Abstract
Background
Although Toxoplasma gondii infection in immune-competent individuals is usually asymptomatic or causes a mild flu-like illness, it may become severe and can occasionally be fatal in immune-compromised people, such as AIDS patients or pregnant women.
Method
Electronic English databases (Pubmed, Google Scholar, Science Direct, and Scopus), parasitology congresses, and theses of Ethiopian medical universities, were systematically searched (published or unpublished data). Full-length articles and abstracts were collected using keywords such as Toxoplasma gondii, Toxoplasmosis, pregnant women, HIV/AIDS, and Ethiopia.
Results
Analysis of seroprevalence estimates was pooled using a random effects meta-analysis. Seventeen studies were included in the present systematic review and meta-analysis. One of these studies reported seroprevalence of T. gondii in HIV/AIDS patients and pregnant women. In this review, a total of 4,030 individuals were included and analyzed. The pooled prevalence of T. gondii in this review was 81.00% (95% CI = 69.10–89.78). Sub-group analysis showed that 2,557 pregnant women were evaluated. In pregnant women, the pooled sero-prevalence was 71.2 (95% CI = [51.9%, 87.1%]. In HIV/AIDS patients, 1,473 individuals were evaluated and the pooled seroprevalence was 88.45 (95% CI = 80.87%–94.31%).
Conclusion
This systematic review and meta-analysis identified a high seroprevalence of Toxoplasma infection of 81% among immunocompromised patients. Scaling up prevention and control methods mainly strengthening educational efforts are necessary to avoid reactivation and to stop the spread of T. gondii infection.
1. Introduction
Toxoplasma gondii is one of the most prevalent obligate intracellular protozoan parasites of man and livestock [1–5]. Feline species are definitive hosts for Toxoplasma gondii and a wide range of animals serve as intermediate hosts. Globally, it is estimated that about one-third of the population is infected with T. gondii [3]. Although T. gondii infection in immune-competent individuals is usually asymptomatic or causes a mild flu-like illness [4], it may become severe and can occasionally be fatal in immune-compromised people, such as AIDS patients or pregnant women [2, 6]. Toxoplasma gondii infection in AIDS patients and pregnant women causes severe encephalitis, and neurologic diseases, and can affect the heart, liver, inner ears, and eyes (chorioretinitis) [2]. Infection with T. gondii during pregnancy can result in spontaneous abortion, still-birth, fetal death, neonatal death, or various congenital defects, such as hydrocephalus, central nervous system abnormalities, and chorioretinitis [7]. HIV infected individuals are at risk of acute toxoplasmosis due to reactivation of T. gondii. It also causes cervical lymphadenopathy or ocular disease in HIV infected immune competent individuals.
Humans get infections with T. gondii after ingesting raw or undercooked meat, by ingesting cat-shed oocysts via contaminated soil, food or water; or trans-placental transmission [3–5, 7].
Serological methods used for T. gondii diagnosis such as enzyme-linked immunesorbent assay (ELISA) and indirect immunofluorescence assay (IFA) are considered as gold standard for the detection of Toxoplasma-specific antibodies (IgG or IgM) [4].
In Ethiopia, human toxoplasmosis infection is a neglected disease [7]. The prevalence of T. gondii infection in Ethiopia has been reported in some populations; mainly in HIV infected individuals, pregnant women, child bearing age women, and in general population [4].
For appropriate diagnosis, treatment, and control of T. gondii infections, information about the seroprevalence of toxoplasmosis in different special populations is very important. So, this systematic review of the literature aimed to evaluate the sero-prevalence of T. gondii among pregnant women and HIV/AIDS patients in Ethiopia.
2. Methods
2.1. Literature Search and Data Extraction
Relevant literatures were searched on Pubmed, Pubmed central, Google scholar, science direct databases, Scopus, theses of Ethiopian medical universities, and Ethiopian journals such as Ethiopia journal of health development and proceedings of professional associations from May, 2018 to June, 2018. Full-length articles and abstracts were collected using keywords such as Toxoplasma gondii, Toxoplasmosis, pregnant women, HIV/AIDS, and Ethiopia. These key words were also used in combination using boolean operators. Overlapped articles found in more than one databases were excluded. Annual research conferences and preceding of Ethiopian medical laboratory association (EMLA), and Ethiopian public health laboratory associations' (EPHLAs) records were reviewed to identify relevant unpublished articles.
The reference lists of published studies included in this meta-analysis were searched for additional articles. Two authors independently reviewed all collected studies for eligibility and they extracted the required information based on the objective this meta-analysis.
2.2. Data Collection
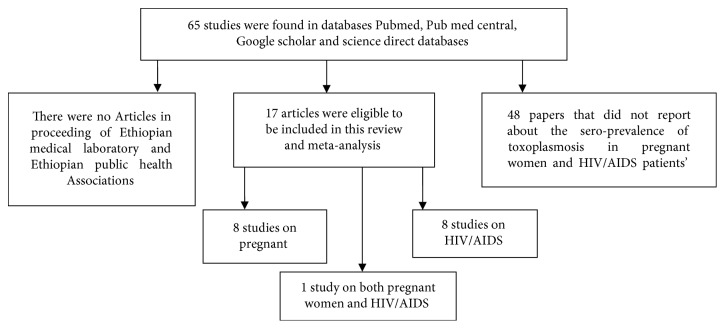
Pre-designed data extraction form was developed by authors based on the objective of this review. Studies conducted in Ethiopia to estimate the sero-prevalence of T. gondii infection in pregnant women and HIV/AIDS patients were included. All collected studies were assessed by two authors for eligibility to be included in this review. In case of disagreement on the eligibility of identified studies, authors held discussion to resolve the issue by considering the quality of identified study and the aim of the present review. Studies performed in study groups other than pregnant women, and HIV/AIDS and those studies that did not use random sampling methods as a sampling technique were excluded (Figure 1). Information about year of publication, first author, study area, study design, total sample size, number of sero-positive individuals, and laboratory methods used for T. gondii diagnoses was carefully investigated.
Figure 1.
Briefly shows the search process in this review article.
2.3. Statistical Analysis
Point estimates and 95% confidence intervals of seroprevalence of all included studies were calculated. An overall seroprevalence and group-specific sero-prevalences were calculated among HIV/AIDS patients and pregnant women. Heterogeneity among studies was visualized using a forest plot chart. The I2 and Cochran's Q tests were used to quantify the variations between studies. The heterogeneity was considered not significant when P > 0.1 and I2 < 50%. Due to the heterogeneity of studies included in this meta-analysis, random effect model was used by considering the included studies used random samples from a population. This meta-analysis was performed using the trial version of StatsDirect statistical software (https://statsdirect.com).
3. Results
Out of 65 studies from literature searches using key words, 17 studies were eligible and included in the present systematic review and meta-analysis. Eight studies described the sero-prevalence of T. gondii in pregnant women, whereas 8 studies reported T. gondii infection in HIV/AIDS patients. There was also one study which reported seroprevalence of T. gondii in HIV/AIDS patients and pregnant women. This study was considered in both pregnant women and HIV/AIDS patient groups during analysis. The study designs of all eligible and included studies were cross-sectional. In this review, Enzyme-linked immunosorbent assay (ELISA) and latex agglutination slide tests were the commonly used methods for the detection of T. gondii antibodies. The higher sero-prevalence of T. gondii (96.7% and 93.6%) was reported in HIV/AIDS patients from Mizan Aman Hospital and selected areas of Ethiopia, respectively. On the other hand the lower seroprevalence (18.5% and 34.9%) reported in this study was in pregnant women from Felege Hiwot Hospital from Jigjiga Hospital (Tables 1, 2 and 3).
Table 1.
The baseline characteristics of the studies included in this literature search.
| Author | Publication Year | Study area | Study group | No of cases | Total sample size | Sero-prevalence | Age range | Serologic test | Ref |
|---|---|---|---|---|---|---|---|---|---|
| Shimelis T. | 2009 | Addis Ababa | HIV/AIDS patients | 154 | 165 | 93.3% | 20–66 | ELISA | [8] |
| Zemene E. | 2012 | Jimma town | Pregnant women | 168 | 201 | 83.6% | 17–35 | ELISA | [3] |
| Walle F. | 2013 | Bahir Dar | HIV/AIDS patients | 101 | 103 | 87.4% | NA | ELISA | [9] |
| Alem H. | 2013 | Addis Ababa (Tikur Anbesa Hospital) | HIV/AIDS patients | 141 | 150 | 94.0% | NA | ELISA | [10] |
| Endris M. | 2013 | University of Gondar Hospital | HIV/AIDS patients | 130 | 170 | 76.5% | NA | LAT | [6] |
| Hailu A. | 2014 | Ethiopia selected areas | HIV/AIDS patients | 178 | 190 | 93.6% | NA | ELISA | [11] |
| Yohanes T. | 2014 | Arba Minch Hospital | HIV/AIDS patients | 150 | 170 | 88.2% | NA | ELISA | [12] |
| Hailu A. | 2014 | Ethiopia selected areas | Pregnant women | 256 | 293 | 87.3% | NA | ELISA | [11] |
| Endris M. | 2014 | University of Gondar Hospital | Pregnant women | 341 | 385 | 88.6% | NA | LAT | [6] |
| Gelaye W. | 2015 | Addis Ababa | Pregnant women | 246 | 288 | 85.4% | 18–42 | LAT | [4] |
| Awoke K. | 2015 | Felegehiwot Hospital, Bahir dar | Pregnant women | 71 | 384 | 18.5% | NA | LAT | [5] |
| Agmas B. | 2015 | Debre Tabor Hospital | Pregnant women | 180 | 263 | 68.4% | 18–44 | LAT | [1] |
| Mohammed K. | 2015 | Mettu Karl Hospital | HIV/AIDS patients | 72 | 120 | 60.0% | NA | LAT | [13] |
| Abamecha F. | 2016 | Mizan Aman Hospital | Pregnant women | 198 | 232 | 85.3% | NA | ELISA | [7] |
| Tegegne D. | 2016 | Agaro town | HIV/AIDS patients | 109 | 135 | 80.7% | NA | LAT | [14] |
| Negero J. | 2017 | Bonga Hospital | Pregnant women | 159 | 210 | 75.7% | 15–44 | LAT | [15] |
| Negussie A. | 2017 | Jigjiga Hospital | Pregnant women | 105 | 301 | 34.9% | NA | LAT | [2] |
| Jejaw A. | 2017 | Mizan Aman Hospital | HIV/AIDS patients | 261 | 270 | 96.7% | 18–49 | ELISA | [16] |
NA: not applicable.
Table 2.
Baseline characteristics of included studies (based on IgG assessment).
| Author | Publication year | Study area | Study group | No of cases | sample size | IgG cases | Sero-prevalence | Age range | Serologic test | Ref |
|---|---|---|---|---|---|---|---|---|---|---|
| Zemene E. | 2012 | Jimma town | Pregnant women | 168 | 201 | 163 | 97.0% | 17–35 | ELISA | [3] |
| Walle F. | 2013 | Bahir Dar | HIV/AIDS patients | 101 | 103 | 90 | 89.1% | NA | ELISA | [9] |
| Alem H. | 2013 | Addis Ababa Tikur Anbesa Hospital | HIV/AIDS patients | 141 | 150 | 141 | 100.0% | NA | ELISA | [10] |
| Hailu A. | 2014 | Ethiopia selected areas | Pregnant women | 256 | 293 | 247 | 96.5% | NA | ELISA | [11] |
| Endris M. | 2014 | University of Gondar Hospital | Pregnant women | 341 | 385 | 341 | 100.0% | NA | LAT | [6] |
| Hailu A. | 2014 | Ethiopia selected areas | HIV/AIDS patients | 178 | 190 | 172 | 96.6% | NA | ELISA | [11] |
| Abamecha F. | 2016 | Mizan Aman Hospital | Pregnant women | 198 | 232 | 191 | 96.5% | NA | ELISA | [7] |
| Jejaw A. | 2017 | Mizan Aman Hospital | HIV/AIDS patients | 261 | 270 | 255 | 97.7% | 18–49 | ELISA | [16] |
NA: not applicable.
Table 3.
Baseline characteristics of included studies (based on IgM assessment).
| Author | Publication year | Study area | Study group | No of cases | Sample size | IgM positive | Sero-prevalence | Age range | Serologic test | Ref |
|---|---|---|---|---|---|---|---|---|---|---|
| Zemene E. | 2012 | Jimma town | Pregnant women | 168 | 201 | 2 | 1.2 | 17–35 | ELISA | [3] |
| Walle F. | 2013 | Bahir dar | HIV/AIDS patients | 101 | 103 | 11 | 10.89 | NA | ELISA | [9] |
| Hailu A. | 2014 | Ethiopia selected areas | Pregnant women | 256 | 293 | 9 | 3.52 | NA | ELISA | [11] |
| Hailu A. | 2014 | Ethiopia selected areas | HIV/AIDS patients | 178 | 190 | 6 | 3.37 | NA | ELISA | [11] |
| Abamecha F. | 2016 | Mizan Aman Hospital | Pregnant women | 198 | 232 | 7 | 3.54 | NA | ELISA | [7] |
| Jejaw A. | 2017 | Mizan Aman Hospital | HIV/AIDS patients | 261 | 270 | 6 | 2.3 | 18–49 | ELISA | [16] |
NA: not applicable.
Detection of T. gondii IgG and IgM is one of the commonest serologic diagnoses. IgG detection indicates either past or present infection while the detection of IgM showed early infection of T. gondii. Based on IgG assessment, most of the current reviewed studies reported above 95% T. gondii IgG sero-prevalence. In general, the sero-prevalence of IgG is higher than IgM in pregnant women and HIV/AIDS patients (Tables 1 and 2).
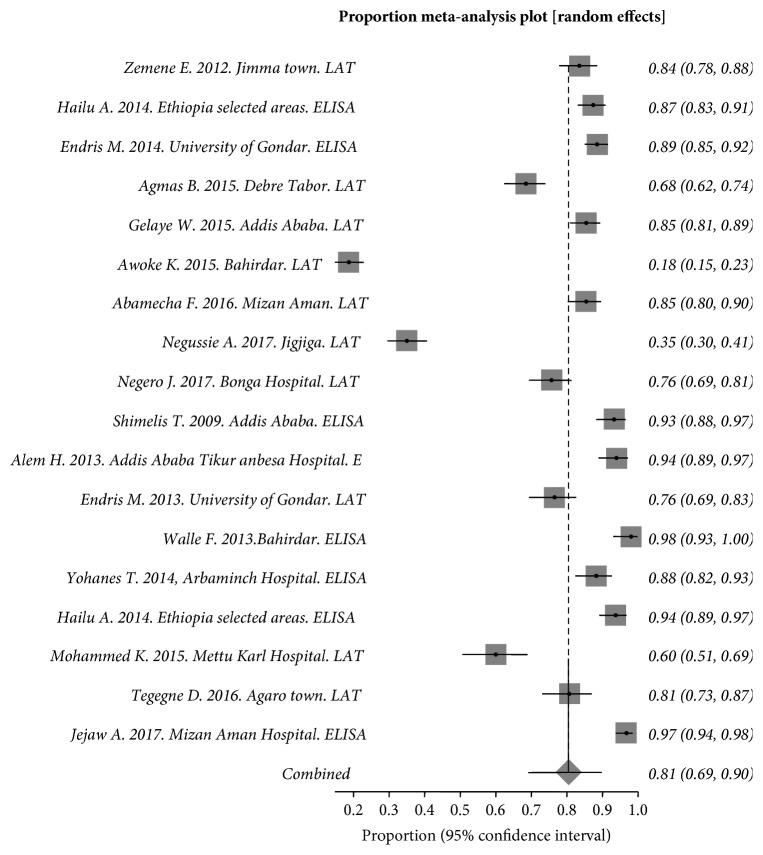
In general, in this review a total of 4,030 individuals were included and analyzed. The pooled prevalence of toxoplasmosis in this review was 81.00% (95% CI = 69.10–89.78). The Q statistic and I2 (inconsistency) were Cochran Q = 1,233.145293 (df = 17, P < 0.0001) and I2 (inconsistency) = 98.6% (95% CI = 98.5%–98.8%) (Figure 2). In this meta-analysis and systematic review, time interval sub-group analysis was performed to observe T. gondii sero-prevalence change from old studies to recent studies. Included studies from 2009 to 2017 were grouped in five years' interval. The pooled sero-prevalence of T. gondii from 2009 to 2013 was 90% (95% CI = 82%–96%) while it was 76% (95% CI = 61%–89%) in recent studies (2014–2017). Majority of the studies were conducted in recent years (2014–2017). Sub group analysis showed the sero-prevalence of T. gondi is decreased in recent years.
Figure 2.
Forest plot diagram of studies showing seropositivity to T. gondii in pregnant women and HIV/AIDS patients from Ethiopia.
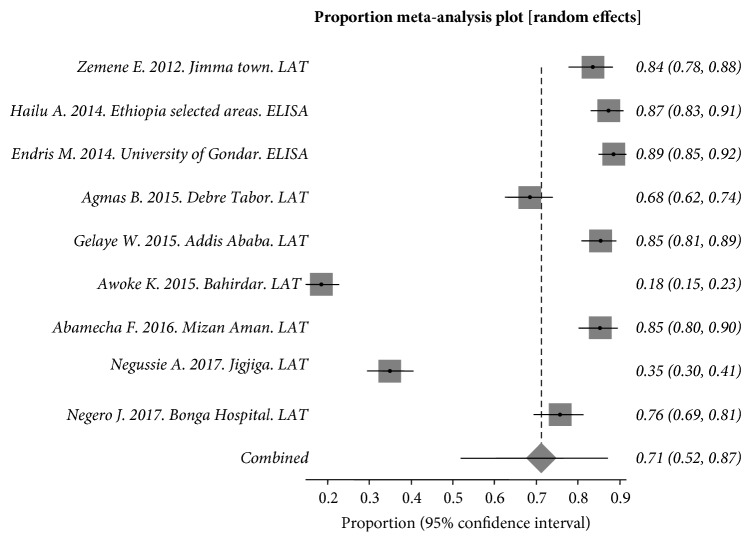
Sub-group analysis showed that 2,557 pregnant women were included and evaluated. Random effect analysis was used due to the heterogeneity between studies. The Q statistic and the pooled sero-prevalence were Cochran Q = 845.808548 (df = 8, P < 0.0001) and 71.2 (95% CI = [51.9%, 87.1%] respectively (Figure 3). I2 (inconsistency) = 99.1% (95% CI = [98.9%, 99.2%] (Figure 3).
Figure 3.
Forest plot diagram of studies showing seropositivity of T. gondii in pregnant women from Ethiopia.
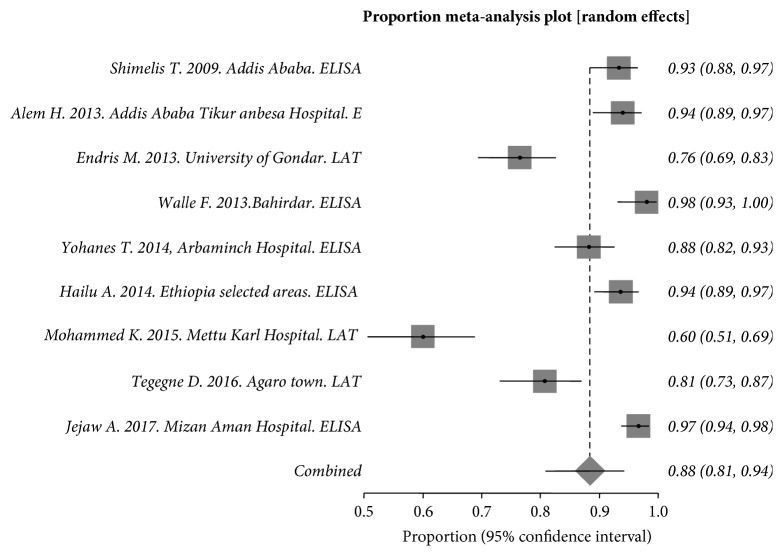
In HIV/AIDS patients, 1,473 individuals were included and evaluated. The Q statistic and the pooled seroprevalence were Cochran Q = 136.254836 (df = 8, P < 0.0001) and 88.45 (95% CI = 80.87%–94.31%) respectively. I2 (inconsistency) = 94.1% (95% CI = 91.5%–95.7%) (Figure 4).
Figure 4.
Forest plot diagram of studies showing seropositivity of T. gondii in HIV/AIDS patients from Ethiopia.
Begg and Egger tests were used for evaluating publication bias. Significant publication bias was not revealed in studies included about pregnant women (P-value >0.05). There was significant bias among studies included about HIV/AIDS patients (P-value >0.05).
4. Discussion
Toxoplasma gondii infection is usually asymptomatic in immune-competent individuals or causes a mild illness [4]. However, it may become severe and can occasionally be fatal in immune-compromised people, such as HIV/AIDS patients or pregnant women [2, 6].
This is the first systematic review and meta-analysis of toxoplasmosis in pregnant women and HIV/AIDS patients in Ethiopia. Among 2,557 pregnant women in Ethiopia, the sero-prevalence of T. gondii was 71.1%. Furthermore, the seroprevalence of T. gondii in 1,473 HIV/AIDS patients was 88.45%. Immune compromised patients are at high risk of toxoplasmosis reactivation [17]. The finding of this meta-analysis showed that the seroprevalence of T. gondii in pregnant women and HIV/AIDS patients was higher than 70%, and there is a risk of reactivation of T.gondii in this group of population. Toxoplasmosis is an opportunistic disease that can cause very severe illness and fatality in immune compromised individuals. Pregnant women and HIV/AIDS patients are immune deficient individuals. This immune inefficiency could be the main risk factor for the higher sero-prevalence of T. gondii.
Toxoplasmosis is mainly transmitted to human by ingestion of oocysts with contaminated food and drinks, by consumption raw or undercooked meat contain bradyzoites. It can also be transmitted during blood transfusion and organ transplantation.
Immunocompromised patients are highly vulnerable groups for toxoplasmosis infection due to debilitated immune system.
In Ethiopia, human toxoplasmosis infection is a neglected disease [7]. Some studies were conducted on the seroprevalence of toxoplasmosis. The study group of majority of the studies was on pregnant women, general population, and HIV/AIDS patients. Toxoplasmosis in this group of the population can have devastating consequences. For instance, congenitally transmitted toxoplasmosis in pregnant women can have serious disease in fetus including chorioretinitis and neurological complications. In HIV/AIDS patients beside the virus toxoplasmosis may play a role in immune suppression and fasten the onset of AIDS symptoms.
Serological tests are considered as the gold standard in the diagnosis of T. gondii infection. Due to some shortcomings in serologic tests and the variation of serologic methods used, the seroprevalence of T. gondii infection might be varied.
In Ethiopia, T. gondii seroprevalence studies in pregnant women and HIV/AIDS mainly used latex agglutination test and Enzyme linked immune sorbent assay (ELISA) methods for diagnosis. The highest prevalence of toxoplasmosis was observed in individuals diagnosed with ELISA. For instance, in HIV/AIDS patients, 96.70% sero-prevalence of T. gondii was observed using ELISA. The incidence and prevalence of T. gondii infection varies depending on geographic areas, weather conditions, and age groups in Ethiopia.In Ethiopia, a review studied on the sero-prevalence of T. gondii in general population revealed the overall pooled prevalence was 74.73% [18]. The seropositivity in pregnant women and HIV/AIDS patients in the present study was 71.1% and 88.45%, respectively. The seroprevalence in HIV/AIDS patients was higher than reported from general population and pregnant women sero-prevelence in the present study.
5. Conclusions
As far as we know and our literature search, this is the first systematic review and meta-analysis that provides information about the seroprevalence of T. gondii in pregnant women and HIV/AIDS patients in Ethiopia. Our finding indicates that researchers must give attention to the seroprevalence of toxoplasmosis in immunocompromised patients especially in HIV/AIDS patients, and pregnant women. Scaling up prevention and control methods and mainly strengthening educational efforts are necessary to avoid reactivation and to stop the spread of T. gondii infection.
Acknowledgments
The authors acknowledge Wollo University Medical Laboratory Science department staff. The authors also thank all their colleagues for their cooperation in the accomplishment of this study.
Abbreviations
- HIV:
Human immunodeficiency virus
- AIDS:
Acquired immunodeficent syndrome
- ELISA:
Enzyme linked immunosorbent assay
- LAT:
Latex agglutination test.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the manuscript.
Ethical Approval
After discussing the aim and the information required for this systematic review and meta-analysis, a letter of approval was obtained from the Department of Medical Laboratory Sciences Research Committee, College of Medicine and Health Science, Wollo University.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
DG, GZ, and AG were involved in proposal writing; they designed the study and participated in all implementation stages of the project. DGF and GZ also analyzed the data and finalized the write up of the manuscript. DGF, GZ, and AG were responsible for critically revising the proposal and the manuscript. All authors reviewed and approved the final manuscript.
References
- 1. Agmas B., Tesfaye R., Koye D. N. Seroprevalence of Toxoplasma gondii infection and associated risk factors among pregnant women in Debre Tabor, Northwest Ethiopia. BMC Research Notes. 2015;8(1) doi: 10.1186/s13104-015-1083-2.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Negussie A., Beyene E., Palani S. Toxoplasmosis and associated risk factors in antenatal clinic follow up Pregnant Women in Selected Health Institutes of Jigjiga, East Ethiopia. International Journal of Tropical Disease & Health. 2017;21(3):1–7. doi: 10.9734/ijtdh/2017/31177. [DOI] [Google Scholar]
- 3.Zemene E., Yewhalaw D., Abera S., Belay T., Samuel A., Zeynudin A. Seroprevalence of Toxoplasma gondii and associated risk factors among pregnant women in Jimma town, Southwestern Ethiopia. BMC Infectious Diseases. 2012;12(1) doi: 10.1186/1471-2334-12-337.337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gelaye W., Kebede T., Hailu A. High prevalence of anti-toxoplasma antibodies and absence of Toxoplasma gondii infection risk factors among pregnant women attending routine antenatal care in two hospitals of Addis Ababa Ethiopia. International Journal of Infectious Diseases. 2015;34:41–45. doi: 10.1016/j.ijid.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 5.Awoke K., Nibret E., Munshea A. Sero-prevalence and associated risk factors of Toxoplasma gondii infection among pregnant women attending antenatal care at Felege Hiwot Referral Hospital, Northwest Ethiopia. Asian Pacific Journal of Tropical Medicine. 2015;8(7):549–554. doi: 10.1016/j.apjtm.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 6.Endris M., Belyhun Y., Moges F., et al. Seroprevalence and associated risk factors of Toxoplasma gondii in pregnant women attending in Northwest Ethiopia. Iranian Journal of Parasitology. 2014;9(3):407–414. [PMC free article] [PubMed] [Google Scholar]
- 7.Abamecha F., Awel H. Seroprevalence and risk factors of Toxoplasma gondii infection in pregnant women following antenatal care at Mizan Aman General Hospital, Bench Maji Zone (BMZ), Ethiopia. BMC Infectious Diseases. 2016;16(1) doi: 10.1186/s12879-016-1806-6.460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shimelis T., Tebeje M., Tadesse E., Tegbaru B., Terefe A. Sero-prevalence of latent Toxoplasma gondii infection among HIV-infected and HIV-uninfected people in Addis Ababa, Ethiopia: a comparative cross-sectional study. BMC Research Notes. 2009;2(1):p. 213. doi: 10.1186/1756-0500-2-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walle F., Kebede N., Tsegaye A., Kassa T. Seroprevalence and risk factors for Toxoplasmosis in HIV infected and non-infected individuals in Bahir Dar, Northwest Ethiopia. Parasites & Vectors. 2013;6(1):p. 15. doi: 10.1186/1756-3305-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aleme H., Tilahun G., Fekade D., Berhe N., Medhin G. Sereoprevalence of immunoglobulin-G and of immunoglobulin-M anti-Toxoplasma gondii antibodies in human immunodeficiency virus infection/acquired immunodeficiency syndrome patients at Tikur Anbessa Specialized Hospital, Addis Ababa Ethiopia. Journal of Infectious Diseases and Therapy. 2013;1(4) doi: 10.4172/2332-0877.1000119. [DOI] [Google Scholar]
- 11.Hailu A., Negashe K., Tasew A., et al. Sero-prevalence, and associated risk factors of Toxoplasma gondii infection in pregnant women and HIV/AIDS patients in selected cities of Ethiopia. Banat’s Journal of Biotechnology. 2014;5(10):17–29. doi: 10.7904/2068-4738-V(10)-17. [DOI] [Google Scholar]
- 12.Yohanes T., Debalke S., Zemene E. Latent Toxoplasma gondii infection and associated risk factors among HIV-infected individuals at Arba Minch Hospital, South Ethiopia. AIDS Research and Treatment. 2014;2014:1–6. doi: 10.1155/2014/652941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohammed Yesuf K., Melese Z. T. Prevalence of toxoplasmosis in HIV/AIDS patients in Mettu Karl hospital. American Journal of Health Research. 2015;3(3):183–188. doi: 10.11648/j.ajhr.20150303.23. [DOI] [Google Scholar]
- 14.Tegegne D., Abdurahaman M., Mosissa T., Yohannes M. Anti-toxoplasma antibodies prevalence and associated risk factors among HIV patients. Asian Pacific Journal of Tropical Medicine. 2016;9(5):460–464. doi: 10.1016/j.apjtm.2016.03.034. [DOI] [PubMed] [Google Scholar]
- 15.Negero J., Yohannes M., Woldemichael K., Tegegne D. Seroprevalence and potential risk factors of T. gondii infection in pregnant women attending antenatal care at Bonga Hospital, Southwestern Ethiopia. International Journal of Infectious Diseases. 2017;57:44–49. doi: 10.1016/j.ijid.2017.01.013. [DOI] [PubMed] [Google Scholar]
- 16.Zeleke A. J., Melsew Y. A. Seroprevalence of Toxoplasma gondii and associated risk factors among HIV-infected women within reproductive age group at Mizan Aman General Hospital, Southwest Ethiopia: a cross sectional study. BMC Research Notes. 2017;10(1) doi: 10.1186/s13104-017-2390-6.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ahmadpour E., Daryani A., Sharif M., et al. Toxoplasmosis in immunocompromised patients in Iran: a systematic review and meta-analysis. The Journal of Infection in Developing Countries. 2014;8(12):1503–1510. doi: 10.3855/jidc.4796. [DOI] [PubMed] [Google Scholar]
- 18.Gebremedhin E. Z., Tadesse G. A meta-analysis of the prevalence of Toxoplasma gondii in animals and humans in Ethiopia. Parasites & Vectors. 2015;8(1) doi: 10.1186/s13071-015-0901-7.291 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the manuscript.