Abstract
The current study examines a military family stress model, evaluating associations between deployment-related stressors (i.e., deployment length/number, posttraumatic stress disorder [PTSD] symptoms) and parent, child, parenting, and dyadic adjustment among families in which a parent had previously deployed to Iraq or Afghanistan in the recent conflicts. Married families (N = 293) with at least one child between the ages of 4 and 12 were recruited from a Midwestern state. Service members were from the Reserve Component (National Guard or Reserves); fathers (N = 253) and/or mothers had deployed (N = 45) to the recent conflicts in the Middle East. Multiple-method (observations of parenting and couple interactions; questionnaires) and multiple informant measures were gathered online and in the homes of participants, from parents, children, and teachers. Findings demonstrated associations between mothers’ and fathers’ PTSD symptoms and a latent variable of child adjustment comprising teacher, parent, and child report. Mothers’ but not fathers’ PTSD symptoms were also associated with dyadic adjustment and parenting practices; parenting practices were in turn associated with child adjustment. The results are discussed in terms of their implications for military family stress research and interventions to support and strengthen parents and families after deployment.
Keywords: Military, Families, Children, Couples, Family Stress Model
INTRODUCTION
The wars of the first 15 years of this century have resulted in combat deployments of almost two million service members of whom approximately 40% are parents (Defense Manpower Data Center, 2015). Almost two million children have been affected by the deployment of a parent to Operations Iraqi and Enduring Freedom, and New Dawn (OIF, OEF, OND; Department of Defense, 2009). Moreover, almost half of the United States’ fighting force comprises “civilian soldiers”—National Guard and Reserve (NG/R) service members who live, for the most part, civilian lives (Defense Manpower Data Center, 2015). Despite the large numbers of U.S. families affected by the recent conflicts, relatively little is known about the family adjustment of parents, couples, and their children in the wake of parents’ deployment to war. In this article, we propose and empirically test a military family stress model. Using multiple-method and multiple-informant data, we examine associations of deployment-related stressors with three key elements of family functioning: parenting practices, dyadic adjustment, and children’s adjustment, in NG/R families in which at least one parent previously deployed to OIF, OEF, or OND.
The last decade has seen a significant increase in empirical research on military families, but studies have been hampered by small sample sizes and mono-informant data (i.e., questionnaire data from a single member of a family, typically a nondeployed mother) or, at best, data from two parents. With few exceptions (e.g., Oshri et al., 2015) studies have typically not gathered multiple-method (i.e., questionnaire and observational data) and multiple-informant family data (i.e., from parents, children, and teachers), both of which increase the robustness of findings. Most studies have sampled active-duty, rather than reserve component families (Siegel, Davis, & Committee on Psychosocial Aspects of Child and Family Health and Section on Uniformed Services, 2013). Several theoretical and conceptual models have been put forth to understand military family adjustment; few have been tested empirically (see, e.g., Bowen, Martin, & Mancini, 2013; Lavee, McCubbin, & Patterson, 1985).
Family Stress Models
Family stress models seek to explain the mechanisms through which external stressors such as marital transitions, poverty, and psychopathology affect family functioning, by considering the impact of these stressors on the behaviors of parents and child(ren). Family stress models were initially proposed by Glen Elder and his colleagues, who sought to understand the influence of economic disadvantage in the Great Depression on fathers’ behaviors and child outcomes (e.g., Elder, Nguyen, & Caspi, 1985). Elder’s seminal research, and subsequently Conger et al.’s (2002) research with farm families in Iowa, demonstrated that socioeconomic stress led to feelings of economic pressure in parents, which in turn led to parents’ distress, which negatively impacted children’s adjustment through impaired parenting, and/or impaired couple or dyadic adjustment (e.g., Conger et al., 2002; Simons et al., 2016).
These mediation models thus posit that stressful family transitions or processes (e.g., poverty, divorce, parental mental illness) increase parental psychological distress, which in turn impairs parenting practices and/or dyadic adjustment, increasing risks for child maladjustment (see Barnett, 2008, for a review of family stress models). For example, couple relationships have been shown to mediate the relationship between poverty and parenting practices (e.g., Conger et al., 2002). In a different stressor context, parenting practices mediated the relationship between divorce-related sequelae and their effects on child adjustment (Forgatch & DeGarmo, 1999; Forgatch, Patterson, Degarmo, & Beldavs, 2009). In a study examining shared and nonshared environmental influences on family functioning in the context of intimate partner violence, hostile unsupportive marital relations were associated with coercive parenting, which in turn predicted child anger (Rhoades et al., 2011). Relevant research also has focused on the detrimental impact of parental psychopathology, particularly maternal depression, on dyadic adjustment, parenting practices, and child adjustment (e.g., Downey & Coyne, 1990; Gartstein & Fagot, 2003).
Deployment-related family stressors
We conceptualize wartime deployment and its consequences (i.e., posttraumatic stress disorder [PTSD] symptoms) as family stressors because of the separation of a parent service member from spouse/partner and children, and the concomitant danger (and potential family anxiety). There is increasing evidence that deployment and combat stressors are associated with child and family adjustment problems (e.g., Card et al., 2011; Mansfield, Kaufman, Engel, & Gaynes, 2011; Sheppard, Weil Malatras, & Israel, 2010). Despite this, few studies have posited or empirically tested mechanisms accounting for child adjustment problems using multiple-method data from various family members.
Research has yielded mixed findings with regard to the associations of parental deployment to war (typically measured by length of the deployment or number of times a parent has previously deployed) with family functioning variables such as dyadic and child adjustment. Some research has found that the number and length of a parent’s deployments are associated with poorer parenting, child adjustment, and/or dyadic adjustment (e.g., Card et al., 2011; Chandra, Burns, Tanielian, & Jaycox, 2011; Davis, Hanson, Zamir, Gewirtz, & DeGarmo, 2015; Flake, Davis, Johnson, & Middleton, 2009; Lester et al., 2010), while other studies have not found significant associations between these factors (Allen, Rhoades, Stanley, & Markman, 2010; Meadows et al., 2016). For example, the Rand Deployment Life Study (Meadows et al., 2016), a longitudinal examination of 2,724 families across the deployment cycle, generally found no significant effects of deployment on child or teen outcomes. Similarly, in a study of 434 active-duty Army couples, Allen et al. (2010) found no differences in couples’ self-reports of dyadic adjustment between those separated by a past year deployment and those who did not experience a deployment. Of note, however, a past year deployment was associated with increased PTSD symptoms in the service member; these, in turn, were associated with poorer dyadic adjustment (Allen et al., 2010).
Posttraumatic stress disorder symptoms may be a consequence of wartime deployment in a significant minority of service members, although prevalence rates vary widely (Ramchand, Rudavsky, Grant, Tanielian, & Jaycox, 2015). A growing body of research has examined links between combat-related PTSD and family relationships, showing PTSD to be associated with parenting difficulties, as well as risks to child and dyadic adjustment (see., e.g., Cozza, 2016; Dekel & Monson, 2010; Gewirtz, Polusny, DeGarmo, Khaylis, & Erbes, 2010).
Testing a Military Family Stress Model Using Baseline Data from the After Deployment, Adaptive Parenting Tools Study
The present study reports baseline findings from a randomized controlled trial of a parenting program for military families. Hypothesized relationships are presented for the military family stress model (see Figure 1). Focal family process variables are highlighted on the right-hand side. Each path is well supported by developmental and family process research as noted above. For the current baseline investigation, stressors associated with deployment (i.e., number and length of deployments and parental PTSD symptoms) are hypothesized to interfere with family functioning in each of the respective domains of dyadic adjustment, parenting practices, and child adjustment (Gewirtz, Erbes, Polusny, Forgatch, & Degarmo, 2011; Gewirtz et al., 2010). Higher levels of dyadic adjustment are expected to be positively associated with higher levels of effective parenting practices. Higher levels of dyadic adjustment and effective parenting practices are expected to be associated with better child adjustment. Specifically, we predict that (a) deployment stressors will be negatively associated with child adjustment, and (b) parenting practices and dyadic adjustment will mediate the association of deployment stressors on child adjustment.
FIGURE 1.
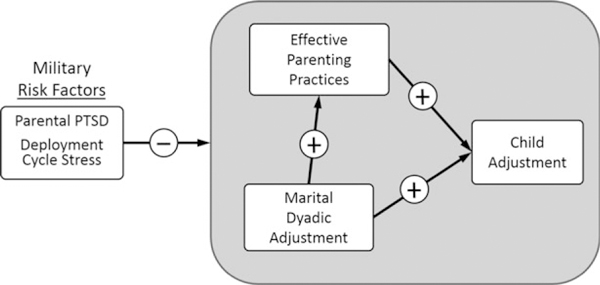
Hypothesized Relationships of the Military Family Stress Model.
METHODS
Participants
The current sample included 293 married military families in a Midwestern state, comprising 287 mothers, 263 fathers, and 293 children. Families had consented and completed a baseline assessment for a prevention study evaluating the effectiveness of a parenting program (After Deployment Adaptive Parenting Tools [ADAPT]). Families were eligible to participate in the study if at least one parent had previously deployed to recent conflicts (i.e., Operation Iraqi Freedom, Operation Enduring Freedom, or Operation New Dawn, OIF/OEF/OND), and at least one child between the ages of 4 and 12 was living in the home. The focal study child was randomly selected in cases of more than one eligible child. The current sample is a subset of the full sample of 336 families in the larger study; single parent families (N = 43) were excluded, leaving 293 families. Of the 293 families, 257 had two parents participating in the study; 36 families had one parent participating (the other partner/parent either was unavailable or declined to participate in this assessment). We did not exclude couples in which only one parent was able to participate in hopes that the other partner would provide data at a later point in time, which indeed was the case. Examination of the demographic data revealed no significant differences between couples with and without data from both partners. Couples were married on average 9.5 (mothers) to 9.7 years (fathers) with a mean of 2.39 children. Parents were predominantly White (88.7% of fathers and 90% of mothers), and in their thirties (mothers’ M = 35.86, SD = 5.82; fathers’ M = 37.35, SD = 6.25). About half (47.7% of fathers and 53.7% of mothers) reported completing at least a Bachelor’s degree. Eighty-three percent of fathers and 45.5% mothers worked full-time, and most families reported income between $40,000 to $79,999 (47.7%), or $80,000 to $119,999 (29.6%). Children (N = 293) were 54.6% girls and 45.4% boys, ages 4–12 (M = 8.3; SD = 2.5).
Almost all of the fathers in the sample (95.8%) but just 15.6% of the mothers were deployed. Both parents had deployed in 11.8% families. The vast majority of parents deployed with the Army (58.5%) or Air National Guard (11.25%), or the Army (12.1%), Navy (4%), Air Force (3.1%), or Marine Reserves (0.31%). About half (54.7%) were deployed more than once, for an average of 2.02 deployments (SD = 1.26); 61.7% of these deployments lasted more than 12 months. Total length of deployments varied widely from less than six months (8.7% of service members) to more than 3 years (12.5% of service members).
Procedures
Participants were recruited through numerous methods, including presentations at predeployment and reintegration events for NG/R families, mailings from the local Veteran’s Administration Medical Center to OIF/OEF/OND veterans, media, and word of mouth. All procedures were approved by the university of Minnesota’s Institutional Review Board. Participant screening and informed consent took place online through the study website. Each participating parent was then directed to a Health Insurance Portability and Accountability Act compliant website to complete self-report measures. Project staff subsequently scheduled an in-home assessment with the family, during which questionnaire and observational data were gathered from parent(s) and target child; afterwards, teachers were contacted to complete surveys. Families were debriefed after the in-home assessment; parents were reimbursed up to $100 and children received a small gift.
Measures
Marital quality
Each spouse completed the Dyadic Adjustment Scale (DAS-7; Hunsley, Best, Lefebvre, & Vito, 2001), a short version of the original 28-item DAS (Spanier, 1976). The scale assesses agreement (three items), dyadic cohesion (three items), and global satisfaction (one item) on a 6-point Likert scale. The scale score was an equally weighted mean of response scores for all items, with higher scores indicating better adjustment. The DAS-7 has well-established criterion and discriminant validity (Hunsley et al., 2001); internal consistency in the present study was α = .866.
Posttraumatic stress symptoms
The Post-Traumatic Stress Checklist (PCL; Weathers, Litz, Herman, Huska, & Keane, 1993) is a 17-item standardized, validated self-report assessing PTSD symptoms as defined by the Diagnostic and Statistical Manual of Mental Disorders–Fourth Edition (American Psychiatric Association, 2000). Previously deployed parents completed the PCL-M (military version), in which the items refer to a traumatic military experience; nondeployed parents completed the PCL-C (civilian version), in which the items refer to any past traumatic experience. Respondents rated the extent to which they were bothered by each symptom in the past month on a 5-point scale; higher average scores indicate more PTSD symptoms. Internal consistency was high for mothers (α = .914) and fathers (α = .948).
Parenting practices
Parenting practices were measured with five previously validated indicators: (a) problem solving outcome, (b) harsh discipline, (c) positive involvement, (d) skill encouragement, and (e) monitoring. Scores were obtained from observation of parent-child interactions during structured Family Interaction Tasks (FITs) originally developed by Patterson, Forgatch, and colleagues at Oregon Social Learning Center (e.g., Dishion, Patterson, & Kavanagh, 1992). FITs included three problem-solving tasks requiring parent(s) and child to address current conflicts, a monitoring task, and two teaching tasks, lasting 40 minutes. An additional problem-solving task, described below, included only parents. The FITs, and the accompanying scoring coder impressions system, have been extensively validated in prior studies conducted in the USA and in Northern Europe. The FIT tasks and the codes demonstrated ecological validity, construct validity, and sensitivity to change with at-risk families (e.g., Bullard et al., 2010; DeGarmo, Patterson, & Forgatch, 2004; Forgatch & DeGarmo, 1999; Gewirtz, DeGarmo, Plowman, August, & Realmuto, 2009; Ogden & Hagen, 2008; Patterson, Forgatch, & Degarmo, 2010).
Trained coders scored FITs using the Coder Impressions system (Forgatch, Knutson, & Mayne, 1992). The Coder Impressions system is a macro coding system designed to assess parenting practices, including verbal and nonverbal (i.e., body posture, facial expression, and tone of voice). Coders individually watch each task and make an overall rating based on intensity, frequency, and duration of each summary code (e.g., empathy, respect, positive reinforcement, etc.). The system evaluates five core parenting practices. Problem solving outcome was scored with a 9-item scale evaluating the quality of parent’s and child’s solution, extent of resolution, satisfaction at the outcome of the discussion, and likelihood the family would put this solution to use (α = .87, ICC = .88). Items were rated on a 5-point Likert scale from 1 (untrue) to 5 (very true). Harsh discipline was measured by an 8-item scale assessing overly strict, authoritarian, erratic, inconsistent, or haphazard parenting practices (α = .75; ICC = .78). Items were rated based on the entire interaction from 1 (never) to 6 (always). Positive involvement was derived from a 10-item scale evaluating parent’s warmth, empathy, encouragement, and affection (α = .75; ICC = .84). Items were rated based on the entire interaction from 1 (never) to 6 (always). Skill encouragement was assessed using an 8-item scale reflecting parent’s ability to promote children’s skill development through encouragement and scaffolding strategies (α = .83; ICC = .72). Items were rated based on teaching tasks from 1 (untrue) to 5 (very true). Monitoring was measured by a 4-item scale assessing parents’ supervision and knowledge of their child’s daily activities (α = .71; ICC = .74). Items were rated from 1 (untrue) to 5 (very true). All scales were averaged to create summary scores, such that higher scores indicated higher positive communication. The final mother and father parenting scores were composites of the five indicators and were scaled from 1–5.
Positive couple communication
Positive couple communication was assessed with a 5-minute conflict discussion adapted from Bullard et al. (2010) and administered as part of the FITs. Partners were asked to rate in order of severity current conflicts related to co-parenting and deployment (e.g., getting back on the same page after deployment). Couples were instructed to attempt to solve the conflict rated as most severe. Couples were left alone during the interactions, which were videotaped. Couples’ communication was assessed with the Positive Communication Scale (Bullard et al., 2010; Zamir, Gewirtz, Labella, DeGarmo, & Snyder, 2016), a 9-item scale assessing expression of humor, affection, empathy, interest in the partner, agreement, positive affect, positive involvement, and engaged body posture. Sample items are: “Showed empathy and genuine concern,” “Used humor in a friendly and supportive way, to set at ease or lighten the situation,” “Was verbally affectionate with partner.” Coders rated duration, intensity, and frequency of behaviors on a 6-point Likert scale ranging from 1 (never) to 6 (always). Items were averaged to create summary scores, such that higher scores indicated higher positive communication. Alphas were .77 for fathers and .76 for mothers. Observers underwent biweekly reliability meetings to minimize observer drift. Inter-rater reliability was assessed for 15% of the videos with different randomly selected coders teams. ICCs were .92 for men’s and .91 for women’s positive communication. To evaluate data structure, we ran exploratory factor analyses in which a one-factor solution was imposed, separately for men and women. The loadings of the positive communication items ranged from 0.34 to 0.71 (M = 0.57) for fathers and 0.32 to 0.70 (M = 0.58) for mothers. Explained variance across the single-factor models ranged from 35% to 39%. Finally, we computed zero-order correlations to test the associations of the scales with marital quality to establish convergent validity (Table 1).
TABLE 1.
Means, Standard Deviations, Sample Size, and Bivariate Correlations Among Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. PTSD mother | — | |||||||||||
| 2. PTSD father | .12† | — | ||||||||||
| 3. Num. deployments | .04 | −.08 | — | |||||||||
| 4. Months deployed | .05 | .12† | .54*** | — | ||||||||
| 5. Pos comm husband | −.13* | −.09 | .04 | −.04 | — | |||||||
| 6. Pos comm wife | −.07 | −.05 | .07 | −.08 | .77*** | — | ||||||
| 7. DAS-7 husband | −.13* | −.27*** | −.07 | −.08 | .24*** | .25*** | — | |||||
| 8. DAS-7 wife | −.23*** | −.19** | .02 | .04 | .19** | .17** | .53*** | — | ||||
| 9. Parenting mother | −.18** | .03 | .01 | −.04 | .38*** | .47*** | .10 | .04 | — | |||
| 10. Parenting father | −.22** | .01 | .00 | .02 | .44*** | .33*** | .08 | .02 | .61*** | — | ||
| 11. Self-esteem-CR | −.18* | −.01 | .02 | −.00 | .04 | .04 | .03 | .07 | .16* | .24** | — | |
| 12. Self-reliance-CR | −.03 | −.06 | −.03 | −.08 | −.05 | −.01 | .05 | −.04 | .19* | .19* | .28*** | — |
| M | 27.01 | 29.12 | 2.02 | 13–24 | 3.59 | 3.66 | 3.56 | 3.53 | 2.41 | 2.28 | 12.48 | 18.68 |
| SD | 9.02 | 11.94 | 1.26 | 2.26 | .84 | .81 | .59 | .64 | .41 | .45 | 2.34 | 4.28 |
| n | 278 | 249 | 293 | 292 | 238 | 238 | 255 | 277 | 271 | 247 | 147 | 147 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 13. School Att.-CR | .09 | .03 | .12† | .10 | .01 | −.04 | −.01 | .03 | −.13* | −.12† | −.50*** | −.33*** |
| 14. Child Dep-CR | .12 | −.01 | .00 | .03 | .10 | .06 | .04 | −.02 | −.09 | .04 | −.38*** | ***23 |
| 15. Adaptive Skill-TR | −.03 | −.08 | .02 | .10 | .10 | .03 | .08 | .06 | .12† | .04 | .31*** | .21* |
| 16. Beh. Severity-TR | .06 | .11 | −.02 | −.05 | −.06 | .02 | −.08 | −.04 | −.02 | −.00 | .34*** | −.21* |
| 17. Inter. Strength-TR | .03 | −.04 | −.03 | .07 | .08 | −.01 | .17* | .11 | .14* | .03 | .17* | .32** |
| 18. Inter. Strength-MR | −.27*** | −.18** | −.12* | −.09 | .08 | .09 | .20** | .31*** | .14* | .07 | .17* | .13 |
| 19. Inter. Strength-FR | −.12* | −.10 | .09 | .03 | .12* | .14* | .30*** | .15* | .12† | .17** | −.22** | .16* |
| 20. Beh. Severity-MR | .31** | .07 | .07 | .03 | .04 | .04 | −.11 | −.09** | −.08 | −.09 | −.21* | −.13 |
| 21. Beh. Severity-FR | .16** | .26*** | −.04 | −.11* | −.06 | −.08 | −.12 | .09 | −.10 | −.12† | .34*** | −.04 |
| 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | |
|---|---|---|---|---|---|---|---|---|---|
| 13. School Att.-CR | — | ||||||||
| 14. Child Dep-CR | .22*** | — | |||||||
| 15. Adaptive Skill-TR | −.04 | −.21** | — | ||||||
| 16. Beh. Severity-TR | .14* | .29*** | −.74*** | — | |||||
| 17. Inter. Strength-TR | −.18** | −.21** | .82*** | −.68*** | — | ||||
| 18. Inter. Strength-MR | −.20*** | −.14† | .19** | −.16** | .26*** | — | |||
| 19. Inter. Strength-FR | −.11 | −.09 | .17* | −.21** | .23*** | .47*** | — | ||
| 20. Beh. Severity-MR | −.20 | .18* | −.36*** | .33*** | −.33*** | −.60*** | −.41*** | — | |
| 21. Beh. Severity-FR | .07 | .16* | −.33*** | .36*** | −.32*** | −.39*** | −.54*** | .59*** | — |
| M | 4.26 | 3.39 | 71.17 | 27.88 | 52.56 | 50.66 | 49.32 | 40.59 | 42.02 |
| SD | 3.84 | 1.86 | 19.77 | 20.97 | 13.20 | 9.91 | 9.64 | 18.92 | 18.30 |
| n | 262 | 174 | 236 | 236 | 202 | 276 | 250 | 275 | 251 |
Notes. Beh. Severity = behavioral severity; Child Dep. = child depression; CR = child report; DAS-7 = Dyadic Adjustment Scale-7; FR = father report; Inter. Strength = interpersonal strength; MR = mother report; Num. Deployments = Number of deployments; Pos Comm = positive communication; PTSD = Posttraumatic Stress Disorder; School att. = School attitudes; TR = teacher report.
p < .001;
p < .01;
p < .05;
P < .10.
Child adjustment
Child adjustment was measured with the Behavioral Assessment Scale for Children (BASC-2; Reynolds & Kamphaus, 2004), including the Parent Rating Scales (PRS), the Teacher Rating Scales (TRS), and the child Self-Report of Personality (SRP). The BASC-2 has established construct validity and convergent validity with other scales such as the Child Behavior Checklist (Achenbach & Rescorla, 2001), good internal consistency, and test-retest reliability (Reynolds & Kamphaus, 2004). The behavioral severity index from the BASC-2 provides a sum score of global problem severity, including hyperactivity, atypicality, attention problems, aggressive behavior, depression, and withdrawal. Cronbach’s as indicated good internal consistency across the subscales (.664–.849). Child adaptive skills and behavior severity were measured with the TRS of the BASC-2. The adaptive skill composite assesses functional communication, adaptability, social skills, leadership, and study skills. Internal consistency was .776–.935 for the adaptability composite, and .826–.938 for the behavioral severity composite. We assessed child’s self-esteem, self-reliance, and negative attitudes toward school using the SRP of the BASC-2. A total score was computed from the three subscales. Internal consistency across age groups and subscales was adequate: self-esteem (.724–.761), self-reliance (.532–.766), and negative attitudes toward school (.772–.814).
The Behavioral and Emotional Rating Scale (BERS-2; Buckley & Epstein, 2004) parent (PRS) and teacher (TRS) rating scales were used to assess children’s interpersonal strength. The scales each contain 15 items describing behaviors that parents and teachers rate from 0 (not at all like the child) to 3 (very much like the child). Scores are summed. The BERS-2 has excellent test-retest reliability, criterion and construct validity (Buckley & Epstein, 2004; Epstein, Cullinan, Ryser, & Pearson, 2002). Alphas were .884 for parent and .960 for teacher report.
The Child Depression Inventory-Short Form (CDI-S; Kovacs, 1983) is a 10-item self-report measure of children’s cognitive, affective, and behavioral symptoms of depression experienced during the prior 2 weeks, rated on a 0–2 scale. A higher mean score reflects greater depressive symptoms. The CDI-S (α = .80) is correlated .89 with the full CDI, correlates highly with other depression measures, and distinguishes clinical from nonclinical samples (Maruish, 2014). The scale demonstrated adequate internal consistency in the current sample (α = .52).
Analytic Strategy
To test the hypothesized family stress model we specified structural equation path models (SEM) with latent variable constructs using Mplus 7.31 (Muthén & Muthén, 1998–2015). To take advantage of the multi-method assessment strategy involving data collected from multiple reporters and multiple methods, we specified measurement of the child adjustment construct as a higher-order latent variable, also known as a second-order or a hierarchical confirmatory factor model (Kline, 2010). A higher-order latent variable is simply a latent variable measured by indicators that are themselves latent variables. The advantage of the higher-order construct is the ability to estimate communality across separate reporters, thus partialling out measurement error related to potential mono-method reporting bias. Using further data reduction of the criterion outcomes and prediction of a higher-order construct is also a more theoretically parsimonious test of the central hypothesis than are separate tests of multiple reporters or methods. Fit of the SEM models was evaluated with several recommended criteria (Byrne, 2011; Kline, 2010) including a non-significant chi-square minimization p value, a comparative fit index above .90, a root mean square error of approximation (RMSEA) lower than .06, and a chi-square ratio (χ2/df) equal to or less than 2.0. Indirect effects and their confidence intervals were estimated with recommended bias-corrected bootstrapped model with 500 sample draws (MacKinnon, Fritz, Williams, & Lockwood, 2007; Preacher & Hayes, 2008).
Missing Data
Models were estimated using full information maximum likelihood (FIML), which uses all available information from the observed data in the SEM analyses. FIML estimates are computed by maximizing the likelihood of a missing value based on observed values in the data. Compared to mean imputation, listwise, or pairwise models, FIML provides more statistically reliable standard errors (Brown et al., 2008; Schafer & Graham, 2002). A missing-values analysis was conducted on the means, variances, and covariances for all study variables presented in Table 1. Little’s chi-square MCAR tests indicated the data were missing at random, Little’s χ2(401) = 441.43, p = .08.
RESULTS
Means, standard deviations, and bivariate correlations for the key study variables are presented in Table 1. Correlations among indicators for each latent variable construct are outlined in dashed lines along the diagonal. Indicator measurement correlations were significant at p < .001 for each construct: self-reported and observed dyadic adjustment, observed parenting practices among mothers and fathers, and child self-reported, teacher-reported, and parent-reported child adjustment scale scores.
We next specified the hypothesized relationships in the theoretical model, first specifying measurement of the criterion construct of child adjustment as a higher-order latent variable measured by (a) child reported self-esteem, self-reliance, negative attitudes toward school, and child depression scales, (b) teacher-reported adaptive skills, behavior severity, and interpersonal strength scales, and (c) mother- and father-reported interpersonal strength and behavioral severity scales. The family process factor of dyadic adjustment was specified by mother’s and father’s couple score for dyadic adjustment and behavioral observation of mothers and fathers during couples’ FITs. The parenting practices factor was specified as the respective effective parenting composite construct scores from the parenting FITs.
First, we tested the main effects of deployment-related variables (numbers and length of parents’ deployments, and fathers’ and mothers’ PTSD symptoms) on the multi-agent construct of child adjustment. Results are presented in Figure 2 in the form of standardized beta paths. The higher-order multi-agent construct of child adjustment obtained excellent factor loadings at the first-order and second-order levels, and the specified SEM model provided adequate fit to the data, χ2 (76) = 126.29, p = .00, CFI = .95, RMSEA = .04; χ2/df = 1.66. Number and length of parents’ deployments were not significantly associated with child adjustment. However, PTSD symptoms of fathers (β = −.17, p < .05) and mothers (β = −.31, p < .001) were negatively associated with the child adjustment construct. In total, the latent SEM path model explained 14% of the variance in child adjustment.
FIGURE 2.
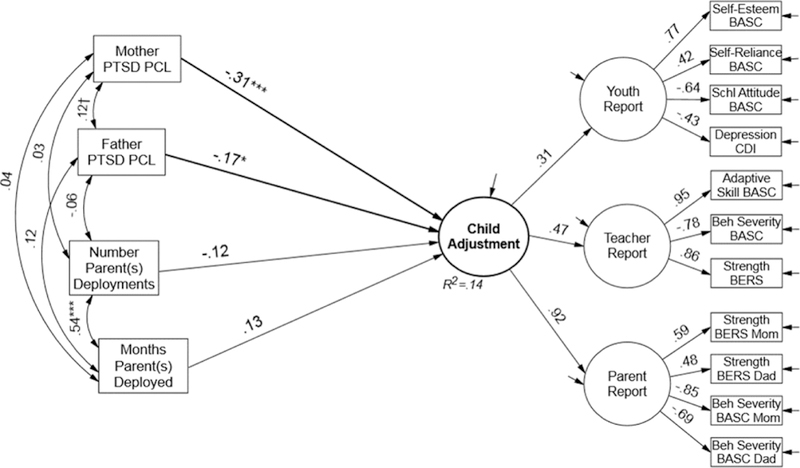
Multi-Agent Structural Equation Path Model for Hypothesized Military Stress Effects on Child Adjustment.
Note: Paths are standardized estimates. Model Fit, χ2(76) = 126.29, p = .00, CFI = .95, RMSEA = .04; χ2/df = 1.66. ***p < .001; **p < .01; *p < .05; †p < .10. Same parent-report residuals covaried with same parent-report residuals among latent variables. BASC = Behavioral Assessment Scale for Children; Beh Severity = behavioral severity; BERS = Behavioral and Emotional Rating Scale; PTSD PCL = Post-traumatic Stress Disorder Checklist; Schl Attitude = School Attitude.
Secondary analyses indicated that among yoked couples, fathers’ PTSD symptoms were significantly higher than mothers’ (M = 29.12 and 27.01, t = 3.59, p < .001). Additionally, for the full sample of yoked and unyoked parents, equality constraints comparing the direct effect paths for mothers’ and fathers’ PTSD symptoms on child adjustment were not statistically different, indicating that although fathers’ levels were higher, both parents’ symptoms independently and equally contributed to child adjustment problems.
Next, we tested the putative mediating role of couples’ dyadic adjustment and parenting practices in the link between fathers’ and mothers’ PTSD symptoms and child adjustment. We also tested the indirect effect of dyadic adjustment on child’s adjustment through parenting practices. Results are presented in Figure 3 in the form of standardized beta paths. Focusing on the primary prediction paths, or the inner model, in general, the family stress model was supported by the data, χ2(158) = 313.31, p = .00, CFI = .90, RMSEA = .05; χ2/df = 1.98. Controlling for deployment factors (i.e., length and number of deployments, and PTSD symptoms), higher levels of dyadic adjustment were positively associated with higher levels of effective parenting (β = .52, p < .001). Effective parenting practices, in turn, were significantly associated with higher levels of child adjustment (β = .26, p < .05). However, counter to expectations, dyadic adjustment was not directly associated with child adjustment.
FIGURE 3.
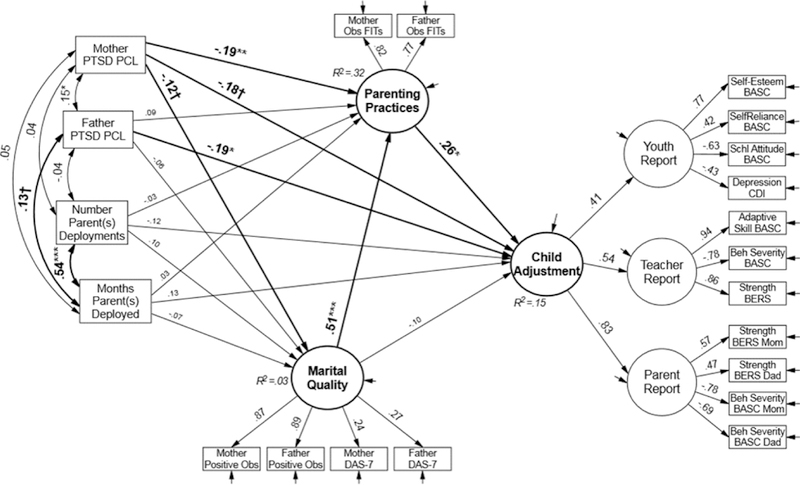
Multi-Agent and Multi-Method Structural Equation Path Model for Hypothesized Social Interaction Learning and Family Stress Model of Military Child Adjustment.
Note: Paths are standardized estimates. Model Fit, χ2(158) = 313.31, p = .00, CFI = .90, RMSEA = .05; χ2/df = 1.98. ***p < .001; **p < .01; *p < .05; †p < .10. Same parent-report residuals covaried with same parent-report residuals among latent variables, same parent observational residuals covaried with same parent observational scores. BASC = Behavioral Assessment Scale for Children; Beh Severity = behavioral severity; BERS = Behavioral and Emotional Rating Scale; Father positive obs = Father (observed) positive communication; Mother positive obs = Mother (observed) positive communication; Obs FITS = observed family interaction tasks; PTSD PCL = Post-traumatic Stress Disorder Checklist; Schl Attitude = School Attitude.
Length and number of deployments were not associated with family process constructs. Mothers’ PTSD symptoms, but not fathers’, were negatively associated with effective parenting practices (β = −.19, p < .05). Thus maternal psychopathology appeared to interfere with observed parenting as expected while paternal psychopathology did not. Finally, we tested the indirect or mediating effects of maternal PTSD symptoms through parenting practices, and the indirect effect of dyadic adjustment through parenting practices. Only dyadic adjustment obtained a significant indirect effect (indirect estimate = .13, t = 2.06, p < .05, 95% C.I. [0.03, 0.26]). We explored whether the association between dyadic adjustment and child adjustment was potentially mediated by effective parenting; results indicated no significant association of dyadic and child adjustment in the absence of effective parenting. Though the indirect path from PTSD symptoms of mothers to child adjustment through parenting practices was not significant, the strong main effect of mothers’ PTSD symptoms on child adjustment was reduced to marginal significance in this model, suggesting partial mediation. Overall, the latent SEM path model explained 15% of the variance or individual differences in the higher-order child adjustment latent variable construct, a large effect size (r = .41, d = .89).
DISCUSSION
Multi-method, multi-informant data from 293 military families partly supported our hypotheses regarding a military family stress model. Number and length of deployments were not associated with dyadic adjustment, parenting, or child adjustment. PTSD symptoms of both fathers and mothers were directly associated with children’s adjustment (Figure 2). Moreover, when parenting practices were included in the model (Figure 3), they mediated the impact of maternal (but not paternal) PTSD symptoms on children’s adjustment. These findings parallel earlier findings that family stressors may impact children primarily via parents’ mental health and their parenting (Grant et al., 2014). In this case the mental health correlates of deployment (i.e., PTSD symptoms) may be more influential for family adjustment than length or number of deployments. It is important to note that for the non-deployed mothers (a majority of the mothers) maternal PTSD symptoms were of unknown origin. Recent literature has demonstrated increased psychopathology among spouses of previously deployed service members compared to civilian norms, or compared to spouses of non-deployed service members (Bjornestad, Schweinle, & Elhai, 2014; Ren-shaw, Rodrigues, & Jones, 2008).
Associations between parental PTSD symptoms and child adjustment have been reported in the military family literature as well as the broader trauma literature (Yehuda, Halligan, & Bierer, 2001), but few studies have utilized multiple informants and methods. Among yoked couples in the present study, both parents’ PTSD symptoms equally and independently contributed to child adjustment problems even though in the overall sample, fathers’ PTSD symptoms were greater than mothers (due to the much higher proportion of combat deployed fathers). Research is emerging to understand how PTSD symptoms might directly and indirectly affect risk for psychopathology in children. For example, Snyder et al. (2016) documented reciprocal cascades among fathers’ and mothers’ PTSD symptoms, and child internalizing and externalizing symptoms over a 2-year period in a sample of military families. Fathers’ and mothers’ positive engagement during parent-child interaction linked their PTSD symptoms and their child’s internalizing symptoms, while coercive behaviors toward their child linked their PTSD symptoms and their child’s externalizing symptoms. The avoidance and emotion dysregulation symptoms characteristic of PTSD may be disturbing to an elementary-aged child (Brockman et al., 2016). Genetic and epigenetic processes may also account for shared environmental variance in psychopathology such that parents vulnerable to PTSD are more likely to have children vulnerable to anxiety, depression, and PTSD (Yehuda et al., 2001).
In this sample of primarily previously deployed fathers and primarily never deployed mothers, mothers’ but not fathers’ PTSD symptoms were significantly negatively associated with observed parenting practices, partially mediating the association between PTSD symptoms and child adjustment. In a similar vein, Allen et al. (2010), examining family stressors among 300 husbands and wives following a deployment, found that ratings of child behavior by fathers were not associated with self-reported deployment related stress, but mothers’ ratings were, concluding that men may have been better at compartmentalizing their roles as fathers and soldiers (i.e., work vs. home). In the current study we further speculate that this population of fathers may be far less involved than mothers in actively parenting their children due to their deployment absences. Indeed, anecdotal data suggest that even when they desire to actively parent, reintegrating fathers find it challenging to reconnect and find their parenting ‘place’ in the family (Walsh et al., 2014). Children are more likely to seek support and care from mothers, and mothers are used to parenting alone, potentially causing a cycle whereby fathers withdraw further. In such situations, it may be that fathers may only gain entry into parenting life when they compartmentalize their deployment-related distress and PTSD symptoms. Longitudinal data are needed to establish whether these relationships remain stable or change over time.
As predicted, better dyadic adjustment was associated with more effective parenting practices. Moreover, dyadic adjustment was not directly associated with child adjustment, suggesting that couple relationship processes may influence children primarily through the couple’s parenting practices rather than the child’s observation of the couple relationship. On the one hand, theoretical models and reviews support the hypothesis that marital relationships may support or interfere with effective parenting (e.g., Belsky, 1984; Pedro, Ribeiro, & Shelton, 2012). Some evidence shows that the effect of negative marital process on child adjustment problems is mediated through parenting behaviors (Katz & Low, 2004; Rhoades et al., 2011); we note, however, that negative marital process, or couple negativity, may not simply be the inverse of positive couple relationship processes (Rogge, Fin-cham, Crasta, & Maniaci, 2016). On the other hand, studies also show direct effects of marital discord on child adjustment independent of parenting (Cummings & Davies, 2002).
These equivocal findings may be sample and measure dependent. Experimental longitudinal multi-method data from our randomized controlled trial of a parenting program (of which the current findings are baseline data) will better inform how marital and parenting domains additively or interactively affect child adjustment in the context of military families. Deployment lifestyles may uniquely impact marital and parenting processes compared to civilian samples. The extended absences of deployment can easily challenge an intimate relationship, with spouses and service members reporting difficulties readjusting to life together after deployment, particularly around couple communication and co-parenting (Knobloch & Theiss, 2012). Our data suggest that improvements in dyadic adjustment might also reap benefits over time to parenting and child adjustment. Longitudinal data on dyadic adjustment and parenting may help explain mutual influences. It would be important to understand, for example, whether an intervention to improve parenting in this population might also reap benefits for dyadic adjustment as has been shown in civilian populations (e.g., Bullard et al., 2010).
The current study is the first to find that more effective observed couple parenting practices were significantly associated with higher levels of child adjustment in a previously deployed military population. The findings are, however, consistent with a large body of civilian literature on the crucial role of parenting practices for children’s behavioral and emotional adjustment and development (e.g., Collins, Maccoby, Steinberg, Hetherington, & Bornstein, 2000; Cox, Mills-Koonce, Propper, & Gariépy, 2010). A key next step for this research is to examine how changes in observed parenting might affect children’s adjustment across development.
Our data are cross-sectional, and therefore we cannot determine the direction of associations. Although our sample was representative of the National Guard/Reserve racial and ethnic demographics of the Midwestern state from which families were recruited, it is not nationally representative of the NG/R nor of the US military. Moreover, the current sample was predominantly middle-income NG/R families, precluding generalization to active-duty military families as well as to lower-income military families. Finally, measurement of spouse PTSD (via the PCL-C) did not reveal the origins of the civilian spouses’ PTSD symptoms, which may or may not have been related to deployed service members’ PTSD symptoms.
Despite its limitations, this is the first study we know of to examine a military family stress model in the context of parenting, dyadic, and child adjustment following deployment. The study employed a rigorous measurement strategy with convergence of reporters from multiple domains observing children’s adjustment, providing preliminary support for a military family stress model, and obtaining a large effect of hypothesized observed behavioral predictors of multiple reporter outcomes. Parents’ PTSD symptoms, rather than length or number of deployments, appear to be the key family stressor for families following deployment, exerting effects on child adjustment both indirectly through parenting (for mothers’ PTSD symptoms) and directly (for both parents). Prior research on parenting practices has demonstrated that improvements in parenting as a result of intervention may reap benefits not only to child and dyadic adjustment, but also to parental depression (Patterson, DeGarmo, & Forgatch, 2004). However, no research has yet examined whether parenting interventions may be beneficial in reducing other parental psychopathology (i.e., PTSD symptoms). It is hoped that the present findings will lay a foundation for a fuller and more robust understanding of parenting, child, and dyadic relationships in the wake of a parent’s deployment to war.
Acknowledgments
This research was funded by a grant from the National Institute of Drug Abuse (R01-DA030114) to the first author, and in part, by grant P50 DA035763.
REFERENCES
- Achenbach TM, & Rescorla L. (2001). ASEBA school-age forms & profiles. Burlington, VT: Aseba. [Google Scholar]
- Allen ES, Rhoades GK, Stanley SM, & Markman HJ (2010). Hitting home: Relationships between recent deployment, post-traumatic stress symptoms, and marital functioning for Army couples. Journal of Family Psychology, 24, 280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. [Google Scholar]
- Barnett MA (2008). Economic disadvantage in complex family systems: Expansion of family stress models. Clinical Child and Family Psychology Review, 11, 145–161. doi: 10.1007/s10567-008-0034-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsky J. (1984). The determinants of parenting: A process model. Child Development, 55, 83–96. [DOI] [PubMed] [Google Scholar]
- Bjornestad AG, Schweinle A, & Elhai JD (2014). Measuring secondary traumatic stress symptoms in military spouses with the posttraumatic stress disorder checklist military version. The Journal of Nervous and Mental Disease, 202, 864–869. doi: 10.1097/NMD.0000000000000213 [DOI] [PubMed] [Google Scholar]
- Bowen GL, Martin JA, & Mancini JA (2013). The resilience of military families: Theoretical perspectives In Bowen GL, Martin JA, & Mancini JA (Eds.), Handbook of family theories (pp. 417–436). New York: Routledge. [Google Scholar]
- Brockman C, Snyder J, Gewirtz A, Gird SR, Quattlebaum J, Schmidt N. et al. (2016). Relationship of service members’ deployment trauma, PTSD symptoms, and experiential avoidance to postdeployment family reengagement. Journal of Family Psychology, 30, 52–62. doi: 10.1037/fam0000152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CH, Wang W, Kellam SG, Muthen BO, Petras H, Toyinbo P. et al. (2008). Methods for testing theory and evaluating impact in randomized filed trials: Intent-to-treat analysis for integrating the perspective of person, place and time. Drug and Alcohol Dependence, 95, S74–S104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckley JA, & Epstein MH (2004). The Behavioral and Emotional Rating Scale-2 (BERS-2): Providing a comprehensive approach to strength-based assessment. The California School Psychologist, 9(1), 21–27. [Google Scholar]
- Bullard L, Wachlarowicz M, DeLeeuw J, Snyder J, Low S, Forgatch M. et al. (2010). Effects of the Oregon model of Parent Management Training (PMTO) on marital adjustment in new stepfamilies: A randomized trial. Journal of Family Psychology, 24, 485–496. doi: 10.1037/a0020267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne BM (2011). Structural equation modeling with Mplus: Basic concepts, applications, and programming. New York: Routledge. [Google Scholar]
- Card NA, Bosch L, Casper DM, Wiggs CB, Hawkins SA, Schlomer GL et al. (2011). A meta-analytic review of internalizing, externalizing, and academic adjustment among children of deployed military service members. Journal of Family Psychology, 25, 508–520. doi: 10.1037/a0024395 [DOI] [PubMed] [Google Scholar]
- Chandra A, Burns RM, Tanielian T, & Jaycox LH (2011). Understanding the impact of deployment on children and families: Findings from a pilot study Risk and resilience in US military families. New York: Springer. [Google Scholar]
- Collins WA, Maccoby EE, Steinberg L, Hetherington EM, & Bornstein MH (2000). Contemporary research on parenting: The case for nature and nurture. The American Psychologist, 55, 218–232. [PubMed] [Google Scholar]
- Conger RD, Wallace LE, Sun Y, Simons RL, McLoyd VC, & Brody GH (2002). Economic pressure in African American families: A replication and extension of the family stress model. Developmental Psychology, 38, 179–193. [PubMed] [Google Scholar]
- Cox MJ, Mills-Koonce R, Propper C, & Gariépy J-L (2010). Systems theory and cascades in developmental psychopathology. Development and Psychopathology, 22, 497–506. doi: 10.1017/S0954579410000234 [DOI] [PubMed] [Google Scholar]
- Cozza SJ (2016). Parenting in military families faced with combat-related injury, illness, or death In Gewirtz AH & Youssef AM (Eds.), Parenting and children’s resilience in military families (pp. 151–173). New York: Springer Press. [Google Scholar]
- Cummings EM, & Davies PT (2002). Effects of marital conflict on children: Recent advances and emerging themes in process-oriented research. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 43, 31–63. [DOI] [PubMed] [Google Scholar]
- Davis L, Hanson SK, Zamir O, Gewirtz AH, & DeGarmo DS (2015). Associations of contextual risk and protective factors with fathers’ parenting practices in the postdeployment environment. Psychological Services, 12, 250–260. doi: 10.1037/ser0000038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Defense Manpower Data Center (2015). Military family life project: Active duty spouse study, longitudinal analyses 2010–2012. Alexandria, VA: Author. [Google Scholar]
- DeGarmo DS, Patterson GR, & Forgatch MS (2004). How do outcomes in a specified parent training intervention maintain or wane over time? Prevention Science, 5(2), 73–89. [DOI] [PubMed] [Google Scholar]
- Dekel R, & Monson CM (2010). Military-related post-traumatic stress disorder and family relations: Current knowledge and future directions. Aggression and Violent Behavior, 15, 303–309. doi: 10.1016/j.avb.2010.03.001 [DOI] [Google Scholar]
- Department of Defense (2009). Profile of the military community. Retrieved from http://download.militaryonesource.mil/12038/MOS/Reports/2009-Demographics-pdf
- Dishion TJ, Patterson GR, & Kavanagh KA (1992). An experimental test of the coercion model: Linking theory, measurement, and intervention. New York: Guilford Press; Retrieved from http://psycnet.apa.org/psycinfo/1992-98237-012 [Google Scholar]
- Downey G, & Coyne JC (1990). Children of depressed parents: An integrative review. Psychological Bulletin, 108(1), 50–76. [DOI] [PubMed] [Google Scholar]
- Elder GH Jr, Nguyen TV, & Caspi A. (1985). Linking family hardship to children’s lives. Child Development, 56, 361–375. [PubMed] [Google Scholar]
- Epstein MH, Cullinan D, Ryser G, & Pearson N. (2002). Development of a scale to assess emotional disturbance. Behavioral Disorders, 28, 5–22. [Google Scholar]
- Flake EM, Davis BE, Johnson PL, & Middleton LS (2009). The psychosocial effects of deployment on military children. Journal of Developmental and Behavioral Pediatrics, 30, 271–278. doi: 10.1097/DBP.0b013e3181aac6e4 [DOI] [PubMed] [Google Scholar]
- Forgatch MS, & DeGarmo DS (1999). Parenting through change: An effective prevention program for single mothers. Journal of Consulting and Clinical Psychology, 67, 711–724. [DOI] [PubMed] [Google Scholar]
- Forgatch MS, Knutson N, & Mayne T. (1992). Coder impressions of ODS lab tasks. Eugene, OR: Oregon Social Learning Center. [Google Scholar]
- Forgatch MS, Patterson GR, Degarmo DS, & Beldavs ZG (2009). Testing the Oregon delinquency model with 9-year follow-up of the Oregon Divorce Study. Development and Psychopathology, 21, 637–660. doi: 10.1017/S0954579409000340 [DOI] [PubMed] [Google Scholar]
- Gartstein MA, & Fagot BI (2003). Parental depression, parenting and family adjustment, and child effortful control: Explaining externalizing behaviors for preschool children. Journal of Applied Developmental Psychology, 24, 143–177. [Google Scholar]
- Gewirtz AH, DeGarmo DS, Plowman EJ, August G, & Realmuto G. (2009). Parenting, parental mental health, and child functioning in families residing in supportive housing. The American Journal of Orthopsychiatry, 79, 336–347. doi: 10.1037/a0016732 [DOI] [PubMed] [Google Scholar]
- Gewirtz AH, Erbes CR, Polusny MA, Forgatch MS, & Degarmo DS (2011). Helping military families through the deployment process: Strategies to support parenting. Professional Psychology, Research and Practice, 42, 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewirtz AH, Polusny MA, DeGarmo DS, Khaylis A, & Erbes CR (2010). Posttraumatic stress symptoms among National Guard soldiers deployed to Iraq: Associations with parenting behaviors and couple adjustment. Journal of Consulting and Clinical Psychology, 78, 599–610. doi: 10.1037/a0020571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant KE, McMahon SD, Carter JS, Carleton RA, Adam EK, & Chen E. (2014). The influence of stressors on the development of psychopathology In Lewis M. & Rudolph KD (Eds.), Handbook of developmental psychopathology (pp. 205–223). New York: Springer; Retrieved from http://link.springer.com/chapter/10.1007/978-1-4614-9608-3_11 [Google Scholar]
- Hunsley J, Best M, Lefebvre M, & Vito D. (2001). The seven-item short form of the Dyadic Adjustment Scale: Further evidence for construct validity. The American Journal of Family Therapy, 29, 325–335. [Google Scholar]
- Katz LF, & Low SM (2004). Marital violence, co-parenting, and family-level processes in relation to children’s adjustment. Journal of Family Psychology, 18, 372–382. doi: 10.1037/0893-3200.18.2.372 [DOI] [PubMed] [Google Scholar]
- Kline RB (2010). Principles and practice of structural equation modeling (Vol. 3). New York: The Guilford Press. [Google Scholar]
- Knobloch LK, & Theiss JA (2012). Experiences of US military couples during the post-deployment transition. Applying the relational turbulence model. Journal of Social and Personal Relationships, 29, 423–450. [Google Scholar]
- Kovacs M. (1983). The Children’s Depression Inventory. A self-rated depression scale for school-aged youngers. Unpublished manuscript, University of Pittsburgh, Pittsburgh, PA. [Google Scholar]
- Lavee Y, McCubbin HI, & Patterson JM (1985). The double ABCX model of family stress and adaptation: An empirical test by analysis of structural equations with latent variables. Journal of Marriage and Family Counseling, 47, 811–825. doi: 10.2307/352326 [DOI] [Google Scholar]
- Lester P, Peterson K, Reeves J, Knauss L, Glover D, Mogil C. et al. (2010). The long war and parental combat deployment: Effects on military children and at-home spouses. Journal of the American Academy of Child and Adolescent Psychiatry, 49, 310–320. [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fritz MS, Williams J, & Lockwood CM (2007). Distribution of the product confidence limits for the indirect effect: Program PRODCLIN. Behavior Research Methods, 39, 384–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansfield AJ, Kaufman JS, Engel CC, & Gaynes BN (2011). Deployment and mental health diagnoses among children of US Army personnel. Archives of Pediatrics & Adolescent Medicine, 165(11), 999–1005. doi: 10.1001/archpediatrics.2011.123 [DOI] [PubMed] [Google Scholar]
- Maruish ME (2014). The use of psychological testing for treatment planning and outcomes assessment: Volume 2: Instruments for children and adolescents. London, UK: Routledge. [Google Scholar]
- Meadows SO, Tanielian T, Karney BR, Schell TL, Griffin BA, Jaycox LH et al. (2016). The deployment life study. RAND Corporation. Retrieved from http://www.rand.org/content/dam/rand/pubs/research_reports/RR1300/RR1388/RAND_RR1
- Muthén LK, & Muthén BO (1998-2015). Mplus user’s guide (7th ed.). Los Angeles, CA: Author. [Google Scholar]
- Ogden T, & Hagen KA (2008). Treatment effectiveness of parent management training in Norway: A randomized controlled trial of children with conduct problems. Journal of Consulting and Clinical Psychology, 76, 607–621. doi: 10.1037/0022-006X [DOI] [PubMed] [Google Scholar]
- Oshri A, Lucier-Greer M, O’Neal CW, Arnold AL, Mancini JA, & Ford JL (2015). Adverse childhood experiences, family functioning, and resilience in military families: A pattern-based approach. Family Relations, 64, 44–63. doi: 10.1111/fare.12108/full [DOI] [Google Scholar]
- Patterson GR, DeGarmo D, & Forgatch MS (2004). Systematic changes in families following prevention trials. Journal of Abnormal Child Psychology, 32, 621–633. [DOI] [PubMed] [Google Scholar]
- Patterson GR, Forgatch MS, & Degarmo DS (2010). Cascading effects following intervention. Development and Psychopathology, 22, 949–970. doi: 10.1017/S0954579410000568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedro MF, Ribeiro T, & Shelton KH (2012). Marital satisfaction and partners’ parenting practices: The mediating role of coparenting behavior. Journal of Family Psychology, 26, 509–522. doi: 10.1037/a0029121 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. [DOI] [PubMed] [Google Scholar]
- Ramchand R, Rudavsky R, Grant S, Tanielian T, & Jaycox L. (2015). Prevalence of, risk factors for, and consequences of posttraumatic stress disorder and other mental health problems in military populations deployed to Iraq and Afghanistan. Current Psychiatry Reports, 17(5), 1–11. [DOI] [PubMed] [Google Scholar]
- Renshaw KD, Rodrigues CS, & Jones DH (2008). Psychological symptoms and marital satisfaction in spouses of Operation Iraqi Freedom veterans: Relationships with spouses’ perceptions of veterans’ experiences and symptoms. Journal of Family Psychology, 22, 586–594. doi: 10.1037/0893-3200.22.3.586 [DOI] [PubMed] [Google Scholar]
- Reynolds CR, & Kamphaus RW (2004). BASC-2: Behavior assessment system for children. San Antonio, TX: Pearson. [Google Scholar]
- Rhoades KA, Leve LD, Harold GT, Neiderhiser JM, Shaw DS, & Reiss D. (2011). Longitudinal pathways from marital hostility to child anger during toddlerhood: Genetic susceptibility and indirect effects via harsh parenting. Journal of Family Psychology, 25, 282–291. doi: 10.1037/a0022886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogge RD, Fincham FD, Crasta D, & Maniaci MR (2016). Positive and negative evaluation of relationships: Development and validation of the Positive-Negative Relationship Quality (PN-RQ) scale. Psychological Assessment, October 13, 2016, [Epub ahead of print]. doi: 10.1037/pas0000392 [DOI] [PubMed] [Google Scholar]
- Schafer JL, & Graham JW (2002). Missing data: Our view of the state of the art. Psychological Methods, 7, 147–177. [PubMed] [Google Scholar]
- Sheppard SC, Weil Malatras J., & Israel AC (2010). The impact of deployment on U.S. military families. The American Psychologist, 65, 599. [DOI] [PubMed] [Google Scholar]
- Siegel BS, Davis BE, & Committee on Psychosocial Aspects of Child and Family Health and Section on Uniformed Services (2013). Health and mental health needs of children in US military families. Pediatrics, 131, e2002–e2015. doi: 10.1542/peds.2013-0940 [DOI] [PubMed] [Google Scholar]
- Simons LG, Wickrama KAS, Lee TK, Landers-Potts M, Cutrona C, & Conger RD (2016). Testing family stress and family investment explanations for conduct problems among African American adolescents. Family Relations, 78, 498–515. doi: 10.1111/jomf.12278 [DOI] [Google Scholar]
- Snyder J, Gewirtz A, Schrepferman L, Gird SR, Quattlebaum J, Pauldine MR et al. (2016). Parent-child relationship quality and family transmission of parent posttraumatic stress disorder symptoms and child externalizing and internalizing symptoms following fathers’ exposure to combat trauma. Development and Psychopathology, 28, 947–969. doi: 10.1017/S095457941600064X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanier GB (1976). Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and Family Counseling, 38, 15–28. doi: 10.2307/350547 [DOI] [Google Scholar]
- Walsh TB, Dayton CJ, Erwin MS, Muzik M, Busuito A, & Rosenblum KL (2014). Fathering after military deployment: Parenting challenges and goals of fathers of young children. Health & Social Work, 39, 35–44. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, & Keane TM (1993). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility (Vol. 141). Presented at the annual convention of the international society for traumatic stress studies, San Antonio, TX. [Google Scholar]
- Yehuda R, Halligan SL, & Bierer LM (2001). Relationship of parental trauma exposure and PTSD to PTSD, depressive and anxiety disorders in offspring. Journal of Psychiatric Research, 35, 261–270. [DOI] [PubMed] [Google Scholar]
- Zamir O, Gewirtz AH, Labella M, DeGarmo DS, & Snyder J. (2016). Experiential avoidance, communication, and marital quality in intimate relationships of military couples. Manuscript submitted for publication. [Google Scholar]


