Abstract
Background
Paraneoplastic chorea is typically a subacute progressive hyperkinetic movement disorder. The mainstay of treatment is managing the underlying neoplasm. However, the clinical course may be variable, and effective symptomatic management can precede the start of cancer treatment.
Case report
A 63-year-old man presented with insidious onset, slowly progressive generalized chorea for 1 year, later diagnosed as anti-CV2/CRMP5 autoantibody positive paraneoplastic chorea. His chorea was markedly improved with intravenous amantadine.
Discussion
In patients with anti-CV2/CRMP5 autoantibody-related chorea, sequential follow-up of brain magnetic resonance imaging reveals progression from active inflammation to atrophy. Our report highlights the efficacy of intravenous amantadine in paraneoplastic chorea.
Keywords: Paraneoplastic, autoimmune, CRMP5, CV2, chorea
Introduction
Paraneoplastic chorea is a rare hyperkinetic movement disorder caused by remote effects of the underlying neoplasm on the basal ganglia.1 Anti-CV2/CRMP5 autoantibody is the most commonly detected anti-neuronal autoantibody.2 Patients with typical paraneoplastic chorea show fully developed chorea in the course of weeks to months with acute inflammation in the striatum.1,2 Median survival period depends on the underlying cancer and related antibody but generally ranges from 10 to 20 months.3,4 Regarding the treatment approach, the best option for symptomatic management remains unclear. We reported a case of anti-CV2/CRMP5 autoantibody positive paraneoplastic chorea presenting with insidious onset and slow progression, decreased striatal volume on serial follow-up magnetic resonance imaging (MRI), effectively managed with intravenous amantadine prior to anti-cancer management.
Case report
A 63-year-old man presented at our clinic with slowly progressive chorea starting from the neck of 1-year duration. The patient was a 60 pack-year smoker with hypertension and was undergoing a statin drug treatment for dyslipidemia at the time of presentation. In anamnesis, there was no family history of movement disorder or stroke, or evidence of recent infection or weight change; slow development of chorea that had spread to the right arm and affected gait as a consequence was noted. Initially, chorea was managed with clonazepam (1 mg/d) and haloperidol (1.5 mg/d). At post-treatment, mild improvement of symptoms was observed initially with gradual worsening over the next 6 months. After increasing the dose of haloperidol, the improvement of chorea was achieved, but the development of Parkinsonism as a side effect was noted. Therefore, haloperidol was switched to quetiapine (400 mg/d), but the relapse of chorea was observed. When the patient was referred to our clinic 12 months after the symptom onset (Video 1), his previous medical records were not accessible.
On the brain MRI images acquired at 12 months after the symptom onset, marked bilateral striatal atrophy was observed (Figure 1B). Peripheral blood smear, fasting glucose, and glucose tolerance test were unremarkable. Tumor markers, including carcinoembryonic antigen, prostate-specific antigen, and carbohydrate antigen 19-9 were normal. Genetic tests for spinocerebellar ataxia type 17 and Huntington’s disease were negative. In the results of detailed neuropsychiatric cognitive assessment (Seoul Neuropsychological Screening Battery, 2nd edition),5,6 mild cognitive impairment was revealed especially regarding frontal lobe function. In addition, mild depression was noted in the abbreviated version of Geriatric Depression Scale (6/15).7
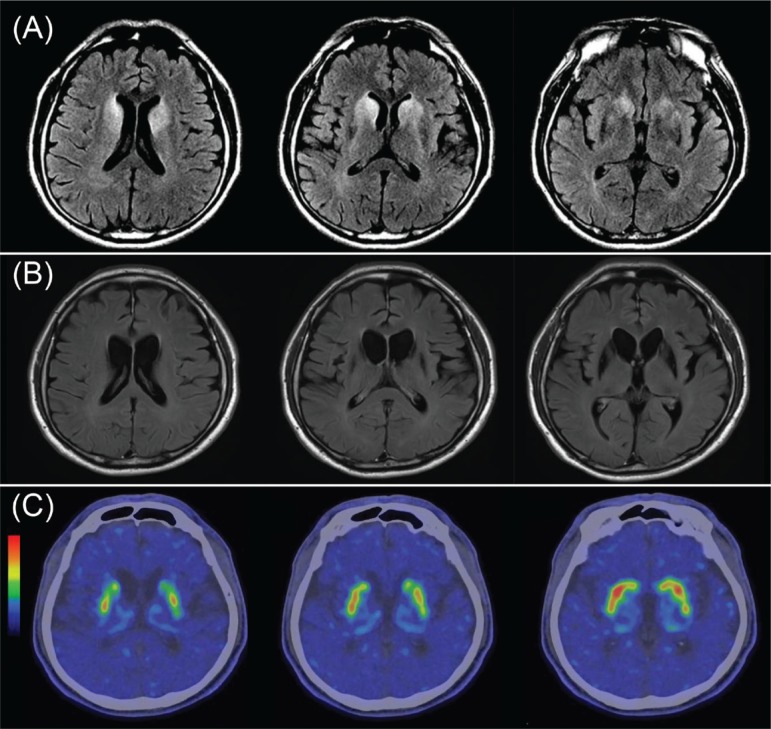
Figure 1.
Structural and Functional Imaging of the Patient’s Brain. Brain MRI nonenhanced T2 FLAIR images acquired 4 months (A) and 12 months (B) after initial symptom showed marked striatal hyperintensity and striatal atrophy, respectively, and FP-CIT PET scan showed a decrease in DAT binding in the bilateral striatum (C). Abbreviations: [18F] N-(3-fluoropropyl)-2β-carbomethoxy-3β-(4-iodophenyl) nortropane (FP-CIT) positron emission tomography (PET); DAT, Dopamine Active Transporter; FLAIR, Fluid Attenuated Inversion Recovery; MRI, Magnetic Resonance Imaging.
After initial work-up at our clinic, we were able to assess the previous brain MRI scans acquired 4 months after the symptom onset. T2-hyperintensities were present in the bilateral caudate nucleus and anterior putamen (Figure 1A). On the [18F] N-(3-fluoropropyl)-2β-carbomethoxy-3β-(4-iodophenyl) nortropane (FP-CIT) positron emission tomography (PET) scan, decreased uptake in the bilateral striatum, especially in the caudate nucleus was obtained (Figure 1C). The anti-CV2/CRMP5 autoantibody was tested positive in a qualitative analysis using serum and cerebrospinal fluid mixture. Meanwhile, the diagnosis of small cell lung cancer with metastasis in the lymph node, first lumbar spine, and left ureter was made based on the malignancy workup.
Before any treatment plan for the lung cancer was implemented, intravenous amantadine (200 mg in 500 cm3 of normal saline given over a 3-hour period, twice per day for 5 days) was administered to manage chorea; in response, remarkable improvements in chorea, especially of the limbs and trunk were attained, and consequently, the patient’s gait was improved (Video 2). We confirmed the efficacy and safety of drug treatment in our patient and made the switch from intravenous amantadine to oral amantadine (200 mg/d). At the outpatient clinic, the dose of oral amantadine was increased from 200 to 300 mg/d, and beneficial effect of the treatment was maintained at 3 years’ follow-up.
Video 1.
Before Intravenous Amantadine Treatment. Chorea mainly involving the face, neck, and both upper extremities, with mild involvement of the lower extremities while sitting down with feet touching the floor is observed. Slight loss of balance and augmentation of chorea is noted when performing the pull-test. Wide-based choreiform gait with irregular step length differential is seen during free gait.
Video 2.
After Intravenous Amantadine Treatment. Partial improvement of chorea involving the face, neck, and both the upper extremities and some restoration in gait and postural balance is observed. At follow-up interview on symptoms, the patient reported improvement in using spoon while eating and in gait.
Discussion
We reported a case of slowly progressive generalized chorea associated with metastatic small cell lung cancer. We demonstrated a change from active inflammatory state to atrophy through serial MRI and suggested the effectiveness of IV amantadine in treatment of the patient’s chorea.
Orolingual chorea and retrocollis may resemble tardive dyskinesia. However, at an initial visit with the attending physician (JH Lee), the patient reported no prior exposure to any antiemetic or antipsychotic medication and was experiencing milder form of chorea that was compatible with hyperkinetic movements observed in our clinic 12 months later (Video 1). Subsequently, the patient underwent treatment with haloperidol, which initially showed improvement of chorea. Based on these facts, we considered that chorea in our patient was due to paraneoplastic syndrome and not tardive dyskinesia.
Brain MRI performed 12 months after the symptom onset revealed severe atrophy in the striatum, most prominently involving bilateral head of the caudate nuclei. Subsequently, we assessed the brain MRI scans acquired previously at other hospitals and observed T2-hyperintensities in the identical regions, which agree with the findings of another report of cases of paraneoplastic chorea with positive anti-CV2/CRMP5 autoantibody that included changes of T2-hyperintenssity in the basal ganglia.2 Moreover, FP-CIT PET revealed decreased uptake of dopamine transporter which may be associated with severe striatal atrophy (Figure 1B), a finding most likely explained as a remnant of active inflammation (Figure 1A). Persistence of atrophic landmarks after inflammation suggests pathophysiology involving irreversible cytotoxic process. Previous studies have reported presynaptic dopaminergic deficit in patients with hyperglycemic chorea and Huntington’s disease,8,9 but not in those with paraneoplastic chorea with anti-CV2/CRMP5 autoantibody. To the best of our knowledge, this is the first case report to present a time-series follow-up brain MRI, with conclusive FP-CIT PET scan finding of decreased presynaptic dopaminergic uptake in the bilateral striatum in a patient with paraneoplastic chorea.
Immunomodulatory therapy with intravenous immunoglobulin and steroids achieved some success in the control of chorea in patients with paraneoplastic chorea; however, there is no consensus on symptomatic management in such cases.10,11 Few randomized placebo-controlled trials on treatment with amantadine are reported for Huntington’s disease.12,13 Studies have indicated that the pathophysiology of chorea in Huntington’s disease can be explained by imbalance between indirect and direct pathways due to selective involvement of indirect pathway.14 We considered that the effectiveness of amantadine on chorea of anti-CV2/CRMP5-related chorea was due to modulation of the imbalance between direct and indirect pathways in the basal ganglia by two possible mechanisms: (1) decrease of glutaminergic input from the neocortices and consequently, decrease of total motor output, and (2) sensitization of the globus pallidus pars interna (GPi) to glutaminergic input and augmentation of inhibitory response at the thalamus. Clinicians should consider IV amantadine as a low-cost alternative treatment to control activity-limiting severe chorea in patients with paraneoplastic chorea before initiating other immunomodulatory therapy or cancer treatment.
One of the limitations of our case report was that our antibody testing was performed only in a qualitative manner. Nevertheless, the method was already validated in previously published literature.15 Future studies focused on changes of autoantibody titers before and after treatment with amantadine are needed.
In conclusion, the findings of time-series follow-up brain MRI in anti-CV2/CRMP5 autoantibody-related chorea indicated the change from active inflammation to atrophy according to the clinical course, which may reflect the mechanisms involved in pathophysiology of the disease. Moreover, IV amantadine showed potential as a viable option for symptomatic management in anti-CV2/CRMP5 autoantibody-related paraneoplastic chorea.
Acknowledgments
We thank the patient and his family for their cooperation.
Footnotes
Citation: Ha J, Na BS, Ahn JH, Kim M, Kim JW, Lee JH, et al. Anti-CV2/CRMP5 paraneoplastic chorea effectively managed with intravenous amantadine. Tremor Other Hyperkinet Mov. 2019: 9. doi: 10.7916/tohm.v0.701
Editor: Elan D. Louis, Yale University, USA
Funding: None.
Financial Disclosures: None.
Conflicts of Interest: The authors report no conflicts of interest.
Ethics Statement: All patients that appear on video have provided written informed consent; authorization for the videotaping and for publication of the videotape was provided.
References
- 1.Goldstein L, Djaldetti R, Benninger F. Anti-Yo, chorea and hemiballismus: a case report. J Clin Neurosci 2017;42:113–114. doi: 10.1016/j.jocn.2017.03.045 [DOI] [PubMed] [Google Scholar]
- 2.Aydin D, Somnier F, Lassen LH. Paraneoplastic choreoathetosis in a patient with small cell lung carcinoma and anti-CRMP5/CV2: a case report. Case Rep Neurol 2016;8(1):16–19. doi: 10.1159/000443522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Honnorat J, Cartalat-Carel S, Ricard D, Camdessanche JP, Carpentier AF, Rogemond V, et al. . Onco-neural antibodies and tumour type determine survival and neurological symptoms in paraneoplastic neurological syndromes with Hu or CV2/CRMP5 antibodies. J Neurol Neurosurg Psychiatry 2009;80(4):412–416. doi: 10.1136/jnnp.2007.138016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vigliani MC, Honnorat J, Antoine JC, Vitaliani R, Giometto B, Psimaras D, et al. . Chorea and related movement disorders of paraneoplastic origIn: the PNS EuroNetwork experience. J Neurol 2011;258(11):2058–2068. doi: 10.1007/s00415-011-6074-1 [DOI] [PubMed] [Google Scholar]
- 5.Kang Y, Jahng S, Na DL. Seoul neuropsychological screening battery, 2nd edition (SNSB-II). Seoul: Human Brain Research & Consulting Co; 2012. [Google Scholar]
- 6.Kang IW, Beom IG, Cho JY, Son HR. Accuracy of Korean-mini-mental status examination based on Seoul neuro-psychological screening battery II results. Korean J Fam Med 2016;37(3):177–181. doi: 10.4082/kjfm.2016.37.3.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sheikh J, Brink TL. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version Clinical gerontology: a guide to assessment and intervention. New York: Haworth Press; 1986. doi: 10.1300/J018v05n01_09 [DOI] [Google Scholar]
- 8.Gamez J, Lorenzo-Bosquet C, Cuberas-Borros G, Carmona F, Hernandez-Vara J, Castillo J, et al. . Does reduced [(123)I]-FP-CIT binding in Huntington’s disease suggest pre-synaptic dopaminergic involvement? Clin Neurol Neurosurg 2010;112(10):870–875. doi: 10.1016/j.clineuro.2010.07.014 [DOI] [PubMed] [Google Scholar]
- 9.Belcastro V, Pierguidi L, Tambasco N, Sironi L, Sacco L, Corso A, et al. . Decreased contralateral putamen [I]FP-CIT SPECT uptake in hyperglycemic hemichorea-hemiballismus. Eur Neurol 2011;65(5):307–308. doi: 10.1159/000327305 [DOI] [PubMed] [Google Scholar]
- 10.Honnorat J. Early-onset immunotherapy by intravenous immunoglobulin and corticosteroids in well characterized onconeural-antibody-positive paraneoplastic neurological syndrome. Clin Exp Immunol 2014;178 Suppl 1:127–129. doi: 10.1111/cei.12539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parsamehr B, Meseeha M, Kolade V. CRMP5-positive paraneoplastic encephalitis in a patient with occult small cell lung cancer. Chest 2016;150(4):750A. doi: 10.1016/j.chest.2016.08.845 [DOI] [Google Scholar]
- 12.Verhagen Metman L, Morris MJ, Farmer C, Gillespie M, Mosby K, Wuu J, et al. . Huntington’s disease: a randomized, controlled trial using the NMDA-antagonist amantadine. Neurology 2002;59(5):694–699. doi: 10.1212/wnl.59.5.694 [DOI] [PubMed] [Google Scholar]
- 13.O’Suilleabhain P, Dewey RB Jr. A randomized trial of amantadine in Huntington disease. Archiv Neurol 2003;60(7):996–998. doi: 10.1001/archneur.60.7.996 [DOI] [PubMed] [Google Scholar]
- 14.Galvan L, André VM, Wang EA, Cepeda C, Levine MS. Functional differences between direct and indirect striatal output pathways in Huntington’s disease. J Huntington’s Dis 2012;1(1):17–25. doi: 10.3233/JHD-2012-120009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lancaster E, Lai M, Peng X, Hughes E, Constantinescu R, Raizer J, et al. . Antibodies to the GABA(B) receptor in limbic encephalitis with seizures: case series and characterisation of the antigen. Lancet Neurol 2010;9(1):67–76. doi: 10.1016/s1474-4422(09)70324-2 [DOI] [PMC free article] [PubMed] [Google Scholar]