Abstract
Introduction
Patient portals are online electronic medical record applications that allow patients greater control of their own health and encourage meaningful interaction with their healthcare providers. The uptake of this technology is commonplace throughout developed healthcare economies and is on the Northern Ireland Electronic Healthcare Record (NIECR) roadmap.
Aim
To assess patients’ perceptions and proposed provision of a patient portal in endocrinology outpatients.
Methods
Patients (n=75) attending three endocrinology outpatient clinics were eligible to participate. After discussion at clinic, invited patients were contacted via e-mail to complete a confidential and anonymised online survey. There were a total of 23 questions in the survey which included a mix of free text and categorical responses. The survey duration was conducted over a 6-month period.
Results
The survey response rate was 51/75 (68%), M33:F18. 46/51 (90%) had access to smart phones, 45/51 (88%) used the internet daily. 31/51 (60%) of respondents were aged between 18-45, 20/51 (40%) were aged ≥ 45 years. 50/51 (98%) reported they would use the technology if available. 47/51 (92%) felt engaging with a patient portal would enhance communication with their doctor and improve understanding of their medical issues. Reported perceived applications of use included; remote access and advice for test results and medical questions, arranging appointments, requesting prescriptions and health promotion. 90% of respondents said they would be content to access results even if abnormal. Possible barriers to adoption of this technology included data protection and understanding medical terminology.
Conclusions
The overall response to the provision of this technology was positive, although concerns regarding data protection remain prevalent. Perceived benefits included enhanced doctor-patient communication, optimizing workflow and improving patient engagement.
Keywords: Northern Ireland Electronic Healthcare Record (NIECR), patient portal, communication, efficiencies
INTRODUCTION
Patient portals (PPs) are online healthcare applications that were introduced around 20 years ago mainly in the USA by large healthcare organisations (e.g. Epic - MyChart, Cerner-HealtheLife). They have gained widespread use over the last 10 years mirroring the adoption of social media and smartphone technology. PPs either link directly to electronic healthcare records (EHR) or are an extension of the platform to individuals; patients can log into their smartphone or computer to view secure online healthcare information.1 The overall purpose is to allow patients and healthcare providers to interact in a meaningful way and to deliver better outcomes. Patients have 24-hour access to healthcare information gaining greater control of their healthcare decisions.
In the primary care setting, PPs have been shown to enhance patient reported understanding of their condition with only a modest increase in physician workload.2 PPs may also facilitate improvements in chronic disease management. For example in diabetes, a small randomised controlled trial found a reduction in HbA1c and psychological distress in patients randomised to using a diabetes specific patient portal vs usual care.3
Portals can provide patients access to their healthcare information including medical diagnoses, laboratory results, and outpatient clinic letters. Further uses include secure messaging with their doctor, prescription requests, scheduling appointments, health promotion and educational information.
PPs can help facilitate patient-doctor communication and can encourage patient empowerment, this can be particularly useful if patients have chronic conditions and have regular testing and hospital visits/admissions. Potential drawbacks to the use of this technology are related to the challenge of “change”, including concerns regarding data security, access to technology and generating patient ‘buy in’. Some physicians are concerned by perceived lack of control or fear of overburdening patients with information; however, there are no validated studies confirming these concerns.
While used on a wide scale in US hospitals,4 PPs are now common practice in some settings within the NHS. A PP developed for patients living with chronic kidney disease in the UK now has over 6000 users and a similar system for patients with inflammatory bowel disease has been piloted.5
Within Northern Ireland there is no PPS that is universally accessible, however, the provision of a PP is on the NIECR roadmap and it is envisaged that it will become part of routine outpatient care. A pilot programme developing a patient and carer portal for patients with dementia and their families is underway. This will lead the way for a wider deployment within NIECR. At present, there is a paucity of region-specific data related to PPs. As such, we sought to examine the acceptability, attitudes and perceived barriers to a hypothetical patient portal system amongst patients attending endocrine outpatient appointments in three clinics in Northern Ireland.
METHODS
Questionnaire design
A questionnaire was designed using the online survey tool Survey Monkey (available at https:// www.surveymonkey.com). The survey used a combination of free-text responses and selection of pre-defined answers. The survey consisted of 23 questions in total. Six questions were designed to measure participant demographics and healthcare resource utilisation, three questions were intended to gauge access to technology and three questions were included to assess the most useful aspects of a hypothetical patient portal from a patient perspective. The remaining questions asked about perceived pros and cons of the PPS using a mixture of free-text and categorical responses.
Participant recruitment
Patients attending three endocrinology outpatient clinics at the Royal Victoria Hospital, Belfast City Hospital and Altnagelvin Hospital were eligible to participate. Patients were identified by their endocrine physician and informed of the study. After discussion at their clinic visit, invited patients were contacted via e-mail to complete a confidential and anonymised online survey. The survey duration was over six months between June to December 2017.
Data Analysis
All data are presented as a percentage of the total number of respondents. To summarise free-text responses a member of the study team reviewed all responses to each question and manually attributed each response to a theme. Bar graphs were prepared using Prism Version 7 (Graphpad, San Diego).
RESULTS
Participant Characteristics
In total 75 patients attending the adult endocrinology services participating in the study were deemed eligible for inclusion, 51 patients completed the survey (response rate = 68%). Participants were more likely to be female than male (65% F, Table 1), 57% were in full or part-time employment and 8% described themselves as retired. The age distribution was bimodal: 51% of participants aged between 18 and 34 years (18-24: 27%, 25-24: 24%, Table 1) with a second modal peak centred on the age range 45 - 64 years (45-54: 16%, 55-64: 18%, Table 1). The most common diagnosis amongst participants in our study was thyroid disease with 37% of participants describing a definitive diagnosis of thyroid disease or attending due to abnormal thyroid function tests. Importantly, 33% of participants had only attended the endocrine service once.
Table 1. Participant demographics *One participant described dual pathology and as such the total number of diagnoses is 52.
| n | % | |
|---|---|---|
| Sex | ||
| Male | 18 | 35 |
| Female | 33 | 65 |
| Age | ||
| 18 to 24 | 14 | 27 |
| 25 to 34 | 12 | 24 |
| 35 to 44 | 5 | 10 |
| 45 to 54 | 8 | 16 |
| 55 to 64 | 9 | 18 |
| 65 to 74 | 2 | 4 |
| 75 or older | 1 | 2 |
| Diagnosis* | ||
| Thyroid disease | 19 | 37 |
| Parathyroid disorder | 1 | 2 |
| Hyperprolactinaemia | 1 | 2 |
| Monitoring pubertal development | 1 | 2 |
| Adrenal nodule | 1 | 2 |
| Polycystic Ovarian Syndrome | 1 | 2 |
| Hypercalcaemia | 1 | 2 |
| Hypoandrogenism | 1 | 2 |
| Unknown | 26 | 51 |
| Frequency of endocrine clinic attendance | ||
| Once | 17 | 33 |
| Annual | 6 | 12 |
| Bi-annually | 12 | 24 |
| 3-4 monthly | 4 | 8 |
| more regularly | 2 | 4 |
| Unknown | 10 | 20 |
Accessing technological resources and access to patient portal
An important concern regarding any PPS is that it will widen inequality in healthcare along lines of income and age. Despite these concerns, 90% of participants in our survey had a smartphone which would have the capability of accessing any online patient portal (Fig. 1A). 82% or participants owned a laptop, 76% owned a tablet computer and 41% owned a desktop computer, 90% stated they accessed the internet daily (Fig. 1B). An important caveat to these findings is that those eligible were invited to participate via e-mail and therefore our findings likely overrepresent access to modern technology.
Fig 1. Patients attending an outpatient adult endocrinology service have the means to access an online PP Participants in our survey were asked (A): to describe which electronic devices they owned from a pre-defined list (B): to describe how often they used the internet, the free text answers were reviewed by a member of the research team and categorized as above (C): if they would or would not use the patient portal service (D): if they had previous knowledge of the service. All values are percentages of the total number of participants in the whole survey.
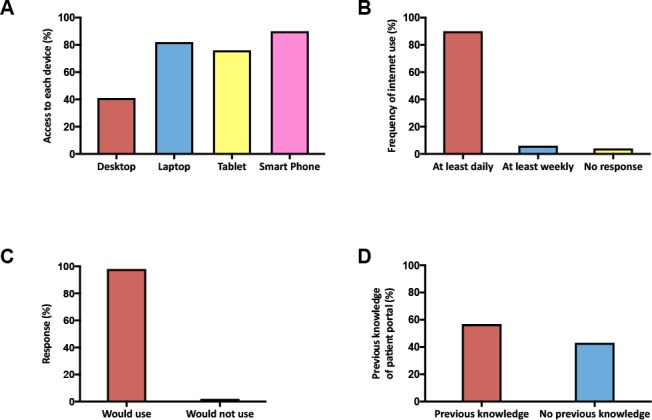
In keeping with the high rates of access to technology, all but one participant stated that they would use the PPS, this was despite the fact that 43% of participants had no previous knowledge of such a service as a means of communicating with their physician. Thus, within our sample a PPS is both accessible and acceptable to patients.
The ownership of Android and Apple smartphones was even in our cohort, this reiterates the need for a PPS that can be deployed on both operating systems. Similarly, the breadth of devices used by members of our cohort highlights that any future PPS should be browser-agnostic and adaptive to monitor, smartphone and tablet displays.
Perceived benefits of a patient portal service
To assess the most important aspects of a PPS from the patient perspective we asked participants which aspects of patient portal they found beneficial and requested that they select one answer from a pre-defined list. 63% of participants identified accessing their test results as the most important benefit. 12% selected the ability to get access to information about their condition as the most important benefit. 22% suggested that they would find the portal most useful to communicate with their physician, with 12% stating they would use the portal to communicate with their doctor about test results and 10% stating they would use the service to ask their doctor a medical question (Fig 2A). Only 4% of participants selected an option relating to management of appointments.
Fig 2. Positive perceptions of a patient portal service Participants in our survey were asked to pick which aspects of a patient portal service they would find beneficial (A). Participants were also given an opportunity to describe in their own words what the benefits of a PP were, these were reviewed by a member of the research team and categorized as above (B). Participants were also asked if they thought use of a patient portal service would improve their medical condition (C) and their patient experience (D). All values are reported as a percentage of the total number of participants.
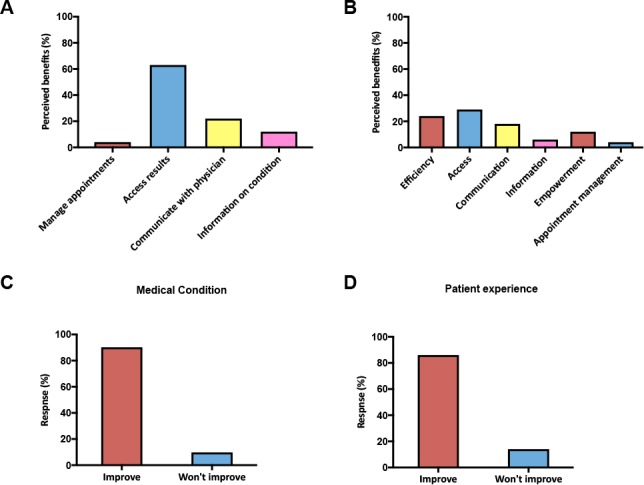
To empirically assess the benefits of a PPS entirely from a patient perspective we repeated this same question, this time allowing a free text response. The answers confirmed what was found using multiple choice questions with 30% of participants describing benefits in terms of enhanced access to test results and healthcare professionals and 18% describing improved communication (Fig 2B). In addition to these findings some novel themes emerged; 24 % described the perceived benefits in terms of increasing efficiency of the service they received and 12% identified patient empowerment as a benefit.
In keeping with a net benefit of a PPS 90% of participants stated that they believed a PPS would improve their patient experience (Fig. 2C) and 86% believed that engagement with the service would improve the healthcare of their medical condition. In summary, the participants in our study viewed the major benefits of patient portal as improved access to test results and enhanced communication with healthcare professionals and believed the patient portal would offer a net benefit to their healthcare and patient experience.
Assessing potential disadvantages of a patient portal service
A major limitation of any electronic medical record is concern around security. We specifically assessed this within our population by directly asking participants if permitting access to medical records via the internet raised concerns with respect to data protection, 51% did not think that the existence of a patient portal posed data protection concerns (Fig 3B).An additional concern that we considered was that accessing abnormal results remotely, without the support of a medical professional, may raise anxiety. Our survey robustly refutes this notion, 90% of respondents said they would be content to access abnormal results remotely (Fig 3C).
Fig 3. Potential disadvantages of a patient portal service Participants were asked to describe in their own words what the disadvantages of a PP were, these were reviewed by a member of the research team and categorized as above (A). Participants were asked if use of a PP raised concerns about data protection (B) or accessing abnormal results (C).
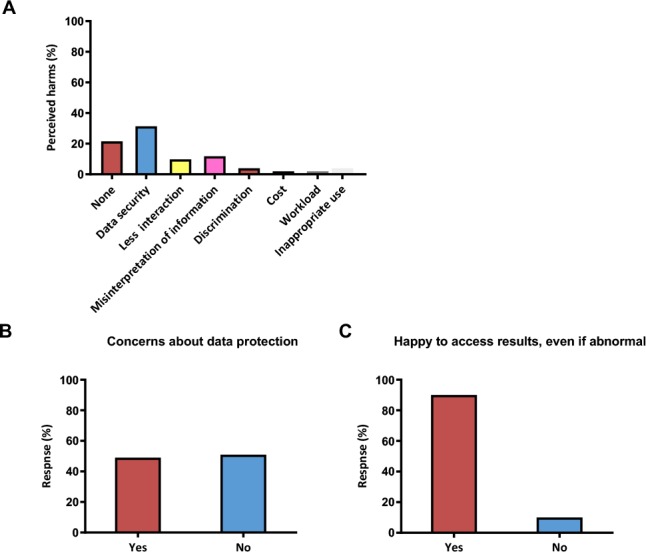
To assess patients’ perceived concerns more thoroughly we included a free text question that asked about potential drawbacks (Fig 3A). Over one fifth of respondents explicitly stated that they did not perceive any drawbacks. In keeping with our own pre-conceptions, 31% of participants had concerns about confidentiality and data security while 11% of participants’ answers raised issues regarding the ability of the general public to deal with medical information. Other concerns raised included risk of discrimination, cost and inappropriate use.
Perceived uses of a patient portal service
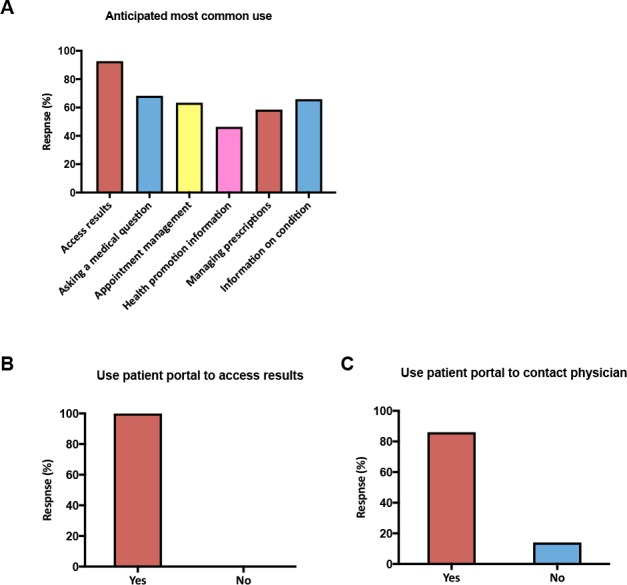
An important part of the development of any service, medical or otherwise, is that it is designed to meet the requirements of its users. To this end we asked participants what they envisioned they would use a PPS for most commonly and presented them with a list of potential services that we thought could be provided via patient portal technology. As can be seen in Figure 4 many respondents selected more than one option, however the most commonly selected response was to access test results. We also considered that patients would like to use the PP to communicate with their doctor. It is important to understand the potential uptake of such a service so that demand can be estimated and managed. 86% of respondents said that they would use the PP to communicate directly with their endocrine physician suggesting that facilitating access in this way would place a considerable demand on existing services and this would need to be considered as part of service delivery.
Fig 4. Anticipated uses of a patient portal service Participants asked to select, from a pre-defined list, what would they anticipate would be most likely to use PP for (A). Participants were also asked if they thought they would use a patient portal service to access their test results (B) and to contact their physician (C). All values are reported as a percentage of the total number of participants.
DISCUSSION
A key part of endocrine practice is management of chronic conditions. Engaging and empowering patients is a key part of this, but the chronicity and high prevalence of many of the diseases endocrinologists manage creates an ever-increasing burden on physician time. This may be lessened by implementation of patient portal systems, but concerns exist about their acceptability to patients. Here, we have demonstrated that perceptions of a PPS are overwhelmingly positive, patients think they would use a patient portal system and that some of the barriers that we as physicians perceive as issues may not be particularly obstructive to patients.
To our knowledge, this is the first study in Northern Ireland to examine the acceptability of a PPS to patients in the region. We found that the majority of patients thought they would use a patient portal if it became available. This is in keeping with findings from the OpenNotes study, 80% of patients opened a note recorded by their medical provider during the study period and 99% of patients continued to use the service after the study ended.2 In contrast, usage of a UK-wide electronic summary record has been disappointing, only 0.4% of patients were found to have opened the record in one study.6
Unexpected findings from our survey were that the majority of patients were happy to access abnormal results and that concerns regarding data protection, although common, were not as prevalent as we would have expected. In Sweden, pioneering efforts to establish an electronic health care record were initially hampered by Swedish physicians’ reticence to allow patients’ electronic access to their health care records, reportedly in part because of concerns re: data security and the ability to access abnormal results in the absence of a physician.6,7 Importantly, a qualitative study has provided evidence that these preconceptions were unfounded.8 While we did not formally assess physician opinion on a PPS the discrepancy in our personal expectations and the patient responses are consistent with the existing literature. Thus, our survey provides region-specific evidence that in the development of any PPS premium should be paid to what patients express their concerns are rather than what physicians perceive them to be. This empowering of patient decisions, encouraging delivery of care in a patient centric manner, is a pivotal part of the transformation agenda in Northern Ireland.
It should be noted that our study is limited by its cross-sectional nature and by the fact that patients were asked to evaluate a hypothetical patient portal without a concrete demonstration of what it might involve. In addition, selection bias is a key issue with respect to assessing acceptability and accessibility as respondents needed to have access to a computer or other electronic device capable of accessing the Internet by virtue of the fact that the survey was completed online.
These limitations notwithstanding, our findings have important implications for the development of a regional electronic medical record (Encompass) and beyond as we work to modernise healthcare within the region. Encompass provides us with an opportunity to reimagine how we provide healthcare in Northern Ireland and our work suggests that patients are ready for and welcome change. They want to use technology to access their own results and communicate with their physician in real time. Potential benefits of this include more efficient, stream-lined communication, less need for outpatient appointments and less strain on primary care colleagues as they try to absorb queries that are better directed to secondary care. One can also envision benefits that go beyond healthcare provision, less travelling to appointments in regionally disparate secondary and tertiary care facilities and less paper communication can reduce our organisation’s environmental footprint. However, challenges of this approach abound. Delivering healthcare in this way will require a gross restructuring of physician work-schedules. Training will need to be provided on how to use the Encompass platform and how to communicate sensitively and effectively via an electronic platform. Resistance to uptake by physicians will need to be managed. Delivery of this service will need to be combined with a stringent and effective quality assurance programme to ensure that the improvements we think this service can deliver are being realised and we must be ready to make rapid, iterative adaptations in response to this data. Perhaps the bottom-line message of our work is: patients are ready for a PPS, but are we?
In conclusion, we have found that a patient portal service is acceptable to patients attending endocrine clinics in Northern Ireland and is largely viewed in positive terms. Further studies will be needed to delineate the specific characteristics of a patient portal system that are welcomed by other groups of patients in Northern Ireland and to determine how introduction of PPs will affect the equitability of health care in the region.
The authors have no conflict of interest
Footnotes
Provenance: externally peer reviewed
Abbreviations: PP = Patient Portal, PPs = Patient Portals, PPS = Patient Portal Service
UMJ is an open access publication of the Ulster Medical Society (http://www.ums.ac.uk).
REFERENCES
- 1.Irizarry T, DeVito Dabbs A, Curran CR. Patient portals and patient engagement: a state of the science review. J Med Internet Res. 2015;17(6):e148. doi: 10.2196/jmir.4255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Delbanco T, Walker J, Bell SK, Darer JD, Elmore JG, Farag N, et al. Inviting patients to read their doctors’ notes: a quasi-experimental study and a look ahead. Ann Intern Med. 2012;157(7):461–70. doi: 10.7326/0003-4819-157-7-201210020-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fonda SJ, McMahon GT, Gomes HE, Hickson S, Conlin PR. Changes in diabetes distress related to participation in an internet-based diabetes care management program and glycemic control. J Diabetes Sci Technol. 2009;3(1):117–24. doi: 10.1177/193229680900300113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Halamka JD, Mandl KD, Tang PC. Early experiences with personal health records. J Am Med Inform Assoc. 2008;15(1):1–7. doi: 10.1197/jamia.M2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mclaughlin J, Stansfield C, Lal S, Bodger K, Robinson JA. OTU-031 My–IBD portal: progress and impact update. Gut. 2018;67(Suppl 1):A223. [Google Scholar]
- 6.Armstrong S. Patient access to health records: striving for the Swedish ideal. BMJ. 2017;357:j2069. doi: 10.1136/bmj.j2069. [DOI] [PubMed] [Google Scholar]
- 7.Scandurra I, Jansson A, Forsberg-Fransson M-L, Ålander T. Is ‘Patient’s Online Access to Health Records’ a Good Reform? – Opinions from Swedish Healthcare Professionals Differ. Procedia Comput Sci. 2015;64:964–8. [Google Scholar]
- 8.Rexhepi H, Åhlfeldt RM, Cajander Å, Huvila I. Cancer patients’ attitudes and experiences of online access to their electronic medical records: A qualitative study. Health Informatics J. 2018;24(2):115–24. doi: 10.1177/1460458216658778. [DOI] [PubMed] [Google Scholar]


