second with an increase of 19.9 cm/second when walking with a dorsiflexion 10° hinged AFO, the cadence was increased from 112.3 steps/minute to 132.8 steps/minute by 20.5 steps/minute. Right step length was 36.28 cm each and left step length increased from 32.7 cm to 40.66 cm with an increase of 7.88 cm. Right stride length showed an increase of 7.3 cm from 69.96 cm to 77.26 cm, and left stride length increased from 69.7 cm to 77.51 cm with an increase of 7.81 cm. Right single leg support time showed a decrease of 0.02 seconds from 0.35 seconds to 0.33 seconds, and left single leg support time showed a decrease of 0.07 seconds from 0.4 seconds to 0.33 seconds. Right double leg support time decreased from 0.28 seconds to 0.24 seconds, which was 0.04 seconds and left double leg support time decreased from 0.29 seconds to 0.24 seconds by 0.05 seconds (Table 1).
Table 1.
Comparison of spatio-temporal gait parameters depending on type of hinged AFO.
| Barefoot | Regular HAFO | DF 10° HAFO | |
|---|---|---|---|
| Velocity (cm/sec) | 64.70 | 67.10 | 84.60 |
| Cadence (steps/min) | 112.30 | 121.70 | 132.80 |
| Rt. step length (cm) | 36.28 | 31.27 | 36.28 |
| Lt. step length (cm) | 32.78 | 35.17 | 40.66 |
| Rt. stride length (cm) | 69.96 | 66.83 | 77.26 |
| Lt. stride length (cm) | 69.70 | 66.68 | 77.51 |
| Rt. single support time (sec) | 0.35 | 0.33 | 0.33 |
| Lt. single support time (sec) | 0.40 | 0.36 | 0.33 |
| Rt. double support time (sec) | 0.28 | 0.28 | 0.24 |
| Lt. double support time (sec) | 0.29 | 0.28 | 0.24 |
HAFO – hinged ankle foot orthosis; DF – dorsiflexion; Rt – right; LT – left.
In comparison with the regular hinged AFO, the gait velocity increased from 17.6 cm/second to 84.6 cm/second when walking with a dorsiflexion 10° hinged AFO, the cadence was increased from 121.7 steps/minute to 132.8 steps/minute by 11.1 steps/minute. Right step length increased from 31.27 cm to 36.28 cm which was 5.01 cm, and left step length increased from 35.17 cm to 40.66 cm and increased to 5.49 cm. Right stride length increased from 66.83 cm to 77.26 cm, which was 10.43 cm. The stride length increased from 66.68 cm to 77.51 cm with an increase of 10.83 cm. Right single leg support time was 0.33 seconds and left single leg support time showed a decrease of 0.03 seconds from 0.36 seconds to 0.33 seconds. The double leg support time showed a 0.04 second decrease from 0.28 seconds to 0.24 seconds in both regular and dorsiflexion 10° hinged AFO (Table 1).
Discussion
The talocrural joint is a hinge joint with a degree of freedom of 1°, with a normal ROM of 20° of dorsiflexion in the neutral and 30° to 50° of the plantar flexion [19]. All movements of the ankle, including dorsiflexion, are essential for gait and balance, as they regulate the interaction between the foot and the ground. At least 10° of dorsiflexion is required for functional activity and normal gait, such as stepping down and squatting require more angles of dorsiflexion, which can cause problems in ADL when there is a restriction of dorsiflexion [11]. The ROM of dorsiflexion is closely related to postural control and functional capacity [20] and correlates with balance ability [21]. Mecagni et al. suggested that the reduction of ROM of ankle joints cause a change in the whole-body movement by restricting the balance and functional ability. As a result, it has been reported that the ability to control posture causing compensatory movement of the hip joint and trunk is reduced [22]. In particular, the limitation of dorsiflexion is manifested by changes in joint motion such as talus position and gliding restriction [23,24]; it is one of the major causes of gait disturbance [25] and increased risk of reduced stride, decreased gait speed, and risk of falls [26].
In this study, to solve the plantar flexion problem in a child with cerebral palsy and to investigate the change of gait parameters according to the angle of dorsiflexion, gait analysis was performed by barefoot, wearing a regular hinged AFO, and wearing a dorsiflexion 10° hinged AFO. The results revealed that when a regular hinged AFO was worn on the barefoot, the gait velocity and the cadence increased, whereas step length, stride length, single leg support time, and double leg support time were decreased. The gait velocity, cadence, step length, and stride length were increase with dorsiflexion 10° hinged AFO compared to regular hinged AFO. The present study showed similar result with a previous study that suggested wearing hinged AFO improved gait velocity, increased dorsiflexion in heel strike and swing phase, and decreased spasticity of the ankle [27]. In addition, Buckon et al. reported a significant increase in stride and step length at the time of wearing hinged AFO compared to solid AFO and posterior leaf spring in spastic diplegia cerebral palsy [28]. Another previous study investigated the effects of hinged AFO compared to solid AFO on spastic cerebral palsy reported a significant change in stride length [7]. The gait features of spastic cerebral palsy interfere with the normal interaction of foot and ankle on the support surface, and plantar flexion maintained throughout the stance phase reduce plantar flexion moment and force production in swing phase [3,18]. Resolving these problems in rehabilitation is an important goal for inducing normal gait of a child with spastic cerebral palsy. Hinged AFO adjusts excessive plantarflexion during swing phase to correct the pre-position of the foot required for initial contact [8]. Toe gait of cerebral palsy, which is an abnormal gait feature, is changed to heel-toe gait [9], allowing normal weight shift within the sole [29]. Aboutorabi et al. (2017) reported that hinged AFO improved spatio-temporal gait parameters such as stride length, walking speed, single limb support, and gait symmetry. Hinged AFO also had positive effects in hemiplegic cerebral palsy on ankle ROM and power as well as knee ROM. So that these factors had a positive effect change on decreased energy expenditure in hemiplegic cerebral palsy patients [30]. Hinged AFO prevents dynamic equine deformity of ankle initial contact so it blocks ankle plantarflexion that it can made free ankle dorsiflexion. Therefore, it can restore the first ankle rocker and produce physiological heel contact [9]. Hinged AFO is effective in improvement of gross motor function [31]; hinged AFO also prevents plantarflexion and provides free dorsiflexion so that it can facilitate development motor skills and can normalizes ankle motion in the stance phase [32].
In this study, a positive change was found in the spatio-temporal gait parameters when dorsiflexion 10° hinged AFO was worn. This suggests that dorsiflexion 10° hinged AFO improves stability and reduces the time required for feet on the ground. This is consistent with the previous studies that stable functional mobility of standing and gait make faster gait speed [33,34], Wearing AFO prevents ankle joint contracture and deformity and improves gait ability [35,36]. Kim and Park (2011) investigated the balance according to the angle of AFO, and they reported that when the bending angle of AFO was dorsiflexed 10°, the movement of the center of pressure was significantly reduced, and it positively affected the balance ability [37]. The stability of the ankle joints not only improve the balance ability by compensating for insufficient instability of the ankle [38–40], but also facilitates the movement of body weight to the weight supporting legs during gait, which may have a positive impact on static and dynamic balance by reducing body asymmetry [41]. The results of these previous studies suggest that wearing dorsiflexion 10° hinged AFO increases the stability of the lower extremities supporting the body weight in the foot as well as improving the balance ability in standing; it is possible to generate sufficient propulsive force in the pre-swing phase of the opposite leg. Also, the increased dorsiflexion angle improves the foot drag in the swing phase, suggesting that other gait parameters are improved as well as stride and step length.
In this study, single and double leg support time decreased when dorsiflexion 10° hinged AFO was applied compared with wearing barefoot and regular hinged AFO. These results are similar to the results reported by Balaban et al. (2007) that showed reduction of single and double leg support time after wearing hinged AFO in a child with rigid hemiplegia cerebral palsy [7]. The dorsiflexion 10° hinged AFO regulates the alignment of the hindfoot and the midfoot during stance phase, indicating a stable weight bearing increase [42]. Like conventional orthoses, dorsiflexion 10° hinged AFO can help the heel to make stronger contact on the ground; proper contact of the heel to the ground plays an important role in maintaining ankle stability and selective control of plantar flexion and dorsiflexion, which appears to affected gait improvement [43].
Therefore, we found that when the child with cerebral palsy wore the dorsiflexion 10° hinged AFO there was a positive effect on the overall gait cycle including velocity, cadence, step length, and stride length. Several other previous study results support this finding. Not all the previous studies had results consistent with our present study. The differences in results might be caused by small study sample sizes and differences in evaluation devices. However, this study only does not itself prove the positive effects of wearing a dorsiflexion 10° hinged AFO since only one patient was included. Future studies are needed on the effects of wearing a dorsiflexion 10° hinged AFO and should include a larger number of patients and should also study the quality of gait.
Conclusions
This study compared the gait abilities of a child with spastic diplegia, according to different dorsiflexion angles of a hinged AFO. It was found that gait velocity, cadence, step length, and stride length were increased, and single and double support times decreased. However, this study had several limitations: it is difficult to generalize the findings drawn from this study to all children with cerebral palsy. Therefore, it is recommended that in the future, high quality studies investigate how hinged AFOs with different dorsiflexion angles influence the gait ability of child with cerebral palsy.
References:
- 1.Scherzer AL, Tscharnuter I. Early diagnosis and therapy in cerebral palsy: A primer on infant developmental problems. 2nd ed. New York: Marcel Dekker; 1990. pp. 678–80. [Google Scholar]
- 2.Krigger KW. Cerebral palsy: An overview. Am Fam Physician. 2006;73(1):91–100. [PubMed] [Google Scholar]
- 3.Ounpuu S, Gage JR, Davis RB. Three-dimensional lower extremity joint kinetics in normal pediatric gait. J Pediatr Orthop. 1991;11(3):341–49. [PubMed] [Google Scholar]
- 4.Sankar C, Mundkur N. Cerebral palsy-definition, classification, etiology and early diagnosis. Indian J Pediatr. 2005;72(10):865–68. doi: 10.1007/BF02731117. [DOI] [PubMed] [Google Scholar]
- 5.Middleton EA, Hurley GR, McIlwain JS. The role of rigid and hinged polypropylene ankle-foot-orthoses in the management of cerebral palsy: A case study. Prosthet Orthot Int. 1988;12(3):129–35. doi: 10.3109/03093648809079396. [DOI] [PubMed] [Google Scholar]
- 6.Im HY. The immediate effect standing balance and dynamic activity on barefoot, wearing SPAFO and wearing HPAFO in hemiplegic patients. J Kor Phys Ther. 2005;17(1):87–97. [Google Scholar]
- 7.Radtka SA, Skinner SR, Johanson ME. A comparison of gait with solid and hinged ankle-foot orthoses in children with spastic diplegic cerebral palsy. Gait Posture. 2005;21(3):303–10. doi: 10.1016/j.gaitpost.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 8.Romkers J, Brunner R. Comparison of a dynamic and a hinged ankle-foot orthosis by gait analysis in patients with hemiplegic cerebral palsy. Gait Posture. 2002;15(1):18–24. doi: 10.1016/s0966-6362(01)00178-3. [DOI] [PubMed] [Google Scholar]
- 9.Balaban B, Yasar E, Dal U, et al. The effect of hinged ankle-foot orthosis on gait and energy expenditure in spastic hemiplegic cerebral palsy. Disabil Rehabil. 2007;29(2):139–44. doi: 10.1080/17483100600876740. [DOI] [PubMed] [Google Scholar]
- 10.Romkes J, Hell AK, Brunner R. Changes in muscle activity in children with hemiplegic cerebral palsy while walking with and without ankle-foot orthoses. Gait Posture. 2006;24(4):467–74. doi: 10.1016/j.gaitpost.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Collins N, Teys P, Vicenzino B. The initial effects of a Mulligan’s mobilization with movement technique on dorsiflexion and pain in subacute ankle sprains. Man Ther. 2004;9(2):77–82. doi: 10.1016/S1356-689X(03)00101-2. [DOI] [PubMed] [Google Scholar]
- 12.Wolfson L, Whipple R, Judge J, et al. Training balance and strength in the elderly to improve function. J Am Geriatr Soc. 1993;41(3):341–43. doi: 10.1111/j.1532-5415.1993.tb06716.x. [DOI] [PubMed] [Google Scholar]
- 13.Kim SG, Ryu YU, Kim WH. The effectiveness of backward gait training on the treadmill in children with spastic diplegic cerebral palsy. A pilot study. Phys Ther Kor. 2012;19(3):81–90. [Google Scholar]
- 14.Webster PJ, Holland GJ, Curry JA, Chang HR. Changes in tropical cyclone number, duration, and intensity in a warming environment. Science. 2005;309(5742):1844–46. doi: 10.1126/science.1116448. [DOI] [PubMed] [Google Scholar]
- 15.van Uden CJ, Besser MP. Test-retest reliability of temporal and spatial gait characteristics measured with an instrumented walkway system(GAITRite) BMC Musculoskelet Disord. 2004;5:13. doi: 10.1186/1471-2474-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Butlner PV, Nene AV. The biomechanics of fixed ankle foot orthoses and their potential in the management of cerebral palsied children. Physiotherapy. 1991;77(2):81–88. [Google Scholar]
- 17.Knutson LM, Clark DE. Orthotic devices for ambulation in children with cerebral-palsy and myelomeningocele. Phys Ther. 1991;71(12):947–60. doi: 10.1093/ptj/71.12.947. [DOI] [PubMed] [Google Scholar]
- 18.Perry J, Davids JR. Gait analysis: Normal and pathological function. J Pediatr Orthop. 1992;12(6):815. [Google Scholar]
- 19.Milner M, Dall D, McConnell VA, et al. Angle diagrams in the assessment of locomotor function. Studies on normal subjects for various speeds and some preliminary work on patients requiring total hip reconstruction (Charnley low-friction arthroplasty) S Afr Med J. 1973;47(22):951–57. [PubMed] [Google Scholar]
- 20.Spink MJ, Fotoohabadi MR, Wee E, et al. Predictors of adherence to a multifaceted podiatry intervention for the prevention of falls in older people. BMC Geriatr. 2011;11:51. doi: 10.1186/1471-2318-11-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bok SK, Lee TH, Lee SS. The effects of changes of ankle strength and range of motion according to aging on balance. Ann Rehabil Med. 2013;37(1):10–16. doi: 10.5535/arm.2013.37.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mecagni C, Smith JP, Roberts KE, et al. Balance and ankle range of motion in community-dwelling women aged 64 to 87 years: A correlational study. Phys Ther. 2000;80(10):1004–11. [PubMed] [Google Scholar]
- 23.Denegar CR, Hertel J, Fonseca J. The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. J Orthop Sports Phys Ther. 2002;32(4):166–73. doi: 10.2519/jospt.2002.32.4.166. [DOI] [PubMed] [Google Scholar]
- 24.Koh EK, Weon JH, Jung DY. Effect of direction of gliding in tibiofibular joint on angle of active ankle dorsiflexion. J Korean Soc Phys Med. 2014;9(4):439–45. [Google Scholar]
- 25.Drewes LK, McKeon PO, Paolini G, et al. Altered ankle kinematics and shank-rear-foot coupling in those with chronic ankle instability. J Sport Rehabil. 2009;18(3):375–88. doi: 10.1123/jsr.18.3.375. [DOI] [PubMed] [Google Scholar]
- 26.Kang DY, Kim YM, Lee KS. Comparisons of lower extremity strength, cognition, and ankle mobility according to the 8.5seconds cut-off point for the 8-foot up-and-go test in elderly women. J Korean Soc Phys Med. 2015;10(3):305–11. [Google Scholar]
- 27.Lintanf M, Bourseul JS, Houx L, et al. Effect of ankle-foot orthoses on gait, balance and gross motor function in children with cerebral palsy: A systematic review and meta-analysis. Ann Phys Rehabil Med. 2018;61:e317. doi: 10.1177/0269215518771824. [DOI] [PubMed] [Google Scholar]
- 28.Buckon CE, Thomas SS, Jakobson-Huston S. Comparison of three ankle-foot orthosis configurations for children with spastic diplegia. Dev Med Child Neurol. 2004;46(9):590–98. doi: 10.1017/s0012162204001008. [DOI] [PubMed] [Google Scholar]
- 29.Rethlefsen S, Kay R, Dennis S, et al. The effects of fixed and articulated ankle-foot orthoses on gait patterns in subjects with cerebral palsy. J Pediatr Orthop. 1999;19(4):470–74. doi: 10.1097/00004694-199907000-00009. [DOI] [PubMed] [Google Scholar]
- 30.Aboutorabi A, Arazpour M, Ahmadi Bani M, et al. Efficacy of ankle foot orthoses types on walking in children with cerebral palsy: A systematic review. Ann Phys Rehabil Med. 2017;60(6):393–402. doi: 10.1016/j.rehab.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 31.Dalvand H, Dehghan L, Feizi A, et al. The impacts of hinged and solid ankle-foot orthoses on standing and walking in children with spastic diplegia. Iran J Child Neurol. 2013;7(4):12–19. [PMC free article] [PubMed] [Google Scholar]
- 32.Russell DJ, Gorter JW. Assessing functional differences in gross motor skills in children with cerebral palsy who use an ambulatory aid or orthoses: Can the GMFM-88 help? Dev Med Child Neurol. 2005;47(7):462–67. doi: 10.1017/s0012162205000897. [DOI] [PubMed] [Google Scholar]
- 33.Andersson C, Grooten W, Hellsten M, et al. Adults with cerebral palsy: Walking ability after progressive strength training. Dev Med Child Neurol. 2003;45(4):220–28. doi: 10.1017/s0012162203000446. [DOI] [PubMed] [Google Scholar]
- 34.Williams EN, Carroll SG, Reddihough DS, et al. Investigation of the timed ‘up & go’ test in children. Dev Med Child Neurol. 2005;47(8):518–24. doi: 10.1017/s0012162205001027. [DOI] [PubMed] [Google Scholar]
- 35.Ferrari A, Neviani R, Borghi C, et al. Effectiveness of AFO orthoses in children affected by cerebral palsy: Clinical evaluation does not always define patient satisfaction. Gait Posture. 2012;35:37–38. [Google Scholar]
- 36.Park ES, Park CI, Chang HJ, et al. The effect of hinged ankle-foot orthoses on sit-to-stand transfer in children with spastic cerebral palsy. Arch Phys Med Rehabil. 2004;85(12):2053–57. doi: 10.1016/j.apmr.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 37.Kim CS, Park SY. Effects of an ankle foot orthosis with ankle angles on balance performance in healthy Adults. Journal of the Ergonomics Society of Korea. 2011;30(2):291–96. [Google Scholar]
- 38.Esquenazi A, Ofluoglu D, Hirai B, et al. The effect of an ankle-foot orthosis on temporal spatial parameters and asymmetry of gait in hemiparetic patients. PM R. 2009;1(11):1014–18. doi: 10.1016/j.pmrj.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 39.Fatone S, Gard SA, Malas BS. Effect of ankle-foot orthosis alignment and foot-plate length on the gait of adults with poststroke hemiplegia. Arch Phys Med Rehabil. 2009;90(5):810–18. doi: 10.1016/j.apmr.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 40.Nolan KJ, Savalia KK, Lequerica AH, et al. Objective assessment of functional ambulation in adults with hemiplegia using ankle foot orthotics after stroke. PM R. 2009;1(6):524–29. doi: 10.1016/j.pmrj.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 41.Wang RY, Yen Lu, Lee CC, et al. Effects of an ankle-foot orthosis on balance performance in patients with hemiparesis of different durations. Clin Rehabil. 2005;19(1):37–44. doi: 10.1191/0269215505cr797oa. [DOI] [PubMed] [Google Scholar]
- 42.Molnar GE, Alexander MA. Pediatric Rehabilitation. 3rd ed. Philadelphia, PA: Hanley & Belfus; 1999. pp. 193–217. [Google Scholar]
- 43.Hwang YI, An DH, Yoo WG. Effects of the dual AFO on gait parameters in stroke patients. Neuro Rehabilitation. 2012;31(4):387–93. doi: 10.3233/NRE-2012-00808. [DOI] [PubMed] [Google Scholar]