Abstract
Bilateral congenital diaphragmatic hernia (CDH) is a rare congenital anomaly with high neonatal mortality. The condition is rarely associated with hepatopulmonary fusion (HPF). We reported the surgical repair of bilateral CDH in a male infant aged 6 weeks. The patient had herniation of the liver on the right side with HPF in association with anomalous drainage of the right pulmonary vein into the hepatic vein and ventricular septal defect. We approached both sides thoracoscopically; however, the right side required a subcostal incision. We separated the liver from the right lower lung lobe laterally using electrocautery, and the defect was closed with a mesh. The medial portion was left intact to avoid injury of the anomalous pulmonary venous drainage. After 2 weeks, the patients had a surgical repair of the cardiac defects, and the postoperative course was complicated by bleeding and prolonged ventilation. No hernia recurrence was observed after 9 months.
Bilateral congenital diaphragmatic hernias (CDH) is a rare anomaly that carries a poor prognosis.1 Intrauterine bilateral herniation of the abdominal contents into the thoracic cavity leads to pulmonary hypoplasia and respiratory failure, which is the main cause of neonatal death.2 In the survivors, the surgical repair of CDH is challenging and associated with high mortality.3
Hepatopulmonary fusion (HPF) is a rare association and was previously reported with right-sided CDH,4 and its association with bilateral CDH is very uncommon. In this case, we reported the surgical repair of a bilateral CHD associated with HPF and anomalous pulmonary venous drainage of the right lung.
Case Report
Patient information
A 5-week-old male infant weighed 3.24 kg was presented to our institution with a suspected diaphragmatic hernia and congenital heart disease. The patient had respiratory distress immediately after birth and required resuscitation and mask ventilation. The appearance, pulse, grimace, activity, and respiration (APGAR) scores at 3 minutes was 6 and at 5 minutes was 7. The patient required mechanical ventilation and surfactant therapy for one week before being transferred to our institution.
Clinical findings
The patient presented in mild respiratory distress and on supplemental oxygen through a face mask. The abdomen was scaphoid, and the patient was hemodynamically stable.
Diagnostic assessment
Chest x-ray (Figure 1), and chest computed tomography scan confirmed the diagnosis of bilateral congenital diaphragmatic hernia with liver herniation on the right side and the spleen, the left adrenal gland and part of the stomach on the left side (Figure 2). Echocardiography showed abnormal drainage of the right pulmonary veins into the hepatic vein (scimitar syndrome), inlet ventricular septal defect, interrupted vena cava, pulmonary hypertension, and patent ductus arteriosus. Angiography confirmed the diagnosis of anomalous pulmonary venous drainage and showed sequestrated right lower lobe with blood supply from the abdominal aorta (Figure 3).
Figure 1.
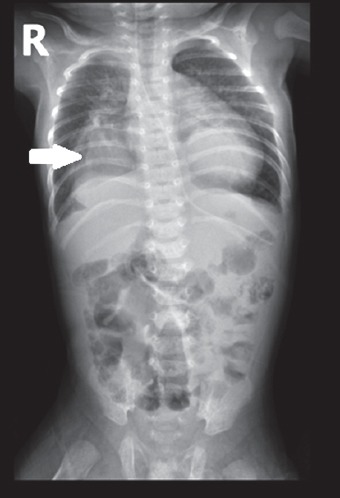
Preoperative chest x-ray showing liver herniation on the right side (arrow) and suspected stomach herniation behind the cardiac shadow on the left side.
Figure 2.
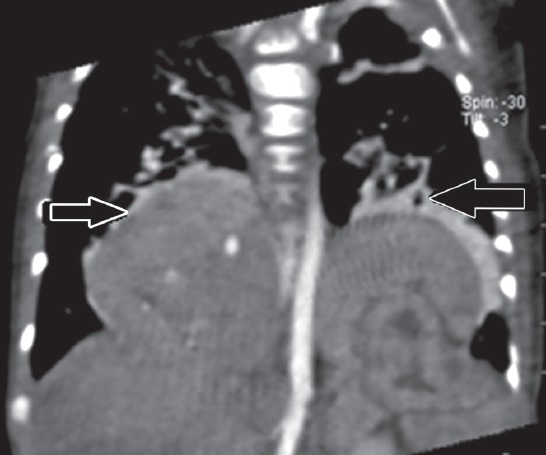
Chest CT scan (coronal view) showing bilateral diaphragmatic hernia (arrows).
Figure 3.
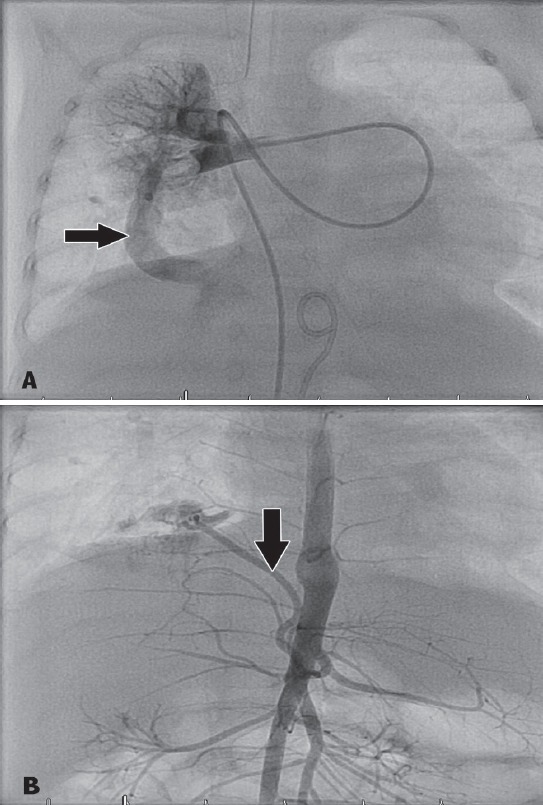
Preoperative angiography showing A) the anomalous pulmonary venous connection of the right lower lobe and B) blood supply of the right lower lobe from the abdominal aorta.
Therapeutic intervention
Pulmonary hypertension was managed by nitrous oxide and sildenafil, and after one week, the patient underwent thoracoscopic surgery to repair the left diaphragmatic hernia. We inserted 3 trocars (one 5-mm camera and 2 3-mm working ports) on the left side. Inspection of the left thoracic cavity revealed herniation of the abdominal content with no hernial sac. Insufflation pressure of 6 mmHg was used to reduce the abdominal contents, and the diaphragmatic defect was repaired with direct 3-0 prolene sutures (Figure 4). A 12 French intercostal drain was placed and secured in position; then the patient was turned to the left lateral position to approach the right diaphragmatic hernia thoracoscopically (Figure 5). Conversion to an open subcostal incision was carried out because of the fusion of the liver with the lower lobe of the right lung. There was no distinct plane between the lung and the liver; therefore, we developed a plane using a LigaSure electrocautery device (Valley Lab, Medtronic, Minneapolis, MN, USA). Because of the abnormal venous drainage, we left the most medial portion of the lung fused to the liver to preserve the anomalous venous drainage. The lateral diaphragmatic defect was then repaired with polytetrafluoroethylene (PTFE) mesh anchored to the surrounding tissue with non-absorbable interrupted sutures. An intercostal drain was placed. Postoperative chest x-ray confirmed the full expansion of the lungs and the reduction of the abdominal contents (Figure 6). The infant was weaned from mechanical ventilation on the 3rd postoperative day, and we removed the chest tubes on the postoperative day 6.
Figure 4.
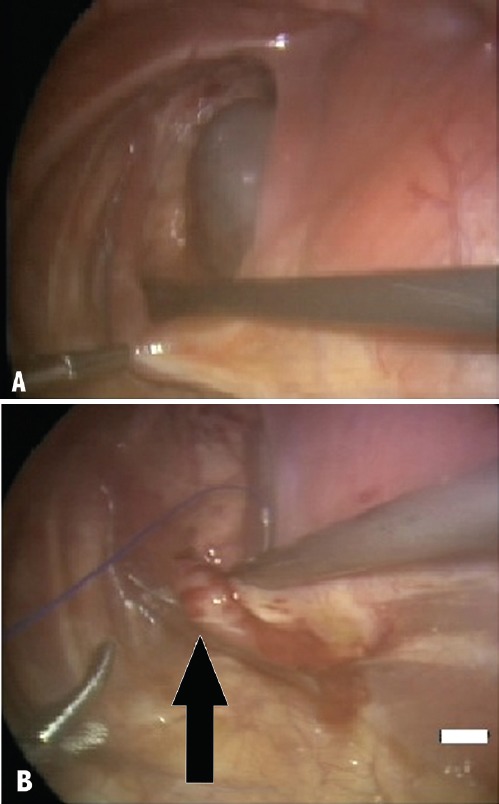
Thoracoscopic view of the A) left thoracic cavity after reduction of the contents and B) the diaphragm is repaired by direct sutures (arrow).
Figure 5.
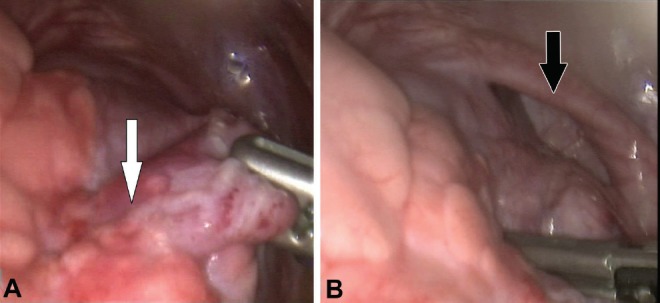
Thoracoscopic view of the right thoracic cavity showing A) the fusion between the right lower lung lobe and the liver (white arrow)and the B) diaphragmatic defect and the hernia sac (black arrow).
Figure 6.
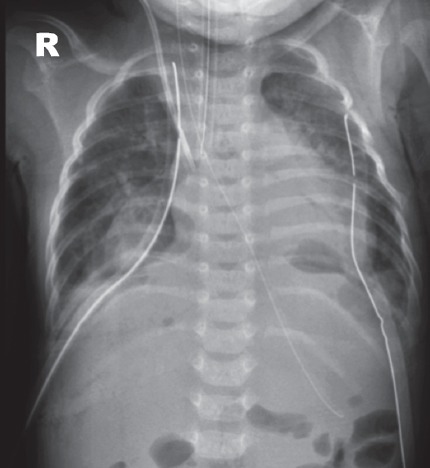
Postoperative chest x-ray showing full lung expansion and reduction of the hernia and bilateral chest tubes.
Follow-up and the outcomes
Repair of the cardiac defects was scheduled 2 weeks later, and the patient had patch closure of the ventricular septal defect, and the anomalous right pulmonary vein was connected to the left atrium. The operation was complicated by bleeding and prolonged mechanical ventilation. After 9 months, the lung was fully expanded and no recurrence of the diaphragmatic hernia (Figure 7).
Figure 7.
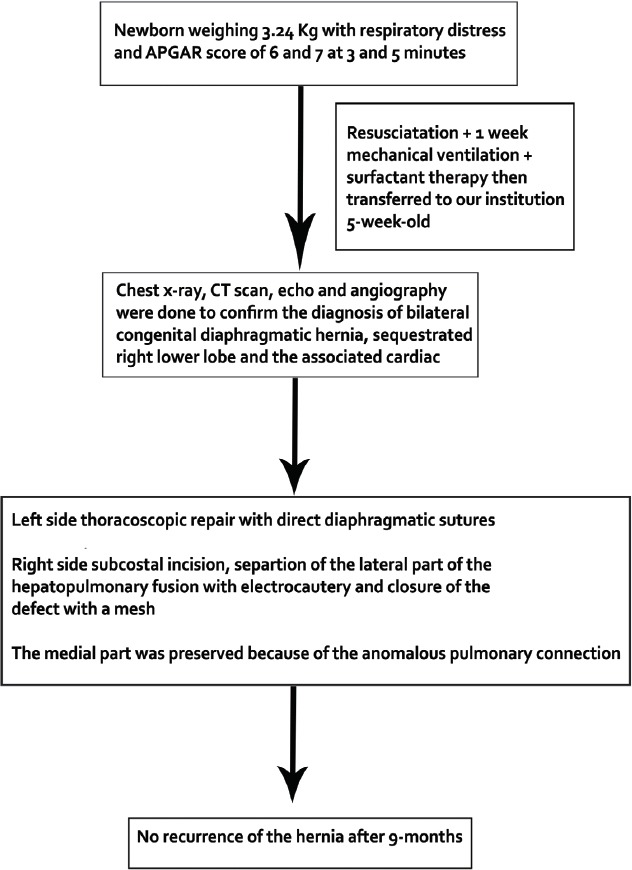
Case flow diagram of a newborn patient with bilateral congenital diaphragmatic hernia.
Discussion
Bilateral CDH is a rare entity which occurs in less than 1-2% of all congenital diaphragmatic hernia cases, and it is associated with worse outcomes and high mortality.3 Congenital diaphragmatic hernia results from partial closure of the pleuroperitoneal canal,5 and the outcome is mainly related to the severity of pulmonary hypoplasia and the associated congenital anomalies; additionally, early surgery was associated with poor outcome.6 Bilateral CDH is commonly associated with genetic defects and other congenital anomalies. Our patient had an associated HPF, sequestrated right lower lobe, ventricular septal defect, patent ductus arteriosus, pulmonary hypertension, and partial anomalous pulmonary venous connection. The most commonly reported cardiac abnormalities associated with bilateral CHD was the ventricular septal defect and occurred in 16% of the patients.3 Hepatopulmonary fusion is an extremely rare association with bilateral CDH. The pathogenesis of this anomaly is not fully understood; however, the failure of the development of the right hemidiaphragm might allow the protrusion of liver tissue into the thorax and the fusion with the right lower lung lobe. Alternatively, HPF could be the initial event that prevents the development of the right hemidiaphragm.7 Olenik et al8 reported that the presence of anomalous venous drainage of the right lung into the hepatic vein is a diagnostic indicator of the presence of HPF.
During the operation, separating the lung from the liver is technically challenging. If a plane is evident, both organs can be separated with the aid of a hemostatic device such as LigaSure. This device helps in coagulating and sealing blood vessels and lung tissues, minimizing bleeding and pulmonary leaks. In some instances, partial pneumonectomy or segmental hepatic resections must be undertaken to enable separation. Extreme caution should be taken on the medial aspect to avoid damage of the abnormal pulmonary venous drainage to the liver. The large remaining defect in the diaphragm was adequately addressed by polytetrafluoroethylene mesh graft.
There were 80 patients reported with bilateral CDH in the International Registry of Congenital Diaphragmatic Hernia in 20 years, mortality was 74%, 38 of them had surgery, and no patient had a concomitant HPF.3 Hepatopulmonary fusion is commonly associated with cardiac lesions and pulmonary hypertension.8
In a review of literature, the combination of right CDH, HPF, and anomalous venous drainage of the right lung was reported in one case,9 and the association of HPF and sequestration was reported in 3 cases.10 However, the association of bilateral CDH, HPF, partial anomalous right pulmonary venous drainage and sequestrated lobe was not reported before.
In summary, the management of infants with bilateral CDH is difficult as it is associated with significant morbidity and mortality. In addition, the presence of HPF can worsen the outcome. Treatment is surgical and consists of a reduction of the herniated liver, release of adhesions, and closure of the diaphragmatic defect. In some cases, partial closure of the defect or using mesh around the fused liver and lung is an option for treatment. However, life-threatening bleeding might occur if complete separation is attempted.
In conclusion, bilateral CDH is rarely associated with HPF and partial anomalous pulmonary venous drainage. Proper preoperative planning and special attention during surgical repair are required to avoid injury to the anomalous pulmonary venous drainage and the abnormal blood supply of the right lung.
Footnotes
References
- 1.Said SM, Moir CR, Ishitani MB, Zarroug AE. Successful thoracoscopic staged repair of bilateral congenital diaphragmatic hernia. J Pediatr Surg. 2010;45:E5–E8. doi: 10.1016/j.jpedsurg.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Reiss I, Schaible T, van den Hout L, Capolupo I, Allegaert K, van Heijst A, et al. Standardized postnatal management of infants with congenital diaphragmatic hernia in Europe:the CDH EURO consortium consensus. Neonatology. 2010;98:354–364. doi: 10.1159/000320622. [DOI] [PubMed] [Google Scholar]
- 3.Botden SM, Heiwegen K, van Rooij IA, Scharbatke H, Lally PA, van Heijst A, et al. Bilateral congenital diaphragmatic hernia:prognostic evaluation of a large international cohort. J Pediatr Surg. 2017;52:1475–1479. doi: 10.1016/j.jpedsurg.2016.10.053. [DOI] [PubMed] [Google Scholar]
- 4.Gander JW, Kadenhe-Chiweshe A, Fisher JC, Lampl BS, Berdon WE, Stolar CJ, et al. Hepatic pulmonary fusion in an infant with a right-sided congenital diaphragmatic hernia and contralateral mediastinal shift. J Pediatr Surg. 2010;45:265–268. doi: 10.1016/j.jpedsurg.2009.10.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ali K, Dassios T, Khaliq SA, Williams EE, Tamura K, Davenport M, et al. Outcomes of infants with congenital diaphragmatic hernia by side of defect in the FETO era. Pediatr Surg Int. 2019;35:743–747. doi: 10.1007/s00383-019-04484-3. [DOI] [PubMed] [Google Scholar]
- 6.Chen D, Hu Y, Wu Y, Li X. Risk factors of death in newborns with congenital diaphragmatic hernia. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2019;48:83–88. doi: 10.3785/j.issn.1008-9292.2019.02.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keller RL, Aaroz PA, Hawgood S, Higgins CB. MR imaging of hepatic pulmonary fusion in neonates. AJR Am J Roentgenol. 2003;180:438–440. doi: 10.2214/ajr.180.2.1800438. [DOI] [PubMed] [Google Scholar]
- 8.Olenik D, Codrich D, Gobbo F, Travan L, Zennaro F, Dell'Oste C, et al. Hepatopulmonary fusion in a newborn. An uncommon intraoperatory finding during right congenital diaphragmatic hernia surgery: case description and review of literature. Hernia. 2014;18:417–421. doi: 10.1007/s10029-012-1042-y. [DOI] [PubMed] [Google Scholar]
- 9.Hamilton J, Jaroszewski D, Notrica D. Fatal complication after repair of a congenital diaphragmatic hernia associated with hepatopulmonary fusion, anomalous right pulmonary venous return, and azygos continuation of the inferior vena cava. Eur J Pediatr Surg. 2014;24:350–352. doi: 10.1055/s-0032-1324695. [DOI] [PubMed] [Google Scholar]
- 10.Almaramhy HH. Hepatopulmonary fusion associated with right-sided congenital diaphragmatic hernia:management of this rare anomaly and a review of the literature. J Int Med Res. 2018;46:5278–5284. doi: 10.1177/0300060518759892. [DOI] [PMC free article] [PubMed] [Google Scholar]


