Abstract
Genome editing has opened up the possibility of heritable alteration of the human germline. The potential of this powerful tool has spurred a call for establishing robust regulatory frameworks to outline permissible uses of genome editing and to map a rational and ethical course. In response, major national scientific bodies and international organizations have convened and released comprehensive reports outlining recommendations for ethical regulatory frameworks. Significantly, these include an emphasis on public participation and the development of principles to guide future applications of genome editing. While essential, public input and principles are not sufficient to ensure ethical uses of this technology. We propose an approach that relies not only on agreed-upon principles and a democratic process but requires a Human Rights Impact Assessment to evaluate the potential burdens that such biomedical interventions may place on human rights.
Introduction
Decades before the first use of CRISPR to edit DNA, advances in genetic techniques such as recombinant DNA, in vitro fertilization, and reproductive cloning stimulated widespread concern, scholarship, and policy statements against genetic manipulation of the human germline.1–3 In response, national and international governments enacted policies restricting or banning manipulation of the human germline for reproductive purposes.4–7 Yet, despite long-standing opposition, the change in technical feasibility brought by CRISPR has launched renewed debate, and the possibility of a path for editing the germline is now being discussed by respected bodies around the world.8–10
What has emerged is the need for public participation and the development of principles to guide future applications of genome editing. We argue here that while essential, public input and abstract principles are not sufficient to ensure ethical uses of this technology. Rather, we propose the addition of a Human Rights Impact Assessment (HRIA), drawing on lessons from the public health discipline, recognizing the unique impact germline interventions may have not only on individuals but also on societies and the future of humanity.11 Such an assessment adds the requirement to evaluate the potential burdens that each application of germline genome editing (GGE) may place on human rights.
Regulatory Frameworks Proposed by Influential Bodies
The development and democratization of CRISPR technology has made targeted human GGE a real possibility, spurring heightened urgency and concerted global efforts to establish new regulatory frameworks that outline GGE's permissibility. Multiple national and international bodies have formed, and numerous position statements have been published.8 While opposition against GGE has continued, others have begun to consider theoretical conditions where germline editing may someday be ethically warranted. Within this debate, reports from two influential bodies have garnered particular attention: the 2017 National Academies of Sciences, Engineering, and Medicine (NASEM) Committee on Human Genome Editing, and the Nuffield Council on Bioethics Working Party on genome editing and human reproduction.9,10
In 2017, the NASEM Human Genome Editing Consensus Report opened the door to scenarios in which GGE might be ethically justifiable, suggesting a multi-step decision-making process beyond examination of physical safety for determining when heritable (as well as nonheritable) genome editing would be acceptable.9 The authors of this report stress the necessity of public participation as a key step in the process.12 Similarly, the 2018 Nuffield Council report calls for public debate as part of its recommendations.10 The Nuffield Council report states some caveats when engaging with the public, but still maintains a strict need for democratic processes. Importantly, the report pairs its call for public participation with an identification of core principles that must be upheld in any application of germline genome editing.10 These influential reports share two common threads that have emerged prominently in other reports and statements: the pillars of public engagement and establishment of guiding principles.
Both public engagement and ethical principles are necessary in considering how GGE may impact society, but they fall short of effectively addressing real-world situations. We propose a tool that contextualizes public stances and core principles and safeguards the rights of all: a HRIA. First, we briefly consider public participation and principles, showing how they are valuable but insufficient to secure human rights.
Public Engagement: Necessary and Insufficient
Public participation is essential to policy making in democracies, as it captures dissenting views and helps to establish conduits of transparency and expanded understanding.13 Societal engagement in decision making promotes procedural justice—fairness and inclusion, as well as respect for autonomy—by incorporating those impacted into the process. Despite the inherent value and utility of public engagement, it is not without fundamental limitations. In aggregate, public opinion can reflect cultural biases and undervalue the perspectives of marginalized groups. Indeed, relying too heavily on public opinion can disregard essential human rights considerations. To illustrate this point, let us consider a notable health care policy case.
In 1989, the state of Oregon initiated an effort to expand eligibility for Medicaid health insurance to include all citizens below the poverty level. To achieve this, the state undertook to reallocate funds by prioritizing coverage of treatments based on their effectiveness. Drawing on ideals of participatory decision making, the state solicited public input regarding preferred health outcomes and quality of life for different conditions, creating a quantitative scale by which to evaluate the effectiveness of a treatment.14 The leaders who established the resulting policy were surprised when the state was later denied federal approval for the program, citing non-compliance with the Americans with Disabilities Act. The Department of Health and Human Services charged that the state discriminated against people with disabilities.15 Research shows that able-bodied people rate the limitations of having a disability much more negatively than do people living with disabilities.16 By using quality of life ratings based on public opinion, the state had inadvertently devalued the lives of persons with disabilities. Using quality of life as a measure by which to prioritize the importance of health services and outcomes presumed an objective, shared understanding that does not exist.14 Furthermore, analysts argued that under the Oregon plan, treatments for people with disabilities were more likely to fall to the bottom of the priority list.15,17 Thus, while public input is critical in decisions that affect the health of a population, it may not suffice to uphold the rights of vulnerable populations.
Given these challenges, simply querying the public suffers from key limitations. For decisions about GGE, public input on decision making about which conditions should be considered debilitating or undesirable enough to warrant possible future eradication may be primed for similar risks of inadvertent discrimination. Even the process by which public input is obtained may suffer from considerable limitations. For example, while a powerful and beneficial tool, public polling can often lead to answers that are not the result of careful, informed deliberation but rather are influenced by readily available information in memory, automatically generated affect, and salient information in the environment.18 To prevent biasing respondents, efforts are often made to avoid framing and contextualization. Yet, contextual information about competing technical, ethical, or social considerations may actually lead to more useful answers. This tension underlines the limitations of polling in ethical policy making. Public forums, surveys, focus groups, and other methods for gathering public input may complement polling, but also suffer from insufficient reach, self-selection of participants, and inattention to differential power dynamics in presumed consensus building or democratic processes.19–22
There are crucial ethical reasons to seek broad public participation in making such a large change in norms as permitting GGE: to respect individual and group autonomy and to be fair and inclusive. The call for public engagement issued after the 2015 International Summit on Human Genome Editing acknowledges the stake that everyone has in these decisions and the diversity of views and values that are often eclipsed by powerful scientific elites.12 In response, multiple efforts have been initiated to involve the public through varying approaches, including polling, town-hall style meetings, deliberative engagement, and online forums, and there is ongoing research into novel approaches that improve engagement.23–33 Yet, while necessary, public participation alone is not sufficient to achieve policies that will genuinely protect individuals and society from changes that may not serve everyone's long-term well-being or rights. Clashing value systems and shifting public attitudes suggest additional approaches beyond public input must be incorporated when drafting robust policy. Establishing principles that protect vulnerable populations and value human rights may help address the limitations of public participation. Yet, despite the value of principles, below we also argue that these alone, or in combination with public opinion, are insufficient to establish ethical germline editing policy.
Building on Principles
Principles are crucial insofar as they involve reason-based arguments that underlie commitments to substantive moral claims. The Nuffield report, for example, asserts that germline editing cannot be ethically acceptable without weighing its use against two important principles: (1) protecting the welfare of future persons, and (2) upholding social justice and solidarity.10 Germline editing will affect future generations, creating an impact on public health as well as individual welfare, thereby extending the moral duty of protection to people not yet born. Social justice demands that burdens and benefits be distributed fairly, so that socially disadvantaged groups do not bear an inequitable share of the burden of health interventions, and that benefits are not solely enjoyed by those already experiencing social and economic advantage. Solidarity recognizes that society as a whole is better off when all members do well. But principles are usually decontextualized in that the reasoning behind the principle is usually based on philosophical commitments that are held to be universal in their scope. Delineating principles balances some limitations of public input. However, like public participation, principles are necessary but not sufficient for ethical decision making.
History shows that relying on principles does not always go far enough in actively determining ethical courses of action. During the 1980s, the U.S. President's Commission on Bioethics deliberated on seriously divisive bioethical issues, including developing criteria for brain death and allowing for the removal of life support. Experts could not agree on principles but did agree on specific cases (such as Karen Quinlan).34 Such case-based analysis is responsive to real—not abstract—human experience, and not bound by a single set of values or principles.35
Further, a reliance on rules or principles to create a guide for ethical conduct has been called a “quest for certainty.”35 This quest is futile when attempting to develop rules for technologies such as GGE where societal effects are so uncertain. Efforts to establish certainty about “permanent” solutions to human problems often reduce variegated human experiences to abstract standards that presume to apply in all situations. A central challenge is that a single agreed-upon set of principles presumes an ethical “universalism,” minimizing social and cultural differences that result in unfair advantage for some groups over others.36 The Oregon case, where an assumption about common understanding of “quality of life” resulted in inequity, illuminates the danger when both public participation and principles omit critical societal contexts where power relations already create unfair advantages and disadvantages.
Where Do We Go From Here? A HRIA
Challenged by clashing value systems and in need of an inclusive shared basis for decision making that upholds crucial principles yet is responsive to dynamic societal contexts, we seek a way forward. We propose adding a third process for evaluating individual and societal harms: a HRIA.11
While in medical ethics impacts of procedures are considered at the individual level, in public health ethics, impacts are considered at both individual and population levels. Because germline editing has the potential to impose burdens on future persons and societies, drawing on approaches from public health such as the HRIA widens considerations beyond individual impact.
The added value of a HRIA comes from providing an empirical assessment of power dynamics—in actual political and socioeconomic contexts—which may threaten human rights. Ethical principles lack context, and democratic processes may not protect the rights of vulnerable minorities. A HRIA provides the necessary third perspective and a way to apply principles to real situations. Empirical assessment of the likely influence of power dynamics on the implementation of new technologies is critical. As the former UN High Commissioner of Human Rights notes about new technologies such as artificial intelligence, there is no way for ethical guidelines to be meaningfully followed in societies where human rights conditions are not met.37 Public health assessments can evaluate the influence of racial, social, and economic inequities, and exclusion of people with disabilities, on health disparities.
There are other contexts beyond public health where empirical assessments have been created to protect individual and societal rights. For example, for almost 50 years, the National Environmental Policy Act of 1969 (NEPA) has required the evaluation of environmental risks in impacted communities.38 More recently, a regulatory process involving race impact assessments has been proposed to examine risk of harm to racial minorities from new biotechnologies that may propagate the centrality of biological race as a primary health determinant, downplaying the role of discrimination.39 And the UN Guiding Principles on Business and Human Rights (2011) directs transnational corporations to use a HRIA to assess impacts on the rights of workers and communities.40
We propose using a HRIA to guide ongoing decision making about GGE. This assessment can provide the socially shared transparent criteria necessary to structure inclusive productive democratic deliberation that aims to protect everyone's rights, irrespective of whether they participate in the deliberation. To achieve this, the HRIA uses a series of questions to help determine whether the potential benefit of a public health intervention or policy is outweighed by an undue burden on human rights. A HRIA would consider the protection of human rights in the specific context of germline editing, operationalizing the Nuffield principles of “welfare of the future person” and “social justice and solidarity,” and using a participatory process.10 The HRIA provides a way to examine how empirical conditions, including political and socioeconomic forces, combined with new technologies, may have the potential to undermine human rights.11
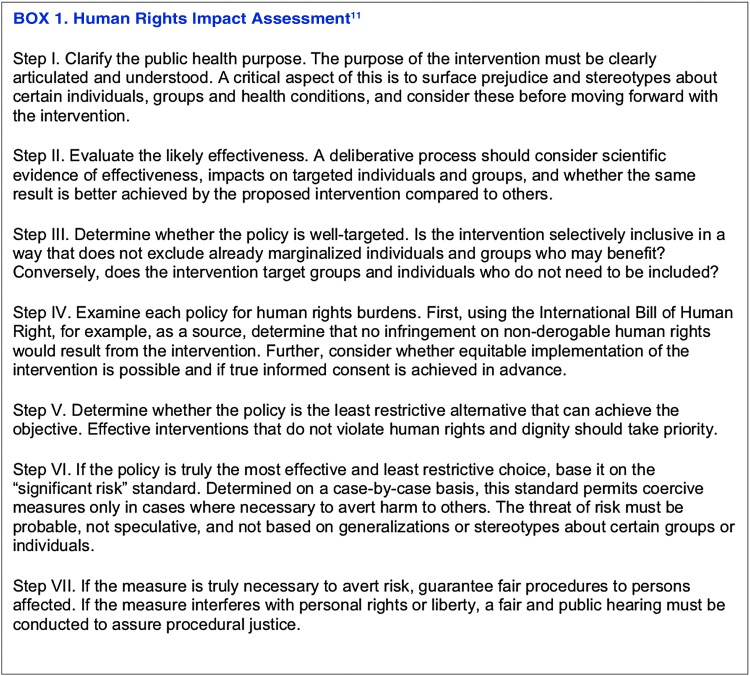
Lawrence Gostin and Jonathan Mann introduced the HRIA in 1994 based on observations that public health interventions can ultimately invoke state power, and that protecting human rights promotes public health.41 They also built upon previously acknowledged rights, including the right to enjoy the benefits of scientific progress,42 which has been recently reaffirmed.43 While there are seven criteria in the HRIA (see Box 1), here we touch on a few of its priorities: (1) whether the proposed innovation or policy is well targeted; (2) whether it is the least restrictive/intrusive (in case of GGE) way to intervene; and (3) what the human rights burden may be.
Is the proposed policy well targeted?
A public health intervention that is not well targeted selectively excludes already marginalized individuals and groups who might benefit or includes groups and individuals who do not need to be included. Both are a significant concern with GGE. As discussed above, already disadvantaged groups may face barriers to access, thus creating an underclass for those with fewer resources. Over-inclusion is possible if genetic alterations are forced upon populations, imposing unnecessary changes to individuals and their offspring. This refers in part to targeting conditions that some do not believe need to be “treated,” for example if it became not only possible to edit deafness but expected that deafness should be eliminated. The subsequent pressure on vulnerable communities is not captured by a specific principle nor, as occurred in Oregon, democratic participation, but is exactly what a HRIA seeks to identify.
Is GGE the least restrictive/intrusive alternative that can achieve the objective?
Consider the recent case of GGE involving the Δ32 mutation within the CCR5 gene to render children HIV resistant.44 As this mutation may increase vulnerability to other infections such as influenza, creating an undue burden on these offspring, we would opt instead for safer ways to prevent HIV infection.45 Additionally, the current safety and efficacy of GGE tools in combination with limited scientific understanding of embryo development suggests that GGE is impermissible on the grounds of effectiveness. Many less intrusive methods are already available to parents, including using third-party gametes and preimplantation genetic testing.
By considering when a less effective intervention burdens people with unnecessary risks, the HRIA addresses not only society-level concerns, but also core scientific concerns stressed in both the NASEM and Nuffield Council reports. The irreversible nature of GGE, its heritability, and its impact on future generations demand that we assess its impact on human rights and seek less intrusive ways of accomplishing public-health goals when possible. Interventions that do not violate human rights and dignity should take priority.
What is the human rights burden?
It is essential to consider the needs of both individuals undergoing gene editing and those who are not. A human rights burden is created when individuals are involved in research or interventions without truly understanding the purpose, risks, and benefits involved. It is widely agreed that informed consent was not sought responsibly in the case of the first genome-edited babies, with the consent forms calling the intervention “AIDS vaccine development.”46 Beyond this problematic case, there may not be sufficient knowledge of long-term GGE risks, including to future generations, to elicit true informed consent.
The HRIA also has the ability to assess the sociological shifts and human rights burdens on those not edited when it becomes the norm to eliminate a particular disease. Consider again germline editing for congenital forms of deafness. Proponents of cochlear implants have met resistance from members of Deaf communities, who view deafness as a vibrant culture not an impairment.47,48 Further, if GGE to eliminate deafness becomes a norm, how will people who cannot afford germline editing be viewed by society? Will people who are deaf risk losing medical benefits if they became members of an “underclass?”
Conclusion
Human germline alteration is possible, due in part to democratization of genetic tools required for genome editing, and international scientific and legislative bodies are developing frameworks to manage the ramifications of this technology. Common among these frameworks are two pillars: public engagement and foundational principles. These components are necessary for respecting the autonomy of individuals and for fair processes and respecting diverse values.
However, they are not sufficient for protecting the most vulnerable members of society who may not even be in a position to participate in democratic processes. We propose implementing a HRIA, which captures concerns of public health and offers an opportunity to evaluate and anticipate the societal impact of GGE iteratively as the technology advances, public sentiments evolve, and cultural contexts shift. We recognize that this will raise new challenges of how such assessments are shared and implemented and how they can be enforced. We urge regulatory bodies and policy makers to consider this assessment approach in helping to establish robust regulatory frameworks necessary for the global protection of human rights.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
Support was provided, in part, by the Innovative Genomics Institute.
References
- 1. Evans JH, Schairer CE. Bioethics and human genetic engineering. In: Handbook of Genetics and Society: Mapping the New Genomic Era. London: Routledge, 2009:349–366 [Google Scholar]
- 2. Lappé M. Ethical issues in manipulating the human germ line. J Med Philos 1991;16:621–639. DOI: 10.1093/jmp/16.6.621. [DOI] [PubMed] [Google Scholar]
- 3. Stock G, Campbell J. Engineering the Human Germline: An Exploration of the Science and Ethics of Altering the Genes We Pass to Our Children. Oxford: Oxford University Press, 2000. [Google Scholar]
- 4. Araki M, Ishii T. International regulatory landscape and integration of corrective genome editing into in vitro fertilization. Reprod Biol Endocrinol 2014;12:108 DOI: 10.1186/1477-7827-12-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Universal Declaration on the Human Genome and Human Rights: UNESCO. Available online at http://portal.unesco.org/en/ev.php-URL_ID=13177&URL_DO=DO_TOPIC&URL_SECTION=201.html (last accessed September17, 2019)
- 6. The Oviedo Convention: protecting human rights in the biomedical field. Available online at https://www.coe.int/en/web/bioethics/oviedo-convention (last accessed September17, 2019)
- 7. Witkowsky LB. The Designer Baby Distraction. Available online at https://www.asm.org/Articles/Cultures-Magazine/Volume-4,-Issue-4-2017/The-Designer-Baby-Distraction (last accessed September17, 2019)
- 8. Brokowski C. Do CRISPR germline ethics statements cut it? CRISPR J 2018;1:115–125. DOI: 10.1089/crispr.2017.0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. National Academies of Sciences, Engineering, and Medicine, et al. Human Genome Editing: Science, Ethics, and Governance. Washington, DC: National Academies Press, 2017 [PubMed] [Google Scholar]
- 10. Nuffield Council on Bioethics. Genome Editing and Human Reproduction: Social and Ethical Issues. London: Nuffield Council on Bioethics, 2018. [Google Scholar]
- 11. Gostin L, Mann JM. Towards the development of a human rights impact assessment for the formulation and evaluation of public health policies. Health Hum Rights 1994;1:58–80. DOI: 10.2307/4065262 [DOI] [PubMed] [Google Scholar]
- 12. National Academies of Sciences, Engineering, and Medicine. Public engagement. In: Human Genome Editing: Science, Ethics, and Governance. Washington, DC: National Academies Press, 2017:163–179 [PubMed] [Google Scholar]
- 13. Gerston LN. Public Policymaking in a Democratic Society: A Guide to Civic Engagement. London: Routledge, 2014. [Google Scholar]
- 14. Hadorn DC. The Oregon priority-setting exercise: quality of life and public policy. Hastings Cent Rep 1991;21:11 DOI: 10.2307/3563329. [DOI] [PubMed] [Google Scholar]
- 15. Menzel PT. Oregon's denial: disabilities and quality of life. Hastings Cent Rep 1992;22:21–25. DOI: 10.2307/3562943. [DOI] [PubMed] [Google Scholar]
- 16. Ubel PA, Loewenstein G, Schwarz N, et al. . Misimagining the unimaginable: the disability paradox and health care decision making. Health Psychol 2005;24:S57–S62. DOI: 10.1037/0278-6133.24.4.S57. [DOI] [PubMed] [Google Scholar]
- 17. Fox DM, Leichter HM. State model: Oregon. The ups and downs of Oregon's rationing plan. Health Aff (Millwood) 1993;12:66–70. DOI: 10.1377/hlthaff.12.2.66. [DOI] [PubMed] [Google Scholar]
- 18. Zaval L, Cornwell JFM. Cognitive biases, non-rational judgments, and public perceptions of climate change. In: Oxford Research Encyclopedia of Climate Science. Oxford: Oxford University Press, 2016:1–23. DOI: 10.1093/acrefore/9780190228620.013.304. [DOI] [Google Scholar]
- 19. Sturgis P. On the limits of public engagement for the governance of emerging technologies. Public Underst Sci 2014;23:38–42. DOI: 10.1177/0963662512468657. [DOI] [PubMed] [Google Scholar]
- 20. Burall S. Rethink public engagement for gene editing. Nature 2018;555:438–439. DOI: 10.1038/d41586-018-03269-3. [DOI] [PubMed] [Google Scholar]
- 21. Kerr A, Cunningham-Burley S, Tutton R. Shifting subject positions: experts and lay people in public dialogue. Soc Stud Sci 2007;37:385–411. DOI: 10.1177/0306312706068492. [DOI] [Google Scholar]
- 22. Karpowitz CF, Mansbridge J. Disagreement and consensus: the need for dynamic updating in public deliberation. J Public Delib 2005;1:2 [Google Scholar]
- 23. Jasanoff S, Hurlbut JB. A global observatory for gene editing. Nature 2018;555:435–437. DOI: 10.1038/d41586-018-03270-w. [DOI] [PubMed] [Google Scholar]
- 24. Montoliu L, Merchant J, Hirsch F, et al. . ARRIGE arrives: toward the responsible use of genome editing. CRISPR J 2018;1:128–129. DOI: 10.1089/crispr.2018.29012.mon. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Van Mil A, Hopkins H, Kinsella S. Potential uses for genetic technologies: dialogue and engagement research conducted on behalf of the Royal Society. Findings Report, 2017. Available online at https://royalsociety.org/~/media/policy/projects/gene-tech/genetic-technologies-public-dialogue-hvm-full-report.pdf (last accessed September17, 2019)
- 26. Grant to fund research on future of human genome editing. Available online at https://www.bcm.edu/news/grants/grant-funds-genome-editing-research (last accessed September17, 2019)
- 27. Blendon RJ, Gorski MT, Benson JM. The public and the gene-editing revolution. N Engl J Med 2016;374:1406–1411. DOI: 10.1056/NEJMp1602010. [DOI] [PubMed] [Google Scholar]
- 28. Pew Research Center. U.S. public wary about use of biomedical technology for human enhancement. Available online at https://www.pewresearch.org/science/2016/07/26/u-s-public-wary-of-biomedical-technologies-to-enhance-human-abilities/ (last accessed September17, 2019)
- 29. Scheufele DA, Xenos MA, Howell EL, et al. . US attitudes on human genome editing. Science 2017;357:553–554. DOI: 10.1126/science.aan3708. [DOI] [PubMed] [Google Scholar]
- 30. Gaskell G, Bard I, Allansdottir A, et al. . Public views on gene editing and its uses. Nat Biotechnol 2017;35:1021 DOI: 10.1038/nbt.3958. [DOI] [PubMed] [Google Scholar]
- 31. The Associated Press-NORC Center for Public Affairs Research. Human genetic engineering. Available online at http://apnorc.org/projects/Pages/Human-Genetic-Engineering.aspx (last accessed September17, 2019)
- 32. Uchiyama M, Nagai A, Muto K. Survey on the perception of germline genome editing among the general public in Japan. J Hum Genet 2018;63:745 DOI: 10.1038/s10038-018-0430-2 [DOI] [PMC free article] [PubMed]
- 33. McCaughey T, Sanfilippo PG, Gooden GE, et al. . A global social media survey of attitudes to human genome editing. Cell Stem Cell 2016;18:569–572 [DOI] [PubMed] [Google Scholar]
- 34. In re Quinlan. A. 2d 355, 647 (Supreme Court 1976)
- 35. Toulmin S. The tyranny of principles. Hastings Cent Rep 1981;11:31 DOI : 10.2307/3560542 [DOI] [PubMed] [Google Scholar]
- 36. Fox RC, Swazey JP. Guest editorial: ignoring the social and cultural context of bioethics is unacceptable. Camb Q Healthc Ethics 2010;19:278–281. DOI: 10.1017/S0963180110000046. [DOI] [PubMed] [Google Scholar]
- 37. Hussein ZRA. Here's what will decide whether technology becomes a force for good, or evil. Available online at https://www.washingtonpost.com/opinions/technology-can-be-put-to-good-use--or-hasten-the-demise-of-the-human-race/2019/04/09/c7af4b2e-56e1-11e9-8ef3-fbd41a2ce4d5_story.html (last accessed June20, 2019)
- 38. U.S.C. Title 42—The Public Health and Welfare. Available online at https://www.govinfo.gov/content/pkg/USCODE-2011-title42/html/USCODE-2011-title42-chap55.htm (last accessed June20, 2019)
- 39. Obasogie OK. The return of biological race: regulating innovations in race and genetics through administrative agency race impact assessments. Cal Interdisc LJ 2012;22:1 [Google Scholar]
- 40. Business & Human Rights Resource Centre. UN guiding orinciples. Available online at https://www.business-humanrights.org/en/un-guiding-principles (last accessed June20, 2019)
- 41. Mann JM. Medicine and public health, ethics and human rights. Hastings Cent Rep 1997;27:6–13. DOI: 10.2307/3528660. [DOI] [PubMed] [Google Scholar]
- 42. United Nations Treaty Collection. Available online at https://treaties.un.org/Pages/ViewDetails.aspx?src=IND&mtdsg_no=IV-3&chapter=4&clang=_en (last accessed June20, 2019)
- 43. Boggio A, Knoppers BM, Almqvist J, et al. . The human right to science and the regulation of human germline engineering. CRISPR J 2019;2:134–142. DOI: 10.1089/crispr.2018.0053. [DOI] [PubMed] [Google Scholar]
- 44. Page ML. Exclusive: Five couples lined up for CRISPR babies to avoid deafness. Available online at https://www.newscientist.com/article/2208777-exclusive-five-couples-lined-up-for-crispr-babies-to-avoid-deafness/ (last accessed July12, 2019)
- 45. Wei X, Nielsen R. CCR5-Δ 32 is deleterious in the homozygous state in humans. Nat Med 2019;25:909–910. DOI: 10.1038/s41591-019-0459-6. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 46. Marchione M. Chinese researcher claims first gene-edited babies. Available online at https://apnews.com/4997bb7aa36c45449b488e19ac83e86d (last accessed June20, 2019)
- 47. Sparrow R. Defending deaf culture: the case of cochlear implants. J Polit Philos 2005;13:135–152. DOI: 10.1111/j.1467-9760.2005.00217.x. [DOI] [Google Scholar]
- 48. Davis DS. Genetic dilemmas and the child's right to an open future. Hastings Cent Rep 1997;27:7–15. DOI: 10.2307/3527620. [DOI] [PubMed] [Google Scholar]