Abstract
Chronic postsurgical pain (CPSP) following laparoscopic donor nephrectomy (LDN) is a disregarded topic. In this cross‐sectional study, all consecutive patients who underwent an LDN at the Radboud University Medical Center (Radboudumc; 2003‐2016) were approached for participation. Five hundred twelve living kidney donors were included and asked to complete two questionnaires, including the McGill Pain Questionnaire and the RAND Short Form‐36 Health Status Inventory (RAND SF‐36) regarding their health‐related quality of life (HRQoL). The mean prevalence of CPSP following LDN was 5.7%, with a mean follow‐up time of 6 years. Possible predictors of CPSP following LDN are severe early postoperative pain, previous abdominal surgery, and preexisting backache. The RAND SF‐36 revealed an impaired HRQoL in patients with CPSP when compared to patients without CPSP. In conclusion, this study revealed that the prevalence of CPSP following LDN is substantial. Given the possible association between the presence of CPSP and impaired HRQoL scores, living kidney donors should be well informed in the preoperative phase about the risk of CPSP.
Keywords: anesthesia/pain management, clinical research/practice, donor follow‐up, donors and donation, kidney transplantation, kidney transplantation/nephrology, living donor, patient safety, quality of life (QoL)
Short abstract
A cross‐sectional study of 512 patients who underwent laparoscopic donor nephrectomy shows a prevalence of chronic postsurgical pain of 5.7%, associated with an impaired quality of life.
Abbreviations
- CPSP
chronic postsurgical pain
- HALDN
hand‐assisted laparoscopic donor nephrectomy
- HARP
hand‐assisted retroperitoneoscopic donor nephrectomy
- HRQoL
health‐related quality of life
- IASP
International Association for the Study of Pain
- LDN
laparoscopic donor nephrectomy
- MPQ
McGill Pain Questionnaire
- NWC
number of words chosen
- PRI‐T
total score of Pain Rating Index
- RAND SF-36
RAND Short Form-36 Health Status Inventory; Radboudumc, Radboud university medical center
- SD
standard deviation
- VAS
visual analogue scale
1. INTRODUCTION
Laparoscopic donor nephrectomy (LDN) is the gold standard approach for living‐donor kidney procurement. When compared to open donor nephrectomy, LDN is associated with less postoperative pain, faster recovery, shorter length of hospital stays, quicker return to normal daily activities, and a better cosmetic result.1 Yet, some long‐term donor outcomes after LDN, such as chronic postsurgical pain (CPSP), seem to be an underexposed topic. CPSP is defined by the International Association for the Study of Pain (IASP) as pain that develops after a surgical procedure and persists for at least 3 months after surgery, where all other causes of pain (eg, infection, recurring malignancy) or preexisting pain problems are excluded.2, 3, 4 Possible pathologic factors leading to CPSP include inflammation, tissue and nerve damage, and altered central pain processing.5, 6 Well‐known preoperative and postoperative risk factors are preoperative pain, early postoperative pain, previous surgery, psychological factors or disorders, patient characteristics (ie, younger age and female gender), comorbidities, and alterations in central pain processing.5, 6 In addition the surgical technique can influence the development of CPSP, which is possibly related to the extent of intraoperative nerve injury and adhesion formation. A laparoscopic technique might reduce intraoperative nerve damage; however, the literature on CPSP following laparoscopic vs open procedures is inconsistent.6 Gerbershagen and colleagues described an incidence of CPSP following open nephrectomy (for benign and malignant renal disease) of 28.6% and 8.6%, after 3 and 6 months, respectively.7 Another study by Alper et al8 compared the incidence of CPSP following open vs laparoscopic nephrectomy for renal cell carcinoma. Two months after surgery they observed postsurgical pain in 16% of the patients who underwent an open procedure, and in 11% of the patients who underwent a laparoscopic procedure. After 6 months, only one patient in both the open nephrectomy group and the laparoscopic nephrectomy group reported CPSP (4% and 3.7%, respectively). Accordingly, they stated that the risk of developing CPSP after open or laparoscopic tumor nephrectomy is comparable. A small cohort study, performed by Owen and colleagues,9 assessed the incidence of CPSP following open donor nephrectomy. After a follow‐up period of 3 months, 33% of 81 participants reported the presence of CPSP following their donor nephrectomy. Wolf and colleagues compared the convalescence after hand‐assisted laparoscopic donor nephrectomy and open donor nephrectomy.10 Two of 11 (18%) of hand‐assisted donors and 14 of 17 (82%) of open surgical donors reported minor residual effects from the operation (P = .0015), with a median follow‐up time of 35‐37 weeks, which included skin numbness, pain (usually with activity), and bulging at the incision. No studies have been performed on the development of CPSP following laparoscopic donor nephrectomy. CPSP can have a significant impact on health‐related quality of life (HRQoL) and daily activities, as described in patients who underwent gastrointestinal surgery.11, 12, 13 To our knowledge, the impact of CPSP after LDN on HRQoL is unknown. The aim of this cross‐sectional study was to explore the prevalence and risk factors of CPSP following LDN and its impact on the HRQoL.
2. MATERIALS AND METHODS
2.1. Study design and patient population
A cross‐sectional study was performed among all living kidney donors who underwent a laparoscopic donor nephrectomy from January 2003 through December 2016 at the Radboud University Medical Center (Radboudumc) Nijmegen. All types of laparoscopic procedures were included. The gold standard at the Radboudumc is a transperitoneal approach; in selected cases the surgeon chooses a hand‐assisted retroperitoneoscopic approach (HARP) or if needed a conversion to a hand‐assisted laparoscopic donor nephrectomy (HALDN). Patients were eligible if they were able and willing to complete two questionnaires regarding chronic pain problems related to their donor nephrectomy and their HRQoL. All patients were approached by phone or mail, and after their consent they received the questionnaires and were asked to complete and return them. The study was approved by the medical ethics committee of the Radboudumc (2017‐3110).
2.2. Measures
The primary analysis consisted of the prevalence of CPSP following LDN. All included patients were asked if they still experienced pain related to their donor nephrectomy at the time that they were approached for this study. Patients were considered to have CPSP if their answer was “yes.” In that case, the patients were asked to complete the Dutch version of the McGill Pain Questionnaire (MPQ).14, 15 In addition, all included patients (with and without chronic pain) were asked to fill in the Dutch version of the RAND Short Form‐36 Health Status Inventory (RAND SF‐36) regarding their HRQoL.16, 17
The MPQ is a validated multidimensional pain questionnaire designed to measure the quality and intensity of chronic pain.14, 15 The main section includes a list of 63 words, arranged in 20 categories, describing different aspects of the experienced pain, each with three or four intensity levels. These words are divided into three major classes, that is, the sensory class describing the sensory quality of the pain; the affective class describing affective qualities of pain, including tension, fear, and autonomic reactions to the pain experience; and the evaluative class, describing the subjective overall intensity of the pain. The quality of the pain is described by the chosen words specifically. Each word is accompanied with a value, based on its rank order within the word set of its category. The pain intensity is measured by the Number of Words Chosen (NWC) and the Pain Rating Index (PRI), which is the sum of the rank values calculated for each of the three classes separately and in total. A higher score indicates worse pain. The PRI scores are useful mainly as a reference value to evaluate the effect of strategies to reduce CPSP. The MPQ also contains a Visual Analogue Scale (VAS), which represents the pain severity at the time point of the questionnaire and is filled out by the participant. In addition, the MPQ includes a section about localization, duration, and course of the pain, and a quality of life section. We did not include the quality of life section because we added a separate quality of life questionnaire.
The RAND Short Form‐36 Health Status Inventory (or RAND SF‐36) is a validated self‐administered questionnaire on HRQoL.16, 17 It is composed of 36 questions, organized into eight multi‐item scales: physical functioning, bodily pain, role limitations due to physical health problems, role limitations due to personal or emotional problems, general mental health, social functioning, energy/fatigue, and general health perceptions. The scores range from 0% to 100% per subscale, with higher scores indicating higher levels of functioning or well‐being.
We obtained preoperative data on quality of life from a selection of our patient group, provided by Wirken and colleagues, who performed a study on predonation cognition of potential living organ donors between 2010 and 2011.18 Therefore, we were able to compare preoperative and postoperative quality of life scores between patients with and without CPSP.
From all included patients, the medical records were reviewed to obtain information on their age during surgery, BMI, and relevant history, including previous abdominal surgery, preexisting pain problems (including spinal disc herniation and whiplash syndrome), and psychiatric disorders. In addition, perioperative and postoperative data were retrieved, including side of nephrectomy, duration of surgery, conversion to hand‐assisted or open procedures, presence of severe early postoperative pain, analgesic use, postoperative complications, length of hospital stay, and readmissions within 3 months after surgery. We specified severe early postoperative pain as pain for which prolonged hospitalization (>5 days), prolonged opioid use (stated as continuation after discharge, which is not standard of care at our center), or anesthesia consultation for adequate pain management was necessary.
2.3. Statistical analysis
Due to the design of this study, no sample size calculation was performed. Continuous data were presented as mean and standard deviation (SD); categorical data were presented as number and percentages. We used Student t‐test to compare normally distributed continuous variables and the chi‐square test for categorical variables. Binary logistic regression was performed to identify possible risk factors for CPSP following LDN. All available variables were included in a univariate model. Variables with a significance level of P < .05 in the univariate analysis were included in the multivariate model. We did not perform data imputation, as the amount of missing data within our study cohort was negligible. For all analyses, statistical significance was defined as P < .05. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS IBM Statistics 22; Armonk, NY).
3. RESULTS
3.1. Patient enrollment
A total of 862 patients underwent an LDN at Radboudumc Nijmegen in the period from January 2003 through December 2016. Forty‐nine patients were ineligible, since they passed away or because their contact details were lost. The remaining 813 patients were approached by phone or mail for written informed consent and participation between April 2017 and July 2017. We received responses from 542 patients (66.7%), of which 28 declined to provide informed consent and 2 were not able to complete the questionnaires because of illness. The remaining 512 adult living kidney donors signed informed consent and returned the questionnaires. The patient enrollment is depicted in Figure 1.
Figure 1.
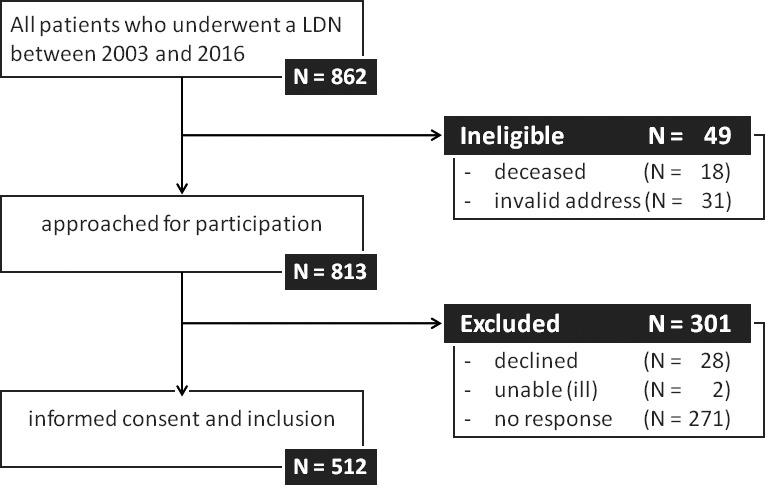
Flowchart patient enrollment. LDN, laparoscopic donor nephrectomy
3.2. Patient characteristics
The mean age ± SD at time of nephrectomy was 54.4 ± 9.9 years. Forty‐seven percent were male patients. The average length of follow‐up after surgery was 75.2 ± 44.3 months. Patient characteristics are presented in Table 1. We compared these patient characteristics with those of the nonrespondents group. The mean age of our respondents group was 6 years older, when compared to the nonrespondents group. There were no statistically significant differences in gender distribution and average length of follow‐up after surgery between the groups.
Table 1.
Patient characteristics
| Variables | All patients n = 512 |
|---|---|
| Age during surgery (y) | 54.4 ± 9.9 |
| Gender (male) | 242 (47.3%) |
| BMI (kg/m²) | 26.2 ± 3.6 |
| Side of nephrectomy (left) | 433 (84.6%) |
| Type of procedure | |
| Transperitoneal | 457 (89.3%) |
| Retroperitoneoscopic | 38 (7.4%) |
| Converted to hand‐assisted | 11 (2.1%) |
| Converted to open surgery | 6 (1.2%) |
| Length of follow‐up period | n (%) |
|---|---|
| 3 mo to <2 y | 74 (14.5%) |
| 2‐<4 y | 96 (18.8%) |
| 4‐<6 y | 89 (17.4%) |
| 6‐<8 y | 76 (14.8%) |
| 8‐<10 y | 84 (16.4%) |
| 10‐14 y | 93 (18.2%) |
Categorical variables are presented as n (%); continuous variables are presented as mean ± SD.
3.3. Prevalence of CPSP
In the group of 512 living kidney donors, 29 patients (5.7%) reported the presence of chronic pain related to their donor nephrectomy. The highest prevalence (12.2%) was reported in the group with a follow‐up time of 3 to 24 months after surgery. The prevalence of CPSP per follow‐up interval is presented in Figure 2.
Figure 2.
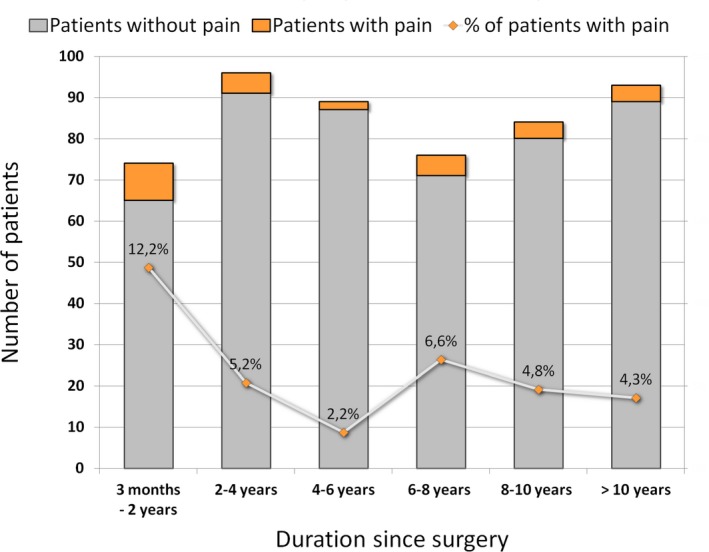
Prevalence of CPSP per period of follow‐up time. CPSP, chronic postsurgical pain
3.4. McGill Pain Questionnaire
Pain characteristics were evaluated by the MPQ, presented in Table 2. Pain unset was slow in 16 patients (55.2%) and acute in 10 patients (34.5%). Various courses of pain were reported; most patients (48.3%) experienced continuous pain, differing in severity, but 37.9% of the patients described pain attacks with pain‐free intervals. The most reported pain localizations were the flank (25.0%), especially at the side of surgery, followed by the groin (18.2%) and suprapubic region (15.9%). Seven patients also experienced referred pain sensations. The mean general pain quantity, measured by a VAS, was a score of 20 (± 22) of 100.
Table 2.
Pain characteristics
| McGill Pain Questionnaire components | Patients with CPSP n = 29 |
|---|---|
| Start of pain | |
| Acute | 10 (34.5%) |
| Slowly | 16 (55.2%) |
| Unknown | 3 (10.3%) |
| Course of pain experience | |
| Pain attacks, with pain‐free moments | 11 (37.9%) |
| Continuous, differing in severity | 14 (48.3%) |
| Continuous, stable severity | 2 (6.9%) |
| VAS, general (0‐100) | 20 ± 22 |
| VAS, least pain (0‐100) | 9 ± 11 |
| VAS, worst pain (0‐100) | 45 ± 28 |
| Localization of pain | |
| Flank | 11 (25.0%) |
| Groin | 8 (18.2%) |
| Suprapubic region | 7 (15.9%) |
| Lower back | 6 (13.6%) |
| Upper back | 4 (9.1%) |
| Extremities | 3 (6.8%) |
| Upper abdomen | 2 (4.5%) |
| Other (scrotum, shoulders, head) | 3 (6.8%) |
| Referred pain present | 7 (24.1%) |
| Pain intensity | |
| NWC‐S (0 to 12 words) | 3.34 ± 2.91 |
| NWC‐A (0 to 5 words) | 0.90 ± 1.24 |
| NWC‐E (0 to 3 words) | 1.97 ± 1.18 |
| NWC‐T (0 to 20 words) | 6.21 ± 4.58 |
| PRI‐S (0 to 36) | 5.69 ± 5.63 |
| PRI‐A (0 to 15) | 1.28 ± 1.81 |
| PRI‐E (0 to 12) | 3.24 ± 2.59 |
| PRI‐T (0 to 63) | 10.21 ± 9.06 |
Categorical variables are presented as n (%); continuous variables are presented as mean ± SD.
CPSP, chronic postsurgical pain; VAS, visual analogue scale; NWC‐S, Number of Words Chosen of the sensory scale; NWC‐A, NWC of the affective scale; NWC‐E, NWC of the evaluative scale; NWC‐T, total NWC; PRI‐S, Pain‐Rating Index of the sensory scale; PRI‐A, PRI of the affective scale; PRI‐E, PRI of the evaluative scale; PRI‐T, total PRI.
The mean NCW was 6.2 of 20 words. Sensory descriptors were chosen more frequently than affective or evaluative terms. The most frequently selected words were nagging (n = 12; 41.4%) and stabbing (n = 11; 37.9%) in the sensory class; tiring (n = 6; 20.7%) in the affective class; and annoying (n = 16; 55.2%) in the evaluative class. The mean pain intensity measured by the total score of the PRI (PRI‐T was 10.21 ([SD 9.06; maximal possible score 63]). We performed subgroup analyses to assess the pain intensity (PRI‐T) in different types of patients; data are shown in Table 3. Pain intensity was higher in younger patients than older patients (P = .01). Gender, BMI, side of nephrectomy, and time since surgery were not of influence on the level of pain. We did not compare the different types of procedures, as the numbers of patients per group were too small to draw conclusions. Eight patients (27.6%) reported the use of analgesics because of their experienced pain, mostly acetaminophen or nonsteroidal antiinflammatory drugs; one patient reported the use of tramadol. None of the patients reported consultation of a pain specialist.
Table 3.
PRI‐T subgroup analyses
| Analysis | Number of patients | Mean PRI‐T | P‐value |
|---|---|---|---|
| All patients | 29 (of 512 patients) | 10.21 ± 9.06 | — |
| Gender | .70 | ||
| Male | 10 | 9.30 ± 2.44 | |
| Female | 19 | 10.68 ± 9.85 | |
| Age (y) | .01 | ||
| 35‐<40 | 3 | 21.00 ± 14.18 | |
| 40‐<45 | 6 | 14.17 ± 10.05 | |
| 45‐<50 | 2 | 13.00 ± 16.97 | |
| 50‐<55 | 4 | 8.50 ± 4.80 | |
| 55‐<60 | 8 | 6.63 ± 5.90 | |
| 60‐65 | 6 | 5.83 ± 4.49 | |
| BMI (kg/m²) | .08 | ||
| <25 | 9 | 13.00 ± 10.59 | |
| 25‐30 | 15 | 11.27 ± 8.27 | |
| >30 | 5 | 2.00 ± 2.12 | |
| Side of nephrectomy | .32 | ||
| Left | 27 (of 433 procedures) | 9.74 ± 8.92 | |
| Right | 2 (of 79 procedures) | 16.50 ± 12.02 | |
| Time since surgery (y) | .48 | ||
| 0‐<2 | 9 (of 74 patients) | 10.22 ± 9.36 | |
| 2‐<4 | 5 (of 96 patients) | 8.20 ± 5.72 | |
| 4‐<6 | 2 (of 89 patients) | 13.50 ± 7.78 | |
| 6‐<8 | 5 (of 76 patients) | 11.20 ± 12.56 | |
| 8‐<10 | 4 (of 84 patients) | 16.50 ± 11.33 | |
| 10‐14 | 4 (of 93 patients) | 3.50 ± 1.00 |
Data were analyzed using analysis of variance (ANOVA). Variables are presented as mean ± standard deviation (SD).
Significant P‐values are in bold.
PRI‐T, total pain rating index (score 0‐63).
3.5. Risk factors for the development of CPSP
The group of patients with CPSP comprised 10 male (34.5%) and 19 female (65.5%) patients, with a mean age at time of nephrectomy of 52 ± 9 years and a BMI of 26.8 ± 4.4 kg/m². Ninety‐three percent of the donors with CPSP donated their left kidney. Relevant history included previous abdominal surgery (41.4%), preexisting pain problems (31.0%), and psychiatric disorders (6.9%). Ten patients (34.5%) had severe early postoperative pain. We performed binary logistic regression to identify predictive factors for CPSP following LDN, presented in Table 4. In the univariate analysis, severe early postoperative pain, previous abdominal surgery, preexisting pain problems, psychiatric history, and postoperative wound problems (ie, wound infection or hernia) had a significance level of P < .05. These variables were included in the multivariate analysis, in which the presence of severe early postoperative pain, previous abdominal surgery, and preexisting pain problems turned out to be predictors for the development of CPSP following LDN. The patients with CPSP localized at the back did not report preexisting backache problems.
Table 4.
Univariate and multivariate regression analysis for CPSP following LDN
| Parameters | Univariate analysis OR (95% CI) | P‐value | Multivariate analysis OR (95% CI) | P‐value |
|---|---|---|---|---|
| Age at time of surgery | 0.975 (0.940‐1.011) | .172 | — | — |
| Gender (male) | 0.569 (0.259‐1.250) | .160 | — | — |
| BMI (kg/m²) | 1.046 (0.946‐1.157) | .378 | — | — |
| Side of nephrectomy (left) | 2.573 (0.599‐11.044) | .204 | — | — |
| Duration of surgery | 1.398 (0.730‐2.675) | .312 | — | — |
| Converted to HARP, HALDN, or open procedure | 2.311 (0.503‐10.626) | .282 | — | — |
| Severe early postoperative pain | 3.143 (1.402‐7.044) | .005 | 2.470 (1.036‐5.888) | .041 |
| Length of hospital stay | 1.054 (0.901‐1.234) | .509 | — | — |
| Postoperative readmission | 2.895 (0.617‐13.591) | .178 | — | — |
| Time from surgery | 0.992 (0.983‐1.001) | .097 | — | — |
| Previous abdominal surgery | 5.608 (2.542‐12.373) | <.001 | 5.170 (2.278‐11.733) | <.001 |
| Preexisting pain problems | 4.174 (1.798‐9.692) | .001 | 3.326 (1.343‐8.237) | .009 |
| Psychiatric history | 5.889 (1.135‐30.559) | .035 | 3.983 (0.537‐29.522) | .176 |
| Postoperative wound infection or hernia | 2.841 (1.018‐7.928) | .046 | 1.210 (0.322‐4.551) | .778 |
Significant P values are in bold.
CPSP, chronic postsurgical pain; HARP, hand‐assisted retroperitoneoscopic procedure; HALDN, hand‐assisted laparoscopic donor nephrectomy; LDN, laparoscopic donor nephrectomy; OR, odds ratio; 95% CI, 95% confidence interval.
Within all 29 patients with CPSP following their LDN, there were no negative outcomes of the recipients (in all cases a well‐functioning graft within the first year). Therefore, we conclude that it is unlikely that our results were influenced by the recipients' outcomes.
3.6. Health‐related quality of life
The postoperative HRQoL of living kidney donors with CPSP was lower, when compared to donors without pain, as shown in Table 5. A major difference (32.6%) was seen with regard to role limitations due to physical health problems between donors without CPSP (89.7% ± 27.5%) and donors with CPSP (57.1% ± 47.1%) (P = .001). Furthermore, on the scale of bodily pain, the level of functioning in the group with CPSP was 20% lower (72.1 ± 21.6) when compared to donors without CPSP (92.1 ± 16.0), (P < .001), and also a reduction in energy of 18.3% was found in the patients with CPSP when compared to patients without CPSP (P < .001).
Table 5.
HRQoL after donor nephrectomy (RAND SF‐36)
| RAND SF‐36 subscales (%) | Whole group n = 512 | Patients with pain n = 29 | Patients without pain n = 483 | P‐value |
|---|---|---|---|---|
| Physical functioning | 91.0 ± 15.4 | 80.7 ± 18.9 | 91.6 ± 14.9 | .005 |
| Role limitations due to physical health problems | 87.9 ± 29.8 | 57.1 ± 47.1 | 89.7 ± 27.5 | .001 |
| Role limitations due to personal or emotional problems | 93.6 ± 22.2 | 80.5 ± 38.3 | 94.4 ± 20.6 | .063 |
| Energy/fatigue | 70.0 ± 19.2 | 52.8 ± 19.7 | 71.1 ± 18.7 | <.001 |
| General mental health | 81.9 ± 14.2 | 71.4 ± 16.9 | 82.6 ± 13.8 | .002 |
| Social functioning | 92.5 ± 16.1 | 83.6 ± 23.4 | 93.0 ± 15.4 | .041 |
| Bodily pain | 90.9 ± 17.0 | 72.1 ± 21.6 | 92.1 ± 16.0 | <.001 |
| General health perceptions | 76.0 ± 18.6 | 63.2 ± 21.1 | 76.7 ± 18.1 | <.001 |
Significant P values are in bold.
Variables are presented as mean ± SD.
HRQoL, health‐related quality of life.
We obtained preoperative data by Wirken and colleagues on the HRQoL of 104 patients of our patient group, including 99 patients without CPSP and 5 patients with CPSP. The preoperative HRQoL scores were comparable between both groups, except for a significant lower score in the general mental health of the patients with CPSP when compared to patients without pain (respectively, 72.8 ± 16.59 vs 85.78 ± 10.46, P = .01). Slight significant impairments were seen in the postoperative scores when compared to preoperative scores in the group without CPSP, in physical functioning, general mental health, and energy level. The group of patients with CPSP showed severe deterioration after surgery in role limitations due to physical health problems, in bodily pain, and in physical functioning. Preoperative and postoperative HRQoL scores of both groups are depicted in Figure 3.
Figure 3.
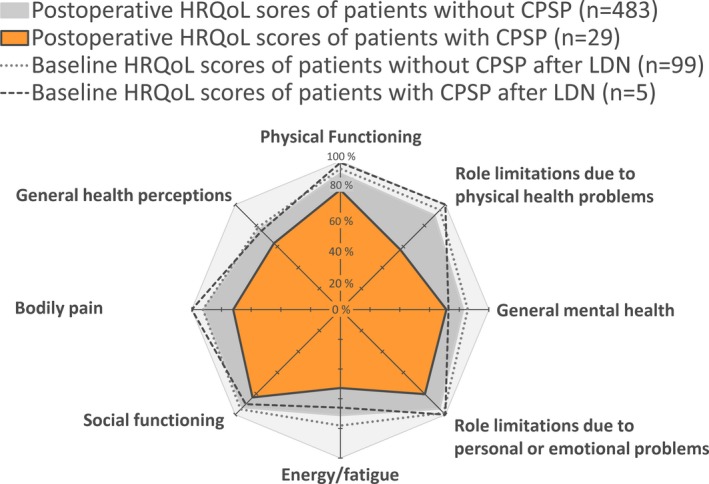
HRQoL before and after LDN. HRQoL, health‐related quality of life; LDN, laparoscopic donor nephrectomy
4. DISCUSSION
This is the first study on the prevalence of CPSP following LDN. In this study, the mean prevalence of CPSP was 5.7% percent of 512 donors who underwent a LDN at the Radboudumc, with a mean follow‐up of 6.3 (±3.7) years. The mean pain intensity measured by VAS was 20 on a scale of 0‐100 and by PRI‐T was 10 on a scale of 0‐63. The multivariable regression analyses revealed that severe early postoperative pain, previous abdominal surgery, and preexisting pain problems are possible risk factors for the development of CPSP following LDN. Furthermore, we found an impaired quality of life in patients with CPSP when compared to patients without CPSP, which is likely to be causally related.
Given the impaired general mental health scores in patients who went on to develop CPSP, future research should pursue if impaired general mental health is a contraindication for kidney donation.
When compared to our findings, Owen et al observed remarkably higher incidences of postsurgical pain in open donor nephrectomy,9 which could be explained by the refinement in surgical techniques with less intraoperative nerve injury, which might lead to a decreased risk of CPSP following LDN. In accordance, a tumor nephrectomy is a more invasive procedure when compared to LDN: first, because kidney removal during tumor nephrectomy includes removal of the renal fascia, and second because of the use of a muscle‐splitting McBurney incision instead of an intermuscular Pfannenstiel incision. This could explain why we found fewer patients with CPSP following LDN, when compared to patients who experienced CPSP following tumor nephrectomy.7, 8 Our study population included six patients in whom the surgery was converted to an open procedure. We performed additional analyses in which we excluded these patients (data not shown), which revealed no influence on our outcomes.
Because of our study design, we were able to compare the prevalence of CPSP in a large number of patients over different periods of time since surgery, with a mean follow‐up time of 6.3 (± 3.7) years. In the prospective study by Owen and colleagues,9 all patients were approached 3 months after surgery. As shown in our patient group, the highest prevalence of CPSP was seen in this early period. However, we showed that the complaints of CPSP are also found over longer periods, even after more than 10 years.
This study has some limitations. First, due to the cross‐sectional design, we could not assess the incidence of CPSP following LDN. The incidence of CPSP might be greater than 5.7%, as CPSP complaints may have resolved prior to the interview. There is also a slight risk of recall bias, as patients with a shorter follow‐up period might be more likely to attribute pain complaints to their donor nephrectomy, compared to patients in whom the surgery was more remote. Another limitation is that we received no response from 271 patients. There was a 6‐year difference with the respondents group and the nonrespondents group, which might have influenced our results. Due to the cross‐sectional design, we could not perform baseline preoperative measurements on the HRQoL. However, we obtained preoperative data on the HRQoL of 20% of the included patients.18 The MPQ is a validated questionnaire. Despite this, there are different methods in the calculation of pain intensity scores, due to different language versions and adjusted short‐form versions. Therefore, the PRI scores cannot be compared between versions of the MPQ. Nevertheless, our PRI scores can serve as reference values when using the Dutch language version. Furthermore, the MPQ is an ideal instrument to evaluate the effects of strategies to reduce CPSP following LDN in future studies. Finally,, due to the small number of events (29 patients with CPSP), there might be overestimation of the regression coefficients in our multivariate analysis. However, our findings are in line with known risk factors for CPSP in general.6 Prospective studies are needed for further investigation of risk factors for CPSP following LDN.
In conclusion, our unique data indicate that CPSP following LDN is a highly relevant issue. We found a substantial prevalence of CPSP of 5.7% following LDN. Given the possible association between the presence of CPSP and impaired HRQoL scores, living kidney donors should be well informed during the preoperative phase about the risk of CPSP. Prospective future studies should pursue strategies to reduce the incidence of CPSP after LDN.
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
Bruintjes MHD, van Helden EV, de Vries M, et al. Chronic pain following laparoscopic living‐donor nephrectomy: Prevalence and impact on quality of life. Am J Transplant. 2019;19:2825–2832. 10.1111/ajt.15350
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Wilson CH, Sanni A, Rix DA, et al. Laparoscopic versus open nephrectomy for live kidney donors. Cochrane Database Syst Rev. 2011(11):Cd006124. [DOI] [PubMed] [Google Scholar]
- 2. Macrae WA. Chronic pain after surgery. Br J Anaesth. 2001;87(1):88‐98. [DOI] [PubMed] [Google Scholar]
- 3. Treede RD, Rief W, Barke A, et al. A classification of chronic pain for ICD‐11. Pain. 2015;156(6):1003‐1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Werner MU, Kongsgaard UEI. Defining persistent post‐surgical pain: is an update required? Br J Anaesth. 2014;113(1):1‐4. [DOI] [PubMed] [Google Scholar]
- 5. Reddi D, Curran N. Chronic pain after surgery: pathophysiology, risk factors and prevention. Postgrad Med J. 2014;90(1062):222‐227; quiz 226. [DOI] [PubMed] [Google Scholar]
- 6. van Rijckevorsel DC, de Vries M, Schreuder LT, et al. Risk factors for chronic postsurgical abdominal and pelvic pain. Pain Manag. 2015;5(2):107‐116. [DOI] [PubMed] [Google Scholar]
- 7. Gerbershagen HJ, Dagtekin O, Rothe T, et al. Risk factors for acute and chronic postoperative pain in patients with benign and malignant renal disease after nephrectomy. Eur J Pain. 2009;13(8):853‐860. [DOI] [PubMed] [Google Scholar]
- 8. Alper I, Yuksel E. Comparison of acute and chronic pain after open nephrectomy versus laparoscopic nephrectomy: a prospective clinical trial. Medicine (Baltimore). 2016;95(16):e3433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Owen M, Lorgelly P, Serpell M. Chronic pain following donor nephrectomy–a study of the incidence, nature and impact of chronic post‐nephrectomy pain. Eur J Pain. 2010;14(7):732‐734. [DOI] [PubMed] [Google Scholar]
- 10. Wolf JS Jr, Merion RM, Leichtman AB, et al. Randomized controlled trial of hand‐assisted laparoscopic versus open surgical live donor nephrectomy. Transplantation. 2001;72(2):284‐290. [DOI] [PubMed] [Google Scholar]
- 11. Bruce J, Krukowski ZH. Quality of life and chronic pain four years after gastrointestinal surgery. Dis Colon Rectum. 2006;49(9):1362‐1370. [DOI] [PubMed] [Google Scholar]
- 12. VanDenKerkhof EG, Hopman WM, Reitsma ML, et al. Chronic pain, healthcare utilization, and quality of life following gastrointestinal surgery. Can J Anaesth. 2012;59(7):670‐680. [DOI] [PubMed] [Google Scholar]
- 13. Jeppesen M, Tolstrup MB, Gogenur I. Chronic pain, quality of life, and functional impairment after surgery due to small bowel obstruction. World J Surg. 2016;40(9):2091‐2097. [DOI] [PubMed] [Google Scholar]
- 14. Vanderiet K, Adriaensen H, Carton H, et al. The McGill Pain Questionnaire constructed for the Dutch language (MPQ‐DV). Preliminary data concerning reliability and validity. Pain. 1987;30(3):395‐408. [DOI] [PubMed] [Google Scholar]
- 15. Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975;1(3):277‐299. [DOI] [PubMed] [Google Scholar]
- 16. Hays RD, Sherbourne CD, Mazel RM. The RAND 36‐Item Health Survey 1.0. Health Econ. 1993;2(3):217‐227. [DOI] [PubMed] [Google Scholar]
- 17. VanderZee KI, Sanderman R, Heyink JW, et al. Psychometric qualities of the RAND 36‐Item Health Survey 1.0: a multidimensional measure of general health status. Int J Behav Med. 1996;3(2):104‐122. [DOI] [PubMed] [Google Scholar]
- 18. Wirken L, van Middendorp H, Hooghof CW, et al. Pre‐donation cognitions of potential living organ donors: the development of the Donation Cognition Instrument in potential kidney donors. Nephrol Dial Transplant. 2017;32(3):573‐580. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


