Abstract
Background:
Solid fuels are widely used in China. Household air pollution from the burning of solid fuels may increase the risk of chronic obstructive pulmonary disease (COPD), but prospective evidence is limited.
Objectives:
We examined the association of solid fuel use for cooking and heating with the risk of COPD in a prospective cohort study.
Methods:
Participants were from the China Kadoorie Biobank. Current and previous fuels used for household cooking and heating were self-reported at baseline in 2004–2008. In the present study, “solid fuels” refers to coal and wood, whereas “cleaner fuels” refers to energy sources that presumably produce lower levels of indoor pollution, including electricity, gas, and central heating. A total of 475,827 adults 30–79 y of age without prevalent COPD were followed through the end of 2015. We used adjusted Cox regression models to estimate hazard ratios for COPD.
Results:
Over 9.1 y of follow-up, 9,835 incident COPD cases were reported. Compared with the use of cleaner fuels for cooking, using coal and wood for cooking was positively associated with COPD, with fully adjusted HRs of 1.06 (95% CI: 0.98, 1.15) and 1.14 (95% CI: 1.06, 1.23), respectively. Adjusted HRs for heating with coal and wood were 1.16 (95% CI: 1.04, 1.29) and 1.21 (95% CI: 1.09, 1.35), respectively. The positive association between cooking with solid fuel and COPD appeared to be limited to women and never- (vs. ever-) smokers. COPD risk increased with a higher number of years of solid fuel use for heating and wood use for cooking.
Conclusions:
The use of solid fuel for cooking and heating was associated with the increased risk of COPD in this prospective cohort study. Studies with more accurate exposure assessment are needed to confirm the association. https://doi.org/10.1289/EHP2856
Introduction
Chronic obstructive pulmonary disease (COPD) is a serious public health problem. The global prevalence of COPD in people of age was estimated to be 11.7% in 2010 (Adeloye et al. 2015). Globally, nearly 3 million people die of COPD each year, and China accounts for about 30% of these deaths (Institute for Health Metrics and Evaluation; http://ghdx.healthdata.org/gbd-results-tool). Although tobacco smoking is the most important risk factor for COPD, approximately 20% of cases occur in nonsmokers (Lamprecht et al. 2011); thus, a better understanding of other risk factors is needed.
Household air pollution (HAP) from the burning of solid fuels (coal, biomass) may contribute to COPD morbidity. Instead of directly measuring pollutant concentrations, fuel type is often used as a proxy for HAP exposure in large epidemiologic studies. Systematic reviews suggest that the prevalence or incidence of COPD is two to three times higher in people who use solid fuels for cooking or heating than in people without these exposures (Hu et al. 2010; Kurmi et al. 2010). Based on existing evidence, solid fuel use is considered a risk factor for COPD. The Global Burden of Disease project included COPD as an outcome for HAP exposure (KR Smith et al. 2014).
However, the epidemiological evidence is inconsistent. Heterogeneity and publication bias may have influenced pooled estimates in systematic reviews (KR Smith et al. 2014). Large studies have also reported null associations (Amaral et al. 2018; Hooper et al. 2012; M Smith et al. 2014; Xu et al. 2007), challenging the role of HAP as an established risk factor for COPD (Gnatiuc and Caramori 2014). Furthermore, previous studies were mainly cross-sectional and case–control studies of the association with COPD prevalence rather than incidence. Longitudinal observations are needed to help support a causal relationship. A cohort study of 280,000 never-smoking adults in the China Kadoorie Biobank (CKB) found that long-term solid fuel use for cooking was associated with hospitalization and death from a range of respiratory diseases, including COPD (Chan et al. 2019). Prospective evidence for the association between solid fuel use for heating and COPD is limited.
Two large cross-sectional studies have examined the association between HAP and COPD among Chinese adults. The Chinese Epidemiological Survey of COPD (CESCOPD), which included adults living in seven provinces, reported that exposure to indoor biomass from cooking or heating was associated with spirometry-confirmed COPD [adjusted odds ratio (OR): 1.35, 95% confidence interval (CI): 1.20, 1.52] (Zhong et al. 2007). However, a cross-sectional analysis of 317,399 never smokers enrolled in the CKB reported adjusted ORs for associations between airflow obstruction and HAP exposures that were close to the null (M Smith et al. 2014). Smaller cross-sectional and case–control studies conducted in China have yielded inconsistent results (Ding et al. 2015; Han et al. 2015; Liu et al. 2007; Xu et al. 2007; Zhou et al. 1995). However, a prospective cohort study of 996 Chinese adults reported that switching cooking fuels and improving ventilation was associated with a reduction in COPD incidence during follow-up (Zhou et al. 2014).
Approximately 2.8 billion people use solid fuels in the world (Bonjour et al. 2013). Social and economic factors are major determinants of household energy sources (Heltberg 2004). Although the Chinese economy is developing rapidly, solid fuels are still widely used for cooking and heating, especially in rural areas, where more than three-fourths of households rely on coal or biomass fuels (Tang and Liao 2014). Given the high prevalence of HAP exposure in China, the COPD disease burden associated with HAP may be considerable. Therefore, we conducted a prospective cohort study of solid fuel use for cooking and heating and the risk of incident COPD in China, using data from the CKB study.
Methods
Study Population
Details of the CKB study have been described previously (Chen et al. 2005, 2011). Adults 30–79 y of age were recruited during 2004–2008 from 10 regions across China, including 5 urban regions (Harbin, Qingdao, Suzhou, Liuzhou, and Haikou) and 5 rural regions (Henan, Gansu, Sichuan, Zhejiang, and Hunan). In each administrative unit (village or street community), all men and women who were permanent residents without a major disability were identified and invited to participate. Multiple people living in the same residence were eligible for enrollment into the CKB. The participation rate was about 30%. A total of 512,891 participants completed the baseline survey. The CKB study was approved by the Ethical Committee of the Chinese Center for Disease Control and Prevention (Beijing, China) and the Oxford Tropical Research Ethics Committee, University of Oxford (UK). Signed informed consent was obtained from all participants.
To limit the present analysis to those at risk of developing COPD during follow-up, we excluded CKB participants who had been diagnosed with chronic bronchitis or emphysema by a physician prior to the baseline survey (), and those who had airflow obstruction [defined as the ratio of forced expiratory volume in 1 s over forced vital capacity () ] at the time of enrollment (). One additional participant was excluded because of an implausible censoring date, leaving 475,827 in the present analysis. Because few people (, ) in Haikou and Zhejiang heat their homes in winter, participants from these regions were excluded from models used to estimate associations with heating fuel, leaving 393,444 participants for these analyses.
Assessment of Exposure and Covariates
Self-reported fuel type was used as a proxy indicator of HAP exposure, consistent with many previous epidemiologic studies (Clark et al. 2013). An interviewer-administered questionnaire was used to collect information in the baseline survey. Participants were asked to provide information about their residence at baseline and to provide information about each residence where they had lived for at least 1 y prior to baseline, up to a maximum of two previous residences. The following data were obtained for each eligible dwelling: duration of residence (in years), how often the participant cooked meals in the dwelling (daily, weekly, monthly, never/rarely, no cooking facility), main cooking fuel (gas, coal, wood, electricity, other), winter heating (yes, no), main heating fuel (central heating, gas, coal, wood, electricity, other). For dwellings with a cooking facility, we further asked if cooking stoves all had a chimney/extractor (all stoves, not all stoves, none). Although participants may have used multiple types of fuel at the same time, only the primary fuel (the fuel that was used most frequently) was recorded. “Central heating” referred to heating systems where heat was generated centrally and carried to individual dwellings by water or steam through pipes. “Gas” mainly included natural gas, coal gas, and liquefied petroleum gas (LPG). For cooking and heating fuel, the “other” category comprised all fuel types not specified above, including animal dung, diesel, kerosene, and solar energy. After the baseline survey, a re-survey involving 19,788 participants (3.9%) randomly selected from all surviving CKB participants was undertaken, with an interval of 0.2–4.2 (mean: 2.6) y from baseline to re-survey. Information about current fuel use was collected in the re-survey, regardless of whether participants were still living in the baseline residence. The kappa coefficients between the baseline and re-survey were 0.61 and 0.71 for cooking and heating fuel, respectively, indicating that the agreement of self-reported fuel use was acceptable.
Solid fuel use was assessed separately for cooking and heating. For the analyses of heating fuels, participants were classified based on their self-reported use at baseline as solid fuel users if coal or wood (as separate exposures, or combined into a single solid fuel exposure group) was used as the primary fuel to heat their residence; as cleaner fuel users if the primary heating fuel was gas, electricity, or central heating; as other fuel users if they used other fuels for heating; or as “non-heating” if their baseline residence was never heated with any type of fuel. For analyses of cooking fuels, participants were classified as users of coal or wood (as separate exposures, or as a single solid fuel exposure) if they indicated that they personally cooked meals in their baseline residence at least once/month and used coal or wood as the primary cooling fuel; as cleaner fuel users if they cooked meals at their baseline residence using gas or electricity; as other fuel users if they cooked with other fuels; or as “non-cooking” if they did not cook meals at least once/month in their baseline residence, regardless of whether someone else cooked meals in the participant’s baseline residence or the type of fuel used by someone else for cooking. Cleaner fuel users were used as the reference exposure group for analyses of both heating and cooking. To investigate the relationship between COPD and the duration of HAP exposure from cooking or heating, respectively, we estimated the cumulative duration of exposure to coal and wood (as separate exposures, or as a single solid fuel exposure) based on the number of years at the baseline residence and up to two previous residences where the participant lived for at least 1 y. For cooking, years of exposure also were limited to years when the participant personally cooked in their residence at least once/month.
Covariate information collected at baseline included region, sociodemographic factors (age, sex, marital status, highest education, occupation, household income), tobacco smoking, passive smoking, physical activity, and medical history (respiratory symptoms, asthma, tuberculosis). The physical activity questionnaire collected information about the type and duration of activities related to work, transportation, housework, and leisure-time exercise during the past year. Metabolic equivalent task-hours per day (MET-h/d) were calculated to quantify the total amount of physical activity. Height and weight were measured at baseline by trained staff using standard instruments and protocols. Body mass index (BMI) was calculated by dividing weight (kg) by the square of height (m). Prebronchodilator and FVC were measured by trained technicians following recommended procedures (American Thoracic Society 1995). Self-reported tobacco smoking was assessed in a quality control survey involving 15,728 participants (3.1%) randomly selected from the entire CKB several weeks (mean interval: 17 d) after the baseline survey (Chen et al. 2011). There was good agreement between the baseline and quality control survey for smoking (kappa: 0.94). The reliability of other covariates was evaluated in the re-survey in July 2008, with kappa or Spearman coefficients ranging from 0.19 for the self-reported respiratory symptom to 0.93 for BMI (see Table S1).
Assessment of Outcome
Participants were followed up until the date of a COPD diagnosis (ICD-10: codes J41–J44), death, loss to follow-up, or 31 December 2015, whichever came first. Incident COPD cases were ascertained via death certificates, hospitalization records, and active follow-up. Vital status and cause of death were ascertained through reviews of official residential records and death certificates submitted to the regional Center for Disease Control and Prevention (CDC). Information on COPD morbidity was obtained through electronic linkage to the national health insurance (HI) system, which was established in all study regions by 2009 and contains detailed hospitalization information, including ICD-10 codes, dates of diagnosis, and procedures. COPD diagnoses made in an outpatient setting were not included. Ninety-eight percent of CKB cohort participants were linked with the HI database during the study period, and active follow-up was conducted annually for participants who were not linked to their local HI database, using a questionnaire to collect self-reported diagnosis of major chronic diseases (including COPD) by a physician in the past year. Fewer than 1% of all CKB participants () were lost to follow-up before the end of the study. To evaluate the validity of COPD diagnosis in the CKB cohort, 3,460 of 11,799 COPD cases identified through 1 January 2014 were randomly selected for medical records review, including cases that were prevalent at baseline (Kurmi et al. 2016). Medical records were successfully retrieved for 1,069 (31%) of the selected cases and independently reviewed by five physicians under the supervision of a specialist in respiratory diseases. A diagnosis of COPD was confirmed in 85% of the reviewed cases. Most of the cases that were not confirmed were classified as pneumonia (67%) or asthma (30%) after medical records review.
Statistical Analysis
All analyses were conducted separately for cooking and heating fuels. We used linear models or logistic models to compare baseline characteristics between solid fuel users, cleaner fuel users, and non-cooking or non-heating people, controlling for age, sex, and region. To identify potential confounders independent of population structure (age, sex, and region), we reported adjusted values of baseline characteristics, which was analogous to direct standardization (Muller and MacLehose 2014). Cox regression models were used to estimate hazard ratios (HRs) and 95% CIs for associations between household solid fuel use and COPD incidence, with time since baseline as the timescale, and joint stratification by region and 5-y baseline age groups. Our models did not account for clustering within homes or families. We found no violation of the proportional hazards assumption based on a criterion for the correlation between Schoenfeld residuals and time for all solid fuel exposures (data not shown).
Covariates were selected based on prior knowledge of COPD risk factors and were assessed at baseline and modeled as time-invariant covariates. Model 1 included age (y; continuous) and sex (male, female). Model 2 also included education (none or primary school, middle or high school, college or university), occupation [agricultural worker, factory worker, other occupations, no occupation (retired, housewife/-husband, and unemployed)], marital status (married, widowed, divorced or separated, never married), household income (, 5,000–9,999, 10,000–19,999, ), smoking status [never or occasional (never smoked regularly but had smoked in lifetime); former, quit ago; former, quit ago; current, ; current, 15–24/d; current, ], passive smoking (never lived with smoker, lived with smoker for , lived with smoker for and exposure , lived with smoker for and exposure ), stoves with chimney/extractor (all stoves, not all stoves, none, had no cooking stoves), physical activity (MET-h/d; continuous), and BMI (continuous). In Model 3, we further adjusted for the presence of respiratory symptoms (including four symptoms: usually become short of breath when walking on level ground, usually slow down due to chest discomfort when walking on level ground, cough frequently during the past 12 months, cough up sputum after getting up in the morning during the past 12 months) and self-reported asthma or tuberculosis at baseline, which may be confounders if they influenced solid fuel use or mediators if they were at least partly a consequence of HAP exposure. We consider Model 3, which estimated the effect of exposure independent of baseline respiratory conditions, to be the primary model for the present analysis, but we also report Model 2 estimates because differences between the models provide some indication of the extent of potential mediation by baseline conditions.
We estimated the association between baseline household fuel type and COPD incidence using the cleaner fuel group as the reference exposure. Mutually adjusted associations with cooking and heating fuel types were estimated using a single regression model. To control for residual confounding by smoking, we performed sensitivity analyses restricted to never smokers (). We also conducted sensitivity analyses excluding participants who developed COPD in the first year of follow-up; fitting random-effect models by region; using the lower-limit of normal (LLN, defined as the lower fifth percentile of ) COPD definition (Quanjer et al. 2012) to exclude participants with airflow obstruction at baseline; including participants from Haikou and Zhejiang when estimating effects of heating fuels; and using proportional subdistribution hazards models to account for competing risks of death.
We also estimated the relationship between exposure duration and COPD using a separate model. Duration of coal use was calculated by summing the number of years in each residence (including the baseline residence and up to two previous residences) where coal was reported as the primary fuel. Duration of wood use was calculated by summing the number of years in each residence where wood was reported as the primary fuel. Duration of solid fuel use was the sum of coal and wood. The exposure duration was counted as 0 y in a residence where the participant cooked less than once/month or did not heat during winter. Exposure duration (coal, wood, and combined as solid fuel) was categorized into five groups: never, 1–20, 21–40, 41–60, . For analyses of coal, wood, and solid fuel, the “never” group was people who had no history of using either wood or coal at baseline. Trends were tested by modeling a continuous variable that was assigned the median years of duration for each participant’s exposure duration category.
We estimated the joint effects of solid fuel use (wood and coal combined, using separate analyses for cooking and heating) and sex, rural or urban region, smoking (ever or never), passive smoking (no or yes), and ventilation (any or none) by modeling product interaction terms, and we tested for multiplicative joint effects based on product term p-values and for additive joint effects based on relative excess risk due to interaction (RERI) (Li and Chambless 2007). In addition, we modeled the joint effects of solid fuel use for cooking and heating. Joint effects models were limited to participants who reported cooking or heating at their baseline residence and to those who used cleaner fuels, wood, or coal. We estimated the association between baseline fuel use and COPD in 10 regions separately by fitting 10 Cox regression models. All analyses were performed using SAS (version 9.4; SAS Institute Inc.). The significance level was set at 0.05.
Results
Among 475,827 participants, 35.8% used solid fuel (wood or coal) to cook at their baseline residence, and (after excluding residents of Haikou and Zhejiang) 44.8% used solid fuel for heating during cold weather (Table 1). A total of 99,973 participants (21.0%) used solid fuel for both cooking and heating at baseline. After adjusting for age, sex, and region, solid fuel users were older, less educated, and more physically active and had a lower household income at baseline than cleaner fuel users and were more likely to live in a rural region, be exposed to passive smoking, live in a residence with poor ventilation, and have respiratory symptoms. The proportion of current regular smokers was comparable between those who cooked using solid versus cleaner fuels (25.4% and 25.5%, respectively) but was slightly higher in those who used solid versus cleaner fuels for heating (27.6% vs. 25.7%). The unadjusted distribution of all model covariates is presented in Table S2. The characteristics of household fuel use varied considerably across the 10 regions, with the use of cleaner fuels among participants who cooked regularly ranging from 2.2% in Henan to 99.4% in Qingdao, and the use of cleaner fuels among those who heated their homes in winter ranging from 1.1% in Gansu to 99.7% in Suzhou (see Table S3).
Table 1.
Baseline characteristics by fuel use for cooking and heating.
| Characteristics | Cooking ()a | Heating ()b | ||||
|---|---|---|---|---|---|---|
| Cleaner fuel | Solid fuel | Non-cooking | Cleaner fuel | Solid fuel | Non-heating | |
| (%) | 182,420 (38.3) | 170,323 (35.8) | 120,440 (25.3) | 98,082 (24.9) | 176,414 (44.8) | 117,135 (29.8) |
| Age (y) | 50.6 | 53.3 | 51.5 | 49.3 | 52.6 | 51.3 |
| Male (%) | 32.3 | 18.2 | 84.9 | 41.2 | 40.9 | 39.6 |
| Rural (%) | 15.2 | 91.5 | 63.3 | 13.9 | 84.1 | 39.3 |
| Married (%) | 90.3 | 90.0 | 93.8 | 91.7 | 90.7 | 89.9 |
| Primary school and lower (%) | 43.3 | 56.3 | 48.0 | 33.9 | 50.7 | 47.9 |
| (%) | 21.5 | 33.9 | 24.6 | 19.7 | 33.4 | 34.1 |
| No occupation (%) | 35.0 | 23.6 | 26.3 | 29.5 | 30.6 | 28.4 |
| Current smoker (%) | 25.5 | 25.4 | 26.6 | 25.7 | 27.6 | 25.7 |
| Passive smoking (%) | 74.7 | 76.6 | 75.2 | 78.8 | 81.4 | 79.6 |
| Good ventilation (%)c | 56.8 | 31.9 | 45.5 | 67.3 | 36.3 | 48.8 |
| BMI () | 23.9 | 23.6 | 23.6 | 23.9 | 23.9 | 23.7 |
| Physical activity (MET-h/d) | 20.8 | 22.3 | 20.7 | 19.9 | 20.8 | 21.9 |
| Respiratory symptoms (%) | 12.5 | 13.8 | 12.5 | 13.5 | 14.1 | 13.9 |
| Asthma (%) | 0.3 | 0.3 | 0.4 | 0.3 | 0.3 | 0.3 |
| Tuberculosis (%) | 1.4 | 1.2 | 1.4 | 1.7 | 1.4 | 1.3 |
Note: No variables had missing values. We used linear (for continuous variables) or logistic models (for categorical variables) to estimate predicted probabilities adjusted for age, sex, and region as appropriate. Participants using other unspecified fuels were very small in number and thus not presented (, 0.56% for cooking; , 0.46% for heating). BMI, body mass index; CI: confidence interval; HR, hazard ratio; MET-h/d, metabolic equivalent task-hours per day.
Participants were classified as cleaner or solid fuel users for cooking if they personally cooked meals at least once/month in the baseline residence. The non-cooking group included people who lived in residences where cooking was performed by someone else (regardless of the type of fuel used) as well as people who lived in residences where no meals were cooked at all.
Participants from Haikou and Zhejiang were excluded from the analysis of heating. The non-heating group included people who did not heat their baseline residence with any type of fuel.
All stoves for cooking had a chimney or extractor.
During a median follow-up of 9.1 y (interquartile range 8.2–10.1 y), we documented 9,835 incident COPD cases. Among these COPD cases, 8,655 (88.0%) were ascertained via health insurance hospitalization database, 1,090 (11.1%) were ascertained via death certificates, and 90 (0.9%) cases were additionally identified through active follow-up. Compared with cases who used cleaner fuels at baseline, cases who used solid fuels at baseline comprised more death events and fewer hospitalization events (see Table S4). Among all COPD cases, 27 cases cooked with “other” fuels at their baseline residence, and (after excluding cases from Haikou and Zhejiang) 43 cases used “other” fuels to heat their baseline residence. The duration of follow-up was similar across exposure groups, with the median follow-up ranging from 9.1 to 9.3 y for cooking and 9.0 to 9.2 y for heating. Participants who used cleaner fuels for cooking or heating at baseline had lower crude COPD incidence rates than those who used coal or wood or those who did not cook at least once/month or heat their homes during winter (Table 2). Compared with those who used cleaner fuels to cook at baseline, fully adjusted HRs (Model 3) were 1.07 (95% CI: 0.99, 1.15) for those who did not cook at least once/month, 1.06 (95% CI: 0.98, 1.15) for those who used coal to cook, and 1.14 (95% CI: 1.06, 1.23) for those who used wood to cook. For heating, HRs were 0.92 (95% CI: 0.85, 1.01), 1.16 (95% CI: 1.04, 1.29), and 1.21 (95% CI: 1.09, 1.35) for non-heating, using coal, and using wood, respectively. Fully adjusted model estimates were consistent with the primary analysis when restricted to never smokers, although associations were slightly stronger for the use of coal or wood for heating [HR 1.28 (95% CI: 1.12, 1.47) and 1.35 (95% CI: 1.17, 1.55), respectively] (see Table S5).
Table 2.
Association of baseline fuel type with COPD risk (HR and 95% CI).
| Solid fuel use | Cleaner fuel | Non-cooking or non-heatinga | Coal | Wood |
|---|---|---|---|---|
| Cooking | ||||
| Median follow-up (y) | 9.1 | 9.1 | 9.3 | 9.2 |
| Cases | 2,099 | 2,947 | 2,236 | 2,526 |
| Person-years | 1,637,725 | 1,067,482 | 875,620 | 665,362 |
| Incidence (per 1,000 person-years) | 1.28 | 2.76 | 2.55 | 3.80 |
| Model 1 | 1.00 | 1.12 (1.04, 1.20) | 1.10 (1.01, 1.19) | 1.26 (1.18, 1.36) |
| Model 2 | 1.00 | 1.07 (0.99, 1.15) | 1.07 (0.99, 1.16) | 1.16 (1.08, 1.25) |
| Model 3 | 1.00 | 1.07 (0.99, 1.15) | 1.06 (0.98, 1.15) | 1.14 (1.06, 1.23) |
| Heating | ||||
| Median follow-up (y) | 9.1 | 9.0 | 9.2 | 9.2 |
| Cases | 1,335 | 2,285 | 1,569 | 2,598 |
| Person-years | 877,957 | 1,048,987 | 989,941 | 589,121 |
| Incidence (per 1,000 person-years) | 1.52 | 2.18 | 1.58 | 4.41 |
| Model 1 | 1.00 | 0.97 (0.89, 1.06) | 1.29 (1.16, 1.43) | 1.39 (1.25, 1.54) |
| Model 2 | 1.00 | 0.92 (0.84, 1.00) | 1.17 (1.06, 1.31) | 1.23 (1.10, 1.37) |
| Model 3 | 1.00 | 0.92 (0.85, 1.01) | 1.16 (1.04, 1.29) | 1.21 (1.09, 1.35) |
Note: All estimates are from Cox models with time of follow-up as the underlying timescale. Model 1 was adjusted for age (y) and sex (male, female); Model 2 adjustments additionally included education (none or primary school, middle or high school, college or university), occupation (agricultural worker, factory worker, other occupations, no occupation), marital status (married, widowed, divorced or separated, never married), household income (, 5,000–9,990, 10,000–19,990, ), smoking (never/occasional; quit ago; quit ago; current, ; current, 15–24/d; current, ), passive smoking (never lived with smoker, lived with smoker for , lived with smoker for and exposure , lived with smoker for and exposure ), stoves with chimney/extractor (all stoves, not all stoves, no stoves, had no stoves), physical activity (MET-h/d), and BMI (); Model 3 adjustments additionally included respiratory symptoms, prevalent asthma, and tuberculosis (presence or absence). Model 2 and Model 3 were mutually adjusted for exposures related to cooking and heating. Results for using other unspecified fuels were not shown. CI, confidence interval; HR, hazard ratio.
Non-cooking group included people who cooked meals less than once/month in the baseline residence. Non-heating group included people who did not heat their baseline residence with any type of fuel.
Results remained largely unchanged after excluding participants who developed COPD in the first year of follow-up (); using LLN definition for airflow obstruction; including participants from Haikou and Zhejiang () in the heating fuel analysis; and when based on competing-risk models (see Table S6). When based on random-effects models by region, associations were slightly stronger for the use of coal and wood for cooking [ (95% CI: 1.02, 1.20) and 1.17 (95% CI: 1.09, 1.26), respectively] but very similar to the primary model for use of solid fuels for heating.
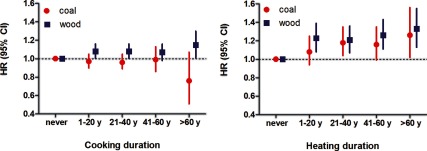
COPD risk increased with the number of years of solid fuel use for heating prior to baseline (Table 3). Compared with no solid fuel use for heating, use for more than 60 y was associated with a 34% higher relative risk (HR: 1.34; 95% CI: 1.18, 1.53). Associations with the use of solid fuels for cooking were null for all categories of duration when based on the fully adjusted model (Model 3, ), although there was some evidence of an increase in COPD with longer duration when adjusted for age and sex only (Model 1, ). We also examined the duration–risk associations by solid fuel type (coal and wood). The reference group included people who had no history of using either wood or coal as primary fuel at baseline. Positive trends were observed for duration of cooking with wood (), heating with coal (), and heating with wood () (Figure 1; see also Table S7).
Table 3.
Duration of solid fuel use and COPD risk (HR and 95% CI).
| Solid fuel use | Duration of solid fuel use (y)a | b | ||||
|---|---|---|---|---|---|---|
| Neverc | 1–20 | 21–40 | 41–60 | |||
| Cooking | ||||||
| Median duration (y) | 0 | 13 | 29 | 47 | 66 | |
| Cases | 3,434 | 1,826 | 2,400 | 1,727 | 448 | |
| Person-years | 1,717,800 | 1,099,524 | 1,033,831 | 372,035 | 46,598 | |
| Incidence (per 1,000 person-years) | 2.00 | 1.66 | 2.32 | 4.64 | 9.61 | |
| Model 1 | 1.00 | 1.01 (0.95, 1.08) | 1.07 (1.00, 1.14) | 1.10 (1.02, 1.18) | 1.10 (0.99, 1.23) | 0.004 |
| Model 2 | 1.00 | 1.00 (0.94, 1.06) | 1.04 (0.98, 1.12) | 1.06 (0.98, 1.14) | 1.04 (0.93, 1.16) | 0.130 |
| Model 3 | 1.00 | 0.99 (0.93, 1.05) | 1.02 (0.95, 1.08) | 1.02 (0.95, 1.10) | 0.98 (0.87, 1.09) | 0.841 |
| Heating | ||||||
| Median duration (y) | 0 | 12 | 34 | 49 | 66 | |
| Cases | 2,720 | 589 | 1,272 | 1,976 | 1,273 | |
| Person-years | 1,285,149 | 422,752 | 867,461 | 803,733 | 145,222 | |
| Incidence (per 1,000 person-years) | 2.12 | 1.39 | 1.47 | 2.46 | 8.77 | |
| Model 1 | 1.00 | 1.17 (1.06, 1.30) | 1.29 (1.17, 1.42) | 1.31 (1.18, 1.44) | 1.42 (1.26, 1.59) | |
| Model 2 | 1.00 | 1.15 (1.03, 1.28) | 1.24 (1.12, 1.36) | 1.26 (1.13, 1.40) | 1.39 (1.13, 1.40) | |
| Model 3 | 1.00 | 1.11 (0.99, 1.23) | 1.19 (1.08, 1.31) | 1.22 (1.09, 1.35) | 1.34 (1.18, 1.53) | |
Note: All estimates are from Cox models with time of follow-up as the underlying timescale. Model 1 was adjusted for age and sex; Model 2 adjustments additionally included education, occupation, marital status, household income, smoking, passive smoking, stoves with chimney/extractor, physical activity, and BMI; Model 3 adjustments additionally included respiratory symptoms, prevalent asthma, and tuberculosis. Model 2 and Model 3 were mutually adjusted for exposures related to cooking and heating. All models were further adjusted for total recall period (y). CI, confidence interval; HR, hazard ratio.
Duration was estimated by summing the number of years in each residence where solid fuel (coal, wood) was reported as the primary fuel.
Trends were tested by including median years of each group as a continuous variable in Cox models.
The never group for cooking included people who had no history of using either wood or coal for cooking at baseline and people who cooked less than once/month. The never group for heating included people who had no history of using either wood or coal for heating and people who did not heat during the winter.
Figure 1.
Associations [HRs (95% CIs)] of duration of solid fuel use with COPD risk by fuel type. Duration of fuel use was estimated by summing the number of years in each residence where this type of fuel was reported as the primary fuel. People in the “never” group for cooking had no history of using either wood or coal for cooking at baseline (). People in the “never” group for heating had no history of using either wood or coal for heating at baseline (). The 0.314 for cooking with coal, 0.048 for cooking with wood, 0.011 for heating with coal, and for heating with wood. (See Table S6 for numeric data.) All estimates are from Cox models with time of follow-up as the underlying timescale. Models were adjusted for age, sex, education, occupation, marital status, household income, smoking, passive smoking, stoves with chimney/extractor, physical activity, BMI, and total recall period. Models were mutually adjusted for duration of coal use and wood use. Participants from Haikou and Zhejiang were excluded from the analysis of heating.
In joint analyses, the fully adjusted HR for ever smoking combined with solid fuel use for cooking at baseline [vs. never smoking and cleaner fuel use for cooking at baseline; (95% CI: 1.47, 1.83)] was less than expected for additive or multiplicative risks based on HRs for ever- versus never-smoking among cleaner fuel users (1.75; 95% CI: 1.57, 1.94) and for solid versus cleaner fuel use for cooking among never smokers (1.17; 95% CI: 1.06, 1.28) (p = 0.002 and for additive and multiplicative risks, respectively) (Table 4). In contrast, the fully adjusted HR for ever-smoking combined with any solid fuel use for heating at baseline [vs. never-smoking and cleaner fuel use for heating; (95% CI: 1.69, 2.24)] was consistent with both additive and multiplicative risks based on HRs for ever- versus never-smoking among cleaner fuel users (1.64; 95% CI: 1.45, 1.86) and for solid versus cleaner fuel use among never smokers (1.25; 95% CI: 1.10, 1.42) (p = 0.6 and 0.4, respectively). Similarly, the joint HR for COPD among men who used solid fuels for cooking at baseline [compared with women who used cleaner fuels for cooking; (95% CI: 0.92, 1.17)] was less than expected based on the HR for COPD in men versus women among those who cooked with cleaner fuels (; 95% CI: 0.95, 1.19) and the HR for solid versus cleaner fuel use for cooking among women (; 95% CI: 1.03, 1.24) (p = 0.01 for both additive and multiplicative risks). The joint HR for COPD among men who used solid fuels for heating at baseline [compared with women who used cleaner fuels for heating; (95% CI: 1.02, 1.35)] was consistent with additive and multiplicative risks based on the HR for COPD in male versus female cleaner fuel users (; 95% CI: 0.84, 1.08) and the HR for solid versus cleaner fuel use among women (; 95% CI: 1.05, 1.34) (p = 0.6 for both additive and multiplicative risks). The adjusted HR for COPD among rural residents who used solid fuels for cooking (; 95% CI: 3.19, 4.36) was larger than expected for additive risk (p = 0.02) and consistent with multiplicative risk (p = 0.3) based on the HR for solid versus cleaner fuel use among urban residents (; 95% CI: 1.01, 1.37) and the HR for rural versus urban among cleaner fuel users (; 95% CI: 2.92, 4.13). The joint effect estimate for solid versus cleaner fuel use for heating in combination with rural versus urban was consistent with both additive and multiplicative risks (both p = 0.8). Joint effect estimates for solid versus cleaner fuel use (for heating and for cooking) in combination with any versus no ventilation or any versus no exposure to passive smoking were not significantly different from expectations for additive or multiplicative risks. Compared with the risk of COPD among those who used cleaner fuels for both cooking and heating their homes, the HR for those who used solid fuels for both cooking and heating was 1.22 (95% CI: 1.02, 1.48). The HR for the use of solid versus cleaner fuels for heating among those who used cleaner fuels for cooking was similar (; 95% CI: 1.07, 1.54), but there was no association between COPD and use of solid versus cleaner fuels for cooking among those who used cleaner fuels for heating (; 95% CI: 0.81, 1.21) (p = 0.7 for both additive and multiplicative risks) (see Table S8). Region-specific HRs comparing participants who were not regular cooks to those who cooked with cleaner fuels were generally close to the null, without obvious differences by rural or urban status, whereas HRs for cooking with solid fuels versus cleaner fuels were more variable but also very imprecise due to small numbers of cases for many regions. HRs for heating with solid fuels versus cleaner fuels or non-heating versus heating with cleaner fuels were highly variable across the 10 regions, but also very imprecise due to substantial differences in the distributions of exposures and COPD cases by region (see Figure S1).
Table 4.
Joint effect of solid fuel use and sex, region, smoking, passive smoking and ventilation [HR (95% CI) and cases/person-years].
| Subgroups | Cooking | Heating | ||||
|---|---|---|---|---|---|---|
| Cleaner fuel | Solid fuel | a | Cleaner fuel | Solid fuel | a | |
| Sex | 0.010/0.011 | 0.622/0.565 | ||||
| Female | 1.00 | 1.13 (1.03, 1.24) | 1.00 | 1.19 (1.05, 1.34) | ||
| 1,345/1,139,284 | 3,423/1,252,472 | 709/524,317 | 1,958/940,861 | |||
| Male | 1.07 (0.95, 1.19) | 1.04 (0.92, 1.17) | 0.95 (0.84, 1.08) | 1.17 (1.02, 1.35) | ||
| 754/498,441 | 1,339/288,510 | 626/353/640 | 2,209/638,201 | |||
| RERI (95% CI) | (, ) | 0.03 (, 0.17) | ||||
| Region | 0.017/0.284 | 0.804/0.774 | ||||
| Urban | 1.00 | 1.18 (1.01, 1.37) | 1.00 | 1.41 (1.20, 1.66) | ||
| 1,460/1,387,359 | 274/131,991 | 811/756,549 | 399/247,511 | |||
| Rural | 3.47 (2.92, 4.13) | 3.73 (3.19, 4.36) | 4.21 (3.33, 5.36) | 4.60 (3.71, 5.73) | ||
| 639/250,366 | 4,488/1,408,991 | 524/121,407 | 3,768/1,331,552 | |||
| RERI (95% CI) | 0.08 (0.01, 0.15) | (, 0.10) | ||||
| Smoking status | 0.002/ | 0.568/0.428 | ||||
| Never | 1.00 | 1.17 (1.06, 1.28) | 1.00 | 1.25 (1.10, 1.42) | ||
| 1,256/1,175,286 | 3,027/1,230,583 | 611/545,957 | 2,033/1,001,260 | |||
| Ever | 1.75 (1.57, 1.94) | 1.64 (1.47, 1.83) | 1.64 (1.45, 1.86) | 1.94 (1.69, 2.24) | ||
| 843/462,438 | 1,735/310,399 | 724/332,000 | 2,134/577,803 | |||
| RERI (95% CI) | (, ) | 0.05 (, 0.25) | ||||
| Passive smoking | 0.363/0.417 | 0.555/0.699 | ||||
| No | 1.00 | 1.04 (0.92, 1.17) | 1.00 | 1.18 (1.01, 1.39) | ||
| 581/407,518 | 897/272,432 | 275/193,847 | 894/341,752 | |||
| Yes | 1.04 (0.94, 1.14) | 1.13 (1.01, 1.26) | 1.05 (0.92, 1.21) | 1.28 (1.10, 1.49) | ||
| 1,518/1,230,206 | 3,865/1,268,550 | 1,060/684,110 | 3,273/1,237,310 | |||
| RERI (95% CI) | 0.05 (, 0.24) | 0.05 (, 0.21) | ||||
| Ventilationb | 0.402/0.337 | 0.188/0.226 | ||||
| Yes | 1.00 | 1.13 (1.00, 1.29) | 1.00 | 1.14 (1.00, 1.30) | ||
| 1,298/1,219,788 | 617/268,621 | 813/689,787 | 1,021/501,430 | |||
| Not all | 1.17 (1.06, 1.30) | 1.24 (1.12, 1.38) | 0.98 (0.86, 1.12) | 1.23 (1.08, 1.39) | ||
| 801/417,937 | 4,145/1,272,361 | 522/188,169 | 3,146/1,077,632 | |||
| RERI (95% CI) | (, 0.11) | 0.12 (, 0.29) | ||||
Note: Participants who did not cook or heat and those reported using other unspecified fuels were excluded from the analysis. All estimates are from Cox models with time of follow-up as the underlying timescale. Models were adjusted for age, sex, education, occupation, marital status, household income, smoking, passive smoking, stoves with chimney/extractor, physical activity, BMI, respiratory symptoms, prevalent asthma, and tuberculosis, as appropriate. Models were mutually adjusted for exposures related to cooking and heating. BMI, body mass index; CI, confidence interval; HR, hazard ratio; RERI, relative excess risk due to interaction.
Interaction on the additive scale/multiplicative scale were presented. We included a product term of fuel use and subgroup variable in a model. We tested for multiplicative interaction based on product term p-values, and for additive joint effects based on RERI.
If all stoves for cooking had chimney or extractor.
Discussion
In this large prospective cohort study in China, we found that the use of solid fuels for cooking and heating was associated with an increased risk of COPD. Compared with those who cooked with cleaner fuels (gas, electricity), the estimated relative risk of COPD among those who cooked with wood was 14% higher (95% CI: 1.06, 1.23), and 6% higher for cooking with coal (95% CI: 0.98, 1.15). Estimated risks for COPD in association with heating with solid fuels versus cleaner fuels (gas, electricity, or central heating) were 21% higher for wood (95% CI: 1.09, 1.35) and 16% higher for coal (95% CI: 1.04, 1.29). We observed a positive trend between COPD and the duration of exposure to heating with solid fuels prior to baseline. Although the CKB cohort was not a random sample of the Chinese population, the study areas were selected to represent major regional differences in disease patterns, lifestyle, and economic levels. Therefore, our findings may be generalizable to diverse populations within China.
Burning solid fuels for cooking and heating produces HAP, including particulate matter, carbon monoxide, nitrous oxides, sulfur oxides, and organic matter (Zhang and Smith 2007). Inhalation of these pollutants may increase lung inflammation and oxidative stress, resulting in COPD (Silva et al. 2015). HAP has been recognized as a risk factor of COPD based on observational studies. Several systematic reviews and meta-analyses have reported significant overall associations between indicators of HAP exposure (e.g., any solid fuel use for cooking, any solid fuel use for cooking or heating) and airway obstruction or COPD (Hu et al. 2010; Kurmi et al. 2010; Po et al. 2011; KR Smith et al. 2014). However, all reported significant heterogeneity among individual studies that may have reflected differences in study designs, populations, confounder adjustment, and other characteristics. For example, Hu et al. (2010) suggested that smaller proportions of stage I COPD patients in case–control versus cross-sectional studies may have contributed to differences between summary estimates when stratified by study design (Hu et al. 2010). A recent pooled analysis of data from adult participants ( of age) in five studies conducted at 13 locations in Latin America, Southeast Asia, and sub-Saharan Africa estimated an overall adjusted OR of 1.41 (95% CI: 1.18, 1.68) for prevalent COPD (based on post-bronchodilator spirometry) in association with any HAP exposure (Siddharthan et al. 2018). In contrast, authors of a pooled analysis of data from study participants ( of age) from 23 low-/middle-, and high-income countries concluded that there was no association between burning solid fuels in an open fire for cooking or heating and the prevalence of air flow obstruction (also based on post-bronchodilator spirometry, but using a different criterion) (Amaral et al. 2018). A cross-sectional analysis of baseline survey data from adult never smokers in the CKB reported that airflow obstruction (based on pre-bronchodilator spirometry) was associated with the use of coal for cooking, but not with other sources of HAP (M Smith et al. 2014). For the present study, we excluded CKB participants with airflow obstruction at baseline, and found that solid fuel use was associated with the incidence of COPD during follow-up. Chan et al. (2019) conducted a prospective analysis using the CKB data and reported that solid fuel use for cooking was associated with increased risk of COPD in never smokers (adjusted HR: 1.10, 95% CI: 1.03, 1.18). Their study included respiratory outcomes other than COPD (i.e., chronic lower respiratory disease, acute respiratory infection, and other upper respiratory diseases), and it was restricted to never smokers and only evaluated solid fuel use for cooking. Based on the same cohort, the present study focused on COPD and further included smokers. We also investigated heating fuel use as an exposure, which was an important source of HAP.
Differences in patterns of HAP exposure from cooking and heating may contribute to differences in associations with respiratory diseases. Cooking produces HAP several times per day, but each episode lasts for a short period, whereas HAP from heating is a seasonal exposure that only occurs during cold weather, but usually persists throughout the day during the heating season. In our study, the association between COPD and the use of solid versus cleaner fuels for heating appeared to be stronger than the association with the use of solid fuels for cooking. A possible explanation is that HAP from heating has longer lifetime exposure duration, and therefore results in higher cumulative doses of inhaled pollutants. Previous association studies and risk assessments of HAP mainly focused on cooking. Our results suggest that pollution from household heating also contributes to COPD development.
Coal and wood are the dominant solid fuels used in Chinese households. In our study, cooking with wood versus cleaner fuels at baseline was associated with an increased risk of COPD during follow-up, whereas cooking with coal was positively, but not significantly associated with COPD. A cross-sectional study of nonsmoking adults from seven provinces in China reported that cooking with biomass, but not coal, was a significant predictor of COPD (defined based on post-bronchodilator spirometry), whereas for heating, use of coal, but not biomass, was a significant predictor (Zhou et al. 2009). Chinese biomass (firewood, crop residue) contains higher volatile matter content, higher moisture content, and lower ash content than coal. Higher emissions of particulate matter were measured for biomass combustion than coal combustion (Li et al. 2017). Previous estimates suggested that biomass users had significantly higher particulate matter exposures than coal users in China (Mestl et al. 2007), which may partly explain differences in associations. In addition, fuel type is related to cookstove type, which also affects ventilation and indoor pollutant concentrations (Peabody et al. 2005; Shen et al. 2015). The complex interaction between fuel type and stove ventilation needs further elucidation in the future. However, our effect estimates for cooking with coal and COPD should be interpreted with caution given that there was a positive association when compared with cooking using cleaner fuels (fully adjusted ; 95% CI: 0.98, 1.15), and we could not account for variation in exposure among coal users due to differences in stove types, ventilation equipment, and cooking duration.
The cleaner fuel group includes diverse energy sources. Electricity and central heating do not produce indoor combustion pollutants. Gas (natural gas, coal gas, and LPG) is relatively clean because pollutant emissions are low compared with solid fuels (Huang et al. 2017; Li et al. 2016). We combined these sources of energy in a single reference group, and we classified non-cooking and non-heating participants into separate exposure groups for our analysis. We observed that compared with cleaner fuel users, non-cooking participants had a slightly higher risk of COPD (fully adjusted ; 95% CI: 0.99, 1.15), whereas non-heating participants had a slightly lower risk (; 95% CI: 0.85, 1.01). One possible explanation is residual confounding related to sex. In addition, some of the non-cooks might live in a dwelling where solid fuels were used for cooking by others, and thus had higher exposures than participants who cooked with cleaner fuels. In contrast, people who lived in a home that was not heated with any fuels may have had lower HAP exposures than those living in homes heated with cleaner fuels. Less than 1% of participants reported using other unspecified fuels, including kerosene, diesel, and solar energy. We did not estimate associations for these uncommon and heterogeneous exposures.
A positive exposure–response relationship would support a causal association between COPD and solid fuel use for cooking or heating. In the present study, we observed a monotonic increase in the estimated risk of COPD as the duration of solid fuel use for heating increased, with a similar pattern when duration was evaluated separately for exposure to wood or coal for heating. Previous evidence showed that long-term exposure to HAP had an adverse effect on lung function (Pérez-Padilla et al. 1996; Balcan et al. 2016). We estimated long-term exposure at baseline using the duration of exposure in up to three residences only, which limited our ability to determine exposure duration accurately. However, we adjusted for the total number of recall years (the number of years in the included residences) to reduce potential bias due to exposure misclassification.
It remains unclear whether the effect of HAP on COPD differed between men and women. Hu et al. (2010) reported a stronger summary estimate for the association between biomass smoke (from cooking or heating) and COPD in men (; 95% CI: 1.85, 10.01) than in women (; 95% CI: 2.28, 3.28), although the estimate for men was imprecise and was based on only 3 studies, compared with 11 studies for women (Hu et al. 2010). KR Smith et al. (2014) reported similar summary ORs for COPD and solid fuel use for cooking in men and women when all studies were included (; 95% CI: 1.15, 3.13 and ; 95% CI: 1.73, 3.06, respectively), but noted that the OR for men (but not women) was attenuated when based only on studies that adjusted for age and smoking (, 95% CI: 0.76, 2.06). In our study, the association between COPD and solid fuel use for cooking appeared to be limited to women. In China, women spend more time at home than men and would, therefore, have more exposure to HAP from both cooking and heating. In addition, women who cook with solid fuels may have more frequent or intense exposures during cooking than men who cook with solid fuels, particularly if men who were classified as cooks (defined as at home) did not cook as often as women. However, other factors might also contribute to differences, including sex-specific susceptibility or confounding.
To the best of our knowledge, this is the first nationwide prospective study to investigate associations between incident COPD and household solid fuel use for cooking or heating in China. The prospective cohort design and large sample size are notable strengths of our study. We excluded participants with prevalent chronic bronchitis, emphysema, and airflow obstruction at baseline, thus avoiding prevalence–incidence bias, which may occur in cross-sectional and case–control studies. We also adjusted for major individual risk factors for COPD, including socioeconomic factors and smoking at baseline. In addition to fuel use at the baseline residence, we also collected information about the history of household fuel use in up to two previous residences, allowing us to estimate cumulative HAP exposure.
Limitations also exist in the present study. First, fuel use for cooking and heating was self-reported, which may lead to exposure misclassification. The reliability of self-reported fuel type was evaluated in a random sample of the CKB population, and the kappa coefficients between baseline and re-survey were acceptable for cooking (0.61) and heating fuels (0.71). However, we did not evaluate the accuracy of self-reported exposures, for example, by comparing self-reported exposures to measured exposures or independent observations of exposures. Primary fuel type is a crude proxy for HAP exposure that does not account for mixed use of various fuels, changes in the types of fuel used, and variation in stove types and ventilation. The primary exposure was solid fuel use at baseline, and those classified as unexposed to solid fuels may have been exposed prior to baseline, and the duration of exposure among those classified as exposed would have varied depending on the amount of time at the baseline residence. Second, the 9-y follow-up was relatively short, and the number of incident COPD cases was limited. Third, we did not account for ambient air pollution, which has been shown to be a risk factor for COPD (Liu et al. 2017) and may confound associations with HAP or mediate associations in locations where ambient air quality is affected by household fuel use. We cannot rule out the potential for residual confounding by unmeasured or unknown confounders or residual confounding because of the misclassification of covariates included in adjusted models. Fourth, the analysis did not account for household clustering despite multiple participants living in the same residence being eligible for enrollment into the CKB. Another limitation is outcome misclassification because COPD is underdiagnosed in China (Zhong et al. 2007), and we may have missed some incident COPD cases because spirometry was not routinely performed during follow-up. In addition, Kurmi et al. (2016) found that in a random sample from the CKB, 15% of COPD cases were incorrectly classified (i.e., false positive) (Kurmi et al. 2016). If the specificity and sensitivity of COPD classification were both nondifferential with regard to household fuel exposures, we would expect bias toward the null. However, we cannot rule out the possibility of differential misclassification given that household use of solid fuels is associated with socioeconomic characteristics that also might be associated with differences in medical care. In addition to disease status, survival time in the proportional hazard model might also be misclassified. In our analysis, incident date was defined as the date of first hospitalization or death of COPD. About 11% of incident cases were deaths of COPD, and a higher proportion of deaths was observed among solid fuel users than cleaner fuel users. Such a difference might attenuate relative risk estimates because the survival time free of COPD was overestimated to a greater extent in solid fuel users than in cleaner fuel users.
Conclusions
In summary, household solid fuel use was associated with an increased risk of incident COPD in our prospective cohort study of Chinese adults. The strength of the association with solid fuel use for heating increased with the duration of exposure prior to baseline. Coal and wood continue to be commonly used fuels for cooking and heating in rural areas within China; therefore, our findings suggest that modernization of household fuel use may help reduce the burden of COPD.
Supplementary Material
Acknowledgments
The most important acknowledgment is to the participants in the study and the members of the survey teams in each of the 10 regional centers, as well as to the project development and management teams based at Beijing, Oxford, and the 10 regional centers.
Footnotes
Supplemental Material is available online (https://doi.org/10.1289/EHP2856).
This work was supported by the National Key Research and Development Program of China (grants 2016YFC1303904, 2016YFC0900500, 2016YFC0900501, and 2016YFC0900504) and the National Natural Science Foundation of China (grants 81390540, 81390544, 81390541). The China Kadoorie Biobank (CKB) baseline survey and the first re-survey were supported by a grant from the Kadoorie Charitable Foundation in Hong Kong. The long-term follow-up is supported by the UK Wellcome Trust (grants 202922/Z/16/Z, 088158/Z/09/Z, and 104085/Z/14/Z) and the Chinese Ministry of Science and Technology (grant 2011BAI09B01). The funders had no role in the study design, data collection, data analysis, and interpretation, writing of the report, or the decision to submit the article for publication.
The authors declare they have no actual or potential competing financial interests.
Note to readers with disabilities: EHP strives to ensure that all journal content is accessible to all readers. However, some figures and Supplemental Material published in EHP articles may not conform to 508 standards due to the complexity of the information being presented. If you need assistance accessing journal content, please contact ehponline@niehs.nih.gov. Our staff will work with you to assess and meet your accessibility needs within 3 working days.
References
- Adeloye D, Chua S, Lee C, Basquill C, Papana A, Theodoratou E, et al. . 2015. Global and regional estimates of COPD prevalence: systematic review and meta-analysis. J Glob Health 5(2):020415, PMID: 26755942, 10.7189/jogh.05-020415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amaral AFS, Patel J, Kato BS, Obaseki DO, Lawin H, Tan WC, et al. . 2018. Airflow obstruction and use of solid fuels for cooking or heating: BOLD results. Am J Respir Crit Care Med 197(5):595–610, PMID: 28895752, 10.1164/rccm.201701-0205OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Thoracic Society. 1995. Standardization of spirometry, 1994 update. Am J Respir Crit Care Med 152:1107–1136, PMID: 7663792, 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- Balcan B, Akan S, Ugurlu AO, Handemir BO, Ceyhan BB, Ozkaya S. 2016. Effects of biomass smoke on pulmonary functions: a case control study. Int J Chron Obstruct Pulmon Dis 11:1615–1622, PMID: 27486318, 10.2147/COPD.S109056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonjour S, Adair-Rohani H, Wolf J, Bruce NG, Mehta S, Prüss-Ustün A, et al. . 2013. Solid fuel use for household cooking: country and regional estimates for 1980–2010. Environ Health Perspect 121(7):784–790, PMID: 23674502, 10.1289/ehp.1205987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan KH, Kurmi OP, Bennett DA, Yang L, Chen Y, Tan Y, et al. . 2019. Solid fuel use and risks of respiratory diseases. A cohort study of 280,000 Chinese never-smokers. Am J Respir Crit Care Med 199(3):352–361, PMID: 30235936, 10.1164/rccm.201803-0432OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z, Chen J, Collins R, Guo Y, Peto R, Wu F, et al. . 2011. China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int J Epidemiol 40(6):1652–1666, PMID: 22158673, 10.1093/ije/dyr120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z, Lee L, Chen J, Collins R, Wu F, Guo Y, et al. . 2005. Cohort profile: the Kadoorie Study of Chronic Disease in China (KSCDC). Int J Epidemiol 34(6):1243–1249, PMID: 16131516, 10.1093/ije/dyi174. [DOI] [PubMed] [Google Scholar]
- Clark ML, Peel JL, Balakrishnan K, Breysse PN, Chillrud SN, Naeher LP, et al. . 2013. Health and household air pollution from solid fuel use: the need for improved exposure assessment. Environ Health Perspect 121(10):1120–1128, PMID: 23872398, 10.1289/ehp.1206429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Y, Xu J, Yao J, Chen Y, He P, Ouyang Y, et al. . 2015. The analyses of risk factors for COPD in the Li ethnic group in Hainan, People’s Republic of China. Int J Chron Obstruct Pulmon Dis 10:2593–2600, PMID: 26664107, 10.2147/COPD.S86402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gnatiuc L, Caramori G. 2014. COPD in nonsmokers: the biomass hypothesis—to be or not to be? Eur Respir J 44(1):8–10, PMID: 24982047, 10.1183/09031936.00029114. [DOI] [PubMed] [Google Scholar]
- Han R, Zou J, Shen X, Wu C, Guo Y, Feng Z, et al. . 2015. The risk factors of chronic obstructive pulmonary disease in Heilongjiang province [in Chinese]. Zhonghua Jie He He Hu Xi Za Zhi 38(2):93–98, PMID: 25908417, 10.3760/cma.j.issn.1001-0939.2015.02.007. [DOI] [PubMed] [Google Scholar]
- Heltberg R. 2004. Fuel switching: evidence from eight developing countries. Energy Econ 26(5):869–887, 10.1016/j.eneco.2004.04.018. [DOI] [Google Scholar]
- Hooper R, Burney P, Vollmer WM, McBurnie MA, Gislason T, Tan WC, et al. . 2012. Risk factors for COPD spirometrically defined from the lower limit of normal in the BOLD project. Eur Respir J 39(6):1343–1353, PMID: 22183479, 10.1183/09031936.00002711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu G, Zhou Y, Tian J, Yao W, Li J, Li B, et al. . 2010. Risk of COPD from exposure to biomass smoke: a metaanalysis. Chest 138(1):20–31, PMID: 20139228, 10.1378/chest.08-2114. [DOI] [PubMed] [Google Scholar]
- Huang Y, Du W, Chen Y, Shen G, Su S, Lin N, et al. . 2017. Household air pollution and personal inhalation exposure to particles (TSP/PM2.5/PM1.0/PM0.25) in rural Shanxi, North China. Environ Pollut 231(Pt 1):635–643, PMID: 28846984, 10.1016/j.envpol.2017.08.063. [DOI] [PubMed] [Google Scholar]
- Kurmi OP, Semple S, Simkhada P, Smith WC, Ayres JG. 2010. COPD and chronic bronchitis risk of indoor air pollution from solid fuel: a systematic review and meta-analysis. Thorax 65(3):221–228, PMID: 20335290, 10.1136/thx.2009.124644. [DOI] [PubMed] [Google Scholar]
- Kurmi OP, Vaucher J, Xiao D, Holmes MV, Guo Y, Davis KJ, et al. . 2016. Validity of COPD diagnoses reported through nationwide health insurance systems in the People’s Republic of China. Int J Chron Obstruct Pulmon Dis 11:419–430, PMID: 27042034, 10.2147/COPD.S100736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamprecht B, McBurnie MA, Vollmer WM, Gudmundsson G, Welte T, Nizankowska-Mogilnicka E, et al. . 2011. COPD in never smokers: results from the population-based Burden of Obstructive Lung Disease study. Chest 139(4):752–763, PMID: 20884729, 10.1378/chest.10-1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q, Jiang J, Wang S, Rumchev K, Mead-Hunter R, Morawska L, et al. . 2017. Impacts of household coal and biomass combustion on indoor and ambient air quality in China: current status and implication. Sci Total Environ 576:347–361, PMID: 27792953, 10.1016/j.scitotenv.2016.10.080. [DOI] [PubMed] [Google Scholar]
- Li R, Chambless L. 2007. Test for additive interaction in proportional hazards models. Ann Epidemiol 17(3):227–236, PMID: 17320789, 10.1016/j.annepidem.2006.10.009. [DOI] [PubMed] [Google Scholar]
- Li T, Cao S, Fan D, Zhang Y, Wang B, Zhao X, et al. . 2016. Household concentrations and personal exposure of PM2.5 among urban residents using different cooking fuels. Sci Total Environ 548–549:6–12, PMID: 26799802, 10.1016/j.scitotenv.2016.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S, Zhou Y, Liu S, Chen X, Zou W, Zhao D, et al. . 2017. Association between exposure to ambient particulate matter and chronic obstructive pulmonary disease: results from a cross-sectional study in China. Thorax 72(9):788–795, PMID: 27941160, 10.1136/thoraxjnl-2016-208910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S, Zhou Y, Wang X, Wang D, Lu J, Zheng J, et al. . 2007. Biomass fuels are the probable risk factor for chronic obstructive pulmonary disease in rural South China. Thorax 62(10):889–897, PMID: 17483137, 10.1136/thx.2006.061457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mestl HE, Aunan K, Seip HM, Wang S, Zhao Y, Zhang D. 2007. Urban and rural exposure to indoor air pollution from domestic biomass and coal burning across China. Sci Total Environ 377(1):12–26, PMID: 17343898, 10.1016/j.scitotenv.2007.01.087. [DOI] [PubMed] [Google Scholar]
- Muller CJ, MacLehose RF. 2014. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol 43(3):962–970, PMID: 24603316, 10.1093/ije/dyu029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peabody JW, Riddell TJ, Smith KR, Liu Y, Zhao Y, Gong J, et al. . 2005. Indoor air pollution in rural China: cooking fuels, stoves, and health status. Arch Environ Occup Health 60(2):86–95, PMID: 16983861, 10.3200/AEOH.60.2.86-95. [DOI] [PubMed] [Google Scholar]
- Pérez-Padilla R, Regalado J, Vedal S, Paré P, Chapela R, Sansores R, et al. . 1996. Exposure to biomass smoke and chronic airway disease in Mexican women. A case-control study. Am J Respir Crit Care Med 154(3 Pt 1):701–706, PMID: 8810608, 10.1164/ajrccm.154.3.8810608. [DOI] [PubMed] [Google Scholar]
- Po JY, FitzGerald JM, Carlsten C. 2011. Respiratory disease associated with solid biomass fuel exposure in rural women and children: systematic review and meta-analysis. Thorax 66(3):232–239, PMID: 21248322, 10.1136/thx.2010.147884. [DOI] [PubMed] [Google Scholar]
- Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, et al. . 2012. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J 40(6):1324–1343, PMID: 22743675, 10.1183/09031936.00080312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen G, Chen Y, Xue C, Lin N, Huang Y, Shen H, et al. . 2015. Pollutant emissions from improved coal- and wood-fuelled cookstoves in rural households. Environ Sci Technol 49(11):6590–6598, PMID: 25938574, 10.1021/es506343z. [DOI] [PubMed] [Google Scholar]
- Siddharthan T, Grigsby MR, Goodman D, Chowdhury M, Rubinstein A, Irazola V, et al. . 2018. Association between household air pollution exposure and chronic obstructive pulmonary disease outcomes in 13 low- and middle-income country settings. Am J Respir Crit Care Med 197(5):611–620, PMID: 29323928, 10.1164/rccm.201709-1861OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva R, Oyarzún M, Olloquequi J. 2015. Pathogenic mechanisms in chronic obstructive pulmonary disease due to biomass smoke exposure. Arch Bronconeumol 51(6):285–292, PMID: 25614376, 10.1016/j.arbres.2014.10.005. [DOI] [PubMed] [Google Scholar]
- Smith KR, Bruce N, Balakrishnan K, Adair-Rohani H, Balmes J, Chafe Z, et al. . 2014. Millions dead: how do we know and what does it mean? Methods used in the comparative risk assessment of household air pollution. Annu Rev Public Health 35:185–206, PMID: 24641558, 10.1146/annurev-publhealth-032013-182356. [DOI] [PubMed] [Google Scholar]
- Smith M, Li L, Augustyn M, Kurmi O, Chen J, Collins R, et al. . 2014. Prevalence and correlates of airflow obstruction in ∼317 000 never-smokers in China. Eur Respir J 44(1):66–77, PMID: 24603814, 10.1183/09031936.00152413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang X, Liao H. 2014. Energy poverty and solid fuels use in rural China: analysis based on national population census. Energy Sustain Dev 23:122–129, 10.1016/j.esd.2014.08.006. [DOI] [Google Scholar]
- Xu F, Yin X, Shen H, Xu Y, Ware RS, Owen N. 2007. Better understanding the influence of cigarette smoking and indoor air pollution on chronic obstructive pulmonary disease: a case–control study in Mainland China. Respirology 12(6):891–897, PMID: 17986120, 10.1111/j.1440-1843.2007.01178.x. [DOI] [PubMed] [Google Scholar]
- Zhang JJ, Smith KR. 2007. Household air pollution from coal and biomass fuels in China: measurements, health impacts, and interventions. Environ Health Perspect 115(6):848–855, PMID: 17589590, 10.1289/ehp.9479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong N, Wang C, Yao W, Chen P, Kang J, Huang S, et al. . 2007. Prevalence of chronic obstructive pulmonary disease in China: a large, population-based survey. Am J Respir Crit Care Med 176(8):753–760, PMID: 17575095, 10.1164/rccm.200612-1749OC. [DOI] [PubMed] [Google Scholar]
- Zhou X, Jin Y, He X. 1995. A study on the relationship between indoor air pollution and chronic obstructive pulmonary disease in Xuanwei County [in Chinese]. Zhonghua Yu Fang Yi Xue Za Zhi 29(1):38–40, PMID: 7600888. [PubMed] [Google Scholar]
- Zhou Y, Wang C, Yao W, Chen P, Kang J, Huang S, et al. . 2009. COPD in Chinese nonsmokers. Eur Respir J 33(3):509–518, PMID: 19251797, 10.1183/09031936.00084408. [DOI] [PubMed] [Google Scholar]
- Zhou Y, Zou Y, Li X, Chen S, Zhao Z, He F, et al. . 2014. Lung function and incidence of chronic obstructive pulmonary disease after improved cooking fuels and kitchen ventilation: a 9-year prospective cohort study. PLoS Med 11(3):e1001621, PMID: 24667834, 10.1371/journal.pmed.1001621. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.