Abstract
Background
Tiotropium bromide (TIO) is a long-acting muscarinic antagonist recommended as an add-on therapy option for patients with uncontrolled asthma on inhaled corticosteroids (ICS) and long-acting β2-agonists (LABA). However, real-world data on TIO use in asthma remains limited. To identify unmet needs, this study explored the use of TIO in US patients with asthma.
Methods
This retrospective cohort study used IQVIATM Health Plan Claims Data (October 1, 2014─December 31, 2016). Patients with asthma diagnoses initiating TIO 1.25 or 2.5 mcg after September 16, 2015 (first dispensing on index date) with ≥6 and ≥3 months continuous enrollment pre- and post-index, respectively, were identified. Patients with COPD diagnoses were excluded. Baseline characteristics, healthcare resource utilization and costs, and treatment patterns before and following TIO initiation were described for TIO cohorts and subgroups classified by concomitant medications received during the 30-day period after initiation.
Results
The study included 766 TIO 1.25 mcg and 1055 TIO 2.5 mcg users. In the TIO 1.25 mcg cohort, 16% (126/766) used TIO monotherapy while 61% (465/766) used TIO+ICS/LABA± leukotriene receptor antagonists (triple therapy). In TIO 1.25 mcg monotherapy and triple therapy subgroups, 39% and 49% were treated by allergists/pulmonologists, 27% and 48% experienced a moderate/severe asthma exacerbation, and 50% and 68% used rescue oral corticosteroids during the baseline period, respectively. Following triple therapy initiation, 44% of patients discontinued ICS within 6 months. The TIO 2.5 mcg cohort demonstrated similar trends.
Conclusion
This study provided insights into real-world US use of TIO in asthma. Overall, 16–19% of patients received TIO monotherapy and had high baseline exacerbation rates, suggesting that additional ICS-containing medication may be beneficial. Patients initiating triple therapy were among the most severe, with high baseline exacerbation rates and rescue medication use, and had high post-treatment ICS discontinuation rates, suggesting unmet needs in this population.
Keywords: LAMA, tiotropium, asthma, treatment patterns, triple therapy
Introduction
In the USA, the prevalence of asthma among adults is approximately 8.3%,1 of whom approximately 50% have uncontrolled disease.2,3 Patients with uncontrolled asthma have a decreased quality of life and increased healthcare resource utilization (HRU) and associated costs compared with patients with controlled asthma, due to the increased risk of morbidity and mortality.3,4 Asthma treatment aims to achieve control of symptoms and to reduce the future risk of exacerbations.5 The Global Initiative for Asthma (GINA) strategy report and US National Heart, Lung and Blood Institute (NHLBI) guidelines currently recommend inhaled corticosteroids (ICS) for long-term care of patients with persistent asthma, with the addition of a long-acting β2-agonist (LABA) in patients unable to control symptoms with ICS therapy alone.5,6 GINA and NHLBI also emphasize the importance of medication adherence in disease management and control for patients with asthma.5,6 However, in practice adherence tends to be poor,7–14 and can be adversely affected by a number of factors, including complexity of the medication regimens in terms of the number of agents, dosing frequency, and convenience of use.9,15–17
Tiotropium bromide (TIO) is a long-acting muscarinic antagonist (LAMA) approved for maintenance treatment of asthma by the US Food and Drug Administration (FDA).18 The GINA strategy report recommends TIO as one of several Step 4/5 add-on treatment options for patients with severe asthma who remain symptomatic during treatment with ICS/LABA or ICS monotherapy and have a history of exacerbation.5 NHLBI guidelines do not currently make any recommendations regarding the place of LAMAs in the treatment of patients with asthma.6
Improved understanding of real-world treatment of asthma is needed to improve its long-term management. However, real-world data on the treatment patterns and characteristics of patients with asthma who are treated with LAMAs in the USA are scarce. This study aimed to understand the real-world use of LAMA by examining patient characteristics and treatment patterns in patients with asthma before and after initiation of treatment with TIO 1.25 mcg and 2.5 mcg, either alone or in combination with other controller medications.
Materials And Methods
Study Design
This was a retrospective cohort study, which was conducted using enrollment, medical, and pharmacy claims data for the period of October 1, 2014 to December 31, 2016 in IQVIATM Health Plan Claims Data. This database contains fully adjudicated claims on more than 150 million health plan enrollees across the USA and contains information on around 40 million active patients in any given recent year. The population included in the database is generally representative of the commercially insured US population under 65 years of age with respect to the distribution of age and gender.
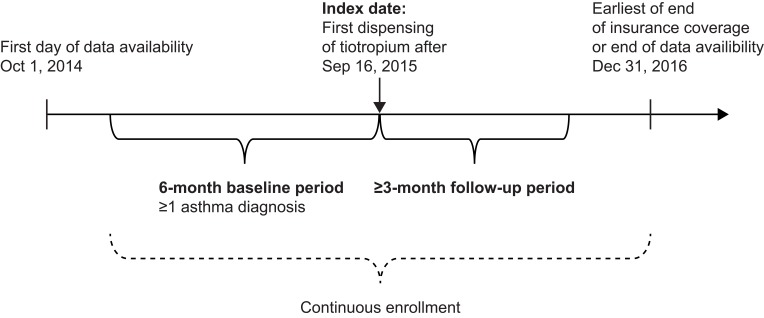
Patients initiating TIO 1.25 or 2.5 mcg with a soft mist inhaler after September 16, 2015 were identified, and the date of the first TIO dispensing was defined as the index date for each patient. Patient demographics and clinical characteristics were assessed during the 6-month baseline period prior to the index date. Treatment patterns for TIO 1.25 mcg and 2.5 mcg cohorts were evaluated during the baseline period and patients were observed from the index date to the earliest of end of insurance coverage or end of data availability (December 31, 2016; Figure 1).
Figure 1.
Study design.
Study Population
Patients with ≥1 dispensing for TIO 1.25 mcg or 2.5 mcg after September 16, 2015 were included in the study population if they had ≥6 months and ≥3 months of continuous enrollment during the baseline and follow-up period, respectively. Additional inclusion criteria were ≥18 years of age at the index date and a primary or secondary diagnosis of asthma (International Classification of Diseases [ICD] 9th Revision, Clinical Modification [9-CM] code: 493.xx; ICD 10th Revision, Clinical Modification [10-CM] code: J45.xxx) during the 6-month baseline period or on the index date.
Exclusion criteria were a diagnosis of chronic obstructive pulmonary disease (COPD; ICD-9-CM: 491.xx, 492.xx, 496.xx; ICD-10-CM: J41.xx, J43.xx, J44.xx) at any time during the baseline or follow-up period, a diagnosis of cystic fibrosis (ICD-9-CM: 277.0, ICD-10-CM: E84.0-E84.9) or acute respiratory failure (ICD-9-CM: 518.81, ICD-10-CM: J96.0) during the baseline period inclusive of the index date, or prior use of TIO 2.5 mcg during the baseline period.
Identification Of TIO Subgroups
TIO users were classified into different subgroups by medications taken concomitantly at the initiation of TIO. Concomitant medication was assessed during the 30-day period following the index date. Analyses were conducted for the overall TIO cohorts (1.25 mcg or 2.5 mcg) and by subgroups classified as TIO monotherapy or concomitant therapy with ICS, ICS+LABA (i.e. triple therapy users) with or without a leukotriene receptor antagonist (LTRA), and in combinations with other asthma medication classes (including biologics, LABAs, LTRAs, mast cell stabilizers, and methylxanthines).
Descriptive Characteristics And Study Measures
Baseline characteristics included demographic information evaluated at the index date as well as clinical characteristics, medication history, and HRU evaluated during the 6-month baseline period for the overall TIO 1.25 mcg and 2.5 mcg cohorts and their subgroups. More specifically, the following baseline characteristics were described: age, sex, geographic region, asthma-related medication use, prescribing provider specialty, exacerbation history (overall, moderate, and severe), list of Elixhauser and other specified asthma comorbidities, asthma-related HRU and costs. The Elixhauser comorbidity classification system, which is used to measure burden of disease, is comprised of 31 comorbidities based on ICD-9-CM or ICD-10-CM codes.19 Asthma-related HRU and costs were identified as episodes (i.e. inpatient, outpatient, or emergency room [ER] visits) with a primary or secondary diagnosis of asthma (ICD-9-CM: 493.xx or ICD-10-CM: J45.xxx). A moderate asthma exacerbation was defined as an asthma-related (primary ICD code) outpatient visit with an oral corticosteroid (OCS) dispensing within 7 days before or after the outpatient visit, whereas a severe asthma exacerbation was defined as an asthma-related (primary ICD code) inpatient or ER visit. Patients with both a moderate and severe exacerbation were classified as having a severe asthma exacerbation only.
Treatment pattern outcomes included the proportion of patients with asthma controller and rescue medication dispensings during the baseline and follow-up periods, and persistence with ICS as measured by time to discontinuation during the follow-up period. Controller medications included ICS, LABA, ICS/LABA, LAMA, LTRA, mast cell stabilizers, methylxanthines, immunoglobulin E (IgE) antagonists, interleukin (IL)-5 inhibitors, and maintenance OCS (consecutive days of OCS use for ≥6 months). LAMA and LABA monotherapy were included as controller medications to reflect real-world treatment patterns, although these medications are not recommended as monotherapy for patients with asthma and should be used in combination with (or as add-on therapy to) ICS for long-term maintenance treatment.5 Rescue medications included short-acting β2-agonists (SABA), short-acting muscarinic antagonists (SAMA), rescue OCS (≥1 dispensing, but <6 months of daily use), and antibiotics. Treatment discontinuation was defined as a gap of 45 days between the end of a dispensing and the next fill or between the end of a dispensing days’ supply and the end of the follow-up period, whichever occurred first.
TIO subgroups were defined by concomitant medications received in the 30-day period prior to TIO initiation, whereas baseline treatment patterns were assessed throughout the 6-month baseline period. Patients in the TIO monotherapy subgroup could therefore receive other controller medications during the 6-month baseline period if they received no concomitant controller medications in the 30-day period prior to TIO initiation.
To summarize the last treatments used prior to TIO initiation, a gap of 60 days was used to define treatment discontinuation.
Statistical Analyses
Baseline characteristics and the proportion of patients with ≥1 dispensing of asthma controller and rescue medications were analyzed descriptively. Characteristics were described using means, standard deviations (SDs), and medians for continuous variables. Frequencies and proportions were used to report categorical variables. No statistical tests were conducted between cohorts/subgroups. Kaplan–Meier curves were generated to describe persistence with ICS, based on time to ICS discontinuation.
Results
Study Population
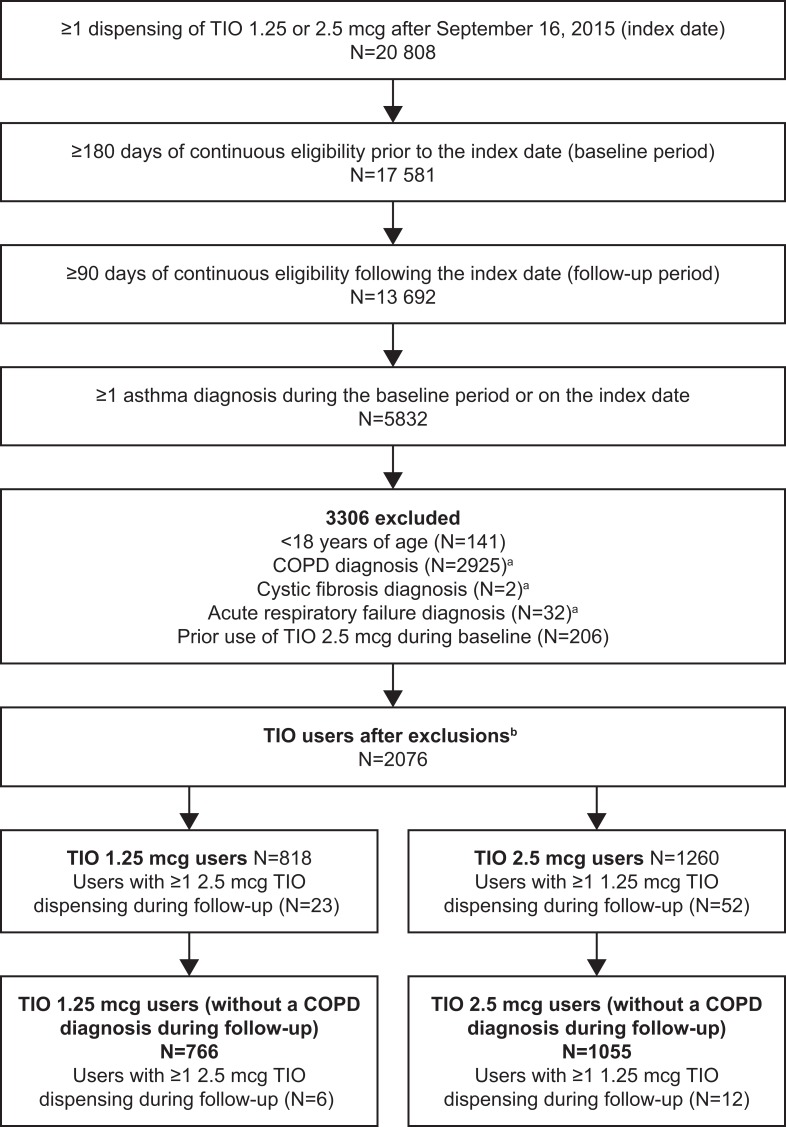
A total of 1821 patients met the study selection criteria, of whom 766 initiated TIO 1.25 mcg and 1055 initiated TIO 2.5 mcg (Figure 2). In the TIO 1.25 mcg cohort, the majority of patients used TIO as triple therapy (i.e with ICS/LABA [±LTRA]; 465, 61%), followed by TIO as monotherapy (126, 16%), TIO in combination with other medications (122, 16%), and TIO+ICS (53, 7%). Similarly, in the TIO 2.5 mcg cohort, the majority of patients used TIO as triple therapy (607, 58%), followed by monotherapy (197, 19%), in combination with other medications (173, 16%), and with ICS (78, 7%).
Figure 2.
Disposition of patients aCOPD was excluded at any time prior to index date and other respiratory-related diseases were excluded during baseline only. bA total of 2 patients had both 1.25 and 2.5 mcg TIO on the index date.
Abbreviations: COPD, chronic obstructive pulmonary disease; TIO, tiotropium bromide.
Baseline Demographics And Clinical Characteristics
Patient demographics and baseline characteristics are described in Table 1. Patients initiating TIO 1.25 and 2.5 mcg had a mean age of 47 and 50 years, respectively, and were primarily female (68% and 64%, respectively). The most common comorbidities in the TIO 1.25 and 2.5 mcg cohorts were allergic rhinitis, uncomplicated hypertension, gastroesophageal reflux disease, obesity, and obstructive sleep apnea. In both the TIO 1.25 and 2.5 mcg cohorts, patients were more commonly treated by allergists or pulmonologists than by primary care physicians or nurse practitioners (43–47% vs 27%). During the baseline period, 38–42% of patients across both cohorts experienced at least one exacerbation; 28–33% had a moderate exacerbation and 9–10% had a severe exacerbation.
Table 1.
Baseline Characteristicsa
| TIO 1.25 mcg | TIO 2.5 mcg | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Overall (N=766) | TIO Monotherapy (N=126) | TIO+ICS (N=53) | Triple Therapy ±LTRA (N=465) | TIO + Other Combinations (N=122) | Overall (N=1055) | TIO Monotherapy (N=197) | TIO+ICS (N=78) | Triple Therapy ±LTRA (N=607) | TIO + Other Combinations (N=173) | |
| Age, years, mean (SD) | 47.2 (13.2) | 45.9 (13.5) | 47.6 (13.6) | 47.8 (13.1) | 46.2 (12.8) | 49.7 (12.2) | 48.6 (12.0) | 51.1 (12.1) | 50.0 (12.4) | 49.4 (12.1) |
| Female, n (%) | 518 (67.6) | 81 (64.3) | 43 (81.1) | 310 (66.7) | 84 (68.9) | 675 (64.0) | 126 (64.0) | 52 (66.7) | 379 (62.4) | 118 (68.2) |
| Region, n (%) | ||||||||||
| Midwest | 189 (24.7) | 22 (17.5) | 12 (22.6) | 132 (28.4) | 23 (18.9) | 246 (23.3) | 44 (22.3) | 16 (20.5) | 152 (25.0) | 34 (19.7) |
| South | 336 (43.9) | 60 (47.6) | 20 (37.7) | 195 (41.9) | 61 (50.0) | 371 (35.2) | 72 (36.5) | 24 (30.8) | 207 (34.1) | 68 (39.3) |
| West | 61 (8.0) | 12 (9.5) | 4 (7.5) | 37 (8.0) | 8 (6.6) | 126 (11.9) | 26 (13.2) | 6 (7.7) | 71 (11.7) | 23 (13.3) |
| Northeast | 171 (22.3) | 32 (25.4) | 16 (30.2) | 93 (20.0) | 30 (24.6) | 292 (27.7) | 51 (25.9) | 29 (37.2) | 166 (27.3) | 46 (26.6) |
| Unknown | 9 (1.2) | 0 (0.0) | 1 (1.9) | 8 (1.7) | 0 (0.0) | 20 (1.9) | 4 (2.0) | 3 (3.8) | 11 (1.8) | 2 (1.2) |
| Most frequent comorbiditiesb, n (%) | ||||||||||
| Allergic rhinitis | 501 (65.4%) | 63 (50.0%) | 33 (62.3%) | 316 (68.0%) | 89 (73.0%) | 552 (52.3%) | 80 (40.6%) | 45 (57.7%) | 341 (56.2%) | 86 (49.7%) |
| Hypertension, uncomplicated | 227 (29.6%) | 42 (33.3%) | 17 (32.1%) | 137 (29.5%) | 31 (25.4%) | 321 (30.4%) | 60 (30.5%) | 24 (30.8%) | 173 (28.5%) | 64 (37.0%) |
| GERD | 191 (24.9%) | 30 (23.8%) | 16 (30.2%) | 112 (24.1%) | 33 (27.0%) | 262 (24.8%) | 43 (21.8%) | 20 (25.6%) | 149 (24.5%) | 50 (28.9%) |
| Obesity | 119 (15.5%) | 24 (19.0%) | 8 (15.1%) | 70 (15.1%) | 17 (13.9%) | 155 (14.7%) | 30 (15.2%) | 10 (12.8%) | 89 (14.7%) | 26 (15.0%) |
| Obstructive sleep apnea | 109 (14.2%) | 10 (7.9%) | 3 (5.7%) | 81 (17.4%) | 15 (12.3%) | 159 (15.1%) | 23 (11.7%) | 9 (11.5%) | 104 (17.1%) | 23 (13.3%) |
| Hypothyroidism | 102 (13.3%) | 11 (8.7%) | 10 (18.9%) | 62 (13.3%) | 19 (15.6%) | 150 (14.2%) | 38 (19.3%) | 16 (20.5%) | 73 (12.0%) | 23 (13.3%) |
| Depression | 101 (13.2%) | 11 (8.7%) | 9 (17.0%) | 63 (13.5%) | 18 (14.8%) | 156 (14.8%) | 29 (14.7%) | 15 (19.2%) | 89 (14.7%) | 23 (13.3%) |
| Diabetes, uncomplicated | 76 (9.9%) | 9 (7.1%) | 2 (3.8%) | 43 (9.2%) | 22 (18.0%) | 127 (12.0%) | 18 (9.1%) | 13 (16.7%) | 75 (12.4%) | 21 (12.1%) |
| Cardiac arrhythmias | 57 (7.4%) | 12 (9.5%) | 4 (7.5%) | 30 (6.5%) | 11 (9.0%) | 75 (7.1%) | 15 (7.6%) | 7 (9.0%) | 39 (6.4%) | 14 (8.1%) |
| Rheumatoid arthritis/collagen vascular disease | 45 (5.9%) | 10 (7.9%) | 3 (5.7%) | 24 (5.2%) | 8 (6.6%) | 58 (5.5%) | 12 (6.1%) | 6 (7.7%) | 33 (5.4%) | 7 (4.0%) |
| Physician specialty, n (%) | ||||||||||
| Allergist/pulmonologist | 361 (47.1) | 49 (38.9) | 29 (54.7) | 229 (49.2) | 54 (44.3) | 448 (42.5) | 59 (29.9) | 38 (48.7) | 297 (48.9) | 54 (31.2) |
| PCP/nurse practitioner | 206 (26.9) | 42 (33.3) | 13 (24.5) | 108 (23.2) | 43 (35.2) | 284 (26.9) | 69 (35.0) | 21 (26.9) | 123 (20.3) | 71 (41.0) |
| Patients with ≥1 asthma exacerbationc, n (%) | 323 (42.2) | 34 (27.0) | 19 (35.8) | 225 (48.4) | 45 (36.9) | 401 (38.0) | 40 (20.3) | 28 (35.9) | 268 (44.2) | 65 (37.6) |
| Moderate (Asthma OP visit + OCS) | 256 (33.4) | 26 (20.6) | 12 (22.6) | 181 (38.9) | 37 (30.3) | 294 (27.9) | 26 (13.2) | 22 (28.2) | 199 (32.8) | 47 (27.2) |
| Severe (Asthma IP or ER visit) | 67 (8.7) | 8 (6.3) | 7 (13.2) | 44 (9.5) | 8 (6.6) | 107 (10.1) | 14 (7.1) | 6 (7.7) | 69 (11.4) | 18 (10.4) |
| Asthma-related HRU | ||||||||||
| Patients with ≥1 IP visits, n (%) | 33 (4.3) | 5 (4.0) | 4 (7.5) | 20 (4.3) | 4 (3.3) | 53 (5.0) | 10 (5.1) | 5 (6.4) | 31 (5.1) | 7 (4.0) |
| IP visits per patient, mean (SD) | 1.0 (0.2) | 1.0 (0.0) | 1.3 (0.5) | 1.0 (0.0) | 1.0 (0.0) | 1.1 (0.7) | 1.0 (0.0) | 1.4 (0.9) | 1.2 (0.9) | 1.0 (0.0) |
| ER visits, mean (SD) | 1.5 (0.9) | 1.2 (0.4) | 1.3 (0.5) | 1.6 (1.1) | 1.2 (0.4) | 1.7 (1.6) | 1.6 (1.2) | 1.1 (0.4) | 1.7 (1.4) | 1.8 (2.4) |
| OP visits, mean (SD) | 3.5 (3.2) | 2.6 (2.0) | 3.0 (2.2) | 3.7 (3.2) | 3.9 (3.9) | 3.4 (3.3) | 2.5 (2.7) | 3.2 (4.3) | 3.6 (3.2) | 3.6 (3.3) |
| Asthma-related healthcare costs, US$, mean (SD) | ||||||||||
| Total healthcare cost | 3060 (6702) | 1466 (3199) | 3607 (7204) | 3421 (7323) | 3090 (6,495) | 3159 (9316) | 1658 (4504) | 2764 (6790) | 3292 (5536) | 4579 (19,375) |
| IP visit costs | 599 (4983) | 290 (1753) | 1413 (5949) | 675 (5887) | 272 (2277) | 705 (3967) | 562 (3252) | 1,127 (5798) | 737 (3909) | 564 (3922) |
| ER visit costs | 160 (961) | 96 (475) | 429 (1542) | 171 (1077) | 71 (304) | 192 (868) | 128 (493) | 59 (239) | 211 (872) | 260 (1270) |
| OP visit costs | 1224 (3316) | 769 (2063) | 1029 (3199) | 1351 (3314) | 1293 (4279) | 1253 (8127) | 642 (2995) | 942 (3082) | 1083 (3285) | 2686 (18,698) |
| Pharmacy costs | 1076 (2054) | 311 (551) | 736 (812) | 1223 (1418) | 1454 (4,181) | 1008 (1504) | 326 (802) | 635 (680) | 1261 (1251) | 1068 (2564) |
Notes: aSubgroups were defined by concomitant medications received in the 30-day period after the index date. For example, patients were classified into the TIO monotherapy subgroup if they initiated TIO without other concomitant asthma medication use within 30 days after the index date. bComorbidities were evaluated during the 6-month baseline period. cModerate exacerbations were defined as an OCS dispensing within 7 days of an asthma-related outpatient visit, and severe exacerbations were defined as an asthma-related inpatient or ER visit.
Abbreviations: ER, emergency room; GERD, gastroesophageal reflux disease; HRU, healthcare resource utilization; ICS, inhaled corticosteroid; IP, inpatient; LTRA, leukotriene receptor antagonist; OP, outpatient; OCS, oral corticosteroid; PCP, primary care physician; SD, standard deviation; TIO, tiotropium bromide.
Between the main TIO 1.25 and 2.5 mcg cohorts, overall HRU and costs were similar. In the TIO 1.25 mcg cohort, 4% of patients had at least one asthma-related inpatient visit in the 6-month baseline period, and among these patients the mean (SD) number of asthma-related inpatient visits was 1.0 (0.2). Mean (SD) total asthma-related medical and pharmacy costs were $3060 (6702). In the TIO 2.5 mcg cohort, 5% of patients had a prior asthma-related inpatient visit with on average 1.1 (0.7) asthma-related inpatient visits and mean total asthma-related costs of $3159 (9316).
Relative to the other TIO 1.25 mcg subgroups, patients in the TIO 1.25 mcg monotherapy subgroup were among the youngest (mean age: 46 vs 46–48 years) and had a lower rate of comorbid allergic rhinitis (50% vs 62–73%). A smaller proportion of patients using TIO monotherapy experienced at least one asthma exacerbation in the 6-month baseline period (total: 27%; moderate: 21%, severe: 6%) compared with the other subgroups (total: 36–48%; moderate: 23–39%, severe: 7–13%).
Patients in the TIO 1.25 mcg +ICS subgroup had a mean age of 48 years, 81% were female, and 36% had an asthma exacerbation in the 6-month baseline period (moderate: 23%, severe: 13%). Patients in the TIO+ICS subgroup had an average of 1.3 asthma-related ER visits in the 6-month baseline period and 8% had >1 asthma-related inpatient visit.
Patients using triple therapy were slightly older than the other TIO 1.25 mcg subgroups (mean age: 48 years). The triple therapy subgroup had the highest baseline exacerbation rates, with 48% of patients experiencing at least one asthma exacerbation in the 6-month baseline period (moderate: 39%, severe: 10%). Patients receiving triple therapy also had a higher mean number of asthma-related ER visits compared with other TIO subgroups (1.6 vs 1.2–1.3) and among the highest mean number of asthma-related outpatient visits (3.7 vs 2.6–3.9).
In the TIO 1.25 mcg cohort, patients were more frequently treated by allergists or pulmonologists than by primary care providers or nurse practitioners in the monotherapy (39% vs 33%), TIO+ICS (55% vs 25%), and triple therapy (49% vs 23%) subgroups. Similar trends were observed in the TIO 2.5 mcg cohort (Table 1).
Baseline Treatment Patterns
Baseline treatment patterns of patients in the main TIO cohorts and concomitant medication subgroups who used each class of controller and rescue medication in the baseline period are displayed in Table 2.
Table 2.
Baseline Treatment Patternsa
| TIO 1.25 mcg | TIO 2.5 mcg | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Overall (N=766) | TIO Monotherapy (N=126) | TIO+ICS (N=53) | Triple Therapy ±LTRA (N=465) | TIO + Other Combinations (N=122) | Overall (N=1055) | TIO Monotherapy (N=197) | TIO+ICS (N=78) | Triple Therapy ±LTRA (N=607) | TIO + Other Combinations (N=173) | |
| Controller medications, n (%) | 641 (83.7) | 55 (43.7) | 33 (62.3) | 439 (94.4) | 114 (93.4) | 825 (78.2) | 69 (35.0) | 43 (55.1) | 556 (91.6) | 157 (90.8) |
| ICS | 580 (75.7) | 47 (37.3) | 42 (79.2) | 429 (92.3) | 62 (50.8) | 726 (68.8) | 65 (33.0) | 60 (76.9) | 529 (87.1) | 72 (41.6) |
| ICS/LABA | 520 (67.9) | 39 (31.0) | 11 (20.8) | 418 (89.9) | 52 (42.6) | 645 (61.1) | 49 (24.9) | 16 (20.5) | 514 (84.7) | 66 (38.2) |
| LTRA | 441 (57.6) | 25 (19.8) | 25 (47.2) | 283 (60.9) | 108 (88.5) | 573 (54.3) | 25 (12.7) | 34 (43.6) | 368 (60.6) | 146 (84.4) |
| LAMA | 52 (6.8) | 6 (4.8) | 9 (17.0) | 27 (5.8) | 10 (8.2) | 108 (10.2) | 12 (6.1) | 7 (9.0) | 68 (11.2) | 21 (12.1) |
| Methylxanthines | 12 (1.6) | 0 (0.0) | 0 (0.0) | 2 (0.4) | 10 (8.2) | 21 (2.0) | 2 (1.0) | 0 (0.0) | 1 (0.2) | 18 (10.4) |
| LABA | 8 (1.0) | 0 (0.0) | 1 (1.9) | 6 (1.3) | 1 (0.8) | 14 (1.3) | 1 (0.5) | 1 (1.3) | 8 (1.3) | 4 (2.3) |
| IgE antagonists | 5 (0.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 5 (4.1) | 5 (0.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 5 (2.9) |
| Mast cell stabilizers | 3 (0.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (2.5) | 1 (0.1) | 0 (0.0) | 0 (0.0) | 1 (0.2) | 0 (0.0) |
| IL-5 inhibitors | 2 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (1.6) | 3 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (1.7) |
| Maintenance OCSb | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.1) | 0 (0.0) | 0 (0.0) | 1 (0.2) | 0 (0.0) |
| Rescue medications, n (%) | 663 (86.6) | 106 (84.1) | 43 (81.1) | 411 (88.4) | 103 (84.4) | 915 (86.7) | 158 (80.2) | 67 (85.9) | 541 (89.1) | 149 (86.1) |
| SABA | 503 (65.7) | 70 (55.6) | 29 (54.7) | 324 (69.7) | 80 (65.6) | 702 (66.5) | 122 (61.9) | 50 (64.1) | 423 (69.7) | 107 (61.8) |
| Antibiotics | 497 (64.9) | 80 (63.5) | 34 (64.2) | 308 (66.2) | 75 (61.5) | 659 (62.5) | 115 (58.4) | 44 (56.4) | 394 (64.9) | 106 (61.3) |
| Rescue OCSc | 482 (62.9) | 63 (50.0) | 30 (56.6) | 318 (68.4) | 71 (58.2) | 591 (56.0) | 83 (42.1) | 39 (50.0) | 375 (61.8) | 94 (54.3) |
| SAMA | 20 (2.6) | 1 (0.8) | 2 (3.8) | 15 (3.2) | 2 (1.6) | 34 (3.2) | 7 (3.6) | 4 (5.1) | 19 (3.1) | 4 (2.3) |
Notes: aTreatment patterns were assessed during the 6-month baseline period prior to the index date. Subgroups were defined by concomitant medications received in the 30-day period after the index date. For example, patients were classified into the TIO monotherapy subgroup if they initiated TIO without other concomitant asthma medication use within 30 days after the index date. TIO monotherapy patients could have received other controller medications during the 6-month baseline period but could not have received any concomitant medication which extended into the 30-day period following the index date. bMaintenance OCS defined as ≥6 months continuous use. cRescue OCS defined as ≥1 dispensing with <6 months use.
Abbreviations: ICS, inhaled corticosteroid; IgE, immunoglobulin E; IL-5, interleukin-5; LABA, long-acting β2-antagonist; LAMA, long-acting muscarinic antagonist; LTRA, leukotriene receptor antagonist; OCS, oral corticosteroid; SABA, short-acting β2-antagonist; SAMA, short-acting muscarinic antagonist; TIO, tiotropium bromide.
In the overall TIO 1.25 mcg cohort, 76% of patients used ≥1 ICS-containing medication in the baseline period. Other controller medication classes used frequently during the baseline period included ICS/LABA (68%) and LTRA (58%). In the TIO 1.25 mcg monotherapy subgroup, 64% of patients received at least one course of antibiotics, 56% received ≥1 SABA-containing medication, and 50% received ≥1 dispensing of OCS during the baseline period. The highest rate of rescue medication use was observed in the TIO 1.25 mcg triple therapy subgroup, in which 70% of patients received ≥1 SABA-containing medication, 68% received ≥1 OCS, and 66% received antibiotics.
The most frequent combinations of asthma controller therapy classes used immediately before TIO 1.25 mcg initiation were ICS/LABA, ICS/LABA+LTRA, LTRA, no treatment, and ICS (Supplementary Table S1).
Similarly, in the overall TIO 2.5 mcg cohort, 69% of patients used ≥1 ICS-containing medication in the baseline period. Other frequently used baseline controller medications included ICS/LABA (61%) and LTRA (54%). In the TIO 2.5 mcg monotherapy subgroup, 62% received ≥1 SABA-containing medication, 58% received antibiotics, and 42% received ≥1 dispensing of OCS. The highest rates of baseline rescue medication use were observed among TIO 2.5 mcg triple therapy users, of which 70% received ≥1 SABA-containing medication, 65% received ≥1 antibiotic medication, and 62% received ≥1 OCS during the baseline period.
The most frequent combinations of asthma controller therapy classes used immediately prior to TIO 2.5 mcg initiation were ICS/LABA, no treatment, LTRA, ICS/LABA+LTRA, and ICS (Supplementary Table S1).
Follow-Up Treatment Patterns
The mean duration of the follow-up period was 187–209 days for the TIO 1.25 mcg cohort and 260─294 days for the TIO 2.5 mcg cohort. In both TIO cohorts, the mean duration of treatment with TIO was shorter in the monotherapy subgroup than in the triple therapy subgroup (TIO 1.25: 120 vs 137 days; TIO 2.5: 123 vs 156 days). Frequently used controller medications in the follow-up period included ICS, ICS/LABA, and LTRA (Table 3).
Table 3.
Follow-Up Treatment Patternsa
| TIO 1.25 mcg | TIO 2.5 mcg | |||||||
|---|---|---|---|---|---|---|---|---|
| TIO Monotherapy (N=126) | TIO+ICS (N=53) | Triple Therapy ±LTRA (N=465) | TIO + Other Combinations (N=122) | TIO Monotherapy (N=197) | TIO+ICS (N=78) | Triple Therapy ±LTRA (N=607) | TIO + Other Combinations (N=173) | |
| Observation (follow-up) period, days, mean (SD) | 209.3 (68.8) | 198.3 (73.5) | 201.8 (71.7) | 187.4 (62.9) | 274.4 (114.6) | 293.8 (110.4) | 271.9 (108.5) | 260.3 (99.9) |
| TIO treatment duration, days, mean (SD) | 119.8 (91.3) | 128.4 (82.9) | 136.7 (88.8) | 107.3 (78.5) | 123.0 (121.7) | 147.4 (123.9) | 155.9 (122.8) | 142.7 (109.8) |
| Controller medications, n (%) | 63 (50.0) | 36 (67.9) | 465 (100.0) | 122 (100.0) | 68 (34.5) | 48 (61.5) | 607 (100.0) | 172 (99.4) |
| ICS | 55 (43.7) | 53 (100.0) | 465 (100.0) | 67 (54.9) | 71 (36.0) | 78 (100.0) | 607 (100.0) | 92 (53.2) |
| ICS/LABA | 45 (35.7) | 11 (20.8) | 465 (100.0) | 60 (49.2) | 51 (25.9) | 18 (23.1) | 607 (100.0) | 86 (49.7) |
| LTRA | 31 (24.6) | 27 (50.9) | 310 (66.7) | 120 (98.4) | 25 (12.7) | 40 (51.3) | 391 (64.4) | 164 (94.8) |
| LABA | 1 (0.8) | 0 (0.0) | 7 (1.5) | 3 (2.5) | 0 (0.0) | 2 (2.6) | 11 (1.8) | 4 (2.3) |
| LAMA | 1 (0.8) | 5 (9.4) | 22 (4.7) | 8 (6.6) | 6 (3.0) | 5 (6.4) | 45 (7.4) | 16 (9.2) |
| Mast cell stabilizers | 0 (0.0) | 0 (0.0) | 1 (0.2) | 2 (1.6) | 1 (0.5) | 0 (0.0) | 0 (0.0) | 1 (0.6) |
| Methylxanthines | 0 (0.0) | 0 (0.0) | 1 (0.2) | 11 (9.0) | 1 (0.5) | 1 (1.3) | 5 (0.8) | 23 (13.3) |
| IgE antagonists | 0 (0.0) | 0 (0.0) | 4 (0.9) | 7 (5.7) | 0 (0.0) | 1 (1.3) | 4 (0.7) | 6 (3.5) |
| IL-5 inhibitors | 0 (0.0) | 0 (0.0) | 4 (0.9) | 3 (2.5) | 0 (0.0) | 0 (0.0) | 3 (0.5) | 4 (2.3) |
| Maintenance OCSb | 0 (0.0) | 0 (0.0) | 2 (0.4) | 1 (0.8) | 0 (0.0) | 0 (0.0) | 6 (1.0) | 1 (0.6) |
| Rescue medications, n (%) | 105 (83.3) | 44 (83.0) | 429 (92.3) | 94 (77.0) | 156 (79.2) | 67 (85.9) | 537 (88.5) | 151 (87.3) |
| Antibiotics | 75 (59.5) | 38 (71.7) | 317 (68.2) | 75 (61.5) | 121 (61.4) | 50 (64.1) | 402 (66.2) | 103 (59.5) |
| Rescue OCSc | 55 (43.7) | 29 (54.7) | 252 (54.2) | 57 (46.7) | 95 (48.2) | 39 (50.0) | 356 (58.6) | 99 (57.2) |
| SABA | 78 (61.9) | 39 (73.6) | 354 (76.1) | 75 (61.5) | 118 (59.9) | 52 (66.7) | 434 (71.5) | 113 (65.3) |
| SAMA | 3 (2.4) | 2 (3.8) | 10 (2.2) | 2 (1.6) | 8 (4.1) | 1 (1.3) | 16 (2.6) | 5 (2.9) |
Notes: aTreatment patterns were assessed during the entire follow-up period from the index date until the end of insurance coverage or end of data availability, whichever occurred first. Subgroups were defined by concomitant medications received in the 30-day period after the index date. For example, patients were classified into the TIO monotherapy subgroup if they initiated TIO without other concomitant asthma medication use within 30 days after the index date. bMaintenance OCS defined as ≥6 months continuous use. cRescue OCS defined as ≥1 dispensing with <6 months use.
Abbreviations: ICS, inhaled corticosteroid; IgE, immunoglobulin E; IL-5, interleukin-5; LABA, long-acting β2-antagonist; LAMA, long-acting muscarinic antagonist; LTRA, leukotriene receptor antagonist; OCS, oral corticosteroid; SABA, short-acting β2-antagonist; SAMA, short-acting muscarinic antagonist; SD, standard deviation; TIO, tiotropium bromide.
The proportion of patients with at least one rescue medication dispensing during the follow-up period after TIO initiation remained high across the TIO subgroups, and was among the highest in patients receiving triple therapy. In the TIO 1.25 mcg and 2.5 mcg cohorts, 62–76% and 60–72% of patients had ≥1 SABA dispensing in the follow-up period, respectively. Across all subgroups in the TIO 1.25 and 2.5 mcg cohorts, 44─55% and 48–59% had at least one course of OCS, and 60–72% and 60–66% received ≥1 antibiotic dispensing, respectively. Within each TIO cohort, OCS and SABA use was highest among triple therapy users compared with other subgroups.
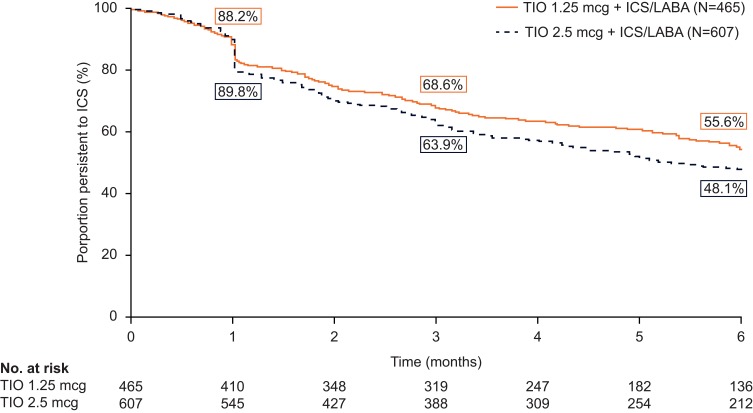
Persistence With ICS
Among patients in the triple therapy subgroups, Kaplan–Meier curves show that 44% and 52% of patients who initiated triple therapy discontinued ICS after 6 months in the TIO 1.25 and 2.5 mcg cohorts, respectively (Figure 3).
Figure 3.
Kaplan–Meier rates of persistence with ICS therapy in TIO 1.25 and TIO 2.5 mcg triple therapy subgroups.a
Notes: aPersistence is defined as no gap in ICS therapy >45 days between the end of a dispensing and the next fill or between the end of a dispensing’s days of supply and the end of the follow-up period, whichever occurred first.
Abbreviations: ICS, inhaled corticosteroid; LABA, long-acting β2-antagonist; TIO, tiotropium bromide.
Discussion
This study assessed patient characteristics and treatment patterns among asthma patients initiating TIO therapy, who were identified from a large US claims database, to understand the real-world use of TIO in patients with asthma. The proportion of patients receiving TIO 1.25 and 2.5 mcg monotherapy treated by allergists or pulmonologists was lower than in other subgroups, but was still over 30%; conversely, 33–35% were treated by primary care providers or nurse practitioners, which was a larger proportion than in the triple therapy and TIO+ICS subgroups. In the 6-month period prior to TIO initiation, over 20% experienced at least one moderate or severe exacerbation, and over 40% received rescue OCS treatment. In contrast, in the TIO 1.25 and 2.5 mcg triple therapy subgroups, approximately 50% of patients were treated by allergists or pulmonologists, and a similar proportion experienced a moderate or severe exacerbation in the 6-month baseline period. Within the TIO 1.25 or 2.5 mcg cohorts, baseline and follow-up rescue OCS medication use was the highest among triple therapy users. Approximately half of all patients in either TIO 1.25 or 2.5 mcg cohort receiving triple therapy discontinued ICS within 6 months of treatment initiation. Overall, these findings suggest a large proportion of the patients who received TIO either as monotherapy or triple therapy in this study had uncontrolled asthma symptoms.
The evaluation of treatment patterns before and after the initiation of TIO therapy in the present study showed 16–19% of patients using TIO 1.25 and 2.5 mcg as monotherapy. In the baseline period, the exacerbation rate in the TIO monotherapy group was lower than in the overall cohort and the TIO concomitant therapy subgroups. Nonetheless, the exacerbation rate in the TIO monotherapy subgroups was still over 20%, and the majority of patients receiving TIO monotherapy required OCS and other rescue medication use. TIO is approved in the US for long-term maintenance treatment of asthma18 and clinical trials have evaluated the efficacy of TIO as add-on therapy to ICS/LABA.20–22 However, there are currently limited clinical data regarding the use of TIO monotherapy in the treatment of asthma, and TIO is not recommended as monotherapy by the GINA strategy report or NHLBI guidelines.5,6 The potential population of US patients with asthma for whom treatment with TIO may be indicated is therefore broader than that defined by the GINA recommendation. Consistent with current GINA recommendations,5 the findings of the present study suggest that TIO monotherapy is not likely to be an effective treatment option for patients with asthma, and that patients receiving TIO monotherapy may additionally benefit from the anti-inflammatory effects of ICS-containing medication to achieve better asthma control.
GINA recommends TIO as add-on maintenance therapy for patients with severe asthma who remain symptomatic on a combination of ICS and LABA, with a history of exacerbations,5 while NHLBI guidelines do not specify the place of LAMAs in triple therapy.6 Among patients receiving triple therapy in the present study, there was a high rate of exacerbations and a high proportion of patients using OCS and other rescue medications in the 6-month baseline period. The triple therapy subgroup also had a low rate of persistence with ICS in the 6-month period following initiation of TIO therapy. Additionally, a large proportion of these patients were treated by allergists or pulmonologists. Taken together, these findings suggest that patients receiving triple therapy may have more severe asthma and a significant level of uncontrolled disease with a high risk of exacerbations, which may be associated with a large disease burden and represent a considerable unmet need in asthma therapy. Due to the considerable heterogeneity in asthma phenotypes, the GINA guidelines recommend that patients with asthma may benefit from treatment according to phenotype categories, such as severe allergic asthma or eosinophilic asthma.5 Better understanding of the effects of TIO, or LAMAs in general, as add-on therapy in patients with different asthma phenotypes may help improve prediction of response to therapy and improve the considerable disease burden among patients with more severe asthma.
Overall, similar trends were observed between the TIO 1.25 mcg and TIO 2.5 mcg cohorts, with the exception of a slightly shorter mean follow-up period observed for the TIO 1.25 mcg cohort than for the TIO 2.5 mcg cohort. This difference may reflect a relatively slower rate of uptake for TIO 1.25 mcg, which received FDA approval for asthma in September 2015, at the beginning of the patient identification period, compared with TIO 2.5 mcg, which was already an established product in the US market.
Several limitations should be considered in the interpretation of the findings of this study. TIO can be prescribed as maintenance treatment for patients with COPD; although patients with a COPD diagnosis were excluded, it was not possible to confirm that TIO was prescribed specifically for the treatment of asthma. The data used for this study were obtained in the year immediately after approval of TIO as a long-term maintenance treatment for asthma and represents the experience of early adopters of TIO. Treatment patterns identified in this study may therefore change over time.
This study was also affected by a set of limitations common to all observational studies based on retrospective claims data. It is not possible to confirm that medications described in pharmacy claims data have been received or taken as prescribed by the patient. Claims data also do not capture the use of over-the-counter medications, drug samples, and medications received during inpatient stays. The analysis may also be vulnerable to coding inaccuracies, such as inaccurate diagnosis codes or misclassification of codes included as a rule-out criterion as opposed to actual disease. Interpretation may also be limited by missing information, though pharmacy claims (on which the present study was based) are generally complete. Nevertheless, this retrospective cohort study using a large US claims database has enabled evaluation of the characteristics and treatment patterns among asthma patients initiating TIO therapy. The findings of this study in a geographically diverse US-based cohort of asthma patients in a real-world setting will improve our understanding of current LAMA use in asthma in the USA.
Conclusion
In conclusion, the findings of this study provide insights into current use of LAMAs in asthma in the real-world setting in the USA. The analysis showed that over 15% of patients received TIO as monotherapy, of whom more than 20% had an exacerbation during the baseline period prior to TIO initiation. These patients may therefore benefit from additional ICS-containing medication. The triple therapy group had high post-treatment ICS discontinuation rates and was among the most severe, with frequent baseline exacerbations and high rescue medication use, suggesting an unmet need in this population. Together, these findings suggest a significant level of uncontrolled asthma and a large associated disease burden among those initiating LAMA and particularly triple therapy. This study highlights unmet needs in current asthma care among such patients with asthma identified from a large real-world US claims database.
Acknowledgments
Medical writing support was provided by Mark Condon, DPhil, of Fishawack Indicia Ltd, and funded by GSK.
Abbreviations
COPD, chronic obstructive pulmonary disease; ER, emergency room; FDA, Food and Drug Administration; GERD, gastroesophageal reflux disease; GINA, Global Initiative for Asthma; HRU, healthcare resource utilization; ICD-9-CM, International Classification of Diseases 9th Revision, Clinical Modification; ICD-10-CM, International Classification of Diseases 10th Revision, Clinical Modification; ICS, inhaled corticosteroid; IgE, immunoglobulin E; IL-5, interleukin-5; IP, inpatient; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; LTRA, leukotriene receptor antagonist; NHLBI, National Heart, Lung and Blood Institute; NOTX, no treatment; OCS, oral corticosteroid; OP, outpatient; PCP, primary care physician; SABA, short-acting β2-agonist; SAMA, short-acting muscarinic antagonist; SD, standard deviation; TIO, tiotropium bromide.
Congress Citation
An abstract of this paper was presented at the 2018 American Thoracic Society (ATS) 114th International Conference as a poster presentation with interim findings. The abstract was published in the American Journal of Respiratory and Critical Care Medicine 2018; 197:A4852; https://www.atsjournals.org/doi/pdf/10.1164/ajrccm-conference.2018.197.1_MeetingAbstracts.A4852
Ethics Approval And Informed Consent
This study utilized de-identified retrospective claims data, and as such, this study does not require institutional review board (IRB) review and approval or informed consent procedures.
Data Sharing
To request access to patient-level data and documents for this study, please submit an enquiry via www.clinicalstudydatarequest.com. Data included in this manuscript are contained in a database owned by IQVIA and contain proprietary elements, and therefore data cannot be broadly disclosed or made publicly available at this time. The disclosure of this data to third-party clients assumes certain data security and privacy protocols are in place and that the third-party client has executed IQVIA’s standard license agreement, which includes restrictive covenants governing the use of the data.
Author Contributions
The authors meet criteria for authorship as recommended by the International Committee of Medical Journal Editors, have made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data, take responsibility for the integrity of the work as a whole, contributed to the writing and revising of the manuscript, and have given final approval for the version to be published. All authors take complete responsibility for the integrity of the data and accuracy of the data analysis.
Funding
This study was funded by GlaxoSmithKline (GSK; study number HO-16-16515). The funders of the study had a role in the study design, data analysis, data interpretation, and writing of the report. Employees of Analysis Group were not paid for manuscript development.
Disclosure
CMA and SF are employees of GSK and hold stocks/shares in GSK. FL, GG, JWW, and MSD are employees of Analysis Group, Inc., a consulting company that has received research funds from GSK to conduct this study. The authors report no other conflicts of interest in this work.
References
- 1.Centers for Disease Control and Prevention. National Current Asthma Prevalence; 2016. Available from: https://www.cdc.gov/asthma/most_recent_data.htm. Accessed October3, 2018.
- 2.Peters SP, Jones CA, Haselkorn T, Mink DR, Valacer DJ, Weiss ST. Real-world Evaluation of Asthma Control and Treatment (REACT): findings from a national web-based survey. J Allergy Clin Immunol. 2007;119(6):1454–1461. doi: 10.1016/j.jaci.2007.03.022 [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Uncontrolled Asthma among Persons with Current Asthma. Available from: https://www.cdc.gov/asthma/asthma_stats/uncontrolled_asthma.htm. Accessed February, 2018.
- 4.Peters SP, Ferguson G, Deniz Y, Reisner C. Uncontrolled asthma: a review of the prevalence, disease burden and options for treatment. Respir Med. 2006;100(7):1139–1151. doi: 10.1016/j.rmed.2006.03.031 [DOI] [PubMed] [Google Scholar]
- 5.Global GINA Strategy for Asthma Management and Prevention; 2018. Available from: http://ginasthma.org/2018-gina-report-global-strategy-for-asthma-management-and-prevention/. Accessed March, 2018.
- 6.US Department of Health and Human Services, National Institutes of Health. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: National Heart, Lung, and Blood Institute (US); 2007. [Google Scholar]
- 7.Wu AC, Butler MG, Li L, et al. Primary adherence to controller medications for asthma is poor. Ann Am Thorac Soc. 2015;12(2):161–166. doi: 10.1513/AnnalsATS.201410-459OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Makhinova T, Barner JC, Richards KM, Rascati KL. Asthma controller medication adherence, risk of exacerbation, and use of rescue agents among texas medicaid patients with persistent asthma. J Manag Care Spec Pharm. 2015;21(12):1124–1132. doi: 10.18553/jmcp.2015.21.12.1124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Llano LP, Sanmartin AP, Gonzalez-Barcala FJ, et al. Assessing adherence to inhaled medication in asthma: impact of once-daily versus twice-daily dosing frequency. The ATAUD study. J Asthma. 2018;55(9):1–6. [DOI] [PubMed] [Google Scholar]
- 10.Williams LK, Joseph CL, Peterson EL, et al. Patients with asthma who do not fill their inhaled corticosteroids: a study of primary nonadherence. J Allergy Clin Immunol. 2007;120(5):1153–1159. doi: 10.1016/j.jaci.2007.08.020 [DOI] [PubMed] [Google Scholar]
- 11.Gamble J, Stevenson M, McClean E, Heaney LG. The prevalence of nonadherence in difficult asthma. Am J Respir Crit Care Med. 2009;180(9):817–822. doi: 10.1164/rccm.200902-0166OC [DOI] [PubMed] [Google Scholar]
- 12.Bender BG, Pedan A, Varasteh LT. Adherence and persistence with fluticasone propionate/salmeterol combination therapy. J Allergy Clin Immunol. 2006;118(4):899–904. doi: 10.1016/j.jaci.2006.07.002 [DOI] [PubMed] [Google Scholar]
- 13.Apter AJ, Boston RC, George M, et al. Modifiable barriers to adherence to inhaled steroids among adults with asthma: it’s not just black and white. J Allergy Clin Immunol. 2003;111(6):1219–1226. doi: 10.1067/mai.2003.1479 [DOI] [PubMed] [Google Scholar]
- 14.Williams LK, Pladevall M, Xi H, et al. Relationship between adherence to inhaled corticosteroids and poor outcomes among adults with asthma. J Allergy Clin Immunol. 2004;114(6):1288–1293. doi: 10.1016/j.jaci.2004.09.028 [DOI] [PubMed] [Google Scholar]
- 15.Dima AL, Hernandez G, Cunillera O, Ferrer M, de Bruin M; Astro-Lab group. Asthma inhaler adherence determinants in adults: systematic review of observational data. Eur Respir J. 2015;45(4):994–1018. doi: 10.1183/09031936.00172114 [DOI] [PubMed] [Google Scholar]
- 16.Makela MJ, Backer V, Hedegaard M, Larsson K. Adherence to inhaled therapies, health outcomes and costs in patients with asthma and COPD. Respir Med. 2013;107(10):1481–1490. doi: 10.1016/j.rmed.2013.04.005 [DOI] [PubMed] [Google Scholar]
- 17.Bender BG, Bender SE. Patient-identified barriers to asthma treatment adherence: responses to interviews, focus groups, and questionnaires. Immunol Allergy Clin North Am. 2005;25(1):107–130. doi: 10.1016/j.iac.2004.09.005 [DOI] [PubMed] [Google Scholar]
- 18.US Food and Drug Administration. New Drug Application (NDA): 207070 (Spiriva Respimat); 2015. Available from: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=207070. Accessed March, 2018.
- 19.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83 [DOI] [PubMed] [Google Scholar]
- 20.Kew KM, Dahri K. Long-acting muscarinic antagonists (LAMA) added to combination long-acting beta2-agonists and inhaled corticosteroids (LABA/ICS) versus LABA/ICS for adults with asthma. Cochrane Database Syst Rev. 2016;1:CD011721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kerstjens HAM, Engel M, Dahl R, et al. Tiotropium in asthma poorly controlled with standard combination therapy. N Engl J Med. 2012;367(13):1198–1207. doi: 10.1056/NEJMoa1208606 [DOI] [PubMed] [Google Scholar]
- 22.Kerstjens HA, Disse B, Schroder-Babo W, et al. Tiotropium improves lung function in patients with severe uncontrolled asthma: a randomized controlled trial. J Allergy Clin Immunol. 2011;128(2):308–314. doi: 10.1016/j.jaci.2011.04.039 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Centers for Disease Control and Prevention. National Current Asthma Prevalence; 2016. Available from: https://www.cdc.gov/asthma/most_recent_data.htm. Accessed October3, 2018.