Abstract
Background
The objective of this study was to utilize a human-centered approach in designing a diet app that would assist in management of patients with metabolic syndrome.
Methods
A convenience sample of 10 dietetic interns (DIs) who were attending their informatics rotation at the City University of New York School of Public Health and Health Policy (CUNY GSPHHP) were recruited during October 2017. The study was conducted in two phases. In phase 1, the DIs received a tutorial on the use of human-centered approach in designing mobile health applications. In phase 2, the DIs were provided a case study for which they designed an app for patients to manage metabolic syndrome using a human centered approach. The goal of phase 2 was to identify the features that were believed to be most important when designing this metabolic syndrome app. An initial questionnaire was administered to the DIs to gather information on their socio-demographics, prior training in nutrition, smart phone usage, perceptions about food logs, and calorie intake calculations. Subsequent questionnaires gathered information from the DIs on their preferred diet app components, app features, rankings of the features, and mock representations of the diet app with the selected features.
Results
The DIs were enrolled in the supervised practice component of their training to be Registered Dietitian Nutritionists (RDNs). Fifty percent of them had previously worked in a nutrition-related field. One-third of them were currently using a nutrition app. The top five features of the proposed diet app which the DIs identified as very important included (I) personalization of the app based on user preferences (80%, n=8); (II) disease specific education tips (90%, n=9); (III) ability to track progress (80%; n=8); (IV) reminders (70%, n=7) and (V) reinforcement based on user feedback (50%, n=5). In translating the identified features into functional requirements, majority of the DIs felt that the five key features identified should incorporate the following components: (I) personalization of the app should comprise information on medical factors, personal information, personal preferences, and recording weights; (II) disease specific educational tips should comprise information on food selections, low sodium options, and recipes for diabetes; (III) tracking progress should comprise features for storing audio files, viewing previous logs and uploading photos into a library; (IV) reminders should comprise daily messages to the users from the app; and (V) reinforcement should comprise provisions to enter motivational messages.
Conclusions
Our study lends support to the need for utilizing human-centered design (HCD) approaches in developing e-health dietary apps as well other non-diet related apps. App developers are encouraged to incorporate user characteristics, needs and preferences using a HCD framework that will allow for reproducibility, tailoring, user satisfaction, and effectiveness assessments.
Keywords: Diet app, nutrition app, human-centered design (HCD), chronic diseases, mhealth
Introduction
The proliferation of mobile health apps has fostered their use in delivering health-related behavior change interventions. More than 70% of Americans and Australians, as well as 60% of Europeans, regularly use a smartphone and/or tablet (1,2). Mobile health apps have been designed to manage chronic diseases and associated co-morbidities, and for weight loss, fitness advice, nutrition counseling, overall health and wellness. These apps have the potential to guide behavior change through education, diet and activity tracking, and personalized health advice. Diet apps have continually evolved in their utility and popularity, owing to the critical role of diet in the self-management of chronic diseases. Diet modifications and energy restriction, along with healthy lifestyle changes, have been recommended as one of the most effective interventions to prevent, manage, and reverse chronic conditions (3,4). New and innovative diet apps allow for dietary data collection, internet-based dietary self-monitoring, and online food databases, to promote ease of recording.
These apps can also include large food databases to enable users identify food products easily in order to enhance the diet recording process (5). In addition, individuals can receive personalized feedback based on their input, which can further generate educational and health behavior change interventions. Mobile apps have diverse features including diet, weight, and physical activity tracking, channels of communication, resource sections to learn more information about specific diseases, community support forums to enable interaction between individuals with similar disease conditions, camera and audio functions to facilitate digital dietary recording. Additional features include progress updates, goal-setting, instant tailored feedback, and many more (5). These functions collectively support disease management and lifestyle behavior change (6). Several studies have assessed the role of diet monitoring for chronic conditions using mobile Health apps (5-8).
Many methods exist for capturing dietary intake information; however, the process remains a challenge. Some common methods include 24-hour recall, food frequency questionnaires, and food records (5). Nevertheless, obstacles in dietary data collection make it difficult to accurately measure diet and nutrient consumption. These include inaccuracies with diet recall, lack of consistency in diet reporting, and the overall burden of diet recording among end users (5). The rise of diet apps have significantly mitigated these challenges by enabling patients to record their food consumption using their smartphones. Innovative technologies allow patients to monitor caloric intake and dietary patterns with ease, by improving the accuracy of dietary data collection and analysis, while reducing the burden on the patient to record their own diet (5). Many studies have focused on the role of diet in conjunction with physical activity and other lifestyle modifications for managing metabolic syndrome, a cluster of conditions including obesity, diabetes, hypertension and hyperlipidemia. However, fewer have studied the effects of diet alone (3). Results suggest that diet alone can be a useful solution for those with metabolic syndrome (3). Prior results have shown high usability and user satisfaction scores for the four developed apps that assist in managing different conditions that patients with metabolic syndrome suffer from (7).
Findings suggest the relevant role which diet apps play in the management of metabolic syndrome. However, existing literature indicates that the efficacy of such apps remains unclear and critical gaps persist in the balance between the user needs and the services provided by the app (9,10). The volume of diet apps available for download is overwhelming to consumers, making it difficult to decide on which ones are likely to meet consumer needs (11). Evidence on the optimal number and combination of app features, behavior change techniques, and user input to maximize user engagement and intervention efficacy are needed (12).
Human-centered design (HCD) approach can facilitate to create more useful and effective apps (13). HCD approach aims to bridge the gap between what users want in an app and what the designers are providing by involving the end user throughout the product development and testing process especially in terms of safety and user experience (13,14). Given the relevance of the HCD approach, we conducted a pilot study using mixed methods to design a diet app that would assist dietetic interns (DIs) to help manage patients with metabolic syndrome. To the best of our knowledge, this is the first study to gather perspectives of the DIs that they believe to be most important when designing an app for patients with metabolic syndrome.
Methods
A convenience sample of 10 DIs who were attending their informatics rotation at the City University of New York School of Public Health and Health Policy (CUNY SPHHP) were recruited during October 2017. The study was conducted in two phases. In phase 1, the DIs received a tutorial on the use of human-centered approach in the design of mobile applications for health (apps.). In phase 2, the DIs were provided a case study for which they designed an app for patients to manage metabolic syndrome using a human centered approach. The goal of phase 2 was to identify the features that were believed to be most important when designing this metabolic syndrome app. Sketching was employed by the DI users to identify the various ways of displaying the app content. An initial questionnaire was developed to gather information on socio-demographics, prior training in nutrition, smart phone usage, perceptions about food logs, and calorie calculation techniques among the DIs. The DIs were asked a series of open-ended questions to record the diet app features that would be essential to assist individuals to manage metabolic syndrome. These questions gathered information related to (I) essential components of food log, (II) caloric calculation, (III) food monitoring, (IV) personalized messaging, (V) home-based monitoring of a food log and (VI) listing of 5 essential features that they believed should be part of the nutrition app to help individuals manage metabolic syndrome.
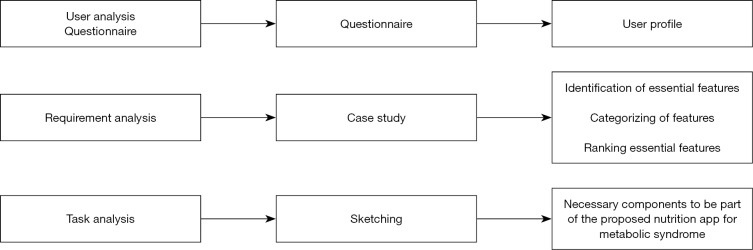
The DIs were also asked to sketch the elements of food log and other essential features that might be useful to have in a nutrition app for individuals with metabolic syndrome. The features identified were classified into broad categories including (I) personalization, (II) educational messages, (III) tracking progress, (IV) reminders, (V) positive reinforcement, (VI) chat, (VII) food log, (VIII) ability to communicate, and (IX) other resources. The DIs were then asked to rank the features on a 4-point Likert scale ranging from very important to not important at all. Lastly the DIs were again asked to utilize the sketching method to organize the categories and the essential features within each category to describe the most important screens of the proposed nutrition app. User sketching can be utilized for establishing user insight into design ideas (15,16). Enabling users to sketch their ideas can facilitate reflection and encourage deeper interpretation and analysis in HCD (16). The users were asked to sketch ideas for specific tasks. The number of elements in each design was counted (17). A design framework for the procedure is provided (Figure 1). This study was approved by the CUNY Graduate School of Public Health and Health Policy’s Institutional Review Board (IRB Number: 2017-1095).
Figure 1.
Design framework for the Diet App.
Variables assessed
Information on the following variables was gathered;
-
User analysis
❖ Socio-demographics: information was gathered on the DIs employment status, years working in public health, any nutrition training, and their experience practicing in the field related to nutrition.
❖ Prior use of Nutrition apps: information was gathered on current or any prior use of nutrition apps, smart phone usage.
❖ Food log: information was collected on participants perceptions about food log and whether they currently kept a food log or not.
-
Requirement analysis A series of open-ended questions gathered information on the essential features that the nutrition app should have. The questions focused on (i) essential food log features, (ii) daily caloric intake assessment, (iii) ongoing diet monitoring, (iv) current methods of recording a food log at home, (v) challenges of recording food logs at home. The DIs were asked to sketch a sample food log. Further, they were given a case scenario to list five essential features a diet app should have to assist individuals with metabolic syndrome.
❖ Diet app categories: the most common categories of the proposed diet app were derived from the initial assessment conducted with the DIs. These categories included: (i) personalization, (ii) disease specific educational tips, (iii) progress updates, (iv) reminders, (v) positive reinforcement, (vi) chat, (vii) tracking, (viii) food log, (ix) communicate, (x) resource section, (xi) other features not mentioned. Information was gathered on the importance of 11 categories according to a 4-point Likert scale ranging from very important to not important at all. Participants were also asked to provide a qualitative description explaining why they ranked features the way they did.
❖ Specific features of the proposed diet app: a list of 50 features were derived from the analysis of the qualitative data gathered during the assessment of the diet app categories as described above. Participants were asked to assign each of the 50 specific diet app features into one of the 11 categories. Participants ranked the features on a 4-point Likert scale ranging from very important to not important at all. Participants were also asked to provide a qualitative description explaining why they ranked features the way they did.
❖ Sketching: participants were asked to sketch their ideas about the proposed nutrition app. These sketches illustrated which features the DI deemed most important when designing a nutrition app for individuals with metabolic syndrome.
Statistical analysis
Descriptive analysis was conducted for various continuous and categorical variables. The results were reported as frequencies and percentage distributions. Thematic analysis was carried out on the qualitative data to identify common features across the participants’ ratings. Quantitative information was derived by making a numerical count of the necessary features within each sketch that might be useful for the newly proposed nutrition app. Features that appeared frequently from more than one participant indicate perceived utility to the task in hand. All analysis was performed using SAS v9.4.
Results
User characteristics
Results showed that the DIs were mostly entering supervised practice from a student background. (90%, n=9). One-third of them were employed part-time (30%, n=3). Less than half of them had worked previously in public health (40%, n=4). Fifty percent (n=5) of them had worked previously in nutrition related field. Only 20% (n=2) had practiced previously as a nutritionist or non-registered dietician (RD). More than half of the DIs owned an iPhone (80%, n=8), while 20% (n=2) owned an Android. One-third of them were currently using a nutrition app (30%, n=3). Less than half of the DIs reported keeping a food log from time to time.
Requirement analysis
The DIs were given a case study to elicit features that would be essential parts of a diet app to be designed specifically to help metabolic syndrome patients between 18 and 65 years of age, having low to high literacy levels, and residing in urban settings. Metabolic syndrome is a cluster of conditions including increased blood pressure, high blood sugar, obesity and abnormal triglyceride levels-which increase the risk of cardiovascular diseases (3). Findings of the case study identified that the following components should be included in the proposed diet app: socio-demographic information, medical profile, food log, diet schedule, ability to set and track the progress of goals, and resource component. Elements of the food log that were identified as most common included portion size (90%, n=9), food name (80%, n=8), time/setting food consumed (60%, n=6), food group (40%, n=4), nutrient information (30%, n=3), and how food was prepared (30%, n=3). Almost all the participants believed that patients should record their food log daily (90%, n=9), while 40% (n=4) felt that users should be able to set the amount of times they can record their diet. The most common methods that DIs reported measuring calorie intake included using a food label and determining portion sizes in reference to a fistful or handful (30%, n=3). While participants felt that patients should be able to calculate calorie content in their diet on a daily basis, they also recognized that food labels listing calories may only be acceptable for packaged foods, and this was a major limitation. DIs reported that dietary recommendations based on existing disease type was most important to tailor messages. Some of the common challenges related to maintaining food log included meal prepared by someone else, or when a meal is eaten at a restaurant (40%, n=4), inputting information related to various food items (30%, n=3), forgetfulness (30%, n=3), and the time it can take to record food intake (30%, n=3). Five features that were identified as essential to the proposed diet app included ability to receive reinforcement (40%, n=4) based on user input, recommendations about healthy food choices, reminders to the users to report food intake, ability for the app to count calories, nutrient tracking, recipes, and a general information section (30%, n=3).
Task analysis: ranking of the specific components identified to be included in the diet app
The DIs ranked the specific diet app features using a 4-point Likert scale (Table 1). One hundred percent of the DIs (n=10) ranked medical factors, weight recording, ability to maintain food logs including ability to enter food name and enter portion size as very important features. More than half of the DIs also ranked calorie intake (90%, n=9), ability to calculate carbohydrate count (90%, n=9), enter measurements and readings’ (90%, n=9), ability to view previous logs (90%, n=9), and type of meals (80%, n=8), as very important. Fifty percent (n=5) of the DIs indicated that receiving advisement about how much insulin one should take with meals was very important. More than half of the DIs thought that having their app sync with an individual calendar (70%, n=7), access to other books (70%, n=7), and ability to communicate with a clinician (60%, n=6) were somewhat important. Half of the participants (50%, n=5) also found it somewhat important to share information with friends, have access to scientific literature in an easy to understand format, and have access to external websites (Table 1).
Table 1. DI rankings of the specific components identified to be included in the diet app.
| Components | Very important |
|---|---|
| Information related to medical factors | 100% [10] |
| Weight recording | 100% [10] |
| Enter food logs | 100% [10] |
| Enter food name | 100% [10] |
| Enter portion size | 100% [10] |
| Calorie intake | 90% [9] |
| Enter measurements/readings | 90% [9] |
| Calculate carbohydrate count | 90% [9] |
| Able to view previous food log | 90% [9] |
| Type of meals | 80% [8] |
| Low sodium options | 80% [8] |
| Enter personal information | 80% [8] |
| Enter lab values | 80% [8] |
| Calculate caloric count | 80% [8] |
| Physical activity | 70% [7] |
| Foods to eat | 70% [7] |
| Foods not to eat | 70% [7] |
| Recipes for diabetes (low carbs) and hypertension (low salt) alone | 70% [7] |
| Combined recipes for both diabetes and hypertension | 70% [7] |
| Information on carbs | 70% [7] |
| Specific nutrients intake | 70% [7] |
| Personal preferences | 60% [6] |
| Number of meals | 60% [6] |
| Information on fat types | 60% [6] |
| Motivational messages | 60% [6] |
| Ability to communicate with dietician | 60% [6] |
DI, dietetic intern.
User preferences
The DIs ranked the essential diet app features based on their importance (Table 2). Qualitative feedback from the DIs was also gathered to explain the rankings chosen. The ability to personalize the app based on user preferences (80%; n=8), disease specific education tips (90%; n=9), ability to track progress (80%; n=8), reminders (70%; n=7) and reinforcement based on user feedback (50%, n=5) were ranked as very important features of the proposed diet app. Forty percent (n=4) believed that the chat function was somewhat important, while half of the participants (50%, n=5) perceived it as neutral, and one participant (10%, n=1) believed it was not important at all. Hundred percent (n=10) of the DIs believed that a food log would be very important feature of the proposed diet app. Having an information resource section (60%, n=6) in the proposed diet app was also perceived to be an important feature. Content analysis was performed to identify the rationale behind the rankings assigned to the various diet app features (Table 2). The DIs believed that obtaining relevant, credible feedback was very important because patients should be able to receive accurate information from their specific provider. They felt that “talking to a medical professional when a question arises provides a sense of safety and security.” Additionally, having the ability to communicate with a physician will help PMDs to have a better sense of their patients’ current health status and be able to give advice based on the patients’ most recent conditions. Similarly, “tracking (patient) progress will also be important to share with their doctor or RD.” The app would be much more helpful “if they can reach out to a dietitian if they have questions.” Some DIs believed it might be burdensome if notifications came too often and that “reminders could be important, but some people (may) choose to ignore or turn them off.” Notifications are important “so that the person remembers, but (the DI was) not sure it is necessary to record every day (since it) could become annoying.” App appearance, design, and ease of app use appeared less frequently in the content analysis. Not many DI believed that ‘app appearance’ was important; however, some believed that “personalized content appearance would make the app more enjoyable” and that patients “should be able to pick (the) screen used the most, but (the app) should not be editable so that people can skip parts.” Likewise, an easy to use “app design (is) important to encourage users to use (the) app” and ensure users can figure out how the app works. Without this knowledge, users are unable to use the app. Additional frequent themes included community/social support (50%, n=5), knowledge of own consumption (50%, n=5), having access to education, recipes, and support links (50%, n=5), and information related to patient factors that impact lifestyle (40%, n=4) (Table 2). DIs believed it was important for patients to have knowledge about their own health status and food consumption because it helps patients “to know if (they) are improving or not” and to be more aware of their current health status. If patients “know what (they’re) consuming” and “how much (they) have eaten,” they can determine how they should move forward and if there are any changes that they should make depending on the feedback given through the app. DIs believed that app personalization should be “based on patient age and socioeconomic status” and that different variables in patients’ lives would call for different features. For example, “differences in the diet schedule of patients will require different timing of reminders and notifications”.
Table 2. Themes identified for the proposed diet app features.
| Themes | Related content | % [N=10] |
|---|---|---|
| Specific disease | “Very important to address specific diseases” | 70% [7] |
| “Useful if patient does not like to go to the doctor” | ||
| “Understand own condition and learn how to improve” | ||
| User involvement/investment/compliance/motivation/encourage participation | “More motivated to use app specific to own needs and disease” | 100% [10] |
| “Progress updates help users feel more motivated to continue when they see how far they’ve come” | ||
| Unique needs | “Each patient has own proper needs” | 70% [7] |
| “Cannot generalize” | ||
| “Makes user feel more invested” | ||
| “More likely to use app if tailored to needs” | ||
| App appearance | “Personalized appearance is more enjoyable” | 30% [3] |
| “Personalized content appearance” | ||
| “Should be able to pick screen used the most but | ||
| should not be editable so that people can skip parts” | ||
| Patient factors/lifestyle | “Based on patient age and socioeconomic status” | 40% [4] |
| “Understandable information for all” | ||
| “Not everyone will chat, some more private” | ||
| “Scheduling of reminders/notifications” | ||
| Disease information/disease and weight management/improvement | “People should have information on how to manage their disease” | 80% [80] |
| “Good to have resources to help manage and learn about disease” | ||
| “More educated regarding their disease” | ||
| “Allows for optimal patient outcomes” | ||
| “Must be understandable for all” | ||
| “Helpful to learn if you are managing disease well or ways to improve” | ||
| “Food log can help in weight and condition management” | ||
| Knowledge of own health status | “Important to know if you are improving or not” | 70% [7] |
| Reminder to complete a task or log | “This is very important because patient may forget his or her medication time” | 90% [9] |
| “Must! I think the biggest problem with tracking is remembering to do it” | ||
| “Letting them know its time to eat and not to forget to track foods” | ||
| Burdensome if notifications too often | “Reminders could be important but some people chose to ignore or turn them off” | 30% [3] |
| “So that the person remembers but not sure it is necessary to record every day could become annoying” | ||
| Communicate with doctor/RD/obtain relevant feedback/questions answered accurately, aid clinician decisions | “Tracking their progress will also be important to share with their doctor or RD” | 80% [8] |
| “If they can reach out to a dietician if they have questions, the app will be much more helpful to them, but probably not completely necessary” | ||
| “Talking to a medical professional when a question arises provides a sense of safety and security” | ||
| Community/social support | “They should be able to chat so they can build social support” | 50% [5] |
| “If this is just chatting with other users then it’s not something that is very much needed. They can do that separately” | ||
| Track progress, activity, food | “Seeing changes from time to time will allow patient to continue making changes” “People become more motivated when they see how far they’ve come” |
40% [4] |
| “Shows user how they might be improving, but also how they have gone backwards” | ||
| “Absolutely necessary to determine if they are following their diet/nutrition recommendations” | ||
| “Tracking what? your progress? activity? Foods? Should do all” | ||
| “Needed to show any progress” | ||
| Quick access to favorite foods | “Quick access to favorite foods when tracking (if eat same thing many days)” | 10% [1] |
| Know correct amount of insulin to take | “Diabetes can track carb to take correct insulin” | 10% [1] |
| Reference for doctors/providers patient data | “Enables RD to track progress of patient and provide relevant feedback; provides user data” | 60% [6] |
| “We need to learn from the patient, this can help with strategic change” | ||
| Nutritional food knowledge | “They can see what are good foods vs bad foods” | 20% [2] |
| Knowledge of own consumption | “Need to know what you’re consuming” | 50% [5] |
| “It’s important for these individuals to know what and how much they have eaten” | ||
| Tools, education, recipes, support links | “Tips for meal plans and recipe suggestions to help make food changings” | 50% [5] |
| “Gives tools to ensure optimal outcomes. IE, recipes, education, support links” |
Translating user preferences into functional requirements
The DIs organized specific features into 11 proposed categories as described earlier (Table 3). More than half of the DIs felt that ‘personalization’ category should include provisions to enter information related to medical factors (70%, n=7), personal information (70%, n=7), personal preferences (60%, n=6), and recording weight (60%, n=6). Forty percent of the DIs felt that ‘assessing disease severity’ should be included under personalization category. Only 10–20% of the DIs felt that calorie intake, number of meals, measurements/readings, audio, photos and calendar could be included in the personalization category. More than half of the DIs felt that ‘disease specific educational tips’ category should include information related to the foods one should eat (70%, n=7), low sodium options (70%, n=7), and recipes for diabetes (60%, n=6). Half of the DIs (n=5) felt that daily nutritional recommendations, information on fat and carb types, and information about the amount of insulin one should take with the meals should be included under ‘disease specific educational tips (Table 3). Only 10–20% of DI reported that ‘progress updates’ should include provisions for sharing information with friends, family, and providers (Table 3). Half of the DIs (n=5) thought that daily messages should be included under ‘reminders.’ Less than one-third of DIs believed that motivational messages and reinforcement, creating a photo library of foods, syncing the app with an individual’s calendar, collaborating with other members who have metabolic syndrome, weight, and physical activity should be a provision under ‘reminders’ (Table 3). More than half of the DIs felt that ‘positive reinforcement’ should include provisions to enter motivational messages (90%, n=9). More than half of the DI thought that ‘chat’ should include provisions for collaborating with other community members who have metabolic syndrome (60%, n=6). Thirty to forty percent of DIs believed that having the ability to communicate with a dietitian or clinician (40%, n=4) and sharing information with friends and family (30%, n=3) should be included under ‘chat.’ More than half of the DIs believed that ‘tracking’ should have features that include storing audio files (70%, n=7), viewing previous logs (70%, n=7), and uploading photos into a library (60%, n=6). Half of the DI believed that calorie intake, and recording physical activity should be included under ‘tracking’ (Table 3). Only 10–20% believed that information/characteristics about foods consumed, weight, how much insulin to take with meals, sync with individual calendar, and assess disease severity should be a provision under ‘tracking’ (Table 3). More than half of the DIs believed that ‘food log’ should include provisions such as food characteristics/information (90%, n=9), type and number of meals, specific nutrient intake, calculate carbohydrate count (80%, n=8), and enter food logs (70%, n=7) (Table 3). Half of the DIs felt that the ability to upload photos should be included under ‘food log.’ Forty percent of DIs believed that calorie intake, ability to create photo library, and store audio files should be included under ‘food log.’ (Table 3). More than half of the DIs thought that ‘communication’ should include features such as the ability to print/email to provider (80%, n=8), the ability to communicate with clinician or dietician (70%, n=7), and sharing information with friends and family (60%, n=6). Thirty percent thought messages and collaborating with other members who have metabolic syndrome should be included under the ‘communication’ category (Table 3). More than half of the DIs reported that ‘resource category’ should include easy to understand information through books, scientific literature, and external websites (90%, n=9). Half of the DIs believed recipes should be included under ‘resource category’ (Table 3).
Table 3. Translating user preferences into functional requirements.
| Categories | Perceived features in each category | % |
|---|---|---|
| Personalization | Medical Factors | 70% |
| Enter lab values | 70% | |
| Personal information | 70% | |
| Weight | 60% | |
| Assess disease severity | 40% | |
| Disease specific education | Foods to eat and not to eat | 70% |
| Recipes for diabetes (low carb) and hypertension (low salt) | 60% | |
| Information on fats and carbs | 50% | |
| Insulin to take with meals | 50% | |
| Progress updates | Messages | 50% |
| Reminders | Daily messages | 50% |
| Positive reinforcement | Motivational messages | 50% |
| Tracking | Calorie intake | 50% |
| Type of meal | 40% | |
| Physical activity levels | 50% | |
| Ability to upload photos | 60% | |
| Create photo library to remind themselves later of the foods they ate | 60% | |
| Able to store audio files | 70% | |
| Able to view previous logs | 70% | |
| Chat | Ability to communicate with dietician, clinician, and other community members who have metabolic syndrome | 40% |
| Maintain Food log | Types of meal | 80% |
| Number of meals | 80% | |
| Specify and calculate nutrient intake | 70% | |
| Calculate carbohydrate count | 80% | |
| Enter food name | ||
| Enter food group | ||
| Enter food type | 90% | |
| Enter portion size | 90% | |
| Preparation methods | 60% | |
| Able to view previous food logs | 60% | |
| Communication | Share information with friends and families | 60% |
| Collaborate with other community members who also have metabolic syndrome | 70% | |
| Ability to communicate with clinician and dietician | 70% | |
| Resource category | More information | 60% |
| Combined recipes for both diabetes and hypertension | 50% | |
| Access to other books, scientific literature, and external useful reliable websites | 90% |
Sketching
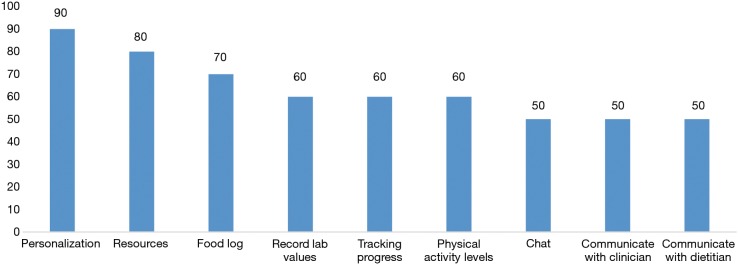
Most common data elements that the DIs wanted to include on the home screen of the proposed diet app included personalization (90%), manage their food log (70%), and have a resource category (80%) that will allow them to access reliable informational resources that can help gain more knowledge related to recipes that have low carbohydrate and low sodium content. Sixty percent of the DIs would want to be able to create their own profile. Sixty percent of the DIs wanted to have the ability to record their lab values and track their progress. Similarly sixty percent of the DIs wanted to record their physical activity levels. Fifty percent of them wanted to have chat and a tracking feature as a part of the proposed diet app. Fifty percent of the DIs wanted to have the ability to communicate with a clinician or registered dietitian (Figure 2). Results of the sketching show additional features that the DIs perceived to be useful in the proposed diet app. These included receiving motivational quotes for positive reinforcement (40%), ability to record height and weight measurements (40%), ability to upload photos of the meals taken (40%), medical history/conditions (30%), and information about healthy recipes specifically focusing on low carbohydrates and fat and low salt (30%) intake.
Figure 2.
Data elements identified in the sketching process.
Discussion
Having concluded their nutrition degrees, and beginning to engage with patients at a relatively early point in their careers, DIs are uniquely suited to consider the needs of patients as potential users of food and nutrition related apps. Having a degree of clinical nutrition knowledge, they also bring a fresh perspective to addressing patient management issues. Only fifty percent of these DIs had previously worked in a nutrition-related field, and less than half of them had worked previously in public health. They also brought that perspective to the assigned task. Only one-third of them were currently using a nutrition app (30%, n=3). Less than half of the DIs reported keeping a food log from time to time.
The top five components that the all DIs felt ranked very important in a diet app included: information related to medical factors, weight recording, food logs, food name and portion size. The top five features ranked by the DIs as very important features of the proposed diet app included (I) personalization of the app based on user preferences (80%, n=8); (II) disease specific education tips (90%, n=9); (III) ability to track progress (80%; n=8); (IV) reminders (70%, n=7) and (V) reinforcement based on user feedback (50%, n=5). The need for user involvement, reminder alerts to complete food logs, and communication and feedback from physicians were the top three rationales behind the rankings assigned to the various diet app features. In an attempt to translate the identified features into functional requirements, the majority of the DIs felt that each of the five key features identified should incorporate the following components: (I) personalization of the app should comprise information on medical factors, personal information, personal preferences, and recording weights; (II) disease specific educational tips should comprise information on food selections, low sodium options, and recipes for diabetes; (III) tracking progress should comprise features for storing audio files, viewing previous logs and uploading photos into a library; (IV) reminders should comprise daily messages to the users from the app; and (V) reinforcement should comprise provisions to enter motivational messages.
Findings of our study were consistent with prior studies that evaluated user characteristics and preferences for developing nutritional apps (18). In a study examining consumers’ needs in the development of a mobile app for nutritional management among pregnant women, the most common features and components preferred by the users included nutrition information for mother and child (36.2%), weight management (33.3%), food choice and cooking (21.9%), menu types (1.9%), and influence of health conditions such as smoking, drinking, exercising (1.0%). This is consistent with some the key diet app components identified by our DIs including information on carbohydrates and specific nutrient intake (70%), weight recording, food logs, and food names (100%).
An important contribution of the present study to the existing literature on diet app design is its focus on the use of a HCD approach which serves to bridge the gap between what users want in an app and what the designers are providing by involving the end user throughout the product development and testing process (8) especially in terms of safety and user experience. The present study implemented a HCD using a systematic sequence that included an identification of user characteristics, requirements analysis to identify user ideas, task analysis to rank the user-identified features of the diet app, qualitative methods to explain user preferences, and finally, translating the user preferences into functional requirements. Using this step-by-step approach in implementing a HCD, readers can appreciate how user profiles can be used to create personalized or tailored products that meet their needs. Such approaches are of critical significance because prior literature reviews have showed that the majority of diet apps lack theoretical components that are known to facilitate health behavior change (19,20). This is largely attributed to findings that such apps were designed based on the developers descriptions and insight of the apps, rather than a user-centered analysis. A study that explored the extent to which health behavior and design theories were incorporated into diet app development using 58 diet apps from iTunes health and fitness category, found that most apps were deficient and only provided general information (21). Scores ranged between 0 and 26 points on a 100-point scale (21). The implications are that these poorly-designed apps often have limited effectiveness. In particular, studies conducted to examine the effectiveness of existing diet apps highlight the need for tailoring approaches that can address the personal needs of the users (22).
Another crucial gap in the design approaches of existing diet apps is the challenge of identifying which specific components are associated with intervention effectiveness. Owing to the lack of a step-by-step human-centered approach in designing diet apps, as illustrated in the present study, the task of identifying specific components associated with effectiveness becomes an arduous one. The first systematic review to investigate the effectiveness of e-health and m-health interventions to promote physical activity and health diets in developing countries showed that it was not possible to identify the specific components associated with app effectiveness among the included studies. This systematic review was included 15 studies across 13 developing countries in Europe, Africa, Latin and South America (23). A HCD approach is needed to address these challenges.
Conclusions
Our study findings in conjunction with the existing literature lend support to the need for utilizing HCD approaches in developing e-health dietary apps as well other non-diet related apps. App developers are encouraged to incorporate user characteristics, needs and preferences using a HCD framework that will allow for reproducibility, tailoring, user satisfaction, and effectiveness assessments. Collaboration with nutrition and dietetics students, interns, and/or professionals can help to facilitate this needs identification process.
Acknowledgments
The authors and Dietetic Interns are acknowledged. The following dietetic interns participated in this project: Helen Cheng, Margot Cohen, Alyssa Costa, Paola Duarte, Leah Galitzdorfer, Jessica Lin, Julie Lin, Mahamoudou Sare, Kathleen Villarino, and Samantha Waters.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the CUNY Graduate School of Public Health and Health Policy’s Institutional Review Board (IRB Number: 2017-1095).
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Deloitte. Mobile Consumer Survey 2015 – The Australian Cut Life’s smarter than you think. 2015. Available online: https://landing.deloitte.com.au/rs/761-IBL-328/images/deloitte-au-tmt-mobile-consumer-survey-2015-291015.pdf
- 2.Smith A. U.S. Smartphone Use in 2015. Pew Internet, 2015. Available online: https://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/
- 3.Mayneris-Perxachs J, Sala-Vila A, Chisaguano M, et al. Effects of 1-year intervention with a Mediterranean diet on plasma fatty acid composition and metabolic syndrome in a population at high cardiovascular risk. PLoS One 2014;9:e85202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dietz WH, Baur LA, Hall K, et al. Management of obesity: improvement of health-care training and systems for prevention and care. Lancet 2015;385:2521-33. [DOI] [PubMed] [Google Scholar]
- 5.Wharton CM, Johnston CS, Cunningham BK, et al. Dietary self-monitoring, but not dietary quality, improves with use of smartphone app technology in an 8-week weight loss trial. J Nutr Educ Behav 2014;46:440-4. 10.1016/j.jneb.2014.04.291 [DOI] [PubMed] [Google Scholar]
- 6.Carter MC, Burley VJ, Nykjaer C, et al. Adherence to a smartphone application for weight loss compared to website and paper diary: pilot randomized controlled trial. J Med Internet Res 2013;15:e32. 10.2196/jmir.2283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schoeppe S, Alley S, Van Lippevelde W, et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act 2016;13:127. 10.1186/s12966-016-0454-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schoeppe S, Alley S, Rebar AL, et al. Apps to improve diet, physical activity and sedentary behaviour in children and adolescents: a review of quality, features and behaviour change techniques. Int J Behav Nutr Phys Act 2017;14:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jeon E, Park HA, Jo S, et al. Mobile Apps Providing Tailored Nursing Interventions for Patients with Metabolic Syndrome. Stud Health Technol Inform 2016;225:510-4. [PubMed] [Google Scholar]
- 10.Direito A, Carraça E, Rawstorn J, et al. mHealth Technologies to Influence Physical Activity and Sedentary Behaviors: Behavior Change Techniques, Systematic Review and Meta-Analysis of Randomized Controlled Trials. Ann Behav Med 2017;51:226-39. 10.1007/s12160-016-9846-0 [DOI] [PubMed] [Google Scholar]
- 11.Zhang C, Zhang X, Halstead-Nussloch R. Assessment, metrics, challenges and strategies for mobile health apps. Iss Inform Syst 2014;15:59. [Google Scholar]
- 12.Xie Z, Nacioglu A, Or C. Prevalence, Demographic Correlates, and Perceived Impacts of Mobile Health App Use Amongst Chinese Adults: Cross-Sectional Survey Study. JMIR Mhealth Uhealth 2018;6:e103. 10.2196/mhealth.9002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abras C, Maloney-Krichmar D, Preece J. User-centered design. In: Bainbridge W. editor. Encyclopedia of Human-Computer Interaction. Thousand Oaks: Sage Publications, 2004;37:445-56. [Google Scholar]
- 14.Harte R, Glynn L, Rodríguez-Molinero A, et al. A Human-Centered Design Methodology to Enhance the Usability, Human Factors, and User Experience of Connected Health Systems: A Three-Phase Methodology. JMIR Hum Factors 2017;4:e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Faiks A, Hyland N. Gaining user insight: a case study illustrating the card sort technique. Coll Res Libr 2000;61:349-57. 10.5860/crl.61.4.349 [DOI] [Google Scholar]
- 16.Tohidi M, Buxton W, Baecker R, et al. User sketches: a quick, inexpensive, and effective way to elicit more reflective user feedback. NordiCHI 2006, 14-18 October 2006:105-14.
- 17.Joshi A. The SanaViz: Human Centered Geovisualization to facilitate visual exploration of Public Health data. 2012. UT SBMI Dissertations (Open Access). 24. Available online: https://digitalcommons.library.tmc.edu/uthshis_dissertations/24
- 18.Kim SB, Kim JW, Kim MH, et al. A study on consumer's needs for development of diet guide application for pregnant women. Korean J Community Nutr 2013;18:588-98. 10.5720/kjcn.2013.18.6.588 [DOI] [Google Scholar]
- 19.Breton ER, Fuemmeler BF, Abroms LC. Weight loss-there is an app for that! But does it adhere to evidence-informed practices? Transl Behav Med 2011;1:523-9. 10.1007/s13142-011-0076-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.West JH, Hall PC, Hanson CL, et al. There’s an app for that: content analysis of paid health and fitness apps. J Med Internet Res 2012;14:e72. 10.2196/jmir.1977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.West JH, Hall PC, Arredondo V, et al. Health behavior theories in diet apps. J Consum Health Internet 2013;17:10-24. 10.1080/15398285.2013.756343 [DOI] [Google Scholar]
- 22.Wang Q, Egelandsdal B, Amdam GV, et al. Diet and Physical Activity Apps: Perceived Effectiveness by App Users. JMIR Mhealth Uhealth 2016;4:e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Müller AM, Alley S, Schoeppe S, et al. The effectiveness of e-& mHealth interventions to promote physical activity and healthy diets in developing countries: a systematic review. Int J Behav Nutr Phys Act 2016;13:109. 10.1186/s12966-016-0434-2 [DOI] [PMC free article] [PubMed] [Google Scholar]