Abstract
Objective
This study aimed to assess the influence of a fused segment on cervical range of motion (ROM) and adjacent segmental kinematics and determine whether increasing number of fusion levels causes accelerated adjacent segment degeneration (ASD) after anterior cervical discectomy and fusion (ACDF).
Methods
A total of 165 patients treated with ACDF were recruited for assessment, and they were divided into 3 groups based on the number of fusion levels. Radiological measurements and clinical outcomes included visual analogue scale (VAS) and Neck Disability Index (NDI) assessed preoperatively and at ≥2 years of follow-up.
Results
ASD occurred in 41 of 165 patients who underwent ACDF (1-level, 12 of 78 [15.38%]; 2-level, 14 of 49 [28.57%]; 3-level, 15 of 38 [39.47%]; p=0.015) at final follow-up (mean, 31.9 months). Significant differences were found in reduction of global ROM based on the number of fusion levels (p<0.001). The upper adjacent segment ROM increased over time (p=0.004); however, lower segment ROM did not. Three-level ACDF did not obtain greater amounts of lordosis than did 1- or 2-level ACDF (p=0.003). Postoperative neck VAS scores and NDI were significantly higher for 3-level ACDF than for 1- or 2-level ACDF (p=0.033 and p=0.001).
Conclusion
ASD occurred predominantly in multilevel cervical fusion, more frequently in the upper segment of the prior fusion and as the number of fusion levels increased. Patients who underwent multilevel fusion had greater reduction of global ROM and increased compensatory motion at the upper adjacent segment. Three-level ACDF did not appear to restore cervical lordosis significantly compared with 1- or 2-level arthrodesis.
Keywords: Adjacent-segment degeneration, Anterior spinal fusion, Cervical degenerative disc disease, Multilevel spondylosis, Range of motion, Alignment
INTRODUCTION
Adjacent segment degeneration (ASD) has been defined as the development of new radiculopathy or myelopathy referable to a motion segment adjacent to the site of a previous anterior arthrodesis of the cervical spine [1]. ASD, which is often clinically silent initially, leads to the development of symptoms and often requires additional surgery at adjacent levels and longer follow-up [2].
Several biomechanical studies have documented a mechanism by which adjacent unfused levels compensate for the loss of cervical range of motion (ROM) in fused levels [3,4]. As the number of fused levels increases, unfused adjacent levels are under heavy pressure to increase changes in ROM [3,4]. A change of cervical ROM after spinal fusion may create pressure changes within adjacent discs and subsequent development of ASD [5]. These findings, associated with segmental instability and degeneration, have been supported in clinical studies [6]. In addition, increasing number of levels fused at the time of index surgery are reported to be correlated with increased rates of ASD [7]. Conversely, some authors insist that the number of fusion levels is not associated with the development of ASD and the need for reoperation [5]. These studies are not conclusive as to whether increased numbers of fusion levels cause accelerated degeneration at adjacent segments, whether loss of ROM at the fused levels could be compensated for by increases in unfused adjacent levels, and whether the alteration of cervical alignment following cervical surgery correlates with pain.
Therefore, we compared radiological ASD, cervical sagittal alignments and clinical outcomes in patients who underwent 1- and multilevel anterior cervical discectomy and fusion (ACDF) for treatment of cervical degenerative disease.
MATERIALS AND METHODS
1. Patient Population
The study protocols were approved by the Institutional Review Board of the Inje University Sanggye Paik Hospital (SGPAIK 2016-07-013-002). This was a retrospective cohort study. For this type of study, formal consent from each patient is not required; instead, ethical approval has been made by the regional ethics board. From February 2013 to March 2016, we treated 388 patients with ventral cord compression caused by cervical disc protrusion or bony spur. We excluded 141 patients with histories of prior cervical surgery, trauma, infection, neoplasm, or ossification of posterior longitudinal ligaments. Other exclusion criteria were (1) operative level, including C2–3 or C7–T1; (2) more than 4-level cervical degenerative diseases; (3) follow-up less than 24 months; and (4) preoperative ASD. We conducted this retrospective study with 165 patients who were treated surgically for 1-, 2-, or 3-level degenerative disc diseases. Of the 165 patients, 78 were diagnosed with single-level cervical degenerative diseases at C3–4 (9 patients), C4–5 (15 patients), C5–6 (36 patients), or C6–7 (18 patients). Forty-nine were diagnosed with 2-level cervical degenerative diseases at C3–4–5 (10 patients), C4–5–6 (11 patients), or C5–6–7 (28 patients). Thirty-eight were diagnosed with 3-level cervical degenerative diseases at C3–4–5–6 (13 patients), or C4–5–6–7 (25 patients). Indications for surgery included radiculopathy uncontrolled by nonsteroidal anti-inflammatory drugs or other pain relievers and neurological deficits such as motor weakness, cervical myelopathy, a combination of radiculopathy and myelopathy, or compatible magnetic resonance imaging (MRI) findings.
The study participants were divided into 3 groups based on the number of levels in the ACDF (Table 1).
Table 1.
Patient demographics
| Variable | 1-Level ACDF (n = 78) | 2-Level ACDF (n = 49) | 3-Level ACDF (n = 38) | p-value |
|---|---|---|---|---|
| Age (yr) | 53.10 ± 11.00 | 52.63 ± 9.67 | 56.55 ± 9.24 | 0.157 |
| Sex, male:female | 49:29 | 37:12 | 37:12 | 0.131 |
| BMI (kg/m2) | 24.20 ± 3.13 | 24.10 ± 2.79 | 25.45 ± 2.33 | 0.191 |
| Smoking (%) | 23.08 | 22.44 | 28.95 | 0.740 |
| Diabetes (%) | 16.67 | 16.33 | 21.05 | 0.703 |
| BMD (T-score) | -2.16 ± 0.96 | -1.89 ± 1.38 | -1.14 ± 1.32 | 0.081 |
| Follow-up (mo) | 33.28 ± 11.40 | 31.02 ± 7.15 | 30.18 ± 4.64 | 0.825 |
| Operation level | ||||
| C3/4 | 9 | - | - | |
| C4/5 | 15 | - | - | |
| C5/6 | 37 | - | - | |
| C6/7 | 17 | - | - | |
| C3/4/5 | - | 7 | - | |
| C4/5/6 | - | 11 | - | |
| C5/6/7 | - | 31 | - | |
| C3/4/5/6 | - | - | 13 | |
| C4/5/6/7 | - | - | 25 |
Values are presented as mean±standard deviation unless otherwise indicated.
ACDF, anterior cervical discectomy and fusion; BMI, body mass index; BMD, bone mineral density.
2. Surgical Technique
The operations were performed by an experienced spinal surgeon according to the procedure described by Smith and Robinson [8]. After completion of the disc excision, bony spurs or uncovertebral joints were removed with a curette or a high-speed drill under surgical microscopy. The endplate cartilage was also removed using a curette, carefully avoiding excessive bony endplate destruction. With the distraction applied, cervical cages (Cervios or Cornerstone cages) or autologous iliac bone grafts were inserted, ensuring that they did not extend too far posteriorly. A polyetheretherketone cage was filled with demineralized bone matrix (DBM, Grafton DBM fibers, Medtronic Sofamor-Danek, Memphis, TN, USA). The size of cages or iliac bone grafts was determined by intraoperative evaluation using a trial cage or gauge. We then placed anterior cervical plates (Atlantis anterior cervical plate system, Medtronic Sofamor-Danek). Anteroposterior and lateral radiographs or fluoroscopy were used to check and ensure the correct placement of cervical disc spacers or iliac bone grafts. All patients were kept immobilized in a Philadelphia neck collar for 6–8 weeks.
3. Radiologic Assessment
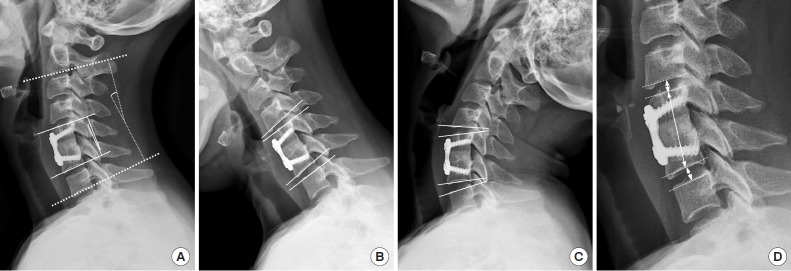
Radiologic examinations were performed immediately after operation, and then at 1, 3, 6, 12, and 24 months after surgery. The spinal alignment was assessed using anteroposterior and lateral (neutral, flexion, and extension) radiographs. The cervical global alignment was measured using the Cobb angle between the inferior endplate of the C2 vertebral body and the inferior endplate of the C7 vertebral body. Lordosis was expressed as a positive value and kyphosis was expressed as a negative value. ROM of the global cervical spine was determined as the difference between the lordotic and kyphotic angle in neck extension and flexion. The ROM of adjacent segments was measured according to a similar method. The regional alignment of fused segments was measured using the Cobb angle between the upper endplate and the lower endplate of a fused vertebral body (Fig. 1). The height of a fused segment was calculated as the distance between the midpoint of the upper margin of the upper vertebral body and the lower margin of the lower vertebral body on the appropriate surgical level. The height of the adjacent segment disc was measured as the distance between the midpoint of the inferior endplate of the upper vertebral body and the superior endplate of the lower vertebral body at the adjacent level. The upper segment disc height (UDH), lower segment disc height (LDH), upper adjacent segment ROM (USROM), and lower adjacent segment ROM (LSROM) were measured (Fig. 1).
Fig. 1.
Radiological measurements. (A) The C2–7 lordotic angle (Cobb angle between the inferior endplate of C2 and C7) and segmental angle (Cobb angle between the upper endplate and the lower endplate of fused vertebral body) were measured in neutral position. (B-C) Upper segment range of motion and lower segment range of motion were calculated in both flexion and extension position. (D) Fused segment height was calculated as the distance between the midpoint of the upper margin of the upper vertebral body and the lower margin of the lower vertebral body at the appropriate surgical level. Upper segment disc height and lower segment disc height were measured along the line passing through the center of the vertebral bodies.
We assessed the presence of ASD based on the modified Hilibrand criteria on radiography and computed tomography (CT) [1]. Radiographic ASD was determined by the presence of disc space narrowing >25%, new or enlarged osteophytes, anterior/posterior disc herniation, endplate sclerosis, and/or calcification of the anterior/posterior longitudinal ligaments as reported in previously published studies [9,10].
Fusion was defined as (1) grade 1 or 2 on the Bridwell fusion grading system [11]; (2) <2° movement; (3) <2-mm widening of interspinous distance on lateral flexion and extension views; (4) the presence of bridging trabecular bone between the endplates on anteroposterior and lateral views; or (5) the lack of implant failure signs of the anterior plate system, and less than 50% radiolucency in the perimeter surrounding the cage [8].
Spacer (cage or iliac bone graft) subsidence was defined as loss of more than 3 mm on fused segment height between immediately after the operation and final follow-up day [8]. Lumbar spine, trochanter, femoral neck, and hip bone mineral density (BMD) were measured using dual-energy X-ray absorptiometry in men and women >50 years of age.
4. Patient-Reported Clinical Outcomes
Patient-reported clinical outcomes were evaluated using visual analogue scale (VAS) of the neck and arm, and Neck Disability Index (NDI) using reviews of hospital chart and telephone questionnaires. All data including radiographs and clinical outcome were reviewed by an independent, experienced academic spine surgeon. All patients were followed-up for at least 2 years after surgery.
5. Statistical Analysis
All values were expressed as mean±standard deviations or percentages. The data were compared using the Student t-test and the chi-square test. If the data did not show a normal distribution, they were compared using the Mann-Whitney U-test or the Kruskal-Wallis test. Fisher exact test used to compare gender proportions between groups. Analysis of variance was used to assess the time-related changes in cervical spine alignment and ROM, VAS, and NDI. Pearson correlation analysis was used to analyze the relationship between the height of the fused segment, cervical segmental angle, and global alignment. We conducted all statistical analyses using MedCalc ver. 19.0.3 software (MedCalc, Mariakerke, Belgium). Values of p<0.05 were considered statistically significant.
RESULTS
A total of 165 patients who underwent ACDF with a minimum of 24-month follow-up were evaluated. The mean follow-up duration was 31.9±9.09 months (range, 25.0–59.2 months). Of the 165 patients, 78 underwent 1-level ACDF, 49 patients for 2-level ACDF, and 38 patients for 3-level ACDF. There were no significant differences with respect to age (p=0.157). No differences were found for patient sex, diabetes, smoking, BMD, or body mass index. A summary of the demographics is presented in Table 1. Preoperative radiologic parameters did not differ significantly among the 3 groups (Table 2). The initial diagnosis was radiculopathy in 92 patients, myelopathy in 32 patients, and myeloradiculopathy in 41 patients.
Table 2.
Comparison of radiological outcome according to surgical levels
| Variable | 1-Level ACDF (n = 78) | 2-Level ACDF (n = 49) | 3-Level ACDF (n = 38) | p-value |
|---|---|---|---|---|
| C2–7 Cobb angle (°) | ||||
| Preoperative | 10.85 ± 10.28 | 8.70 ± 7.95 | 13.24 ± 7.99 | 0.074 |
| Postoperative 6 mo | 14.53 ± 9.24 | 15.25 ± 9.37 | 14.21 ± 7.35 | 0.849 |
| Postoperative 6-mo change (Δ) | 3.68 ± 9.62 | 6.92 ± 10.02 | 0.97 ± 5.68 | 0.010* |
| Postoperative 12 mo | 13.15 ± 9.79 | 13.95 ± 7.14 | 13.53 ± 7.42 | 0.875 |
| Postoperative 12-mo change (Δ) | 2.30 ± 7.78 | 5.26 ± 6.93 | 0.29 ± 6.56 | 0.006* |
| Postoperative 24 mo | 13.01 ± 9.05 | 14.32 ± 7.09 | 13.52 ± 7.42 | 0.678 |
| Postoperative 24-mo change (Δ) | 2.16 ± 7.80 | 5.62 ± 7.38 | 0.28 ± 6.50 | 0.003* |
| C2–7 ROM (°) | ||||
| Preoperative | 46.36 ± 13.55 | 45.16 ± 11.19 | 42.39 ± 10.40 | 0.260 |
| Postoperative 6 mo | 39.96 ± 11.38 | 33.11 ± 11.44 | 26.42 ± 13.69 | < 0.001* |
| Postoperative 6-mo change (Δ) | -6.41 ± 13.77 | -12.05 ± 15.19 | -15.97 ± 12.98 | 0.002* |
| Postoperative 12 mo | 44.08 ± 10.56 | 36.93 ± 9.79 | 26.02 ± 11.67 | < 0.001* |
| Postoperative 12-mo change (Δ) | -2.29 ± 13.74 | -8.22 ± 12.52 | -16.36 ± 13.40 | < 0.001* |
| Postoperative 24 mo | 43.60 ± 10.55 | 36.49 ± 9.20 | 24.76 ± 9.45 | < 0.001* |
| Postoperative 24-mo change (Δ) | -2.76 ± 14.15 | -8.67 ± 12.18 | -17.63 ± 13.26 | < 0.001* |
| Segmental angle (°) | ||||
| Preoperative | 1.45 ± 4.51 | 3.29 ± 6.66 | 8.32 ± 5.88 | < 0.001* |
| Postoperative 6 mo | 5.33 ± 3.84 | 7.38 ± 5.85 | 10.66 ± 6.34 | < 0.001* |
| Postoperative 6-mo change (Δ) | 3.89 ± 6.21 | 4.09 ± 8.52 | 2.33 ± 5.33 | 0.428 |
| Postoperative 12 mo | 3.41 ± 2.79 | 5.91 ± 5.93 | 9.38 ± 6.27 | < 0.001* |
| Postoperative 12-mo change (Δ) | 1.96 ± 4.16 | 2.62 ± 5.68 | 1.06 ± 4.81 | 0.325 |
| Postoperative 24 mo | 3.26 ± 2.78 | 6.17 ± 5.37 | 9.42 ± 6.11 | < 0.001* |
| Postoperative 24-mo change (Δ) | 1.76 ± 4.17 | 2.42 ± 5.67 | 0.86 ± 4.82 | 0.325 |
| Segmental height (mm) | ||||
| Preoperative | 37.25 ± 10.28 | 55.13 ± 5.66 | 75.59 ± 8.31 | < 0.001* |
| Postoperative 6 mo | 34.58 ± 6.12 | 54.23 ± 5.28 | 79.48 ± 9.32 | < 0.001* |
| Postoperative 6-mo change (Δ) | -2.67 ± 5.18 | -0.90 ± 2.54 | 3.89 ± 3.93 | < 0.001* |
| Postoperative 12 mo | 37.63 ± 4.56 | 56.34 ± 5.54 | 77.25 ± 7.98 | < 0.001* |
| Postoperative 12-mo change (Δ) | 0.38 ± 1.75 | 1.21 ± 2.47 | 1.66 ± 3.47 | 0.020* |
| Postoperative 24 mo | 36.93 ± 4.36 | 55.64 ± 5.23 | 76.55 ± 7.61 | < 0.001* |
| Postoperative 24-mo change (Δ) | -0.32 ± 1.75 | 0.51 ± 2.47 | 0.96 ± 3.47 | 0.020* |
| UDH (mm) | ||||
| Preoperative | 6.46 ± 1.02 | 6.50 ± 0.89 | 6.37 ± 0.71 | 0.809 |
| Postoperative 6 mo | 5.77 ± 0.88 | 5.80 ± 0.90 | 5.96 ± 0.93 | 0.545 |
| Postoperative 6-mo change (Δ) | -0.69 ± 0.63 | -0.70 ± 0.77 | -0.41 ± 0.62 | 0.077 |
| Postoperative 12 mo | 5.84 ± 0.91 | 5.81 ± 0.83 | 5.57 ± 0.91 | 0.281 |
| Postoperative 12-mo change (Δ) | -0.69 ± 1.04 | -0.69 ± 0.56 | -0.80 ± 0.87 | 0.786 |
| Postoperative 24 mo | 5.59 ± 0.82 | 5.57 ± 0.84 | 5.17 ± 0.87 | 0.032* |
| Postoperative 24-mo change (Δ) | -0.86 ± 0.67 | -0.93 ± 0.73 | -1.20 ± 0.89 | 0.070 |
| LDH (mm) | ||||
| Preoperative | 6.28 ± 0.96 | 6.25 ± 1.05 | 5.84 ± 1.19 | 0.089 |
| Postoperative 6 mo | 5.74 ± 0.97 | 5.74 ± 0.94 | 5.45 ± 1.12 | 0.305 |
| Postoperative 6-mo change (Δ) | -0.55 ± 0.72 | -0.51 ± 0.57 | -0.39 ± 0.43 | 0.435 |
| Postoperative 12 mo | 5.77 ± 0.84 | 5.47 ± 0.94 | 5.09 ± 1.09 | 0.001* |
| Postoperative 12-mo change (Δ) | -0.58 ± 0.99 | -0.78 ± 0.84 | -0.75 ± 0.44 | 0.392 |
| Postoperative 24 mo | 5.64 ± 0.74 | 5.44 ± 0.80 | 5.07 ± 1.06 | 0.004* |
| Postoperative 24-mo change (Δ) | -0.64 ± 0.54 | -0.81 ± 0.71 | -0.77 ± 0.51 | 0.251 |
| USROM (°) | ||||
| Preoperative | 13.56 ± 6.93 | 12.79 ± 6.06 | 10.77 ± 3.71 | 0.069 |
| Postoperative 6 mo | 17.11 ± 6.35 | 15.72 ± 6.53 | 13.19 ± 4.26 | 0.005* |
| Postoperative 6-mo change (Δ) | 3.56 ± 9.04 | 2.93 ± 9.45 | 2.43 ± 3.45 | 0.773 |
| Postoperative 12 mo | 16.54 ± 6.79 | 16.31 ± 5.87 | 17.71 ± 4.29 | 0.515 |
| Postoperative 12-mo change (Δ) | 2.98 ± 9.72 | 3.52 ± 7.25 | 6.95 ± 3.88 | 0.039* |
| Postoperative 24 mo | 16.91 ± 6.78 | 17.08 ± 5.62 | 19.37 ± 4.37 | 0.098 |
| Postoperative 24-mo change (Δ) | 3.36 ± 9.61 | 4.29 ± 7.46 | 8.60 ± 4.11 | 0.004* |
| LSROM (°) | ||||
| Preoperative | 13.37 ± 7.00 | 11.35 ± 6.86 | 11.70 ± 7.19 | 0.228 |
| Postoperative 6 mo | 14.07 ± 8.01 | 12.46 ± 6.67 | 11.03 ± 4.40 | 0.142 |
| Postoperative 6-mo change (Δ) | 0.69 ± 10.45 | 1.11 ± 9.82 | -0.67 ± 4.49 | 0.650 |
| Postoperative 12 mo | 13.95 ± 6.70 | 15.12 ± 6.73 | 13.96 ± 4.41 | 0.550 |
| Postoperative 12-mo change (Δ) | 0.58 ± 8.70 | 3.77 ± 8.29 | 2.26 ± 5.21 | 0.085 |
| Postoperative 24 mo | 14.29 ± 6.78 | 15.22 ± 6.11 | 14.24 ± 4.33 | 0.678 |
| Postoperative 24-mo change (Δ) | 0.92 ± 8.75 | 3.87 ± 8.29 | 2.54 ± 5.23 | 0.122 |
Values are presented as mean±standard deviation.
ACDF, anterior cervical discectomy and fusion; C2–7 SVA, C2–7 sagittal vertical axis; ROM, range of motion; UDH, upper segmental disc height; LDH, lower segmental disc height; USROM, upper segmental range of motion; LSROM, lower segmental range of motion.
p<0.05, statistically significant differences.
1. Radiological Outcomes
1) Adjacent segment degeneration
Overall, 41 patients had radiological ASD after anterior cervical fusion at final follow-up. Twelve of 78 patients (15.38%) underwent 1-level fusion, 14 of 49 patients (28.57%) underwent 2-level fusion, and 15 of 38 patients (39.47%) underwent 3-level fusion (p=0.015). The adjacent levels were located at C3/4 in 19 patients, C4/5 in 16 patients, C5/6 in 2 patients, and C6/7 in 4 patients. Radiological ASD occurred in the upper adjacent segment of the prior fusion in 30 patients, lower adjacent segment in 3 patients, and at both adjacent levels in 8 patients. The average onset time of radiological ASD was 29.30±12.12 months (range, 20–42.6 months) (1-level mean, 21.29±5.93 months; 2-level mean, 39.82±28.24 months; 3-level mean, 26.79±8.89 months; p=0.030).
2) Cervical lordosis
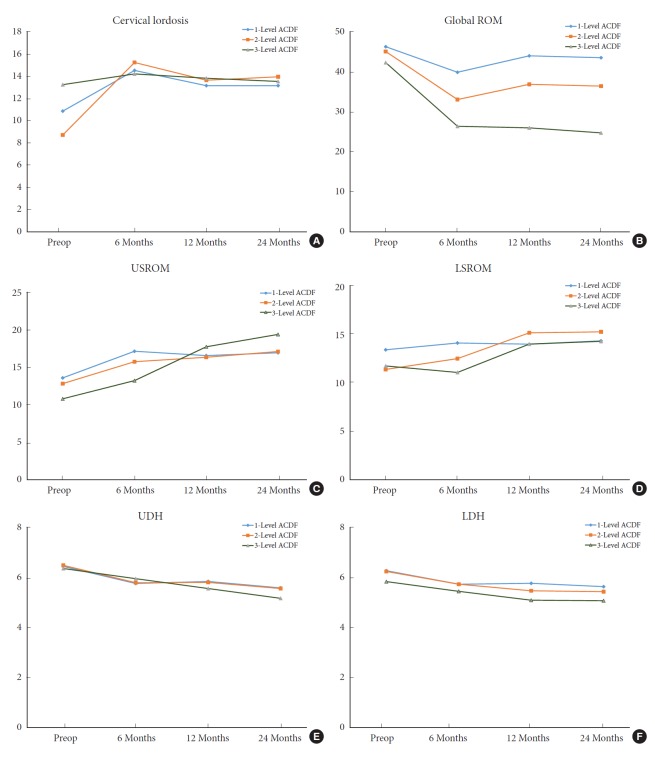
At 6 and 12 months postoperatively, and at the final follow-up, the changes in C2–7 lordotic angles were significantly different among the 3 groups. The increase of lordotic angle was greater for the 2-level ACDF group than for the 1-level or 3-level ACDF groups (Table 2). Patients who underwent 3-level ACDF had straighter cervical alignment than those who underwent 1- or 2-level ACDF (p=0.003) (Fig. 2).
Fig. 2.
Radiological kinematic graphs at time point of measurement. Line graphs illustrating the cervical lordosis (A), global range of motion (ROM; B), upper adjacent segment ROM (USROM; C), lower adjacent segment ROM (LSROM; D), upper adjacent disc height (UDH; E), lower adjacent disc height (LDH; F) for 1-, 2-, and 3-level anterior cervical discectomy and fusion (ACDF) groups preoperatively, and then at 6, 12, and 24 months after surgery. Preop, preoperative.
3) C2–7 global ROM
With respect to the cervical global ROM, patients who underwent one-level ACDF maintained neck motion better than did those who underwent 2-level or 3-level ACDF at final follow-up. Significant differences were found in the percentage of reduction of global ROM based on the number of fusion levels at 24-month follow-up, compared with preoperative global ROM (1-level, 98.5%; 2-level, 84.3%; 3-level, 62.8%; p<0.001) (Table 2, Fig. 2). The reduction of global ROM was mean -2.76°±14.15° in 1-level group, -8.67°±12.18° in the 2-level group, and -17.63°±13.26° in the 3-level group. These data suggest that the limitation of cervical motion was associated with the number of fusion levels.
4) Adjacent segment ROM
Patients with 3-level arthrodesis had greater ROM of the adjacent upper segment than did those with 1- or 2-level arthrodesis at final follow-up (Table 2), compared with preoperative ROM of the same adjacent segment (Fig. 2). At 6 months postoperatively, there were no differences in USROM among the 3 groups. However, USROM gradually increased in the 2- and 3-level arthrodesis groups over time (Table 2). With the passage of time, as the number of fusion levels increased, the USROM was greater than that of the preoperative period. On the other hand, the increase of LSROM showed no significant differences among the 3 groups over time (Table 2) (Fig. 2).
5) Adjacent segment disc height
UDH and LDH decreased in all 3 groups over time (Table 2). The UDH tended to decrease in the 3-level ACDF group at each follow-up visit and the LDH tended to decrease in the 2-level ACDF group; however, there were no significant differences (Fig. 2).
6) Fusion rate and subsidence
At the 6-month follow-up visit, fusion rates were 96.15% (75 of 78) in the 1-level ACDF group, 91.84% (45 of 49) in the 2-level fusion group, and 60.53% (23 of 38) in the 3-level fusion group. At the 12-month follow-up visit, fusion rates were 100% (78 of 78) in the 1-level ACDF group, 97.96% (48 of 49) in the 2-level fusion group, and 97.37% (37 of 38) in the 3-level fusion group (p=0.3911). At the final follow-up, subsidence was observed in 8 cases in the 1-level ACDF (10.25%), in 5 cases (10.20%) in the 2-level ACDF, and in 6 cases (15.79%) in the 3-level ACDF. However, these differences were not statistically significant (p=0.642).
2. Clinical Outcomes
1) Patient-reported outcomes
Preoperative neck and arm VAS scores did not differ significantly among the 3 groups. After cervical fusion, VAS scores for the neck and arm decreased significantly in the 3 groups. Pain intensity for the arm was not significantly different among the 3 groups at the final follow-up (Table 3). On the other hand, the neck VAS scores (1-level, 1.79±1.03; 2-level, 1.70±1.08; 3-level 2.34±1.42; p=0.033) and NDI scores (1-level, 7.17±1.87; 2-level, 8.37±3.52; 3-level, 9.08±3.27; p=0.001) (Table 3) were significantly higher in the 3-level ACDF group than in the 1- and 2-level ACDF groups.
Table 3.
Comparison of clinical outcome according to surgical levels
| Variable | 1-Level ACDF (n=78) | 2-Level ACDF (n=49) | 3-Level ACDF (n=38) | p-value |
|---|---|---|---|---|
| Neck VAS | ||||
| Preoperative | 5.44 ± 0.91 | 5.35 ± 1.42 | 4.95 ± 1.51 | 0.128 |
| Postoperative 6 mo | 2.01 ± 1.10 | 2.43 ± 1.26 | 2.95 ± 1.51 | < 0.001* |
| Postoperative 12 mo | 2.19 ± 1.07 | 2.20 ± 1.10 | 2.55 ± 1.61 | 0.291 |
| Postoperative 24 mo | 1.79 ± 1.03 | 1.70 ± 1.08 | 2.34 ± 1.42 | 0.033* |
| Arm VAS | ||||
| Preoperative | 6.03 ± 0.97 | 6.20 ± 1.10 | 5.84 ± 1.90 | 0.421 |
| Postoperative 6 mo | 2.04 ± 1.01 | 2.65 ± 1.93 | 3.29 ± 1.30 | < 0.001* |
| Postoperative 12 mo | 2.35 ± 0.58 | 2.43 ± 1.02 | 2.24 ± 1.13 | 0.595 |
| Postoperative 24 mo | 2.05 ± 0.56 | 2.12 ± 1.15 | 1.94 ± 1.11 | 0.196 |
| NDI | ||||
| Preoperative | 19.34 ± 2.52 | 20.43 ± 3.59 | 20.58 ± 4.02 | 0.082 |
| Postoperative 24 mo | 7.17 ± 1.87 | 8.37 ± 3.52 | 9.08 ± 3.27 | 0.001* |
Values are presented as mean±standard deviation.
ACDF, anterior cervical discectomy and fusion; VAS, visual analogue scale; NDI, Neck Disability Index.
p<0.05, statistically significant differences.
2) Reoperations
Among 41 patients who developed radiological ASD, 6 underwent additional anterior cervical fusion surgery (n=5) or posterior foraminotomy with discectomy (n=1) because of development of new radiculopathy or myelopathy (1-level [3 of 78, 3.85%]), 2-level [2 of 49, 4.08%], 3-level [1 of 38, 2.63%], p=0.9291). The other 35 patients experienced effective relief of their pain and disability and were closely followed-up. There were no cases of mechanical failure, including cage migration, or screw back-out during the follow-up period.
DISCUSSION
ACDF is commonly used as a surgical treatment for cervical myelopathy and radiculopathy resulting from cervical degenerative diseases [12-14]. An increase in the number of fused levels is likely to increase the complexity and risks of the surgery. The development of loss of cervical lordosis, graft subsidence, sagittal malalignment, and ASD are the common concerns associated with regard to multilevel ACDF [8]. In particular, adjacent level degeneration, often clinically silent initially, leads to the development of symptoms, necessitating additional surgery at adjacent levels and longer follow-up [2].
Adjacent degenerative changes include both radiographic ASD and symptomatic ASD. In a prospective 10-year follow-up MRI study, Matsumoto et al. [15] reported a significantly higher incidence of radiographic progression of ASD in ACDF patients; 2.9% of patients per year who had previously undergone ACDF also developed symptomatic ASD, including new radiculopathy and myelopathy [1]. Radiographic ASD develops into symptomatic ASD, leading to the neck or arm pain, or to neurological deficits requiring additional surgeries [1,16,17]. The overall rate of ASD ranged from 16% to 32% [1,18]. The prevalence of radiographic ASD, symptomatic ASD, and reoperation ASD varies according to reports. The prevalence of radiographic ASD after cervical surgery ranges from 4.74% to 28.28% [19,20]. The prevalence of symptomatic ASD ranges from 0% to 13.34% [21]. The prevalence of reoperation ASD ranges from 0% to 16.9% [5,19]. In the present study, overall radiographic ASD developed in 24.85% of patients after anterior cervical fusion at final follow-up (mean, 31.9 months). There was a significant difference in the incidence of radiological ASD at each fusion level (1-level [15.38%], 2-level [28.57%], 3-level [39.47%], p=0.0146). By contrast, the overall rate of reoperation was 3.64% (6 of 165), not significantly different at each fusion level (1-level [3.85%], 2-level [4.08%], 3-level [2.63%], p=0.825).
Biomechanical studies suggested that cervical arthrodesis influences the mechanical properties of intervertebral disc levels, including hypermobility and increased stresses next to a fused level [3]. Maiman et al. [4] demonstrated that increased internal stress and changes in load sharing occurred at the adjacent segments after fusion. Dang et al. [22] reported using a finite element model that mechanical load strain increasing in the adjacent segment is much higher after 2-level fusions than after 1-level fusions. Clinically, the number of fused segments affects the occurrence of ASD. Veeravagu et al. [7] reported that the incidence of revision surgery is 3.4%/yr for multilevel ACDF patients and 2.9%/yr for 1-level fusions. Increasing number of fused levels correlated with increasing incidences of reoperation [7]. By contrast, ASD is less common after multilevel fusion surgery because multilevel fusions usually include higher-risk levels, including C5–6 and/or C6–7 and have an end adjacent to segments that are at lower risk for the development of new degeneration [23]. Maldonado et al. [23] showed that the increased stresses on the adjacent discs associated with the increased number of fused segments did not lead to ASD. Ishihara et al. [24] reported lower rates of clinically significant ASD in patients undergoing multilevel cervical arthrodesis. Furthermore, some studies have reported that the number of arthrodesis segments is not a significant risk factor for ASD [24]. In the present study, patients with 3-level arthrodesis had a higher incidence of radiologic ASD than did those with 1- or 2-level arthrodesis. Although the patients who underwent 4-level anterior fusion were excluded to prevent a protective effect of multilevel arthrodesis, the rate of reoperation was not significantly different in the 3 groups based on the number of fused segments. These results may be attributed to the fact that this study included a relatively small number of patients and had a relatively short follow-up period (mean, 31.9 months). A future study performed prospectively with a larger number of patients with a longer follow-up period will be required to settle the argument for a protective effect of multilevel arthrodesis.
1. Location of ASD Development
In the present study, ASD above the fused segments was more common than was degeneration below the fused segments, consistent with results of previous studies [10]. Radiological ASD occurred in the upper segment adjacent to the prior fusion in 30 patients, the lower adjacent segment in 3 patients, and at both adjacent levels in 8 patients. Van Eck et al. [5] reported that intradiscal pressure (IDP) at the nucleus increased during flexion by 73.2% proximally and by 45.3% distally after C5–6 fusion. Wigfield et al. [25] reported a significant increase in IDP of the proximal adjacent level during flexion after anterior cervical arthrodesis. Komura et al. reported that ASD was more likely to occur at the C5–6 and C6–7 levels than at other levels [26]. The present study confirmed that adjacent segment disease occurs most commonly at C3–4 and C4–5 with lower incidence at C5–6 and C6–7 because previous fusions already included higher-risk levels, including C5–6 or C6–7.
2. Change of Adjacent Segment ROM and Disc Height
Some researchers reported that upper and LSROM increased after anterior fusion [10]. In agreement with the findings of a previous study [10], patients who underwent ACDF in the current study demonstrated that USROM and LSROM increased in the 3 groups over time. Patients who underwent 3-level ACDF showed a gradual increase in USROM over time and significant differences at final follow-up, compared with preoperative ROM. In addition, decreased adjacent disc height was observed in most of the upper and lower adjacent segments in all patients. The mean disc height change of the upper and lower adjacent segments tended to be greater in multilevel arthrodeses than in 1-level arthrodesis. Consequently, the excessive mobility above the fused segments increased with increasing fused levels and then the decrease of adjacent segment disc height followed. As the facets degenerate, translation of the adjacent segment may occur and may produce increased ROM [27]. Facet hypertrophy and thickening of the ligamentum flavum may precede disc collapse and disc herniation and may be the main cause of compression of neural elements [27].
3. Global Lordosis
Some researchers found that cervical lordosis after multilevel ACDF increased to a significantly greater extent than after 1-level ACDF [9,28]. However, in the present study, patients who underwent 3-level ACDF did not appear to regain cervical lordosis compared to 1-level arthrodesis. Cervical lordotic curvature remained straighter from preoperative to final follow-up after 3-level ACDF. Cervical lordosis after 1- or 2-level arthrodesis increased slightly from preoperatively to final follow-up. The explanation for this result is as follows: First, the improvement of global lordosis may be explained by maintenance of better surgical position using the round neck roll in 1- or 2-level arthrodesis. With 3 or more level fusions, it is difficult to maintain lordotic alignment during surgery; Second, postoperative lordosis changes are likely lower because of the few remaining mobile segments after a 3-level arthrodesis; Third, all patients underwent ACDF with rigid plate augmentation. The anterior plate and screw system has a limited length and rigid motion even if the anterior cervical plate system provides immediate segmental stability, fixation strength, thereby increasing the fusion rate [29]. Taken together, these mechanisms explain the difficulty in achieving lordosis in 3-level arthrodesis.
4. Global ROM
In agreement with the results of previous studies [30,31], patients who underwent ACDF showed a significant reduction in global ROM at 6 months. By contrast, Landers et al. [31] reported a significant improvement in ROM after anterior cervical fusion surgeries, even in those with multilevel arthrodeses. In the present study, as the number of fused levels increased, global ROM decreased significantly. Although cervical global ROM in patients undergoing 1- and 2-level ACDF reduced at 6 months, patients undergoing 1- and 2-level ACDF regained their cervical ROM at 12 and 24 months. The intact adjacent segments physiologically compensate for the motion loss at the fused segment to maintain neck motion for daily activities [32]. However, this phenomenon was not observed in 3-level ACDF patients because of less compensatory motion resulting from more fused levels.
5. Clinical Outcomes
VAS scores and NDI in 3 groups improved at each time point after surgery. VAS scores for arm pain were comparable among the 3 groups at final follow-up. Interestingly, the current study indicated that, in 3-level arthrodesis patients, neck pain and disability levels were unfavorably observed rather than in 1- and 2-level arthrodesis patients. In other words, patients who underwent 3-level fusion perceived neck pain and neck disability. This finding may be explained by the multifactorial situation involving a combination of progression of degenerative changes in the adjacent segments and the disadvantages of multilevel arthrodesis, including limitation of neck motion and less lordosis restoration. All these have an adverse impact on patient-reported outcomes.
6. Fusion Rate and Subsidence
Previous studies reported fusion rates of 84.9%–100% for 1-level ACDF, 79.9%–95.9% for 2-level ACDF, and 65.0%–96.2% for 3-level ACDF [33,34]. Multilevel ACDF has shown greater risks of nonunion, revisions, and complications [7,33]. In the present study, we found that the fusion rates of multilevel ACDF were lower than that of single-level ACDF. Compared with previous studies [33,35], favorable fusion rates (1-level [100%], 2-level [97.96%], 3-level [97.37%]) were found at 12-month follow-up. The use of plate augmentation in all patients increased fusion rates. Plate and screw fixations are recommended to achieve solid bony fusion after ACDF, particularly with multilevel surgery [8,35]. The subsidence rates were not different among the 3 groups (1-level [10.25%], 2-level [10.20%], 3-level [15.79%]).
7. Limitations
The limitations of our study include the relatively small number of patients who were enrolled and the short follow-up period. Two-year follow-up is insufficient to document ASD; however, increased adjacent ROM change in patients undergoing multilevel fusions may lead to the development of ASD over time. A multicenter prospective study with extended follow-up may help accurately determine the prevalence of ASD. In the present study, plain radiographic images provided limited information on ASD. Recently, there have been several trials to assess ASD with MRI [2,15]. The utility of MRI in the detection of ASD was not assessed in this study. Further evaluations using CT and MRI are needed to confirm our findings.
8. Recommendations
In approaching surgical management decisions, it is important to understand that, in comparison with single-level fusion, multilevel fusion is associated with relatively higher rates of ASD, higher limitations of cervical motion, and lower fusion rates. Our data suggest that multilevel arthrodesis is disadvantageous with respect to progression of ASD, limitation of neck motion and lower lordosis restoration, all of which have an adverse impact on patient-reported outcomes. We showed that the radiological and clinical outcomes of patients who were treated with multilevel ACDF were different from those of patients treated with 1-level fusion. Based on the results, 2-level or less than 3-level arthrodesis obtains favorable radiological and clinical outcomes rather than 3-level or more than 3-level arthrodesis. Careful consideration of the radiological and clinical outcomes is recommended when performing anterior cervical fusions of 3 or more levels. Great effort has been devoted to preventing progressive deterioration of ASD, including the development of artificial disc replacements and hybrid surgical techniques (ACDF combined with arthroplasty) as opposed to 2-level ACDF.
CONCLUSION
Patients who underwent multilevel fusions demonstrated greater reduction of global ROM and increased compensatory motion at the upper adjacent segment. Patients with greater numbers of fused levels more frequently developed radiological ASD. Three-level ACDF did not appear to restore cervical lordosis better than 1- or 2-level arthrodesis. These data suggest that surgeries with 3 or more levels might cause substantial degeneration of upper adjacent segments, limitation of global ROM, and difficulty in regaining cervical lordotic curvature, as well as perceived neck pain and disability. These findings may assist surgical decision-making for more effective and safer treatment of multilevel cervical degenerative diseases.
Acknowledgments
This work was supported by the 2018 Inje University research grant. The author wishes to thank Hyun Kyung Park, PhD and Seung Hwan Baik, MD for their contributions in drafting the manuscript and revising it for important intellectual content.
Footnotes
The authors have nothing to disclose.
REFERENCES
- 1.Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 2004;4(6 Suppl):190S–194S. doi: 10.1016/j.spinee.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 2.Iseda T, Goya T, Nakano S, et al. Serial changes in signal intensities of the adjacent discs on T2-weighted sagittal images after surgical treatment of cervical spondylosis: anterior interbody fusion versus expansive laminoplasty. Acta Neurochir (Wien) 2001;143:707–10. doi: 10.1007/s007010170050. [DOI] [PubMed] [Google Scholar]
- 3.Park J, Shin JJ, Lim J. Biomechanical analysis of disc pressure and facet contact force after simulated two-level cervical surgeries (fusion and arthroplasty) and hybrid surgery. World Neurosurg. 2014;82:1388–93. doi: 10.1016/j.wneu.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 4.Maiman DJ, Kumaresan S, Yoganandan N, et al. Biomechanical effect of anterior cervical spine fusion on adjacent segments. Biomed Mater Eng. 1999;9:27–38. [PubMed] [Google Scholar]
- 5.van Eck CF, Regan C, Donaldson WF, et al. The revision rate and occurrence of adjacent segment disease after anterior cervical discectomy and fusion: a study of 672 consecutive patients. Spine (Phila Pa 1976) 2014;39:2143–7. doi: 10.1097/BRS.0000000000000636. [DOI] [PubMed] [Google Scholar]
- 6.Elsawaf A, Mastronardi L, Roperto R, et al. Effect of cervical dynamics on adjacent segment degeneration after anterior cervical fusion with cages. Neurosurg Rev. 2009;32:215–24. doi: 10.1007/s10143-008-0164-2. [DOI] [PubMed] [Google Scholar]
- 7.Veeravagu A, Cole T, Jiang B, Ratliff JK. Revision rates and complication incidence in single- and multilevel anterior cervical discectomy and fusion procedures: an administrative database study. Spine J. 2014;14:1125–31. doi: 10.1016/j.spinee.2013.07.474. [DOI] [PubMed] [Google Scholar]
- 8.Yu J, Ha Y, Shin JJ, et al. Influence of plate fixation on cervical height and alignment after one- or two-level anterior cervical discectomy and fusion. Br J Neurosurg. 2018;32:188–95. doi: 10.1080/02688697.2017.1394980. [DOI] [PubMed] [Google Scholar]
- 9.Basques BA, Louie PK, Mormol J, et al. Multi-versus single-level anterior cervical discectomy and fusion: comparing sagittal alignment, early adjacent segment degeneration, and clinical outcomes. Eur Spine J. 2018;27:2745–53. doi: 10.1007/s00586-018-5677-y. [DOI] [PubMed] [Google Scholar]
- 10.Ahn SS, Paik HK, Chin DK, et al. The fate of adjacent segments after anterior cervical discectomy and fusion: the influence of an anterior plate system. World Neurosurg. 2016;89:42–50. doi: 10.1016/j.wneu.2016.01.013. [DOI] [PubMed] [Google Scholar]
- 11.Bridwell KH, Lenke LG, McEnery KW, et al. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976) 1995;20:1410–8. [PubMed] [Google Scholar]
- 12.Chung HJ, Hur JW, Ryu KS, et al. Surgical outcomes of anterior cervical fusion using deminaralized bone matrix as stand-alone graft material: single arm, pilot study. Korean J Spine. 2016;13:114–9. doi: 10.14245/kjs.2016.13.3.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kwon OI, Son DW, Lee SW, et al. Comparison of radiologic outcomes of different methods in single-level anterior cervical discectomy and fusion. Korean J Spine. 2016;13:91–6. doi: 10.14245/kjs.2016.13.3.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Han SY, Kim HW, Lee CY, et al. Stand-alone cages for anterior cervical fusion: are there no problems? Korean J Spine. 2016;13:13–9. doi: 10.14245/kjs.2016.13.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matsumoto M, Okada E, Ichihara D, et al. Anterior cervical decompression and fusion accelerates adjacent segment degeneration: comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine (Phila Pa 1976) 2010;35:36–43. doi: 10.1097/BRS.0b013e3181b8a80d. [DOI] [PubMed] [Google Scholar]
- 16.Gore DR, Sepic SB. Anterior discectomy and fusion for painful cervical disc disease. A report of 50 patients with an average follow-up of 21 years. Spine (Phila Pa 1976) 1998;23:2047–51. doi: 10.1097/00007632-199810010-00002. [DOI] [PubMed] [Google Scholar]
- 17.Li J, Li Y, Kong F, et al. Adjacent segment degeneration after single-level anterior cervical decompression and fusion: disc space distraction and its impact on clinical outcomes. J Clin Neurosci. 2015;22:566–9. doi: 10.1016/j.jocn.2014.08.019. [DOI] [PubMed] [Google Scholar]
- 18.Yue WM, Brodner W, Highland TR. Long-term results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year radiologic and clinical follow-up study. Spine (Phila Pa 1976) 2005;30:2138–44. doi: 10.1097/01.brs.0000180479.63092.17. [DOI] [PubMed] [Google Scholar]
- 19.Zhang JT, Cao JM, Meng FT, et al. Cervical canal stenosis and adjacent segment degeneration after anterior cervical arthrodesis. Eur Spine J. 2015;24:1590–6. doi: 10.1007/s00586-015-3975-1. [DOI] [PubMed] [Google Scholar]
- 20.Song KJ, Choi BW, Jeon TS, et al. Adjacent segment degenerative disease: is it due to disease progression or a fusion-associated phenomenon? Comparison between segments adjacent to the fused and non-fused segments. Eur Spine J. 2011;20:1940–5. doi: 10.1007/s00586-011-1864-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shiban E, Gapon K, Wostrack M, et al. Clinical and radiological outcome after anterior cervical discectomy and fusion with stand-alone empty polyetheretherketone (PEEK) cages. Acta Neurochir (Wien) 2016;158:349–55. doi: 10.1007/s00701-015-2630-2. [DOI] [PubMed] [Google Scholar]
- 22.Dang AB, Hu SS, Tay BK. Biomechanics of the anterior longitudinal ligament during 8 g whiplash simulation following single- and contiguous two-level fusion: a finite element study. Spine (Phila Pa 1976) 2008;33:607–11. doi: 10.1097/BRS.0b013e318166e01d. [DOI] [PubMed] [Google Scholar]
- 23.Maldonado CV, Paz RD, Martin CB. Adjacent-level degeneration after cervical disc arthroplasty versus fusion. Eur Spine J. 2011;20 Suppl 3:403–7. doi: 10.1007/s00586-011-1916-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ishihara H, Kanamori M, Kawaguchi Y, et al. Adjacent segment disease after anterior cervical interbody fusion. Spine J. 2004;4:624–8. doi: 10.1016/j.spinee.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 25.Wigfield CC, Skrzypiec D, Jackowski A, et al. Internal stress distribution in cervical intervertebral discs: the influence of an artificial cervical joint and simulated anterior interbody fusion. J Spinal Disord Tech. 2003;16:441–9. doi: 10.1097/00024720-200310000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Komura S, Miyamoto K, Hosoe H, et al. Lower incidence of adjacent segment degeneration after anterior cervical fusion found with those fusing C5-6 and C6-7 than those leaving C5-6 or C6-7 as an adjacent level. J Spinal Disord Tech. 2012;25:23–9. doi: 10.1097/BSD.0b013e31820bb1f8. [DOI] [PubMed] [Google Scholar]
- 27.Aota Y, Kumano K, Hirabayashi S. Postfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord. 1995;8:464–73. [PubMed] [Google Scholar]
- 28.Gillis CC, Kaszuba MC, Traynelis VC. Cervical radiographic parameters in 1- and 2-level anterior cervical discectomy and fusion. J Neurosurg Spine. 2016;25:421–9. doi: 10.3171/2016.2.SPINE151056. [DOI] [PubMed] [Google Scholar]
- 29.Ouyang P, Lu T, He X, et al. Biomechanical comparison of integrated fixation cage versus anterior cervical plate and cage in anterior cervical corpectomy and fusion (ACCF): a finite element analysis. Med Sci Monit. 2019;25:1489–98. doi: 10.12659/MSM.913630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chien A, Lai DM, Wang SF, et al. Comparison of cervical kinematics, pain, and functional disability between single- and two-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2016;41:E915–22. doi: 10.1097/BRS.0000000000001502. [DOI] [PubMed] [Google Scholar]
- 31.Landers MR, Addis KA, Longhurst JK, et al. Anterior cervical decompression and fusion on neck range of motion, pain, and function: a prospective analysis. Spine J. 2013;13:1650–8. doi: 10.1016/j.spinee.2013.06.020. [DOI] [PubMed] [Google Scholar]
- 32.Schwab JS, Diangelo DJ, Foley KT. Motion compensation associated with single-level cervical fusion: where does the lost motion go? Spine (Phila Pa 1976) 2006;31:2439–48. doi: 10.1097/01.brs.0000239125.54761.23. [DOI] [PubMed] [Google Scholar]
- 33.Fraser JF, Härtl R. Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. J Neurosurg Spine. 2007;6:298–303. doi: 10.3171/spi.2007.6.4.2. [DOI] [PubMed] [Google Scholar]
- 34.Jagannathan J, Shaffrey CI, Oskouian RJ, et al. Radiographic and clinical outcomes following single-level anterior cervical discectomy and allograft fusion without plate placement or cervical collar. J Neurosurg Spine. 2008;8:420–8. doi: 10.3171/SPI/2008/8/5/420. [DOI] [PubMed] [Google Scholar]
- 35.Kaiser MG, Haid RW, Jr, Subach BR, et al. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery. 2002;50:229–36. doi: 10.1097/00006123-200202000-00001. [DOI] [PubMed] [Google Scholar]