Abstract
Hip fractures usually occur in elderly patients who commonly have pre-existing medical problems or comorbidities. We retrospectively reviewed 100 patients admitted to our unit with a hip fracture to quantify their medical complexity. Age and comorbidity profile were used to determine an age-adjusted Charlson Co-morbidity Index (ACCI). The findings were then compared to 100 patients admitted under the care of the acute medical team. The patients in the fracture group were significantly older (p<0.0001), had significantly more co-morbidities (p<0.0001) and had a significantly greater predicted one-year mortality (p<0.0001). Cardiorespiratory disorders were the most common co-morbidities in the hip fracture group. We discuss our findings in combination with a review of the pertinent literature.
Keywords: hip fracture, co-morbidity
INTRODUCTION
Approximately 80,000 hip fractures are treated each year in the United Kingdom representing a significant public health issue.1 With an ageing population it is predicted that the overall number of fragility fractures, including hip fractures, will continue to rise resulting in a significant financial challenge to healthcare systems.2-7 In Northern Ireland, the incidence of hip fractures rose from 54 in 100,000 in 2000 to 86 in 100,000 in 2015 with the incidence predicted to rise to 128 in 100,000 in 2030.8
Hip fractures are associated with significant morbidity and mortality 9 and are being seen in an increasingly elderly population.8,10 Furthermore, patients sustaining a proximal femoral fracture are becoming increasingly frail in conjunction with fracture patterns that have become more complex.8 Increasing age and comorbidity are key factors for in-hospital mortality and cardiorespiratory disease accounts for the majority of cases of early hip fracture mortality.11 Hip fractures usually occur in patients who have pre-existing medical problems or comorbidities.12,13 It is recognised that comorbidity influences the treatment and prognosis of an index condition.14
Due to the changing demographics of patients sustaining a hip fracture, Trauma and Orthopaedic surgeons are increasingly being faced with caring for elderly, frail patients requiring more complex surgical procedures. The aim of this study was to quantify the medical complexity of patients admitted to our unit with a hip fracture and compare the findings to a group of patients admitted to the Acute Medical Unit under the care of the medical team. We discuss our findings and provide a review of the literature.
PATIENTS AND METHODS
Our Trauma and Orthopaedic Unit is based within a District General Hospital setting serving a population of approximately 440,000. On average, approximately 420 hip fractures are admitted to our unit each year. There are eight Trauma and Orthopaedic Consultants, one Orthogeriatrician, one Orthophysician and a complement of junior medical staff comprised of foundation trainees, core trainees, higher surgical trainees and staff grades. Within our institution we have a dedicated Consultant-led hip fracture service, which adheres to the multidisciplinary principles of national guidance. Currently, acute medical problems out of hours and at weekends are managed by the Trauma and Orthopaedic team with referral to the on-call medical team as required. Although we do not have Orthogeriatric care at the weekends, we have anaesthetic cover to ensure patients are optimised out of hours, aiming for 95% of hip fracture patients to have surgery within 48hours of being declared medically fit for the procedure. In order to achieve this, our centre has daily trauma lists and dedicated weekend trauma lists.
We retrospectively reviewed the charts of 100 patients admitted to our unit with a hip fracture. Subtrochanteric and diaphyseal fractures were excluded. For this group (Group A) we recorded the following parameters: age at presentation, gender, comorbidities on admission and the radiographic hip fracture pattern. Comorbidities were defined as pre-existing and previously diagnosed conditions. We then prospectively reviewed the charts of 100 patients admitted under the medical team to the Acute Medical Unit and for this group (Group B) we recorded age at presentation, gender, the reason for admission, and comorbidities.
The Charlson Comorbidity Index (CCI),14 which comprises 19 weighted comorbidity items has been validated in various clinical settings and is widely used to predict inpatient and one- year mortality in hospitalised patients and the survival of critically ill patients.15,16,17 Age is reportedly a significant predictor of survival outcome and has therefore been incorporated into the CCI score to create a single index that accounts for both comorbidity and age, the age-adjusted Charlson comorbidity index (ACCI)18 [Table 1]. The recorded data was used to produce an ACCI for each patient in both groups.
Table 1. The Age-adjusted Charlson Comorbidity Index (ACCI).
| Age-comorbidity score | Estimated relative risk of death (99% confidence interval) |
|---|---|
| 0 | 1.0 |
| 1 | 1.45 (1.25, 1.68) |
| 2 | 2.10 (1.57, 2.81) |
| 3 | 3.04 (1.96, 4.71) |
| 4 | 4.40 (2.45, 7.90) |
| 5 | 6.38 (3.07, 13.24) |
| 6 | 9.23 (3.84, 22.20) |
| 7 | 13.37 (4.81, 37.22) |
| 8 | 19.37 (6.01, 62.40) |
Data was tested for normality using the Shapiro-Wilk test. For parametric data, the Wilcoxon test was used and for non parametric data the Mann-Whitney U Test. All tests were performed using SPSS v22 for Mac (IBM Ltd, Armonk, NY, USA). For all analyses, a value <0.05 was considered statistically significant.
RESULTS
In Group A, there were 11 males and 89 females. The average age was 80 years (SD, 10.48 years). Fifty-four patients sustained an intracapsular fracture and 46 sustained an extracapsular fracture. Ninety-four of the patients had operative management for their hip fracture. The average number of comorbidities was 2.79 (SD, 2.2). In this group the commonest comorbidities were cardiac (28%), respiratory (14%) and renal (12%) disorders. Of note, for those patients with a cardiac disorder, 20 patients and 7 patients had two and three different cardiac conditions respectively (e.g. a combination of atrial fibrillation and ischaemic heart disease). Seventeen patients (17%) had dementia on admission. Based on the ACCI, the estimated relative risk of mortality at one year for group A was calculated at 8. At one-year follow-up of our cohort, the actual one-year mortality was 17%.
In group B, there were 70 males and 30 females. The average age was 60.44 years (SD, 19.79 years). The average number of comorbidities was 1.39 (SD, 1.16). In this group the commonest comorbidities were cardiac (40%), metabolic/ endocrine (17%) and respiratory (16%) disorders. Only 5 patients had two different cardiac conditions. Nine patients (7%) had dementia on admission. Based on the ACCI, the estimated relative risk of mortality at one-year for group B was calculated at 4.84. At one-year follow-up of our cohort, the actual one-year mortality for group B was 11%. The reason for the medical admission is summarised in Figure 1. Statistical analysis demonstrated that patients in group A were significantly older, had significantly more co-morbidities and a significantly higher relative one-year mortality when compared to group B (p <0.0001- all parameters) [Table 2].
Fig 1. Reason for medical admission Group B.
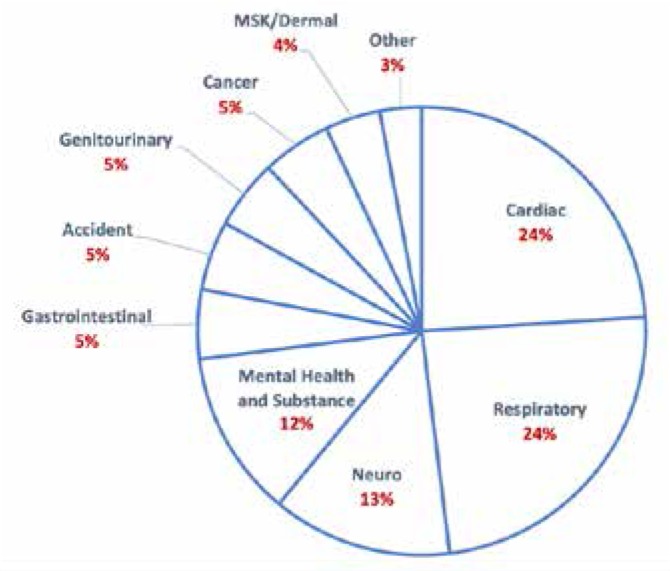
Table 2. Statistical analysis of key parameters.
| Group A | mean | SD | median | min | max | range | Significance |
|---|---|---|---|---|---|---|---|
| Age | 80.04 | 10.48 | 81 | 48 | 97 | 49 | p<0.00001 |
| No. of Comorbidities | 2.79 | 2.2 | 2 | 0 | 13 | 13 | p<0.00001 |
| Charlson Score | 5.11 | 1.93 | 5 | 0 | 9 | 9 | |
| Est. Relative Risk | 8 | 5.05 | 6.38 | 1 | 19.37 | 18.37 | p<0.00001 |
| Male | 11% | ||||||
| Female | 89% |
| Group B | mean | SD | median | min | max | range | Significance |
|---|---|---|---|---|---|---|---|
| Age | 60.44 | 19.79 | 65 | 14 | 96 | 82 | p<0.00001 |
| No. of Comorbidities | 1.39 | 1.16 | 1 | 0 | 4 | 4 | p<0.00001 |
| Charlson Score | 3.22 | 2.57 | 3 | 0 | 12 | 12 | |
| Est. Relative Risk | 4.84 | 4.65 | 3.04 | 1 | 19.37 | 18.37 | p<0.00001 |
| Male | 70% | ||||||
| Female | 30% |
DISCUSSION
Fractures of the hip are a common and profound cause of morbidity and mortality and pose a great challenge to healthcare services and patients. Hip fractures often occur in medically frail patients.13 Surgery is the definitive treatment for almost all hip fractures. Pre-existing illness, functional deficit, surgical stress and postoperative immobilisation result in mortality one-year after operation of up to 30%.19
Extensive guidance regarding the management of patients with a fracture of the hip has been issued by the British Orthopaedic Association and British Geriatric Society, the National Institute for Health and Clinical Excellence, the Department of Health, and the National Confidential Enquiry into Peri-operative Deaths. However, despite all the recommendations it is inevitable that a proportion of patients with a hip fracture will die irrespective of the quality of the medical care.
Whilst proper surgical technique and implant choice play a role in outcome, the decision-making outside the operating room and the manner in which preoperative care is delivered and co-ordinated play an important role in medically complex, hip fracture patients. With this in mind, the aim of this study was primarily to quantify the medical complexity of hip fracture patients admitted to our unit based on their co-morbidities. In order to provide a benchmark, we compared the age, gender and comorbidity profile of our hip fracture patients to that of a ‘snapshot’ of patients admitted under the care of the Acute Medical Team who can provide emergent 24hour medical cover for their patients.
The average age of the patients in our hip fracture group was 80 years which is representative of national data and in keeping with other published studies.8,11 There was a female to male ratio of approximately 8:1 which is a higher preponderance of female patients when compared with national data and that reported by other authors8,11 but may simply reflect the relatively small sample size of our study group. With regards to gender, it is well-recognised that males are more likely to have an adverse outcome following a hip fracture.8,11,20 This may therefore be a specific patient subgroup that should warrant special attention when admitted with a hip fracture. Age has also been reported as a significant predictor of survival outcome18 and it is worthy of mention that the patients in the hip fracture group were on average 20 years older than the medical patients.
When assessing fracture pattern, 54% patients sustained an intracapsular fracture and 46% an extracapsular fracture which is in keeping with the findings noted in a recently published, large demographic study of hip fracture patients in Northern Ireland.8 Furthermore, Tucker et al.8 noted a simultaneous increase in both complex extracapsular fractures and subtrochanteric fractures from 2009 onwards with a rise in the need for hip hemiarthoplasty, cephalo-medullary nails and other more complex implants. In essence, older and more medically frail patients need more complex surgical procedures which may have an impact on the patient’s medical stability during the in-hospital period.
In our hip fracture group, cardiac, respiratory and renal conditions were the most common co-morbidities. Furthermore, a significant number of patients had several different cardiac disorders. Chatterton et al.11 retrospectively studied 4426 hip fracture patients and found that the majority of deaths (77%) within 30 days occurred in hospital with the majority within the first ten days of admission. Male gender, increasing age and comorbidity were significantly associated with in-hospital mortality however the strongest predictor of mortality was increasing comorbidity.11 Furthermore, Chatterton et al.11 noted that respiratory infections and cardiovascular disease were the predominant causes of in-hospital death which has also been reported in other studies.21,22
The ASA classification is a measure of intraoperative and immediate postoperative risk based on the severity of patient co-morbidities.23 Donegan et al.24 demonstrated that medical complications were more common in hip fracture patients in ASA class 3 and class 4 than those in ASA class 2 and there was no significant relationship between ASA class and surgical complications. They also noted that almost 75% of patients in ASA class 4 had some medical problem that required acute medical management in the peri-operative period and almost one third in ASA class 4 had a cardiac or pulmonary issue requiring medical management postoperatively.
In our study we used the ACCI18 as a marker of co-morbidity instead of ASA grade. The patients in the hip fracture group had approximately twice the number of co-morbidities when compared to the medical admissions and this combined with being significantly older resulted in a significantly greater ACCI score for the hip fracture group. This is without taking into consideration the physiological impact of the hip fracture and the stress imparted by the surgical procedure. It is also worthy of mention that 17% of the hip fracture patients had dementia on admission versus only 7% of the medical group. Although not surprising, the addition of dementia adds to the challenge of caring for hip fracture patients with multiple medical co-morbidities.
Tarrant et al.25 following a review of in-patient deaths in hip fracture patients in their institution concluded that preventable errors were found, some of which were considered to have contributed to the patients’ death. They found that that very few errors occurred during the operation and that inadequate medical team involvement and inadequate management of medical conditions were two key factors. Interestingly, despite the fact that most of the patients who died in hospital presented and had their surgery during normal working hours, more than two-thirds of deaths occurred outside this time and most commonly from cardiorespiratory disease.25
Thomas et al.26 found that weekend admission for patients with a fractured neck of femur was both significantly and independently associated with a rise in 30-day mortality. They suggested that increased mortality with weekend admission may be explained by a combination of factors including the loss of early orthogeriatric input, the reduction in the number of ward-based medical staff and the decreased access to diagnostic tools and subspecialty opinions. Other studies have not demonstrated a similar association between weekend admission and 30-day mortality.11,27
Whilst several models of care have been proposed for patients with a hip fracture, in the United Kingdom most patients still receive traditional orthopaedic management such as that in our unit. The treatment of elderly patients with a hip fracture with a multidisciplinary approach has been shown to result in fewer postoperative medical complications, fewer transfers to the intensive care unit, improvement in ambulatory status and walking distance at the time of discharge, a higher return-to-home rate with fewer discharges to nursing homes, and a decreased length of the hospital stay.13,28,29 The early identification of high-risk patients and daily individualised medical care have been shown to reduce the incidence of medical complications associated with the treatment of elderly patients with a hip fracture.29 A relatively recent development has been the establishment of so-called ‘co-management services’ which refers to services set up in an institution in which both medical and surgical teams work together as primary caregivers directly co-ordinating care.30 Several recent studies have demonstrated a significant relationship between co-management and clinical outcomes31,32 whilst other studies have however demonstrated no benefit.33,34
We believe that the findings of our study highlight the multidisciplinary medical challenges of the in-hospital management of patients with a hip fracture admitted to a Trauma and Orthopaedic unit. We acknowledge the limitations of our study- retrospective design, the relatively small numbers of patients in each group and the use of a ‘snapshot’ group for comparison. We also acknowledge that the 30-day mortality for hip fracture patients admitted to our unit is below the national average.35 However we believe that there remains a message from the findings of our study. Armed with the knowledge of those factors associated with early mortality i.e. advancing age, male gender and increasing comorbidities, we propose that these high-risk patients should be identified for early multidisciplinary intervention so that the medical condition of these patients can be optimised and the surgical insult minimised. Senior anaesthetic, surgical and orthophysician input is essential given the poor physiological reserve of these patients and is the one of the key elements to improving outcomes. The published literature, whilst not conclusive, is highlighting medical and economic benefits of co-management and streamlined care pathways for patients with a hip fracture and may in time replace the traditional model of care for patients sustaining a hip fracture.
ACKNOWLEDGEMENTS
Dr. Mark McCann MRC/CSO Social and Public Health Sciences Unit, University of Glasgow for advice on statistical analysis.
Footnotes
Provenance: externally peer-reviewed.
UMJ is an open access publication of the Ulster Medical Society (http://www.ums.ac.uk).
REFERENCES
- 1.Johansen A, Wakeman R, Boulton C, Plant F, Roberts J, Williams A. National Hip Fracture Database. National report 2013. London: Royal College of Physician; 2013. Available from: https://www.nhfd.co.uk/20/hipfractureR.nsf/0/CA920122A244F2ED802579C900553993/$file/NHFD%20Report%202013.pdf. Last accessed May 2019. [Google Scholar]
- 2.White SM, Griffiths R. Projected incidence of proximal femoral fracture in England: a report from the NHS Hip Fracture Anaesthesia Network (HIPFAN) Injury. 2011;42(11):1230–3. doi: 10.1016/j.injury.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 3.Holt G, Smith R, Duncan K, Hutchison JD, Reid D. Changes in population demographics and the future incidence of hip fracture. Injury. 2009;40(7):722–6. doi: 10.1016/j.injury.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 4.Fisher AA, O’Brien ED, Davis MW. Trends in hip fracture epidemiology in Australia: possible impact of bisphosphonates and hormone replacement therapy. Bone. 2009;45(2):246–53. doi: 10.1016/j.bone.2009.04.244. [DOI] [PubMed] [Google Scholar]
- 5.Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):15739. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leslie WD, O’Donnell S, Jean S, Lagacé C, Walsh P, Bancej C, et al. Osteoporosis SurveillanceExpertWorking Group. Trends in hip fracture rates in Canada. JAMA. 2009;302(8):883–9. doi: 10.1001/jama.2009.1231. [DOI] [PubMed] [Google Scholar]
- 7.Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, et al. IOF CSA Working Group on Fracture Epidemiology. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011;22(5):1277–88. doi: 10.1007/s00198-011-1601-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tucker A, Donnelly KJ, McDonald S, Craig J, Foster AP, Acton JD. The changing face of fractures of the hip in Northern Ireland: a 15-year review. Bone Joint J. 2017;99B:1223–31. doi: 10.1302/0301-620X.99B9.BJJ-2016-1284.R1. [DOI] [PubMed] [Google Scholar]
- 9.NICE Clinical Guideline; 124. Hip fracture: management. London: National Institute for Health and Care Excellence; 2017. Available from: http://www.nice.org.uk/Guidance/CG124. Last accessed May 2019. [PubMed] [Google Scholar]
- 10.Boulton C, Bunning T, Burgon V, Cromwell D, Johansen A, Rai S. National Hip Fracture Database (NHFD): annual report 2015. London: Royal College of Physicians; 2015. Available from: http://www.nhfd.co.uk/nhfd/nhfd2015reportPR1.pdf. Last accessed May 2019. [Google Scholar]
- 11.Chatterton BD, Moores TS, Ahmad S, Cattell A, Roberts PJ. Cause of death and factors associated with early in-hospital mortality after hip fracture. Bone Joint J. 2015; 97B(2):246–51. doi: 10.1302/0301-620X.97B2.35248. [DOI] [PubMed] [Google Scholar]
- 12.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007; 22(3):465–75. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 13.Zuckerman JD. Hip fracture. N Eng J Med. 1996;334(23):1519–25. doi: 10.1056/NEJM199606063342307. [DOI] [PubMed] [Google Scholar]
- 14.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 15.Deyo RA, Cherkin DC, Cool MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992; 45(6);;613-9 doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 16.D’Hoore W, Sicotte C, Tilquin C. Risk adjustment in outcome assessment: the Charlson comorbidity index. Methods Inf Med. 1993;32(5):382–7 . [PubMed] [Google Scholar]
- 17.Poses RM, McClish DK, Smith WR, Bekes C, Scott WE. Prediction of survival of critically ill patients by admission comorbidity. J Clin Epidemiol. 1996; 49(7):743–7. doi: 10.1016/0895-4356(96)00021-2. [DOI] [PubMed] [Google Scholar]
- 18.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–51. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 19.Mundi S, Pindiprolu B, Simunovic N, Bhandari M. Similar mortality rates in hip fracture patients over the past 31years. Acta Orthop. 2014;85(1):54–9 . doi: 10.3109/17453674.2013.878831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fox HJ, Pooler J, Prothero D, Bannister GC. Factors affecting the outcome after proximal femoral fractures. Injury. 1994;25(5):297–300 . doi: 10.1016/0020-1383(94)90239-9. [DOI] [PubMed] [Google Scholar]
- 21.Boereboom FT, Raymakers JA, Duursma SA. Mortality and causes of death after hip fractures in The Netherlands. Neth J Med. 1992;41(12):4–10 . [PubMed] [Google Scholar]
- 22.Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331(7529):1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tarrant SM, Hardy BM, Byth PL, Brown TL, Attia J, Balogh ZJ. Preventable mortality in geriatric hip fracture inpatients. Bone Joint J Br. 2014;96B(9):1178–84. doi: 10.1302/0301-620X.96B9.32814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thomas CJ, Smith RP, Uzoigwe CE, Braybrooke JR. The weekend effect. Short-term mortality following admission with a hip fracture. Bone Joint J Br. 2014;96B(3):373–8. doi: 10.1302/0301-620X.96B3.33118. [DOI] [PubMed] [Google Scholar]
- 25.Foss NB, Kehlet H. Short-term mortality in hip fracture patients admitted during weekends and holidays. Br J Anaesth. 2006;96(3):450–4. doi: 10.1093/bja/ael012. [DOI] [PubMed] [Google Scholar]
- 26.Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. Mortality risk after hip fracture. J Orthop Trauma. 2003;17(8 Suppl):S2–5. doi: 10.1097/00005131-200309001-00002. [DOI] [PubMed] [Google Scholar]
- 27.Donegan DJ, Gay N, Baldwin K, Morales EE, Esterhai JL, Jr, Mehta S. Use of medical co-morbidities to predict complications after hip fracture surgery in the elderly. J Bone Joint Surg Am. 2010;92A(4):807–13. doi: 10.2106/JBJS.I.00571. [DOI] [PubMed] [Google Scholar]
- 28.Menzies IB, Mendelson DA, Kates SL, Friedman SM. The impact of co-morbidity on perioperative outcomes of hip fractures in a geriatric fracture model. Geriatr Orthop Surg Rehabil. 2012;3(3):129–34. doi: 10.1177/2151458512463392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vidan M, Serra JA, Moreno C, Riquelme G, Ortiz J. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized controlled trial. J Am Geriatr Soc. 2005;53(9):1476– 82. doi: 10.1111/j.1532-5415.2005.53466.x. [DOI] [PubMed] [Google Scholar]
- 30.Swart E, Kates S, McGee S, Ayers DC. Current concepts review: The case for comanagement and care pathways for osteoporotic patients with a hip fracture. J Bone Joint Surg Am. 2018;100A(15):1343–50. doi: 10.2106/JBJS.17.01288. [DOI] [PubMed] [Google Scholar]
- 31.Grigoryan KV, Javedan H, Rudolph JL. Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma. 2014;28(3):e49–55. doi: 10.1097/BOT.0b013e3182a5a045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Prestmo A, Hagen G, Sletvold O, Helbostad JL, Thingstad P, Taraldsen K, et al. Comprehensive geriatric care for patients with hip fractures: a prospective, randomised controlled trial. Lancet. 2015;385(9978):162333. doi: 10.1016/S0140-6736(14)62409-0. [DOI] [PubMed] [Google Scholar]
- 33.Friedman SM, Mendelsohn DA, Bingham KW, Kates SL. Impact of a comanaged geriatric fracture centre on short-term hip fracture outcomes. Arch Intern Med. 2009;169(18):1712–7. doi: 10.1001/archinternmed.2009.321. [DOI] [PubMed] [Google Scholar]
- 34.Roy A, Heckman MG, Roy V. Associations between the hospitalist model of care and quality-of-care-related outcomes in patients undergoing hip fracture surgery. Mayo Clin Proc. 2006;81(1):28–31. doi: 10.4065/81.1.28. [DOI] [PubMed] [Google Scholar]
- 35.Boulton C, Bunning T, Johansen A, Judge A, Liddicoat M, Majrowski B. National Hip Fracture Database (NHFD): annual report 2017. London: Royal College of Physicians; 2017. Available from: https://www.nhfd.co.uk/files/2017ReportFiles/NHFD-AnnualReport2017.pdf. Last accessed May 2019. [Google Scholar]


