Abstract
Adverse childhood experiences (ACEs; e.g., parental divorce, physical or sexual abuse) are more prevalent in individuals with chronic pain compared to the general population. Both increased maternal ACEs and chronic pain have been associated with poor physical and emotional functioning in offspring. However, the mechanisms driving these associations are poorly understood. Thus, this cross-sectional study evaluated the relation between maternal ACEs, mothers’ current functioning, and children’s physical and emotional functioning in a sample of mothers with chronic pain and their 8–12 year-old children. Results indicated a higher prevalence of at least 1 ACE in this sample of mothers with chronic pain (84%) compared to normative data from a community sample of women. Higher maternal ACE scores corresponded with lower physical and social functioning, greater anxiety and depressive symptoms, greater fatigue and sleep disturbances, and greater pain intensity and pain interference in mothers. Higher maternal ACE scores significantly correlated with higher child self-reported depressive symptoms, but not somatic symptoms or functional impairment. A path model indicated that maternal depressive symptoms accounted for the relation between higher maternal ACE scores and children’s depressive symptoms. Intervening on maternal depression among mothers with chronic pain may reduce the impact of intergenerational ACE transmission.
Perspective:
This article presents evidence regarding the intergenerational impact of adverse childhood experiences in a large sample of mothers with chronic pain and their school-aged children. Maternal depressive symptoms accounted for the relation between maternal ACEs and children’s depressive symptoms providing evidence regarding targets for preventive interventions.
Keywords: chronic pain, pediatric pain, adverse childhood experiences, ACEs, depression
Introduction
Exposure to adverse childhood experiences (ACEs) (e.g. abuse, neglect, parental divorce, etc.) has been linked to a number of poor physical and mental health outcomes in adulthood.12 These poor health outcomes often include multiple somatic symptoms, chronic pain, depression and anxiety.9, 28, 42 In a study examining ACE prevalence in childhood, and risk of frequent headaches in adulthood, researchers found that as ACE scores increased, the prevalence and risk of headaches increased significantly.1 Individuals diagnosed with fibromyalgia are more likely to report experiencing ACEs than the general population,33 and among adults with headaches, ACEs are associated with overlapping chronic pain conditions,42 chronic versus episodic migraine,41 and comorbid anxiety and depressive symptoms.40 Further, women experience higher levels of ACEs than men with approximately 15% of women experiencing 4 or more ACEs compared to 9% of men.35 Thus, the relation between ACEs and chronic pain symptoms may be particularly important to evaluate in females.
Maternal ACEs and chronic pain have both been associated with poor physical and emotional health in children.29, 39 A recent study found maternal ACEs were significantly associated with their children’s developmental risk and that maternal depressive symptoms may be a potential mediator of this relationship.39 Additional work has demonstrated that there is an intergenerational transmission of maternal adversity on infant socioemotional symptoms via adult maternal emotional outcomes (specifically depressive symptoms).29 Similarly, children of mothers with chronic pain are at increased risk for poor emotional and physical functioning.16 A recently developed integrative conceptual model proposed potential mechanisms through which risk for chronic pain may be intergenerationally conferred, including social learning, parenting, and stressful environments.38 While the present article focuses on baseline data, the larger study that this data was derived from will examine intergenerational pain transmission over three years. A history of ACEs in mothers with chronic pain could impact a number of these proposed mechanisms. For example, mothers who have experienced more ACEs are more likely to experience depression or posttraumatic stress symptoms which may lead to difficulties with parenting and fostering secure attachments with their children.7 Although the impact of maternal ACEs has not been examined in offspring of parents with chronic pain, the increased rates of trauma in adults with chronic pain relative to the general population suggests ACEs in mothers with chronic pain and their potential impact on children may be important to evaluate.20
This study first aimed to evaluate the prevalence of ACEs in a large sample of mothers with chronic pain who have school-aged children. We expected a higher number of total ACEs in our sample relative to published rates of ACEs for women in the general population. Second, we aimed to examine the relation between maternal ACEs and mothers’ own physical and emotional functioning, hypothesizing that a higher number of maternal ACEs would be associated with lower physical functioning and greater psychological symptoms. Third, we evaluated the association between maternal ACEs and children’s pain, somatic symptoms, physical function, and depressive symptoms. We hypothesized that children of mothers who reported more ACEs would report greater pain frequency, somatic symptoms, functional impairment, and depressive symptoms. Finally, the present study evaluated two models to examine potential mechanisms which may account for the association between maternal ACEs and children’s symptoms: (1) whether maternal physical functioning accounts for the association between maternal ACEs and children’s functional impairment, and (2) whether maternal depressive symptoms account for the association between maternal ACEs and children’s depressive symptoms. We hypothesized that mothers with more ACEs would experience greater depressive symptoms and have poorer physical functioning which would account for greater depressive symptoms and greater functional impairment in their children.
Methods
Participants
Mothers with chronic pain and their children (n = 326 dyads) were recruited as a part of a longitudinal, observational, multisite study evaluating the impact of maternal chronic pain on children’s emotional and physical functioning as they transition from childhood to adolescence. The present study utilized baseline data collected between August 16, 2016 and March 22, 2018; reported results are cross-sectional. Eligibility criteria for mothers included: (a) the presence of a current chronic pain condition for the past 6 months or more, (b) pain occurring at least weekly, (c) seeking specialty medical care for chronic pain within the past 6 months, (d) living in the same home as the participating biological child at least 50% of the time, and (e) ability to complete online questionnaires in English. Children were eligible to participate in the present study if they were 8–12 years old at the start of participation and had the cognitive and English language abilities to complete online questionnaires. Children were enrolled between the ages of 8–12 to capture pain experiences during the transition to adolescence over a 3–year period of development. By the end of the study, child participants will be 11–15 years of age, a period of development when the incidence of chronic pain increases. Exclusion criteria for both mothers and children included: (a) current pain attributable to a life-threatening or chronic illness (e.g., cancer or diabetes) and (b) psychiatric hospitalization within the past 6 months.
Procedures
Mothers were recruited from tertiary referral pain clinics at three major academic medical centers in the Western United States, research databases (e.g., ResearchMatch), and through online advertisements on social media (e.g., Facebook, Twitter). The institutional review board at each academic medical center where participant recruitment occurred approved the study protocol. Mothers first completed an initial contact form indicating interest in receiving more information about the study. Once received by the study team, trained research assistants spoke with each interested individual over the phone to provide further information regarding the study, screen for eligibility, and review the informed consent and assent forms. After consent, dyads were enrolled in the study and completed all study questionnaires through Research Electronic Data Capture (REDCap), a secure online data collection site.13 Mothers were specifically instructed to have their child complete the questionnaires independently and only provide assistance with unfamiliar words in order to reduce bias. After completing all study procedures for the baseline time point, mother and child were each compensated with a $30 electronic gift card to an online retailer; compensation increased by $10 each year that the family continued to participate.
Measures
Parent Measures:
Adverse Childhood Experiences (ACE) Questionnaire.
The ACE questionnaire was designed to assess ten categories of childhood trauma that occurred before an individual’s 18th birthday. These categories include: 1) emotional, 2) physical, or 3) sexual abuse, 4) lack of emotional support, 5) basic needs unmet, 6) parental separation or divorce, 7) violence against female relatives, or 8) living with household members who were substance abusers, 9) mentally ill, or 10) imprisoned.12
Maternal Pain Characteristics.
Mothers completed a questionnaire regarding their current pain problem and chronic pain history. Current pain locations were assessed with a body map in REDCap. Generalized pain was calculated with criteria commonly used for diagnosing fibromyalgia by computing sum scores for each of the five body regions (left upper, right upper, axial, left lower, right lower).45 If 4 out of 5 regions were reported as having pain on the Widespread Pain Index (WPI) body map then the participant met criteria for generalized pain. Jaw, chest, and abdominal pain were not included in the definition of generalized pain. In addition to current pain characteristics, mothers also reported age of onset. Mothers who reported a pain onset prior to age 18 were considered to have childhood-onset chronic pain.
PROMIS-29 Profile v.2.0.
Mothers completed the PROMIS-29 Profile,15 which assesses general emotional health and physical functioning throughout 7 domains (4 questions each). The domains include Pain Interference, Physical Functioning, Anxiety, Depression, Fatigue, Sleep Disturbance, and Ability to Participate in Social Roles and Activities. For each PROMIS domain, the prorated total raw score is computed using the number of items completed and is then converted to T-scores. For each of the domains, excluding Ability to Participate in Social Roles and Activities and Sleep disturbance, a T-score of 50 is representative of the average United States population. Ability to Participate in Social Roles and Activities and Sleep disturbance was enhanced for chronic illness and represents a calibration sample rather than the general United States population. An 8th domain, pain intensity, is rated on a numeric rating scale ranging from 0 “not at all” to 10 “worst pain imaginable” and is not converted to a T-score during the scoring process.4 In the present study, all 7 domains exhibited high internal consistency (Cronbach’s α range: 0.83 – 0.94).
Child Measures:
Child Pain Frequency.
Children reported on their own pain frequency using a survey question asking, “In the past three months how often have you had aches or pains?” Response options range from “0 – Not at all” to “6 – Daily.”
PROMIS Pediatric Depressive Symptoms Short Form.
Children completed the PROMIS pediatric depressive symptoms short form (8 items).19 This measure assesses depressive symptoms in pediatric samples, aged 8–17 years and was developed through the use of the PROMIS pediatric item banks. It is not meant to be a diagnostic test for depression, but for general depressive symptoms. Similar to the adult PROMIS profile, this measures depressive symptoms over a 7–day period rated on a 5–point, “0” (Never) to “4” (Almost always) scale. The summed scores are scaled based on a T-score of 50, the same for the adult PROMIS profile. The 8-item short form showed a reliability coefficient of 0.85 in the current sample.
Functional Disability Inventory.
Children completed the Functional Disability Inventory (FDI).44 The FDI measured the extent to which children would have had trouble completing activities due to their health over the past two weeks. Examples of items assessed include difficulty walking upstairs, being at school all day, watching TV, getting to sleep and staying asleep, etc. Children were asked to rate their difficulties on a “0” (No trouble) to “4” (Impossible) scale. The FDI comprised 15-items, yielding total scores ranging from 0 to 60. Higher scores indicate greater functional impairment. Alpha reliability for the FDI in this sample was 0.92.
Children Somatic Symptoms Inventory (CSSI-24).
Children completed the 24–question CSSI to assess children’s somatic symptoms (e.g. headaches, weakness in body, nausea, etc.).43, 44 Children were asked to rate how much they were bothered by each symptom in the past two weeks on a 5–point, “0” (Not at all) to “4” (A whole lot) scale. Total scores range from 0–96 and were computed through summing the items. Higher scores indicate greater somatic symptom distress. Alpha reliability for the CSSI–24 in this sample was 0.91.
Data Analyses
Data analyses were completed using SPSS version 24. First, descriptive statistics were conducted for the ACEs measure to examine the prevalence and distribution of the number of ACEs reported in the current sample. We conducted a chi-square to compare the proportion of mothers reporting at least one ACE in our sample to normative data for women in the United States provided by the Centers for Disease Control and Prevention (CDC)-Kaiser ACE Study.5 Next, independent samples t-tests evaluated differences in ACE scores between mothers with particular pain characteristics (generalized vs. localized, childhood-onset vs. adult-onset). The total number of ACEs were correlated with PROMIS domains using Pearson r correlations to evaluate the relation between ACE scores and mothers’ current symptoms and functioning. Due to the number of maternal domains assessed, the alpha level was set at 0.001 for correlations between maternal ACEs and their own symptoms and functioning. Pearson r correlations also evaluated the relation between maternal ACE scores and children’s depressive symptoms, somatic symptoms, and functional impairment. Spearman’s rho evaluated the relation between maternal ACEs and children’s pain frequency due to its ordinal nature. For correlations with child self-reported symptoms and functioning, the alpha level was set a 0.05. Finally, mediation analyses were conducted using the PROCESS Macro for SPSS.14 The indirect effect was tested using a bootstrap estimation approach with 5000 samples. With this approach, the indirect effect is considered statistically significant if the 95% confidence interval does not cross 0. Based on monte carlo simulations, mediation analyses were adequately powered (β = 0.81) to detect a small effect (0.20) for the indirect pathway with a sample size of 326. A small proportion of dyads were missing data for one of the key variables for the path analyses (n = 2, 0.6%) and were excluded from analyses given that these data were considered missing at random.
RESULTS
Demographics and Pain Characteristics
Table 1 provides a summary of demographic characteristics. The sample is comprised of mothers who were on average 40.3 years old (SD = 5.85, range: 24.49 – 54.31), predominately Caucasian, and married. Children were on average 9.89 years old (SD = 1.39), predominately Caucasian, and female. The majority of mothers reported adult-onset chronic pain (≥ 18 years of age; 73.9%, n = 241), with about one fourth reporting childhood-onset chronic pain (26.1%, n = 85). Mothers reported an average pain intensity of 5.04 (SD = 1.62) on a 0 to 10 numeric rating scale. Nearly half the mothers met criteria for generalized pain based on their self-reported pain locations (45.7%, n = 149).
Table 1.
Demographic characteristics
| Demographic Variable | n = 326 |
|---|---|
| Mother | |
| Maternal age in years, M (SD) | 40.30 (5.85) |
| Marital status, % (n) | |
| Married | 77.6% (253) |
| Divorced or separated | 16.9% (55) |
| Never married | 5.5% (18) |
| Employment status, % (n) | |
| Employed, full or part time | 47.2% (154) |
| Not currently working | 33.4% (109) |
| Receiving disability | 18.4% (60) |
| Annual household income, % (n) | |
| $25,000 or less | 22.7% (38) |
| $25,001 - $49,999 | 21.5% (70) |
| $50,000 - $79,999 | 17.8% (58) |
| $80,000 - $119,999 | 27.9% (91) |
| $120,000 - or more | 17.8% (58) |
| Race, % (n) | |
| Caucasian | 89.9% (293) |
| Minority racial group (Asian, Black, American Indian, Other) | 5.2% (17) |
| Biracial or multiple races | 4.9% (16) |
| Ethnicity, Hispanic, % (n) | 6.7% (22) |
| Generalized pain, % (n) | 45.7% (149) |
| Years since chronic pain onset, M (SD) | 15.81 (9.92) |
| Child | |
| Child age in years, M (SD) | 9.89 (1.39) |
| Child sex, % (n) | |
| Female | 52.1% (170) |
| Male | 47.9% (156) |
| Child race, % (n) | |
| Caucasian | 83.1% (271) |
| Minority racial group (Asian, Black, American Indian, Other) | 4.9% (16) |
| Biracial or multiple races | 12.0% (39) |
| Child ethnicity, Hispanic, % (n) | 12.3% (40) |
| Child pain frequency (past 3 months), % (n) | |
| None | 11.5% (57) |
| Less than 1 time per month | 15.3% (50) |
| 1 to 3 times per month | 26.1% (85) |
| About 1 time per week | 16.3% (53) |
| 2 to 3 times per week | 11.3% (37) |
| 4 to 6 times per week | 6.1% (20) |
| Daily | 7.1% (23) |
Distribution of ACEs in Mothers with Chronic Pain
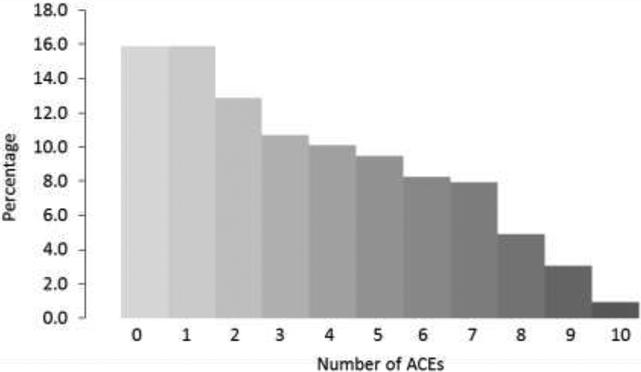
On average, mothers reported 3.42 out of 10 possible ACEs (see Figure 1 for distribution, and Table 2 for Frequency of ACEs). A small proportion of the sample (16.0%, n = 52) reported never experiencing an ACE; thus, a significant majority of the sample experienced at least one ACE (84.0%, n = 274). Results from a chi-square test comparing the proportion of women who experienced at least one ACE in our sample to women in the original CDC-Kaiser ACE Study5 indicated that mothers with chronic pain in our sample were significantly more likely to endorse at least one ACE compared to a sample of women recruited from the general population (65.5%; difference = 18.5%, 95% CI: 14.02 – 22.21%, X2(1) = 48.13, p < 0.001). Further, mothers with chronic pain in our sample were significantly more likely to endorse 4 or more ACEs (44.5%) compared to the sample of women from the CDC-Kaiser ACE Study (15.2%, difference = 29.3%, 95% CI: 23.95 – 34.77, X2(1) = 199.35, p < 0.001).5
Figure 1.
Distribution of ACEs in mothers with chronic pain
Table 2.
Frequency of ACEs in mothers with chronic pain
| Types and frequencies of Maternal ACEs reported* | |
|---|---|
| ACE Q9: Mental illness in household % (n) | 54.0% (176) |
| ACE Q6: Parental separation or divorce % (n) | 50.0% (163) |
| ACE Ql: Emotional abuse % (n) | 47.9% (156) |
| ACE Q4: Emotional neglect % (n) | 44.8% (146) |
| ACE Q8: Household substance abuse % (n) | 40.2% (131) |
| ACE Q3: Sexual abuse % (n) | 34.7% (113) |
| ACE Q2: Physical abuse % (n) | 30.1% (98) |
| ACE Q5: Physical neglect % (n) | 16.6% (54) |
| ACE Q7: Observation of mother/step-mother being treated violently % (n) | 16.3% (53) |
| ACE Q10: Household member in prison % (n) | 8.0% (26) |
| Total ACEs endorsed M (SD) | 3.42 (2.71) |
n=326
ACE Q# refers to the question number on the ACE questionnaire
Mothers most frequently endorsed the following ACEs: (a) mental illness in household, (b) parental separation or divorce, (c) emotional abuse, (d) emotional neglect, and (e) household substance abuse. Sexual abuse and physical abuse were each reported by approximately one-third of the sample (interpersonal violence was determined by a positive answer to either item 2 or item 3) with nearly half (47.9%, n=156) the sample reporting either form of interpersonal violence. Physical neglect, observing their mother being treated violently, and a household member in prison were less frequently endorsed.
Relation of ACEs to Maternal Pain Characteristics
Mothers with childhood-onset chronic pain, compared to mothers with adult-onset chronic pain, reported significantly more ACEs (t[324] = −2.49, p = 0.013; childhood-onset: mean = 4.05, adult-onset: mean = 3.20). Mothers with generalized pain, compared to those without, reported slightly more ACEs (mean = 3.72 vs. mean = 3.17), but this difference did not reach statistical significance (t[299] = −1.83, p = 0.07). Table 3 presents the correlations between maternal ACE scores and domains of physical and emotional functioning from the PROMIS–29. While statistically significant, all correlation coefficients between ACE scores and other variables were small. Higher maternal ACE scores corresponded with lower physical and social functioning, greater anxiety and depressive symptoms, greater fatigue and sleep disturbances, and greater pain intensity and pain interference in mothers.
Table 3.
Correlations between maternal ACE scores and mother’s own symptoms and functioning measured by the PROMIS-29 Profile
| Maternal ACEs | Pain intensity | Pain interference | Anxiety | Depressive symptoms | Fatigue | Sleep disturbance | Physical functioning | Functioning in social roles | |
|---|---|---|---|---|---|---|---|---|---|
| Maternal ACEs Pain intensity | .15 | ||||||||
| Pain interference | .19* | .57* | |||||||
| Anxiety | .23* | .29* | .39* | ||||||
| Depressive symptoms | .18* | .30* | .44* | .71* | |||||
| Fatigue | .23* | .35* | .57* | .46* | .49* | ||||
| Sleep disturbance | .22* | .33* | .44* | .37* | .39* | .52* | |||
| Physical functioning | −.19* | −.43* | −.58* | −.27* | −.37* | −.44* | −.40* | ||
| Functioning in social roles | −.20* | −.36* | −.68* | −.29* | −.38* | −.58* | −.36* | .59* | |
| Mean | 3.42 | 5.91 | 65.01 | 59.22 | 56.52 | 64.17 | 57.99 | 39.29 | 39.93 |
| SD | 2.71 | 1.65 | 6.25 | 8.31 | 8.73 | 8.20 | 7.69 | 6.67 | 6.76 |
Notes:
Significant at the p < 0.001 level
Relation of Maternal ACEs to Children’s Physical and Emotional Functioning
Table 4 presents the correlations between maternal ACE scores and child emotional and physical functioning. Higher maternal ACE scores significantly correlated with higher child self-reported depressive symptoms (r = 0.14, p = 0.02), but not pain frequency (r = 0.08), somatic symptoms (r = 0.02) or functional impairment (r = 0.03). Due to the lack of relation between maternal ACEs and children’s pain, somatic symptoms, and functional impairment, further analyses focus exclusively on children’s depressive symptoms.
Table 4.
Correlations between maternal ACE scores and child symptoms and functioning
| Maternal ACEs | Pain frequency | Depressive symptoms | Somatic symptoms | Functional impairment | |
|---|---|---|---|---|---|
| Maternal ACEs | |||||
| Pain frequency | 0.08 | ||||
| Depressive symptoms | 0.14* | 0.21* | |||
| Somatic symptoms | 0.02 | 0.53* | 0.48* | ||
| Functional impairment | 0.03 | 0.34* | 0.40* | 0.59* | |
| Mean | 48.45 | 14.34 | 7.10 | ||
| SD | 9.47 | 12.59 | 9.08 |
Notes: Correlations with pain frequency are Spearman’s rho. See Table 1 for pain frequency descriptive statistics.
Significant at the p < 0.05 level
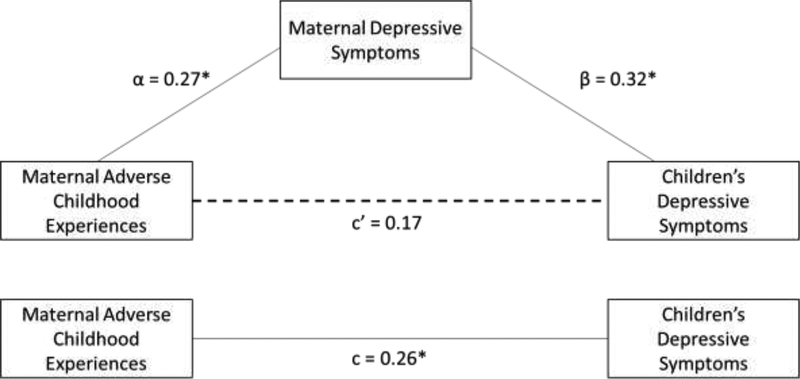
We tested a path model to evaluate the direct and indirect associations between maternal ACEs and children’s depressive symptoms via mother’s own depressive symptoms. Higher maternal ACE scores were associated with greater maternal depressive symptoms (α path, b = 0.27, 95% CI: 0.12, 0.42, p < 0.001), and greater maternal depressive symptoms were associated with greater child depressive symptoms (β path, b = 0.32, 95% CI: 0.15, 0.50, p < 0.001). Higher maternal ACE scores were associated with greater child depressive symptoms (c path, b = 0.26, 95% CI: 0.01, 0.51, p = 0.04), but with the inclusion of maternal depressive symptoms, the relation between maternal ACE scores and child depressive symptoms (c’ path, b = 0.17, 95% CI: −0.08, 0.42, p = 0.17) was no longer significant. The indirect path for the relation between maternal ACE scores and child depressive symptoms via maternal depressive symptoms was significant (αβ = 0.09, bootstrapped 95% CI: 0.03, 0.17, p = 0.01).
Discussion
The experience of multiple ACEs can have lasting adverse effects into adulthood and have been associated with a number of poor health outcomes including chronic pain.18, 20 Consistent with this literature, our study found that mothers with chronic pain reported experiencing significantly more ACEs compared to women in the general population. Furthermore, a higher number of maternal ACEs significantly corresponded with greater maternal pain interference, anxiety, depressive symptoms, fatigue, sleep disturbance, and lower physical and social functioning. Both maternal chronic pain and ACEs could have an intergenerational impact on offspring38, 46 potentially contributing to the perpetuation of a high level of disease burden for some families. We found a significant association between a higher number of maternal ACEs and child depressive symptoms, but not child pain frequency, somatic symptoms, or functional impairment. Results from a path model indicated that for mothers with chronic pain, the intergenerational association between maternal ACEs and children’s psychological functioning may be accounted for by the mother’s depressive symptoms. Other studies suggest similar models for ACE transmission between generations.25, 30 Thus, the intergenerational impact of maternal ACEs on their child’s psychological functioning may be mitigated through preventive interventions focused on maternal depressive symptoms as well as supportive interventions for parenting within the context of challenging health conditions.
As hypothesized, mothers in the current study reported a high number of ACEs compared to women in the general population. The CDC reports that 65.5% of the U.S. women report at least one ACE, while 84% of this chronic pain sample reports at least one ACE, demonstrating a significant difference between groups.35 The occurrence of many ACEs in childhood could result in alterations in physiological processes such as hypothalamic-pituitary-adrenal axis functioning,2 neuronal plasticity6 and epigenetic regulation22 which contribute to the development of chronic pain or exacerbation of other pain complaints; some ACEs may also result in physical injuries that could contribute to the development of chronic pain.
In the current study, a dose-response relationship was observed among ACEs such that as ACEs increased, physical and social functioning declined, anxiety and depressive symptoms increased, as did reports of fatigue, sleep disturbances, pain intensity, and pain interference. These findings align with other literature suggesting that ACEs significantly impact the occurrence and persistence of pain in adulthood.9, 23, 36 For instance, one chronic pain study found that individuals who reported higher tender point counts were significantly more likely to report ACEs.27
Mothers with childhood-onset chronic pain reported experiencing more ACEs compared to mothers with adult-onset chronic pain suggesting that ACEs may contribute to the development of pediatric chronic pain, which then persists into adulthood; ACEs have indeed been associated with pediatric chronic pain.24, 32 A recent study showed that youth who reported ACEs were approximately 20% more likely to be diagnosed with a chronic pain condition in their childhood.32 Adverse experiences in childhood leave a lasting imprint during critical pediatric developmental periods, and appear to alter the trajectory of physical and mental health into adulthood, which can extend into the next generation.22
Contrary to one of our hypotheses, maternal ACEs were not significantly related to children’s somatic symptoms or functional impairment. The current study presents only baseline data from a longitudinal study; all children included in this study denied having any severe illness and were intentionally recruited prior to the onset of adolescence when the incidence of chronic pain substantially increases and thus, represent a generally healthy, but at-risk sample. As the study progresses, it’s possible that longitudinal follow-up will show a relationship between maternal ACEs and trajectories of children’s pain, somatic symptoms, or disability that was not observed in baseline analyses. There is some evidence that children’s depressive symptoms increase risk for the development of pain problems11, 37 and thus, following these children longitudinally could provide greater insight into indirect pathways through which maternal ACEs and chronic pain may impact the development of chronic pain in youth. Although certain pain conditions have a strong genetic component, research indicates that children of parents with chronic pain are at increased risk of developing a chronic pain condition in adulthood beyond any genetic contributions.8, 17, 38 General parenting, family health, and exposure to a stressful environment may play key roles in explaining why children of parents with chronic pain may be at risk for developing chronic pain and poorer psychological outcomes in their adult lives.
Further, it is important to consider the cumulative impact ACEs, current depressive symptoms, and chronic pain could have on parenting. Indeed, research has revealed that among women with chronic pain who have dependents living with them, pain, guilt, and anxiety about how their pain negatively impacts their parent-child relationships is substantial.47 Additionally, these same women report having difficulty prioritizing appropriate self-care due to the competing interests of caregiving for others. Future research is needed to further understand how specific supports and interventions might help support parenting in the context of chronic pain. Furthermore, future studies should examine the effects of paternal ACEs on parent, child, and family functioning.
Our results should be interpreted in light of a number of limitations. The results presented are cross-sectional, therefore no temporal effects can be inferred. However, maternal ACEs are a retrospective report of events which occurred prior to the age of 18, thus it can be inferred that these events preceded current depressive symptom severity. It is also important to note that while maternal ACEs preceded current maternal depressive symptoms, these symptoms may also stem from current stressors; the same may also be true for child depressive symptoms. Child depressive symptoms were, on average, not in the clinical range in this at-risk sample; however, subclinical levels of depressive symptoms are known to impact child and adolescent social development and increase risk for major depressive disorder in adulthood.21, 34
Participants were instructed verbally by study staff during the consent process and in both the parent consent form and the child assent form to have the child complete their study materials independently however, we cannot definitively guarantee that every child report was completed independently by the child. Additionally, while the ACE questionnaire has been well-validated there is the possibility that given the nature of the questions, participants may have underreported or inaccurately reported on these items.3, 31 Children in this study were enrolled when they were between the ages of 8–12 years old; findings may not be generalizable to other age ranges as research suggests that stress effects have a unique impact depending on the developmental period in which they are experienced.26 Lastly, this study’s sample appears to have slightly higher educational attainment on average, compared to general population samples in other studies;10, 35 this, or other sociodemographic features specific to the current sample may limit the generalizability of results.
Despite these limitations, the current study has several strengths, namely the large number of participants, and the dyadic design – comprised of mothers and their biological children – that allowed for examination of symptoms across generations. Further, the focus on possible mechanisms accounting for the relation between maternal ACEs and children’s symptoms is a strength as ACEs in and of themselves likely do not exert a direct path in intergenerational transmission of risk. Given both a high number of maternal ACEs and the presence of maternal chronic pain have been associated with increased risk for adverse physical and psychological health outcomes in children, it is important to consider the potential additive effects of both a high ACE burden and chronic pain in mothers.
Figure 2.
Direct and indirect effects of maternal adverse childhood experiences on children’s depressive symptoms in mothers with chronic pain
Note: *paths significant at p < 0.05 level.
Highlights.
Mothers with chronic pain were more likely to endorse 4+ adverse experiences.
Higher parent childhood adversity scores correlated with higher child depression.
Higher adversity scores correlated with lower physical and social functioning.
Path model identified relation between maternal experiences and child outcomes.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures:
This study was supported by the National Institutes of Health (NIH), Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01 HD082200; PI Wilson), as well as by CTSA awards UL1TR000128/UL1TR002369. AL Stone is supported by award numbers TL1TR002371 and T32GM108554 from NIH. DS Clohessy is supported by the NIH Common Fund and Office of Scientific Workforce Diversity under three awards UL1GM118964, RL5GM118963, and TL4GM118965, administered by the National Institute of General Medical Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The authors have no conflicts of interest to disclose.
References
- 1.Anda R, Tietjen G, Schulman E, Felitti V, Croft J. Adverse childhood experiences and frequent headaches in adults. Headache. 50:1473–1481, 2010 [DOI] [PubMed] [Google Scholar]
- 2.Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, Dube SR, Giles WH. The enduring effects of abuse and related adverse experiences in childhood. European archives of psychiatry and clinical neuroscience. 256:174–186, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bethell CD, Carle A, Hudziak J, Gombojav N, Powers K, Wade R, Braveman P. Methods to Assess Adverse Childhood Experiences of Children and Families: Toward Approaches to Promote Child Well-being in Policy and Practice. Acad Pediatr. 17:S51–S69, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Amtmann D, Bode R, Buysse D, Choi S, Cook K, DeVellis R, DeWalt D, Fries JF, Gershon R, Hahn EA, Lai J-S, Pilkonis P, Revicki D, Rose M, Weinfurt K, Hays R. Initial Adult Health Item Banks and First Wave Testing of the Patient-Reported Outcomes Measurement Information System (PROMIS(™)) Network: 2005–2008. Journal of clinical epidemiology. 63:1179–1194, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention: The ACE Study Survey Data, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Atlanta, GA, 2016. [Google Scholar]
- 6.Champagne DL, Bagot RC, van Hasselt F, Ramakers G, Meaney MJ, de Kloet ER, Joels M, Krugers H. Maternal care and hippocampal plasticity: evidence for experience-dependent structural plasticity, altered synaptic functioning, and differential responsiveness to glucocorticoids and stress. J Neurosci. 28:6037–6045, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chapman DP, Dube SR, Anda RF. Adverse childhood events as risk factors for negative mental health outcomes. Psychiatric Annals. 37:359–364, 2007 [Google Scholar]
- 8.Craig TK, Cox AD, Klein K. Intergenerational transmission of somatization behaviour: a study of chronic somatizers and their children. Psychol Med. 32:805–816, 2002 [DOI] [PubMed] [Google Scholar]
- 9.Davis DA, Luecken LJ, Zautra AJ. Are reports of childhood abuse related to the experience of chronic pain in adulthood? A meta-analytic review of the literature. The Clinical journal of pain. 21:398–405, 2005 [DOI] [PubMed] [Google Scholar]
- 10.Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, Loo CM, Giles WH. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse Negl. 28:771–784, 2004 [DOI] [PubMed] [Google Scholar]
- 11.Dunn KM, Jordan KP, Mancl L, Drangsholt MT, Le Resche L. Trajectories of pain in adolescents: a prospective cohort study. Pain. 152:66–73, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American journal of preventive medicine. 14:245–258, 1998 [DOI] [PubMed] [Google Scholar]
- 13.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 42:377–381, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hayes AF: Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Second Edition edition, Guilford Press, New York, NY, 2013. [Google Scholar]
- 15.Hays RD, Spritzer KL, Schalet BD, Cella D. PROMIS((R))-29 v2.0 profile physical and mental health summary scores. Qual. Life Res, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higgins KS, Birnie KA, Chambers CT, Wilson AC, Caes L, Clark AJ, Lynch M, Stinson J, Campbell-Yeo M. Offspring of Parents with Chronic Pain: A Systematic Review and Meta-Analysis of Pain, Health, Psychological, and Family Outcomes. Pain. 156:2256–2266, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoftun GB, Romundstad PR, Rygg M. Association of parental chronic pain with chronic pain in the adolescent and young adult: family linkage data from the HUNT Study. JAMA Pediatr. 167:61–69, 2013 [DOI] [PubMed] [Google Scholar]
- 18.Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, Jones L, Dunne MP. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet. Public health. 2:e356–e366, 2017 [DOI] [PubMed] [Google Scholar]
- 19.Irwin DE, Stucky B, Langer MM, Thissen D, DeWitt EM, Lai J-S, Varni JW, Yeatts K, DeWalt DA. An item response analysis of the pediatric PROMIS anxiety and depressive symptoms scales. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 19:595–607, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jones GT, Power C, Macfarlane GJ. Adverse events in childhood and chronic widespread pain in adult life: Results from the 1958 British Birth Cohort Study. Pain. 143:92–96, 2009 [DOI] [PubMed] [Google Scholar]
- 21.Kochel KP, Ladd GW, Rudolph KD. Longitudinal associations among youth depressive symptoms, peer victimization, and low peer acceptance: an interpersonal process perspective. Child Dev. 83:637–650, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Labonte B, Suderman M, Maussion G, Navaro L, Yerko V, Mahar I, Bureau A, Mechawar N, Szyf M, Meaney MJ, Turecki G. Genome-wide epigenetic regulation by early-life trauma. Arch Gen Psychiatry. 69:722–731, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lampe A, Doering S, Rumpold G, Solder E, Krismer M, Kantner-Rumplmair W, Schubert C, Sollner W. Chronic pain syndromes and their relation to childhood abuse and stressful life events. J Psychosom Res. 54:361–367, 2003 [DOI] [PubMed] [Google Scholar]
- 24.Larsson B, Sund AM. Emotional/behavioural, social correlates and one-year predictors of frequent pains among early adolescents: influences of pain characteristics. Eur J Pain. 11:57–65, 2007 [DOI] [PubMed] [Google Scholar]
- 25.Le-Scherban F, Wang X, Boyle-Steed KH, Pachter LM. Intergenerational Associations of Parent Adverse Childhood Experiences and Child Health Outcomes. Pediatrics. 141, 2018. [DOI] [PubMed] [Google Scholar]
- 26.Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 10:434–445, 2009 [DOI] [PubMed] [Google Scholar]
- 27.McBeth J, Macfarlane GJ, Benjamin S, Morris S, Silman AJ. The association between tender points, psychological distress, and adverse childhood experiences: a community-based study. Arthritis Rheum. 42:1397–1404, 1999 [DOI] [PubMed] [Google Scholar]
- 28.McCall-Hosenfeld J, Winter M, Heeren T, Liebschutz JM. The association of interpersonal trauma with somatic symptom severity in a primary care population with chronic pain: exploring the role of gender and the mental health sequelae of trauma. Journal of psychosomatic research. 77:196–204, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McDonnell CG, Valentino K. Intergenerational Effects of Childhood Trauma:Evaluating Pathways Among Maternal ACEs, Perinatal Depressive Symptoms, and Infant Outcomes. Child Maltreatment. 21:317–326, 2016 [DOI] [PubMed] [Google Scholar]
- 30.Metzler M, Merrick MT, Klevens J, Ports KA, Ford DC. Adverse childhood experiences and life opportunities: Shifting the narrative. Children and Youth Services Review. 72:141–149, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Murphy A, Steele M, Dube SR, Bate J, Bonuck K, Meissner P, Goldman H, Steele H. Adverse Childhood Experiences (ACEs) questionnaire and Adult Attachment Interview (AAI): implications for parent child relationships. Child Abuse Negl. 38:224–233, 2014 [DOI] [PubMed] [Google Scholar]
- 32.Nelson SM, Cunningham NR, Kashikar-Zuck S. A Conceptual Framework for Understanding the Role of Adverse Childhood Experiences in Pediatric Chronic Pain. The Clinical journal of pain. 33:264–270, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Olivieri P, Solitar B, Dubois M. Childhood risk factors for developing fibromyalgia. Open Access Rheumatology : Research and Reviews. 4:109–114, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry. 55:56–64, 1998 [DOI] [PubMed] [Google Scholar]
- 35.Prevention CfDCa: The ACE Study Survey Data, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Atlanta, GA, 2016. [Google Scholar]
- 36.Sherman AL, Morris MC, Bruehl S, Westbrook TD, Walker LS. Heightened temporal summation of pain in patients with functional gastrointestinal disorders and history of trauma. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 49:785–792, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stahl M, Kautiainen H, El-Metwally A, Hakkinen A, Ylinen J, Salminen JJ, Mikkelsson M. Non-specific neck pain in schoolchildren: prognosis and risk factors for occurrence and persistence. A 4-year follow-up study. Pain. 137:316–322, 2008 [DOI] [PubMed] [Google Scholar]
- 38.Stone AL, Wilson AC. Transmission of risk from parents with chronic pain to offspring: an integrative conceptual model. Pain. 157:2628–2639, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sun J, Patel F, Rose-Jacobs R, Frank DA, Black MM, Chilton M. Mothers’ Adverse Childhood Experiences and Their Young Children’s Development. American journal of preventive medicine. 53:882–891, 2017 [DOI] [PubMed] [Google Scholar]
- 40.Tietjen GE, Brandes JL, Peterlin BL, Eloff A, Dafer RM, Stein MR, Drexler E, Martin VT, Hutchinson S, Aurora SK. Childhood maltreatment and migraine (part I). Prevalence and adult revictimization: a multicenter headache clinic survey. Headache: The Journal of Head and Face Pain. 50:20–31, 2010 [DOI] [PubMed] [Google Scholar]
- 41.Tietjen GE, Brandes JL, Peterlin BL, Eloff A, Dafer RM, Stein MR, Drexler E, Martin VT, Hutchinson S, Aurora SK, Recober A, Herial NA, Utley C, White L, Khuder SA. Childhood maltreatment and migraine (part II). Emotional abuse as a risk factor for headache chronification. Headache. 50:32–41, 2010 [DOI] [PubMed] [Google Scholar]
- 42.Tietjen GE, Brandes JL, Peterlin BL, Eloff A, Dafer RM, Stein MR, Drexler E, Martin VT, Hutchinson S, Aurora SK, Recober A, Herial NA, Utley C, White L, Khuder SA. Childhood maltreatment and migraine (part III). Association with comorbid pain conditions. Headache. 50:42–51, 2010 [DOI] [PubMed] [Google Scholar]
- 43.Walker LS, Beck JE, Garber J, Lambert W. Children’s Somatization Inventory: Psychometric Properties of the Revised Form (CSI-24). Journal of Pediatric Psychology. 34:430–440, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Walker LS, Greene JW. The Functional Disability Inventory: Measuring a Neglected Dimension of Child Health Status1. Journal of Pediatric Psychology. 16:39–58, 1991 [DOI] [PubMed] [Google Scholar]
- 45.Wolfe F, Clauw DJ, Fitzcharles M-A, Goldenberg DL, Häuser W, Katz RL, Mease PJ, Russell AS, Russell IJ, Walitt B. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Seminars in Arthritis and Rheumatism. 46:319–329, 2016 [DOI] [PubMed] [Google Scholar]
- 46.Yehuda R, Halligan SL, Grossman R. Childhood trauma and risk for PTSD: relationship to intergenerational effects of trauma, parental PTSD, and cortisol excretion. Dev Psychopathol. 13:733–753, 2001 [DOI] [PubMed] [Google Scholar]
- 47.Ziadni M, You DS, Wilson AC, Darnall BD. CARE Scale-7: Development and Preliminary Validation of a Measure to Assess Factors Impacting Self-Care in Chronic Pain. The Clinical journal of pain. 34:818–824, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]