Abstract
Background
Holmium laser enucleation of the prostate (HoLEP) is considered the standard endoscopic treatment of benign prostatic hyperplasia (BPH), but traditional HoLEP surgery will cause some postoperative complications. This study was attempted to evaluate the safety and efficacy of modified two-lobe technique versus traditional three-lobe technique of HoLEP focusing mainly on incidences of retrograde ejaculation (RE) and urinary incontinence (UI).
Methods
From March 2014 to February 2017, 191 men with BPH were randomly assigned to two groups: 97 underwent modified two-lobe technique; 94 underwent traditional three-lobe technique. All patients were followed up for 12 months. Primary outcomes were incidences of RE and UI, and secondary outcomes were international prostate symptom score (IPSS), quality of life (QOL), maximal urine flowing rate (MFR), and residual urine among the studied patients.
Results
Compared with the traditional technique, patients in the modified group had a statistically significant decrease in frequency of UI (1.03% vs 8.51%, p=0.036) and RE in the 6th month (33.33% vs 63.64%, p=0.030) and 12th month (13.33% vs 50%, p=0.034) and a significant increase in ejaculatory volume in the 6th month (p=0.050) and 12th month (p=0.003). Besides, the modified HoLEP was more beneficial to patients according to the change of QoL score at 1 month (p=0.002), 3 months (p=0.004), 6 months (p=0.026), and 12 months (p=0.015).
Conclusions
The modified two-lobe technology of HoLEP reduced the incidence of RE and UI, which improved the quality of life of the patients after surgery compared to the traditional three-lobe technology. This trial is registered with ChiCTR1800018553.
1. Introduction
Benign prostatic hyperplasia (BPH) is a common medical condition in elderly men, and although it can be managed with medication, surgery remains the mainstay of treatment. Nowadays, many studies have demonstrated the advantages of HoLEP in resecting a larger amount of tissue compared to transurethral resection of the prostate (TURP) and photovaporization of the prostate (PVP) [1–3].
Nevertheless, long-term data indicated that enucleation could cause postoperative complications, including retrograde ejaculation (RE) and urinary incontinence (UI) [4, 5]. Shigemura et al. reported that among 497 patients who had been treated by 39 surgeons, the incidence of UI was >10% [6]. A recent study reported a 73.1% rate of RE following HoLEP [7]. Urologists thought that patients' RE or UI after HOLEP was probably because of an excessive damage to bladder neck and other normal tissue during surgery [8, 9]. We tried to introduce a set of modified techniques of HoLEP to reduce the incidences of RE and UI on the basis of anatomy and physiology [10, 11].
2. Methods
2.1. Study Design
Inclusion criteria were as follows: patients aged >50 years, refractory LUTS secondary to BPH, International Prostate Symptom Score (IPSS) of >15, maximum urinary flow rate (Qmax) of <15 ml/s or patients with acute urinary retention secondary to BPH, whose trial of voiding had failed, and prostate size on preoperative transrectal ultrasonography (TRUS) was 40–150 ml. Exclusion criteria included history of previous prostate or urethral surgery and voiding disorders not related to benign prostatic hyperplasia. If suspected, prostate carcinoma was ruled out by biopsy.
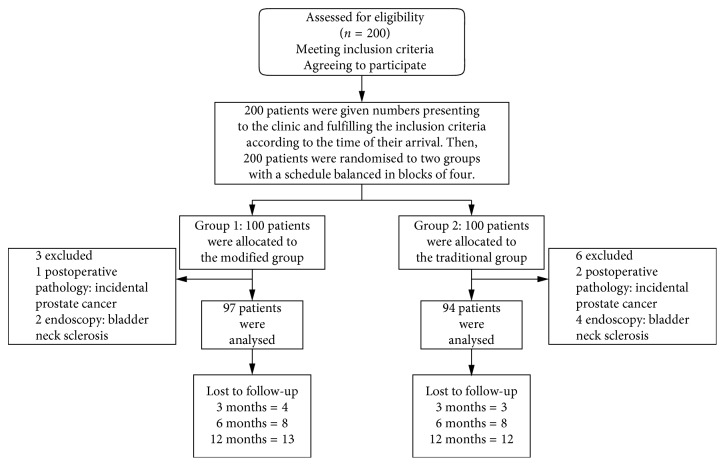
Two hundred patients who met the inclusion criteria with BPH were recruited from March 2014 to February 2017. Patients participating in the study were randomly divided into 2 groups (using consecutively numbered envelopes containing the treatment applied). In the course of the experiments, 3 and 6 patients were excluded in the modified and traditional groups, respectively (Figure 1). The patient's age, prostate volume, prostate-specific antigen (PSA), postvoid residual urine volume (PVR), Qmax, IPSS, Qol score, and International Index Of Erectile Function (IIEF) were recorded before operations. Perioperative outcomes, like operative time, transfusion rate, catheter duration, hospital stay, and drop in HGB levels were also collected. After surgery, follow-up was scheduled by the investigator who was blinded to the treatment grouping at 1, 3, 6, and 12 months. The follow-up protocol included checking for PVR, IPSS, QoL score, Qmax questionnaires, IIEF score, UI that was diagnosed by a thorough history and pad use, urinary retention, ejaculatory volume and RE that was evaluated by semen analysis, and postejaculatory urinalysis [12]. In case of a significant deterioration in the micturition parameters, further investigations were conducted and repeat surgeries were performed when indicated.
Figure 1.
Flow of participants through the study.
2.2. Surgical Procedures
All surgical procedures were performed under general anesthesia by a single surgeon with 8 years of experience in HoLEP, who have performed 500 HoLEP procedures. Holmium: YAG laser (fiber size 550 μm; Versa Pulse Select, Coherent Corp., Palo Alto, Calif.) with a power setting of 2 J/40–50 Hz and a 26-F Olympus continuous fluid irrigation resectoscope with 0.9% saline as the irrigation fluid were used for HoLEP. At the end of the surgery, a 20-F three-way catheter was inserted and retained in situ until the urine was clear.
2.2.1. Traditional HoLEP
HoLEP was performed as per the procedure previously mentioned by Tan and Gilling [13].
Step 1 (enucleation of the lobes). —
Bilateral bladder neck incisions were made at the 5 and 7 o'clock positions, and the depth was increased until all the circular fibers had been divided. The incisions were extended downward just adjacent to the verumontanum. The distal ends of the bladder neck incisions were then joined just proximal to the verumontanum with a transverse incision, and the median lobe was dissected on the capsule in a retrograde fashion toward the bladder neck. Next, the lateral lobes were undermined on each side by extending the initial bladder neck incision laterally and circumferentially at the apex, working toward the 2 and 10 o'clock positions. The plane was developed from the apex toward the bladder neck. A bladder neck incision was also made at the 12 o'clock position, down to the capsule. A sweeping motion was used to continue the incision circumferentially, laterally, and distally, until the resectoscope could be partially withdrawn, and the upper and lower resection planes could be visualized and connected. Once each of the lateral lobes had been released from the bladder neck, hemostasis was performed with a defocused laser beam.
Step 2 (morcellation of the prostate fragments). —
A mechanical morcellator extracted the tissue using reciprocating blades and a high-powered suction inside the bladder. Fragments of the tissue passed through the suction tubing assisted by using a roller pump and were collected in a special sock that fitted over the end of the tubing.
2.2.2. Modified HoLEP
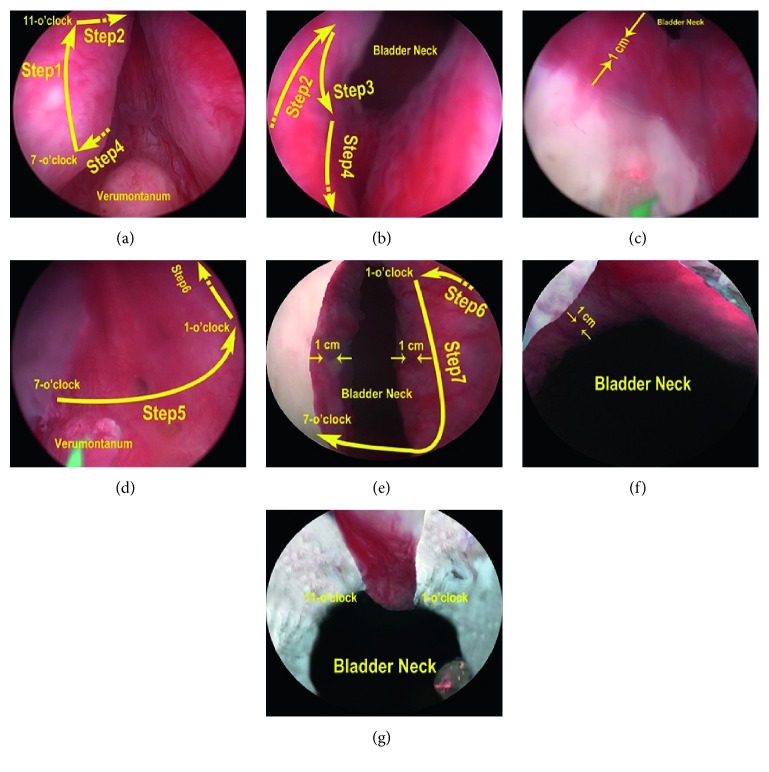
Step 3 (enucleation of the lobes). —
The first incision was made circumferentially extending from the 7 o'clock position to the 11 o'clock position near the verumontanum, and the depth was extended into the surface of the glands (Figure 2 Step 1). Subsequently, the incisions were lengthened down to the 11 o'clock position, approximately 1 cm from the bladder neck (Figure 2 Step 2). A sweeping motion was used to continue the incision to the 7 o'clock position proximal to the bladder neck, laterally (Figure 2 Step 3). After this, the incisions were joined at the 7 o'clock position near the verumontanum (Figure 2 Step 4). Following the incisions, the lateral lobe was thoroughly enucleated. Once the unilateral lobe had been released, more space was available for enucleating the remaining lobes.
Then, the incision was made, commencing from the previous 7 o'clock position proximal to the verumontanum toward 1 o'clock position, and the depth was extended into the surface of glands (Figure 2 Step 5). Subsequently, at the 1 o'clock position, approximately 1 cm from the bladder neck, the incisions were extended inward (Figure 2 Step 6). A sweeping motion was used to continue the incision to the previous 7 o'clock position proximal to the bladder neck, laterally (Figure 2 Step 7). Following the incisions, the remaining lobes were thoroughly enucleated.
Caution was required during the surgery to avoid damaging the mucosa of the bladder neck and part of the membranous urethra, as well as the circular fibers of the internal urethral sphincter (Figure 2(f)). The mucous membrane of the prostatic urethra from the 11 o'clock to 1 o'clock positions were preserved as much as possible (Figure 2(g)). Also, the edge of some glands mostly overtopped the verumontanum; hence, to enucleate these glands completely, the surgeon had to pry them up. Some oversized glands needed to be excised to half their size, to make it easier for them to pass through the bladder neck; some glands, whose edge extended beyond the neck of bladder, swelled toward inside the bladder so that the enucleation could be performed along the edge of these glands in order to protect circular fibers.
Figure 2.
Surgical procedures of modified two-lobe technique. (a) Step 1: incision is made circumferentially from the 7 o'clock position to the 11 o'clock position near the verumontanum. (a, b) Step 2: incision is lengthened down to 11 o'clock, approximately 1 cm from the bladder neck. (b) Step 3: Incision is made laterally to the 7 o'clock position near the bladder neck. (a, b) Step 4: incision is made back to the starting point. (c) Bladder neck after the unilateral lobe has been released. (d) Step 5: incision is made circumferentially from the 7 o'clock position to the 1 o'clock position near the verumontanum. (d, e) Step 6: incision is lengthened down to 1 o'clock, approximately 1 cm from the bladder neck. (e) Step 7: incision is made back to the 7 o'clock near the verumontanum. (f) Bladder neck after three lobes has been released. (g) The mucous membranes of the prostatic urethra from the 11 o'clock to 1 o'clock positions are preserved.
Step 4 (morcellation of the prostate fragments). —
Morcellation was performed as mentioned in Step 2 of Section 2.2.1. Before the end of the surgery, 20 mg of IV furosemide was routinely administered; then, a 22-F three-way Foley catheter was placed in the bladder and connected to a drainage bag.
2.3. Statistical Analysis
Continuous data were recorded as mean ± SD, if normally distributed, or as mean rank, if not normally distributed. Normally distributed data were analyzed with Student's t test, while the Wilcoxon rank sum test was used for data that were not normally distributed. Categorical data were compared with the chi-square test or Fisher's exact test (proportions). p values of <0.05 were considered statistically significant. Statistical analysis was performed using SPSS 23.0 for Windows (SPSS Inc, Chicago, Ill).
3. Results
As shown in Table 1, there were no statistically significant differences in the baseline characteristics between the two groups. IIEF scores were compared between the two groups among patients who had a sexual urge (30/97 in the modified group; 22/94 in the traditional group).
Table 1.
Preoperative patients' characteristics.
| Variables | Modified HoLEP | Traditional HoLEP | p value |
|---|---|---|---|
| Age (yr) | 70.3 ± 7.1 | 71.9 ± 8.0 | 0.145∗ |
| Prostate volume (cc) | 71.3 ± 10.9 | 72.0 ± 11.1 | 0.661∗ |
| PSA (ng/ml) | 3.2 ± 1.51 | 3.3 ± 1.50 | 0.647∗ |
| PVR (ml) | 126.2 ± 101.9 | 139.9 ± 70.8 | 0.283∗ |
| Q max (ml/s) | 7.0 ± 0.87 | 6.9 ± 0.91 | 0.438∗ |
| IPSS | 22.6 ± 2.02 | 22.2 ± 2.11 | 0.182∗ |
| QoL score | 4.7 ± 1.09 | 4.6 ± 1.07 | 0.523∗ |
| Indwelling catheter | 7.2% (7/97) | 7.4% (7/94) | 0.951‡ |
| IIEF | |||
| Erectile function | 13.4 ± 6.7 | 13.0 ± 6.7 | 0.832∗ |
| Orgasmic function | 6.6 ± 3.6 | 5.5 ± 2.7 | 0.233∗ |
| Intercourse satisfaction | 4.9 ± 2.7 | 6.8 ± 4.4 | 0.060∗ |
| Overall satisfaction | 5.5 ± 3.7 | 4.6 ± 5.2 | 0.469∗ |
HoLEP = holmium laser enucleation of the prostate; PSA = prostate-specific antigen; PVR = postvoid residual urine volume; Qmax = maximum flow rate; IPSS = International Prostate Symptom Score; QoL = quality of life; IIEF = International Index of Erectile Function; ∗t-test; ‡Pearson's chi-square test.
Preoperatively, there were no significant differences between the analyzed groups (Table 2).
Table 2.
Perioperative data.
| Variables | Modified HoLEP | Traditional HoLEP | p value |
|---|---|---|---|
| Operative time (min) | 72.1 ± 20.3 | 70.1 ± 22.7 | 0.521∗ |
| Enucleation time (min) | 50.1 ± 15.1 | 49.2 ± 13.9 | 0.669∗ |
| Morcellation time (min) | 15.6 ± 8.8 | 15.2 ± 8.3 | 0.747∗ |
| Transfusion rate, % | 0 | 0 | |
| Hospitalization (days) | 3.5 ± 1.22 | 3.6 ± 1.47 | 0.609∗ |
| Catheterization (days) | 2.7 ± 0.6 | 2.8 ± 0.8 | 0.329∗ |
| HGB levels drop (g/dl) | 1.7 ± 1.1 | 1.9 ± 1.4 | 0.273∗ |
∗ t-test.
Postoperative outcomes of the two groups are given in Table 3. Some patients discontinued postoperative assessments until 12 months of follow-up. After the surgery, obvious improvement of QoL score was observed in the modified group at 1, 3, 6, and 12 months, and this difference was found to be statistically significant. One month after the surgery, the change in maximum urinary flow rate (i.e., detrusor pressure) was significantly lower in the modified group than in the traditional group.
Table 3.
Patient outcome scores over time.
| Follow-up | 1 month | 3 months | 6 months | 12 months |
|---|---|---|---|---|
| No. of patients | ||||
| Modified | 97 | 93 | 89 | 84 |
| Traditional | 94 | 91 | 86 | 82 |
| PVR change (ml) | ||||
| Modified | −86.0 ± 57.1 | −92.4 ± 55.0 | −93.3 ± 49.6 | −97.1 ± 58.5 |
| Traditional | −102.0 ± 55.9 | −107.9 ± 56.2 | −108.6 ± 60.2 | −111.4 ± 42.6 |
| p value | 0.052∗ | 0.060∗ | 0.068∗ | 0.074∗ |
| IPSS score change | ||||
| Modified | −13.8 ± 3.07 | −15.8 ± 3.56 | −16.3 ± 2.76 | −16.6 ± 2.10 |
| Traditional | −13.7 ± 3.41 | −16.0 ± 3.29 | −16.4 ± 2.51 | −16.8 ± 2.83 |
| p value | 0.831∗ | 0.693∗ | 0.803∗ | 0.605∗ |
| QoL score change | ||||
| Modified | −2.2 ± 0.99 | −3.1 ± 0.63 | −3.2 ± 0.58 | −3.4 ± 0.52 |
| Traditional | −1.8 ± 0.76 | −2.8 ± 0.77 | −3.0 ± 0.60 | −3.2 ± 0.53 |
| p value | 0.002∗ | 0.004∗ | 0.026∗ | 0.015∗ |
| Q max change | ||||
| Modified | +15.3 ± 2.43 | +16.6 ± 2.88 | +17.4 ± 3.19 | +17.3 ± 3.28 |
| Traditional | +16.7 ± 4.12 | +17.4 ± 3.71 | +18.4 ± 4.23 | +18.1 ± 3.16 |
| p value | 0.005∗ | 0.428∗ | 0.079∗ | 0.163∗ |
| IIFF score change | ||||
| Modified | −1.3 ± 0.8 | +0.8 ± 0.4 | ||
| Traditional | −1.4 ± 0.9 | +0.7 ± 0.4 | ||
| p value | 0.146∗ | 0.109∗ |
PVR = postvoid residual urine volume; IPSS = International Prostate Symptom Score; QoL = quality of life; Qmax = maximum flow rate; IIEF = International Index of Erectile Function; ∗t-test.
Table 4 shows the early and late postoperative complications. Early postoperative complications (at 1-month follow-up) were seen in 10 patients: 2 from the modified group and 8 from the traditional group. Transient UI was more frequent significantly in the traditional group (p=0.036). RE was the most common complication, especially in the traditional group. Among patients who had a sexual urge, the occurrence rate of RE was 33.33% in the modified HoLEP group and 63.64% in the traditional HoLEP group (10/30 vs. 14/22; p=0.030) in the 6th month. In the 12th month, this difference still had statistical significance. Besides, the ejaculatory volume was more in the modified group (1.5 ± 1.0 vs 1.0 ± 0.7, p=0.050 for 6th month; 1.8 ± 0.6 vs 1.2 ± 0.8, p=0.003 for 12th month). The frequency of urinary retention, permanent urinary incontinence, and urethral stricture did not show significant differences between the two groups.
Table 4.
Incidence of late complications.
| Complication | Modified | Traditional | p value |
|---|---|---|---|
| Early postoperative complications | |||
| Transient urinary incontinence | 1.03% (1/97) | 8.51% (8/94) | 0.036† |
| Acute urinary retention | 1.03% (1/97) | 0 | 1.000† |
| Late postoperative complications | |||
| 6-month postoperative retrograde ejaculation | 33.33% (10/30) | 63.64% (14/22) | 0.030‡ |
| 6-month postoperative ejaculatory volume (ml) | 1.5 ± 1.0 | 1.0 ± 0.7 | 0.050∗ |
| 12-month postoperative urinary incontinence | 0 (0/84) | 2.38% (2/82) | 0.242§ |
| 12-month postoperative urethral stricture | 3.57% (3/84) | 1.21% (1/82) | 0.630† |
| 12-month postoperative retrograde ejaculation | 13.33% (4/30) | 50% (11/22) | 0.034‡ |
| 12-month postoperative ejaculatory volume (ml) | 1.8 ± 0.6 | 1.2 ± 0.8 | 0.003∗ |
| 12-month postoperative re-TURP | 0 (0/84) | 0 (0/82) | — |
BPH = benign prostatic hyperplasia; TURP = transurethral resection of the prostate; †continuity correction chi-square test; ‡Pearson's chi-square test; §Fisher's exact test; ∗t-test.
4. Discussion
In our modified HoLEP technique, the mucous membrane of the bladder neck, the circular fibers of the internal urethral sphincter, and the urethral membrane between the 11 and 1 o'clock positions were preserved. Retrograde passage of semen is prevented by reflex closure of the bladder neck [14], and contraction of this sphincter prevents retrograde movement of semen into the bladder during ejaculation [10, 15]. This bladder neck closure mechanism is the etiology of RE after transurethral surgery for BPH [16]. Also, a wide array of studies confirms that bladder neck preservation done improves early return of urinary continence [17–20]. The preprostatic part of the urethra is about 1 cm long, extends from the base of the bladder to the prostate, and is associated with a circular cuff of smooth muscle fibers (the internal urethral sphincter) [10, 21]. Additionally, research has shown that there is a fibromuscular tissue called anterior lobe, which contains less glandular tissue than others in the abdomen of the prostate urethra [11]. Moreover, selective preservation of partial epithelia in the anterior wall of the urinary tract increases epithelialization of the urinary tract after surgical trauma and thus minimizes irritation of the surgical wound by urine and reduces scar formation [22, 23]. Beyond that, in our view, the urethral membrane, which was not cut off between the 11 and 1 o'clock positions, maintained the shape of prostatic fossa and helped to speed prostate contractions. In the current study, selective transurethral resection of the prostate, preserving the urethral membrane between the 11 and 1 o'clock positions, offers a more effective and safer alternative to TURP for small volume BPH patients [24].
The results showed that the occurrence rates of RE and UI were low at 33.33% and 1.03% in the modified group, respectively. The change of QoL score was better in the modified group than in the traditional group at 1th, 3th, 6th, and 12th months after surgery. A large-scale multinational survey among approximately 14,000 men aged between 50 and 80 years, highlighted that the ejaculation function plays an important role in the QoL, even in aged men with symptomatic BPH [25]. Also, some articles reported that patients with RE had higher QoL scores [26–28] and agreed with our results. The change of maximum urinary flow rate was significantly lower in the modified group than in the traditional group. We think this is because the modified group preserved more detrusor tissue and urethral membrane than the traditional group, resulting in higher flow resistance. Although the decrease of the maximum urinary flow rate indicated the possibility of urethral stricture or obstruction, Qmax of two groups was still in the normal range. Besides, the frequency of postoperative urinary retention did not show significant differences between the two groups.
However, a recent study thought that bladder neck closure may not be important for maintaining antegrade ejaculation [7]. Kim et al. [7] listed two articles [29, 30], which have shown that retrograde ejaculation occurred in patients after retroperitoneal lymphadenectomy for testis tumor with a closed bladder neck. However, these two articles did not say RE would not occur when bladder neck was destroyed. Kim et al. also listed other three articles [31–33] in order to explain that patients could sustain orthostatic ejaculation after prostate sparing cystectomy and neobladder formation. However, there were some patients in all of these three articles who had retrograde ejaculation after surgery. In our opinion, when in the absence of comparison, we could not draw the conclusion that RE had no correction with the structure of bladder neck region. In our study, we selectively retained the mucous membrane of the bladder neck, the circular fibers of the internal urethral sphincter, and the urethral membrane between the 11 and 1 o'clock positions in the modified HOLEP group, but not in the traditional group. The results showed 33.33% rate of RE in the modified group, but 63.64% in the traditional group. It might be because of bladder neck closure mechanism and maintaining the shape of prostatic fossa.
Several studies have shown that HoLEP had a steeper learning curve than TURP, leading to hesitation to learn HoLEP among urologists. Placer et al. found that UI was seen in the early stages of the self-taught learning curve although the procedure remained effective [34]. Another study showed that an experience of more than 20 cases significantly helped a surgeon to decrease patients' post-HoLEP urinary incontinence [6]. Gong et al. [35] introduced a modified two-lobe enucleation technique of HoLEP that made work easier to perform and decreased operative time. In their study, the incidence of transient incontinence was 2% because of preserving the external sphincter. Recently, Miernik and Schoeb presented “3 horse shoe-like incision” HoLEP for bladder neck sparing which was easier to learn, but the incidence of postoperative UI and RE was not recorded and studied [36].
HoLEP continues to be a viable treatment option in BPH. Differences between surgical procedure designs may be factors that influence the therapeutic outcomes. Our study tried to introduce a new procedure for HoLEP to reduce the incidence of UI and RE. However, it had several limitations. Many patients discontinued the postoperative follow-ups, but the reasons for the dropouts were not investigated. It is possible that some of the dropouts developed severe complications, BPH recurrence, or sought treatment elsewhere. In addition, this study was a single-center study whose generalizability should be concerned. Next, it will be launched in the other institutions.
5. Conclusion
We found that the patients in the modified group suffered less postoperative urinary incontinence. Although UI had no significantly difference between two groups in the 12th month, there was a declining trend in the figures of UI in the modified group. Moreover, RE and ejaculatory volume had significant difference in the 6th and 12th months. In the clinic, we also found that the patients in the modified group recovered urinary control quickly, winning acclaim and decreasing contradiction between patients and doctors.
Acknowledgments
This study was funded by the Zhejiang Provincial Natural Science Foundation of China (LY16H160028) and National Natural Science Foundation of China Grant (NFSC 81202022).
Abbreviations
- BPH:
Benign prostatic hyperplasia
- LUTS:
Lower urinary tract symptoms
- HoLEP:
Holmium laser enucleation of the prostate
- TURP:
Transurethral resection of the prostate
- PVP:
Photovaporization of the prostate
- RE:
Retrograde ejaculation
- UI:
Urinary incontinence
- IPSS:
International Prostate Symptom Score
- TRUS:
Transrectal ultrasonography
- Qmax:
Maximum urinary flow rate
- PVR:
Postvoid residual urine volume
- QoL:
Quality of life
- IIEF:
International Index of Erectile Function.
Data Availability
The supplementary material contains the original data of this study.
Ethical Approval
This study had been approved by Human Ethics Review Committee of Zhejiang University Second Affiliated Hospital (I2018001198). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Authors' Contributions
Yichun Zheng was responsible for project administration. Congcong Xu wrote the original draft. Caixiu Lin and Zhen Xu were involved in visualization. Sheng Feng, Mingwei Sun, and Jijun Chen performed data curation.
Supplementary Materials
The supplementary file is the original data for the results of all patients. Sheet1: modified group. Sheet2: traditional group.
References
- 1.Moody J. A., Lingeman J. E. Holmium laser enucleation for prostate adenoma greater than 100 Gm: comparison to open prostatectomy. Journal of Urology. 2001;165(2):459–462. doi: 10.1097/00005392-200102000-00025. [DOI] [PubMed] [Google Scholar]
- 2.Ahyai S. A., Lehrich K., Kuntz R. M. Holmium laser enucleation versus transurethral resection of the prostate: 3-year follow-up results of a randomized clinical trial. European Urology. 2007;52(5):1456–1464. doi: 10.1016/j.eururo.2007.04.053. [DOI] [PubMed] [Google Scholar]
- 3.Tan A. H. H., Gilling P. J., Kennett K. M., Frampton C., Westenberg A. M., Fraundorfer M. R. A randomized trial comparing holmium laser enucleation of the prostate with transurethral resection of the prostate for the treatment of bladder outlet obstruction secondary to benign prostatic hyperplasia in large glands (40 to 200 grams) Journal of Urology. 2003;170(4):1270–1274. doi: 10.1097/01.ju.0000086948.55973.00. [DOI] [PubMed] [Google Scholar]
- 4.Li S., Zeng X. T., Ruan X. L., et al. Holmium laser enucleation versus transurethral resection in patients with benign prostate hyperplasia: an updated systematic review with meta-analysis and trial sequential analysis. PLoS One. 2014;9(7) doi: 10.1371/journal.pone.0101615.e101615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuntz R. M., Ahyai S., Lehrich K., Fayad A. Transurethral holmium laser enucleation of the prostate versus transurethral electrocautery resection of the prostate: a randomized prospective trial in 200 patients. Journal of Urology. 2004;172(3):1012–1016. doi: 10.1097/01.ju.0000136218.11998.9e. [DOI] [PubMed] [Google Scholar]
- 6.Shigemura K., Yamamichi F., Kitagawa K., et al. Does surgeon experience affect operative time, adverse events and continence outcomes in holmium laser enucleation of the prostate? A review of more than 1,000 cases. Journal of Urology. 2017;198(3):663–670. doi: 10.1016/j.juro.2017.04.087. [DOI] [PubMed] [Google Scholar]
- 7.Kim M., Song S. H., Ku J. H., Kim H.-J., Paick J.-S. Pilot study of the clinical efficacy of ejaculatory hood sparing technique for ejaculation preservation in Holmium laser enucleation of the prostate. International Journal of Impotence Research. 2015;27(1):20–24. doi: 10.1038/ijir.2014.22. [DOI] [PubMed] [Google Scholar]
- 8.Meng F., Gao B., Fu Q., et al. Change of sexual function in patients before and after Ho:YAG laser enucleation of the prostate. Journal of Andrology. 2006;28(2):259–261. doi: 10.2164/jandrol.106.000372. [DOI] [PubMed] [Google Scholar]
- 9.Nam J. K., Kim H. W., Lee D. H., Han J.-Y., Lee J. Z., Park S.-W. Risk factors for transient urinary incontinence after holmium laser enucleation of the prostate. The World Journal of Men’s Health. 2015;33(2):88–94. doi: 10.5534/wjmh.2015.33.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drake R. L. P. D., Vogl W., Mitchell A. W. M., Gray H. Gray’s Anatomy for Students. Philadelphia, PA, USA: Elsevier/Churchill Livingstone; 2005. [Google Scholar]
- 11.Sun Z., Na Y. Miniao Wake Linchuang Jiepo Xue. Jinan, China: Shandong Keji Chuban; 2010. [Google Scholar]
- 12.Shoshany O., Abhyankar N., Elyaguov J., Niederberger C. Efficacy of treatment with pseudoephedrine in men with retrograde ejaculation. Andrology. 2017;5(4):744–748. doi: 10.1111/andr.12361. [DOI] [PubMed] [Google Scholar]
- 13.Tan A. H. H., Gilling P. J. Holmium laser prostatectomy: current techniques. Urology. 2002;60(1):152–156. doi: 10.1016/s0090-4295(02)01648-5. [DOI] [PubMed] [Google Scholar]
- 14.Bonora M., Wieckowsk M. R., Chinopoulos C., et al. Erratum: molecular mechanisms of cell death: central implication of ATP synthase in mitochondrial permeability transition. Oncogene. 2015;34(12):p. 1608. doi: 10.1038/onc.2014.462. [DOI] [PubMed] [Google Scholar]
- 15.Learmonth J. R. A contribution to the neurophysiology of the urinary bladder in man. Brain. 1931;54(2):147–176. doi: 10.1093/brain/54.2.147. [DOI] [Google Scholar]
- 16.Terrone C., Castelli E., Aveta P., Cugudda A., Rocca Rossetti S. Iatrogenic ejaculation disorders and their prevention. Minerva Urologica e Nefrologica = The Italian journal of urology and nephrology. 2001;53(1):19–28. [PubMed] [Google Scholar]
- 17.Brunocilla E., Borghesi M., Schiavina R., Pultrone C. V., Martorana G. Re: impact of complete bladder neck preservation on urinary continence, quality of life and surgical margins after radical prostatectomy: a randomized, controlled, single blind trial. European Urology. 2013;64(2):338–339. doi: 10.1016/j.eururo.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 18.Nyarangi-Dix J. N., Radtke J. P., Hadaschik B., Pahernik S., Hohenfellner M. Impact of complete bladder neck preservation on urinary continence, quality of life and surgical margins after radical prostatectomy: a randomized, controlled, single blind trial. Journal of Urology. 2013;189(3):891–898. doi: 10.1016/j.juro.2012.09.082. [DOI] [PubMed] [Google Scholar]
- 19.Chen J. Y., Chen D., Wang J. L., et al. Strategies of preserving urinary continence in transurethral plasmakinetic enucleation of the prostate for benign prostate hyperplasia. Zhonghua Nan Ke Xue = National Journal of Andrology. 2018;24(2):138–141. [PubMed] [Google Scholar]
- 20.Ruszat R., Seitz M., Wyler S. F., et al. Prospective single-centre comparison of 120-W diode-pumped solid-state high-intensity system laser vaporization of the prostate and 200-W high-intensive diode-laser ablation of the prostate for treating benign prostatic hyperplasia. BJU International. 2009;104(6):820–825. doi: 10.1111/j.1464-410x.2009.08452.x. [DOI] [PubMed] [Google Scholar]
- 21.Gilpin S. A., Gosling J. A. Smooth muscle in the wall of the developing human urinary bladder and urethra. Journal of Anatomy. 1983;137(3):503–512. [PMC free article] [PubMed] [Google Scholar]
- 22.Yeni E., Unal D., Verit A., Gulum M. Minimal transurethral prostatectomy plus bladder neck incision versus standard transurethral prostatectomy in patients with benign prostatic hyperplasia: a randomised prospective study. Urologia Internationalis. 2002;69(4):283–286. doi: 10.1159/000066127. [DOI] [PubMed] [Google Scholar]
- 23.Reich O., Gratzke C., Bachmann A., et al. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. Journal of Urology. 2008;180(1):246–249. doi: 10.1016/j.juro.2008.03.058. [DOI] [PubMed] [Google Scholar]
- 24.Li X., Pan J. H., Liu Q. G., et al. Selective transurethral resection of the prostate combined with transurethral incision of the bladder neck for bladder outlet obstruction in patients with small volume benign prostate hyperplasia (BPH): a prospective randomized study. PLoS One. 2013;8(5) doi: 10.1371/journal.pone.0063227.e63227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rosen R., Altwein J., Boyle P., et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7) European Urology. 2003;44(6):637–649. doi: 10.1016/j.eururo.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 26.Jahnson S., DalÉn M., Gustavsson G., Pedersen J. Transurethral incision versus resection of the prostate for small to medium benign prostatic hyperplasia. British Journal of Urology. 1998;81(2):276–281. doi: 10.1046/j.1464-410x.1998.00535.x. [DOI] [PubMed] [Google Scholar]
- 27.Dørflinger T., Jensen F. S., Krarup T., Walter S. Transurethral prostatectomy compared with incision of the prostate in the treatment of prostatism caused by small benign prostate glands. Scandinavian Journal of Urology and Nephrology. 1992;26(4):333–338. doi: 10.3109/00365599209181222. [DOI] [PubMed] [Google Scholar]
- 28.Riehmann M., Knes J. M., Heisey D., Madsen P. O., Bruskewitz R. C. Transurethral resection versus incision of the prostate: a randomized, prospective study. Urology. 1995;45(5):768–775. doi: 10.1016/s0090-4295(99)80081-8. [DOI] [PubMed] [Google Scholar]
- 29.Narayan P., Lange P. H., Fraley E. E. Ejaculation and fertility after extended retroperitoneal lymph node dissection for testicular cancer. Journal of Urology. 1982;127(4):685–688. doi: 10.1016/s0022-5347(17)53996-8. [DOI] [PubMed] [Google Scholar]
- 30.Leiter E., Brendler H. Loss of ejaculation following bilateral retroperitoneal lymphadenectomy. Journal of Urology. 1967;98(3):375–378. doi: 10.1016/S0022-5347(17)62894-5. [DOI] [PubMed] [Google Scholar]
- 31.Horenblas S., Meinhardt W., Ijzerman W., Moonen L. F. M. Sexuality preserving cystectomy and neobladder: Journal of Urology. 2001;166(3):837–840. doi: 10.1016/s0022-5347(05)65847-8. [DOI] [PubMed] [Google Scholar]
- 32.Meinhardt W., Horenblas S. Sexuality preserving cystectomy and neobladder (SPCN): functional results of a neobladder anastomosed to the prostate. European Urology. 2003;43(6):646–650. doi: 10.1016/s0302-2838(03)00099-x. [DOI] [PubMed] [Google Scholar]
- 33.Girgin C., Oder M., Sahin M. O., et al. Erection- and ejaculation-preserving cystectomy with orthotopic urinary diversion: is it feasible? Journal of Andrology. 2006;27(2):263–267. doi: 10.2164/jandrol.05074. [DOI] [PubMed] [Google Scholar]
- 34.Placer J., Gelabert-Mas A., Vallmanya F., et al. Holmium laser enucleation of prostate: outcome and complications of self-taught learning curve. Urology. 2009;73(5):1042–1048. doi: 10.1016/j.urology.2008.12.052. [DOI] [PubMed] [Google Scholar]
- 35.Gong Y.-G., He D.-L., Wang M.-Z., et al. Holmium laser enucleation of the prostate: a modified enucleation technique and initial results. Journal of Urology. 2012;187(4):1336–1340. doi: 10.1016/j.juro.2011.11.093. [DOI] [PubMed] [Google Scholar]
- 36.Miernik A., Schoeb D. S. Three horse shoe-like incision” holmium laser enucleation of the prostate: first experience with a novel en bloc technique for anatomic transurethral prostatectomy. World Journal of Urology. 2019;37(3):523–528. doi: 10.1007/s00345-018-2418-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The supplementary file is the original data for the results of all patients. Sheet1: modified group. Sheet2: traditional group.
Data Availability Statement
The supplementary material contains the original data of this study.