Abstract
Objectives:
To evaluate whether pre-emptive analgesia is an effective technique to reduce postoperative delirium (PD) in geriatric patients with hip fracture.
Methods:
This is a double-blind randomized clinical trial. Ninety elderly patients scheduled for hipfracture surgery at HongHui Hospital, Xi’an Jiaotong University, Xi’an, China between March 2018 and January 2019 were divided into 2 groups. On arrival at the emergency department, the experimental group (n=44) received ultrasound-guided continuous fascia iliaca compartment block (FICB) for preoperative analgesia, while the control group (n=46) received generic continuous FICB. All patients received spinal anaesthesia and postoperative patient controlled epidural analgesia (PCEA). We compared the change in preoperative and postoperative pain scores, the incidence of PD, and the consumption of opioid between the 2 groups.
Results:
Five patients did not meet the participation requirements; therefore, 85 patients were included in the study. Patients in the experimental group experienced less preoperative pain (p<0.05). Between the 2 groups, no significant differences were found for postoperative pain scores. The incidence of PD was lower in the experimental group (13.9% versus 35.7%, p=0.018). In addition, before the surgery, a drop in consumption of fentanyl was noted in the experimental group (0.08±0.21 versus 0.28±0.13, p=0.037).
Conclusion:
Pre-emptive analgesia with continuous FICB is an effective technique to reduce PD in geriatric patients with hip fracture.
Hip fracture is common in the elderly. The number of patients undergoing hip fracture surgery is increasing.1 Postoperative delirium (PD) is a common surgical complication and the incidence has been reported to be as high as 40% after hip fracture surgery.2 Postoperative delirium results in increased mortality and morbidity.3 Therefore, it is necessary to explore methods to reduce PD. Severe pain is frequently observed in patients with hip fracture.4 In elderly patients, time to surgery is often prolonged due to poor health and preoperative examination and treatment.5 Thus, patients often suffer longer with preoperative pain. Whether effective preoperative analgesia can reduce the occurrence of PD is unknown.
Fascia iliaca compartment block (FICB) is an alternative method of preoperative analgesia for elderly patients with hip fracture.6 Therefore, we conducted the study to investigate whether pre-emptive analgesia with FICB is an effective technique to reduce PD in geriatric patients with hip fracture.
Methods
The study protocol was approved by the Institutional Review Board of HongHui Hospital. The trial was designed in accordance with the principles of the Declaration of Helsinki and registered at the Chinese Clinical Trial Registry (ChiCTR1800014917). Ninety elderly patients scheduled for hip fracture surgery were enrolled in the study. Inclusion criteria included age 60-80 years and American Society of Anesthesiologists (ASA) physical status II or III. Patients with serious cardiovascular, respiratory, and endocrine diseases (ASA IV); known allergies to local anesthetics; and taking sedatives and analgesics within the last week before hip fracture were excluded from the study. Patients with Mini-Mental State examination (MMSE) scores <27, sleep disorders, and psychiatric illnesses were also excluded.
Using a sealed envelope technique, patients were randomized into the experimental group or control group. On arrival at the emergency department, the experimental group received ultrasound-guided continuous FICB for preoperative analgesia. Continuous FICB was performed under ultrasound guidance by the same anesthesiologist. A total of 30 ml (0.45%) ropivacaine solution was infused. Then an electronic pump was connected to the catheter with 200 ml (0.9%) sodium chloride (NaCl) at a concentration of 0.25% ropivacaine and a speed of 6 ml/h. The control group received generic continuous FICB using 0.9% sodium chloride. On the ward, when patients suffered from severe pain (visual analogue scale [VAS] ≥5), fentanyl 0.05 mg intramascular was given each time by the surgeon. The surgeon was blinded to the study.
The VAS was used to assess the pain (0=no pain, 10=worst pain). Pain assessment was repeated at admission (T1), 2 hours after preoperative analgesia (T2), 4 hours after preoperative analgesia (T3), 6 am on the day of surgery (T4), and upon entering the operation room (T5). The consumption of fentanyl was also recorded.
After completion of the preoperative preparation, patients were scheduled for hip fracture surgery. All patients received intravertebral anesthesia, and the level of anesthesia was maintained at ~T10. Patients received patient controlled epidural analgesia (PCEA) within 48 hours. Age, height, weight, surgical procedure, blood loss, infusion quantity, and surgical time were record in our anesthesia chart.
Postoperative delirium was assessed one hour after the surgery and then twice daily (8 to 10am and 6 to 8pm). At the same time, the intensity of postoperative pain was evaluated using the VAS or Wong-Baker FACE Pain Rating Scale7 (WBS; WBS was used to assess the pain in the patients who became delirious). The diagnostic criteria for PD are as follows: a) acute onset of mental changes and fluctuating course; b) inattention; c) disorganized thinking; and d) altered levels of consciousness. If a patient had the characteristics of a and b, c, or d, the patient was diagnosed with PD.8
Data are shown as the mean±SD, number of patients or n (%). The data was performed using the Statistical Package for Social Sciences for Windows version 19.0 (IBM Corp, Armonk, NY, USA). The demographic characteristics and clinical data were compared using student’s t-test or the χ2 test. The time from admission to surgery, pain scores, and fentanyl consumption were analyzed using the Mann-Whitney U test. The incidence of nausea and vomiting, pruritus, and delirium were analyzed using the χ2 test. A p-value of <0.05 was considered statistically significant.
Results
We recruited a total of 90 patients, and 5 did not meet the participation requirements (Figure 1); therefore, 85 patients were included in the study.
Figure 1.
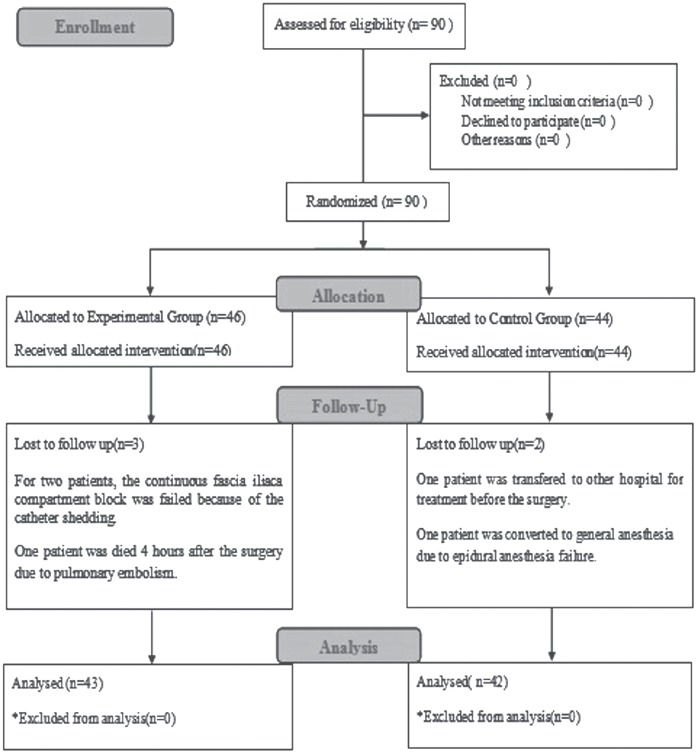
The flowchart of the design and the protocol of the study.
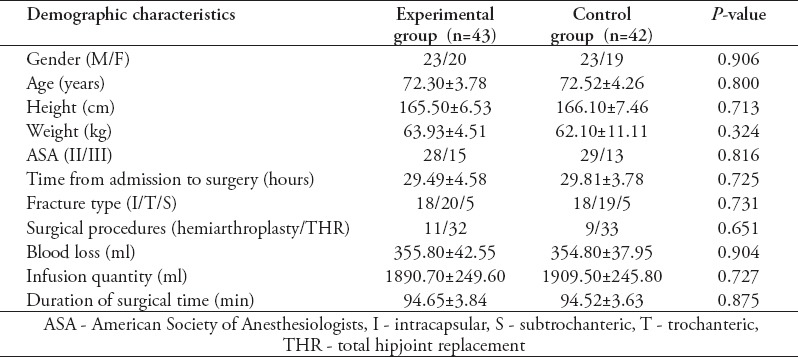
No significant differences were found for age, height, weight, ASA physical status, time from admission to surgery, fracture type, surgical procedures, duration of surgery, infusion quantity, and volume of bleeding between the 2 groups (Table 1).
Table 1.
Demographic characteristics and clinical date in both groups.
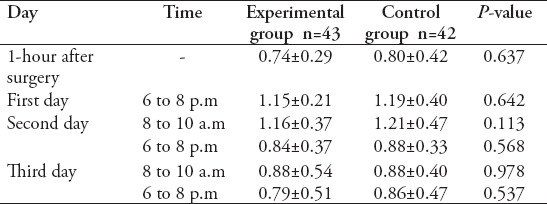
Patients in the experimental group had lower VAS scores compared with the control group, except upon admission (p<0.05) (Table 2), and no significant differences were found for postoperative pain scores between the 2 groups (Table 3).
Table 2.
The intensity of preoperative pain in 2 groups.
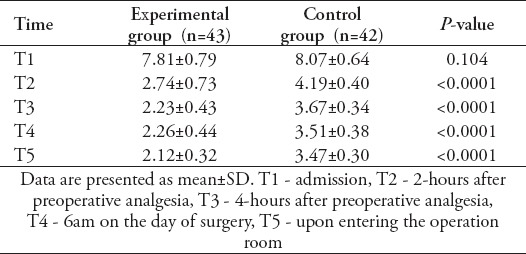
Table 3.
The intensity of postoperative pain after surgery.
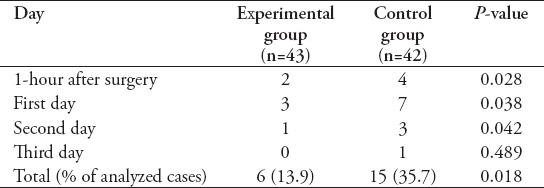
The incidence of PD was significantly lower in the experimental group (13.9% versus 35.7%, p=0.018) (Table 4).
Table 4.
Comparison of the incidence of postoperative delirium between groups.
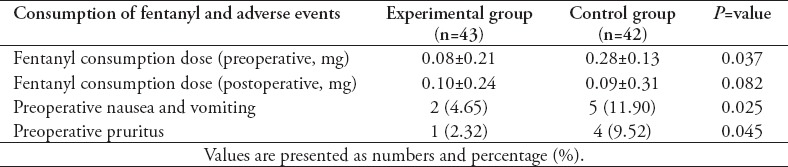
The consumption of fentanyl in the experimental group was significantly less than that in the control group before the surgery (0.08±0.21 versus 0.28±0.13, p=0.037). Before the surgery, there were 5 patients with nausea and vomiting and 4 patients with pruritus in the control group, while there were 2 patients with nauseacand vomiting in the experimental group (p=0.025) (Table 5).
Table 5.
Comparison of total consumption of fentanyl and adverse events between groups.
Discussion
This first outcome of this study is that early continuous FICB significantly attenuated preoperative pain in geriatric patients with hip fracture. Patients with hip fracture often experience severe pain. Opioids remain the most commonly used analgesia. In our study, pain was relieved quickly after fentanyl was administered to the patients. However, the clinical use of opioid drugs still faces many obstacles, such as side effects and analgesic tolerance.9-10
Fascia iliaca compartment block could provide effective preoperative analgesia for the elderly with hip fracture, and its efficacy has been reported to be 90%.11 In our study, there were only 2 failures of the FICB, with a total efficiency of 95%. The use of ultrasonography to guide the FICB increases the reliability of blockade.
Fascia iliaca compartment block is superior to traditional analgesia, such as intramuscular opioids or oral nonsteroidal anti-inflammatory drugs.12,13 In our study, on arrival at the emergency department, patients who received continuous FICB experienced less pain before the surgery, and we found that pre-emptive analgesia with continuous FICB reduced the consumption of fentanyl. Patients who received the FICB before surgery experienced fewer opioid-related symptoms such as nausea, vomiting and pruritus. Therefore, compared with traditional analgesia, continuous FICB was a more effective method to provide preoperative analgesia for the elderly with hip fracture.
The second outcome of this study is that patients who received FICB for preemptive analgesia experienced less PD. The causes of PD are multifactorial, and studies have found that intense postoperative pain is an important precipitating factor and adequate postoperative pain control in patients who have undergone hip fracture surgery allows faster rehabilitation and reduces the rate of PD.14,15 However, the influence of preoperative pain on PD is unknown. In our study, no significant difference in gender, age, height, weight, ASA physical status, time from admission to surgery, fracture type, surgical procedures, duration of surgery, infusion quantity, and volume of bleeding during the operation between the 2 groups. Postoperative delirium was associated with these factors.14 To eliminate the influence of postoperative pain on PD, both groups received PCEA after the surgery in our study; no significant differences were found for postoperative pain scores. The only difference is that patients who received FICB for preemptive analgesia experienced less preoperative pain. Therefore, we can conclude that PD may be associated with preoperative pain, and preoperative pain is also a risk factor for the development of PD.
The reasons for the influence of preemptive analgesia with continuous FICB on PD may be related to relief of preoperative pain and the reduction in the “rescue” opioid requirements. Severe pain can cause activation and release of proinflammatory cytokines.16 Excessive release of proinflammatory cytokines can promote the development of delirium.17,18 Pre-emptive analgesia with continuous FICB may reduce the release of proinflammatory cytokines, which prevents the occurrence of PD. In addition, opioids can also stimulate the production of proinflammatory cytokines.19 Preoperative analgesia with lesser amounts of opioid drugs may be an important factor for reduced levels of proinflammatory cytokines and reduced PD in patients managed with early continuous FICB.
Study limitations
First, this study possibly did not identify all the predictive factors of PD in the 2 groups, such as preoperative anxiety and preoperative fasting time. Second, the intensity of postoperative pain was assessed using the WBS in the patients who became delirious. However, the pain severity ratings on the WBS was highly correlated with those on a VAS.20 Third, plasma cytokines were not measured concomitantly in this experiment, so further studies will be necessary to evaluate the systemic inflammatory response.
In conclusion, the results demonstrated that preoperative pain was also a risk factor for the development of PD, and pain management is critical in patients with hip fractures. Preemptive analgesia with continuous FICB is an effective technique to reduce preoperative pain, opioid requirements and PD in geriatric patients with hip fracture.
Acknowledgment
The authors would like to thank the American Journal Experts (www.aje.com) for the English language editing.
Footnotes
References
- 1.Colais P, Di Martino M, Fusco D, Perucci CA, Davoli M. The effect of early surgery after hip fracture on 1-year mortality. BMC Geriatrics. 2015;15:141–143. doi: 10.1186/s12877-015-0140-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sieber FE, Zakriya KJ, Gottschalk A. Sedation depth during spinal anesthesia and the development of postoperative delirium in elderly patients undergoing hip fracture repair. Mayo Clin Proc. 2010;85:18–26. doi: 10.4065/mcp.2009.0469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moskowitz EE, Overbey DM, Jones TS, Jones EL, Arcomano TR, Moore JT. Post-operative delirium is associated with increased 5-year mortality. Am J Surg. 2017;214:1036–1038. doi: 10.1016/j.amjsurg.2017.08.034. [DOI] [PubMed] [Google Scholar]
- 4.Williams H, Paringe V, Shenoy S, Michaels P, Ramesh B. Standard preoperative analgesia with or without fascia iliaca compartment block for femoral neck fractures. J Orthop Surg. 2016;24:31–35. doi: 10.1177/230949901602400109. [DOI] [PubMed] [Google Scholar]
- 5.Moja L, Piatti A, Pecoraro V, Ricci C, Virgili G, Salanti G. Timing matters in hip fracture surgery:patients operated within 48 hours have better outcomes A meta-analysis and meta-regression of over 190,000 patients. PLoS One. 2012;7:46175. doi: 10.1371/journal.pone.0046175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ma Y, Wu J, Xue J, Lan F, Wang T. Ultrasound-guided continuous fascia iliaca compartment block for pre-operative pain control in very elderly patients with hip fracture:A randomized controlled trial. Exp Ther Med. 2018;16:1944–1952. doi: 10.3892/etm.2018.6417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khin Hla T, Hegarty M, Russell P, Drake-Brockman TF, Ramgolam A. Perception of pediatric pain:a comparison of postoperative pain assessments between child, parent, nurse, and independent observer. Paediatr Anaesth. 2014;24:1127–1131. doi: 10.1111/pan.12484. [DOI] [PubMed] [Google Scholar]
- 8.Inouye SK, Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion:the confusion assessment method A new method for detection of delirium. Ann Intern Med. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 9.Godoy Monzón D, Vazquez J, Jauregui JR, Iserson KV. Pain treatment in post-traumatic hip fracture in the elderly:regional block vs systemic non-steroidal analgesics. Int J Emerg Med. 2010;3:321–325. doi: 10.1007/s12245-010-0234-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Petre BM, Roxbury CR, McCallum JR, Defontes KW, Belkoff SM, Mears SC. Pain reporting, opiate dosing, and the adverse effects of opiates after hip or knee replacement in patients 60 years old orolder. Geriatr Orthop Surg Rehabil. 2012;3:3–7. doi: 10.1177/2151458511432758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elkhodair S, Mortazavi J, Chester A, Pereira M. Single fascia iliaca compartment block for pain relief in patients with fractured neck of femur in the emergency department:a pilot study. Eur J Emerg Med. 2011;18:340–343. doi: 10.1097/MEJ.0b013e32834533dd. [DOI] [PubMed] [Google Scholar]
- 12.McRae PJ, Bendall JC, Madigan V, Middleton PM. Paramedic-performed fascia iliaca compartment block for femoral fractures:a controlled trial. J Emerg Med. 2015;48:581–589. doi: 10.1016/j.jemermed.2014.12.016. [DOI] [PubMed] [Google Scholar]
- 13.Hogh A, Dremstrup L, Jensen SS, Lindholt J. Fascia iliaca compartment block performed by junior registrars as a supplement to pre-operative analgesia for patients with hip fracture. Strategies Trauma Limb Reconstr. 2008;3:65–70. doi: 10.1007/s11751-008-0037-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Radinovic K, Markovic Denic L, Milan Z, Cirkovic A, Baralic M, Bumbasirevic V. Impact of intraoperative blood pressure, blood pressure fluctuation, and pulse pressure on postoperative delirium in elderly patients with hip fracture:a prospective cohort study. Injury. 2019:0020–1383. doi: 10.1016/j.injury.2019.06.026. 30389-30394. [DOI] [PubMed] [Google Scholar]
- 15.Yamamoto N, Sakura S, Noda T, Nishiyama A, Dan'ura T, Matsui Y. Comparison of the postoperative analgesic efficacies of intravenous acetaminophen and fascia iliaca compartment block inhipfracture surgery:a randomised controlled trial. Injury. 2019;S0020-1383:30105–30106. doi: 10.1016/j.injury.2019.03.008. [DOI] [PubMed] [Google Scholar]
- 16.Cidral-Filho FJ, Martins DF, Moré AO, Mazzardo-Martins L, Silva MD, Cargnin-Ferreira E. Light-emitting diode therapy induces analgesia and decreases spinal cord and sciatic nerve tumour necrosis factor-a levels after sciatic nerve crush in mice. Eur J Pain. 2013;17:1193–1204. doi: 10.1002/j.1532-2149.2012.00280.x. [DOI] [PubMed] [Google Scholar]
- 17.Plaschke K, Fichtenkamm P, Schramm C, Hauth S, Martin E, Verch M. Early postoperative delirium after cardiac surgery was characterized by increased stress levels and inflammatory reaction. Intensive Care Med. 2010;36:2081–2089. doi: 10.1007/s00134-010-2004-4. [DOI] [PubMed] [Google Scholar]
- 18.Munster BC, Aronica E, Zwinderman AH, Eikelenboom P, Cunningham C, Rooij SE. Neuroinflammation in delirium:a postmortem case–control study. Rejuvenation Res. 2011;14:615–622. doi: 10.1089/rej.2011.1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Winterhalter M, Brandl K, Rahe-Meyer N, Osthaus A, Hecker H, Hagl C. Endocrine stress response and inflammatory activation during CABG surgery A randomized trial comparing remifentanil infusion to intermittent fentanyl. Eur J Anaesthesiol. 2008;25:326–335. doi: 10.1017/S0265021507003043. [DOI] [PubMed] [Google Scholar]
- 20.Sánchez-Rodríguez E, Castarlenas E, Vega R, Roset R, Miro J. On the electronic measurement of pain intensity:Can we use different pain intensity scales interchangeably? J Health Psychol. 2017;22:1658–1667. doi: 10.1177/1359105316633284. [DOI] [PubMed] [Google Scholar]


