Supplemental Digital Content is available in the text.
Keywords: airway management, direct laryngoscopy, emergency care, prehospital intubation, randomized controlled trial, video laryngoscopy
Objectives:
Tracheal intubation in prehospital emergency care is challenging. The McGrath Mac Video Laryngoscope (Medtronic, Minneapolis, MN) has been proven to be a reliable alternative for in-hospital airway management. This trial compared the McGrath Mac Video Laryngoscope and direct laryngoscopy for the prehospital setting.
Design:
Multicenter, prospective, randomized, controlled equivalence trial.
Setting:
Oesterreichischer Automobil- und Touring Club (OEAMTC) Helicopter Emergency Medical Service in Austria, 18-month study period.
Patients:
Five-hundred fourteen adult emergency patients (≥ 18 yr old).
Interventions:
Helicopter Emergency Medical Service physicians followed the institutional algorithm, comprising a maximum of two tracheal intubation attempts with each device, followed by supraglottic, then surgical airway access in case of tracheal intubation failure. No restrictions were given for tracheal intubation indication.
Measurements Main Results:
The Primary outcome was the rate of successful tracheal intubation; equivalence range was ± 6.5% of success rates. Secondary outcomes were the number of attempts to successful tracheal intubation, time to glottis passage and first end-tidal Co2 measurement, degree of glottis visualization, and number of problems. The success rate for the two devices was equivalent: direct laryngoscopy 98.5% (254/258), McGrath Mac Video Laryngoscope 98.1% (251/256) (difference, 0.4%; 99% CI, –2.58 to 3.39). There was no statistically significant difference with regard to tracheal intubation times, number of attempts or difficulty. The view to the glottis was significantly better, but the number of technical problems was increased with the McGrath Mac Video Laryngoscope. After a failed first tracheal intubation attempt, immediate switching of the device was significantly more successful than after the second attempt (90.5% vs 57.1%; p = 0.0003), regardless of the method.
Conclusions:
Both devices are equivalently well suited for use in prehospital emergency tracheal intubation of adult patients. Switching the device following a failed first tracheal intubation attempt was more successful than a second attempt with the same device.
Tracheal intubation (TI) remains the golden, but challenging and rare (2–12%) standard of care for securing the airway and ensuring appropriate ventilation in the prehospital emergency setting (1–4). Lacking routine (even < 12 intubations per physician and year) and the specific prehospital setting (5–7) may contribute to difficult TIs, with the literature documenting up to 50% as being impossible (8–10).
Consequently, identification of devices that may facilitate TI appears to be of utmost importance. Presently, video laryngoscopes (VLs) are considered to be effective alternatives to direct laryngoscopes (DLs) when a difficult airway is presumed (11, 12). Yet, in-hospital findings, even in the emergency department (13), as well as manikin studies (14, 15) obviously may not be transferred to the prehospital setting. The few available randomized controlled trials (RCTs) evaluating VL there (16–18) failed to prove superiority or at least equality to DL. Nevertheless, VL have become part of standard Emergency Medical Service (EMS) equipment (19–21). The Austrian Air Rescue provider OEAMTC (Austrian Automobile, Motorcycle and Touring Club) implemented the McGrath Mac VL (McGrathVL; Medtronic, Minneapolis, MN) for prehospital airway management in its Helicopter EMS (HEMS) program in 2015. This offered the opportunity to compare the McGrathVL and the DL for prehospital TI in the skilled hands of the OEAMTC HEMS crews. The hypothesis of this multicenter, RCT was that both the McGrathVL and the DL (Medicon, Tuttlingen, Germany) have equivalent success rates for TI in the prehospital emergency environment. Primary outcome was the TI success rate for each device. Secondary outcome variables were the total number of TI attempts, time until passage of the tracheal tube through the glottis and to first end-tidal Co2 as a surrogate variable for successful TI. Additionally, the median category of visualization of the glottis, the median category of HEMS physician’s subjective assessment of TI performance, technical difficulties, and any harm during TI were documented.
MATERIALS AND METHODS
This prospective, multicenter, open-label, patient-blinded, RCT was conducted at 10 physician-staffed HEMS bases operated by OEAMTC Air Rescue, following approval by the Ethics Committee of the State of Lower Austria (GS1-EK-3/124–2016).
Participants
Adult emergency patients requiring prehospital TI were enrolled and randomly assigned. Exclusion criteria were age less than 18 years and futility of further measures if survival was unlikely. The following data were collected as follows: demographic data, indication for TI, vital variables (electrocardiogram, heart rate, blood pressure, peripheral oxygen saturation, end-tidal Co2) at various time points during prehospital care and hospital handover, modified National Advisory Committee for Aeronautics Index (22), cervical spine immobilization, and administered medication. HEMS physicians were either board-certified anesthesiologists or EMS physicians with at least 4 years of postgraduate training including inpatient anesthesia.
Interventions
Patients were randomly assigned to TI with either the McGrathVL or a DL.
Objective
The hypothesis of this trial was that both the McGrathVL and the DL (Medicon) have equivalent success rates for TI in the prehospital emergency environment. The equivalence range of success rates was ± 6.5%.
Outcome
Primary outcome was the TI success rate for each method. Secondary outcome variables were total number of TI attempts, time until passage of the tracheal tube through the glottis and to first end-tidal Co2 as a surrogate variable for successful TI. Additionally, the median category of visualization of the glottis, defined by a slightly modified Cormack and Lehane score (1 = whole glottis, 2 = arytenoid cartilage only, 3 = posterior commissure, 4 = epiglottis only, 5 = soft palate only), the median category of HEMS physician’s subjective assessment of TI performance (1 = problem-free, 2 = slightly aggravated, 3 = difficult, 4 = very difficult, 5 = impossible), technical difficulties and any harm during TI were documented.
Randomization
The web-based documentation (EDV Trimmel, Ternitz, Austria), including a computed random generator (1:1 ratio) and the electronic case report form determined the device assigned to each patient at each HEMS base. A printout of the assignment was archived at each participating HEMS base and opened by the HEMS technician on occasion. HEMS physicians subsequently performed airway management as herein defined; time was measured by the HEMS technician (triple chronometer; Oregon Scientific WB 388, Portland, OR).
Standardized Airway Management Protocol
Adherence to the predefined airway management algorithm of OEAMTC HEMS was mandatory. Whichever laryngoscope was used—video or direct—all blades were Macintosh-style blades. All tracheal tubes used in this study were factory-equipped with a semi-rigid stylet which can be bend and shaped as needed for the individual patient, thus facilitating guidance and manipulation (Kindwell Medical Equipment, Ltd., Tianjin, China). All patients were in supine position during the airway management process.
To guarantee the safety of study patients, preoxygenation and denitrogenization were ensured by high-flow oxygen via face mask or bag mask valve (AMBU, Bad Nauheim, Germany). HEMS technicians closely monitored oxygen saturation during induction of anesthesia and TI. They were instructed to prompt interruption of intubation attempts when saturation levels neared 90% or minus 10% of the basic level. Switching the device following the failed first intubation attempt, but not later than after the second attempt for each device was allowed. Accordingly, if the second TI attempt with the randomized device was not successful or discontinued, HEMS physicians were allowed to perform a further maximum of two attempts with the alternative device after ensuring appropriate oxygenation. After four failed TI attempts, a supraglottic airway had to be inserted: either a laryngeal tube (VBM Medizintechnik GmbH, Sulz am Neckar, Germany) or a laryngeal mask (Fastrach; Teleflex Medical Europe Ltd, Westmeath, Ireland) at the discretion of the HEMS physician. If this too was not feasible, a coniotomy had to be performed.
In patients undergoing cardiopulmonary resuscitation (CPR), TI was attempted without sedative drugs; in all others, rapid sequence induction (RSI) was performed using midazolam or propofol supplemented with esketamine and/or fentanyl. Succinylcholine or rocuronium (both 1.5 mg/kg body weight) was administered for RSI at the discretion of the HEMS physician. Anesthesia was maintained with repetitive boli of midazolam or propofol, esketamine and/or fentanyl.
Power Analysis
Preceding studies (17) led to the assumption that TI success rate for DL in the field should be around 97–98%. The suspected success rate for TI with the McGrathVL was 96% (13, 16, 23, 24). With a power of 90%, a significance level of 0.01 and an equivalence range of 6.5% of the success rates, 451 enrolled patients were required per group. We calculated a dropout rate of 10%. Thus, a total of 992 persons had to be included. An interim analysis was preplanned following enrollment of half of the study population (500 patients).
Statistical Analysis
In addition to descriptive statistics, analysis was performed using SPSS (release 24.0, 2016; IBM, Chicago, IL). Normal distribution was proven with the Shapiro-Wilk test. Equivalence of the success rate for the two devices was evaluated by computing the difference between the success rates and its two-sided 99% CIs. If the CI for the difference between the success rates was within the equivalence range of ± 6.5%, the two devices were deemed equally successful. The Mann-Whitney U test, chi-square test, and Fisher exact test were used to detect significant inter-group differences when investigating study population characteristics and secondary endpoints, as appropriate. The association between the success rate and potentially influencing factors (gender, body mass index, age, cervical spine immobilization, indication for airway management, and helicopter base) was assessed using multiple logistic regression analysis. A p value of 0.01 was deemed statistically significant throughout the study. Correspondingly, the CIs were 99%.
RESULTS
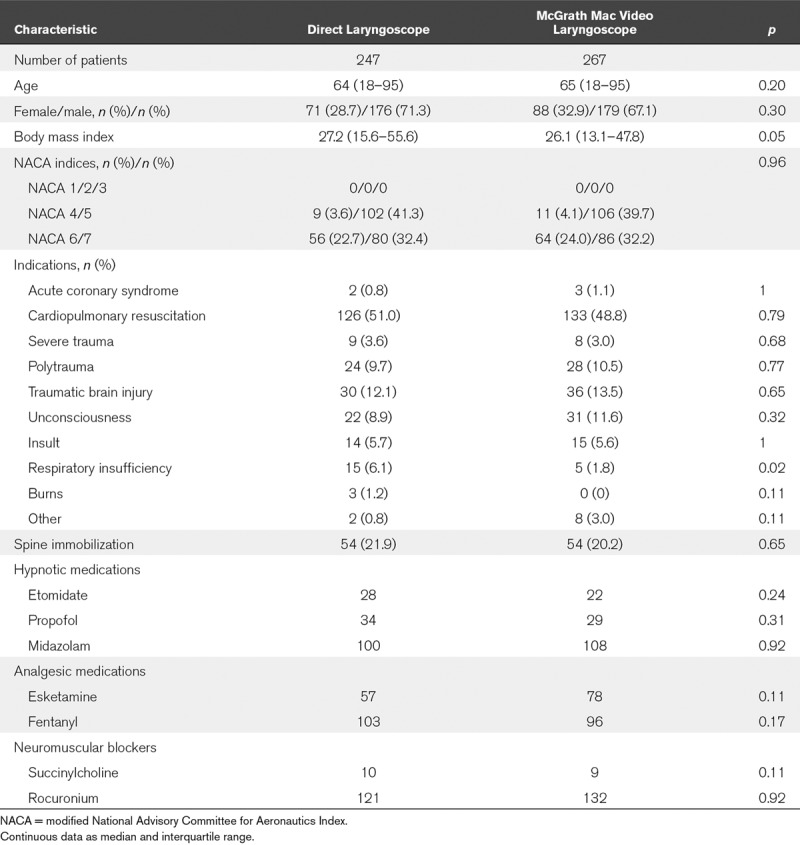
Between April 2017 and July 2018, the participating OEAMTC HEMS bases tended to 9,901 patients on emergency missions. Of these, 514 patients were included for analysis (Fig. 1). No baseline differences were observed between the groups (Table 1). There was only one protocol violation: one patient underwent three attempts with the McGrathVL. All results were evaluated by intention-to-treat analysis.
Figure 1.
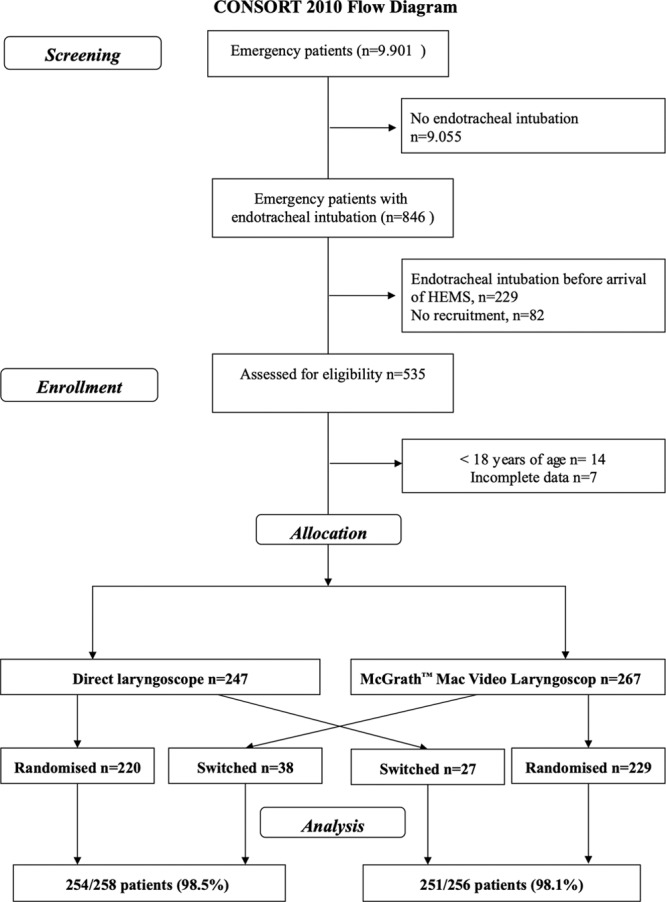
Consolidated Standards of Reporting Trials (CONSORT) 2010 flow diagram. HEMS = Helicopter Emergency Medical Service. Adapted from Schulz et al (25). Adaptations are themselves works protected by copyright. So in order to publish this adaptation, authorization must be obtained both from the owner of the copyright in the original work and from the owner of copyright in the translation or adaptation.
TABLE 1.
Study Population Characteristics
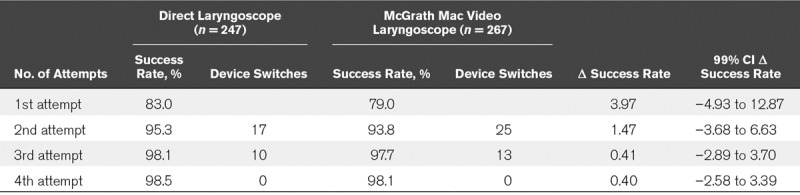
Following a maximum of four TI attempts, 505 of the 514 patients were successfully intubated showing equivalent results for the two devices: 254 of 258 patients (98.5%; CI, –0.6% to 2.6%) with the DL and 251 of 256 patients (98.1%; CI, –0.6% to 2.6%) with the McGrathVL. Thus, the difference in the success rates was 0.4%, and the 99% CIs for the difference in the success rates (99% CI, –2.58 to 3.39) were within the supposed equivalence range of ± 6.5% (Table 2).
TABLE 2.
Rate of Successful Tracheal Intubation With the Direct Laryngoscope and the McGrath Mac Video Laryngoscope, Equivalence Margin ± 6.5%
The remaining nine patients were successfully ventilated with alternative airways: five of nine (55.6%) with a larynx tube, two of nine (22.2%) with a laryngeal mask, and two of nine (22.2%) with a coniotomy.
Multiple regression analysis showed no association between success rates and patient gender, body mass index, age, cervical spine immobilization, indication for airway management, or helicopter base.
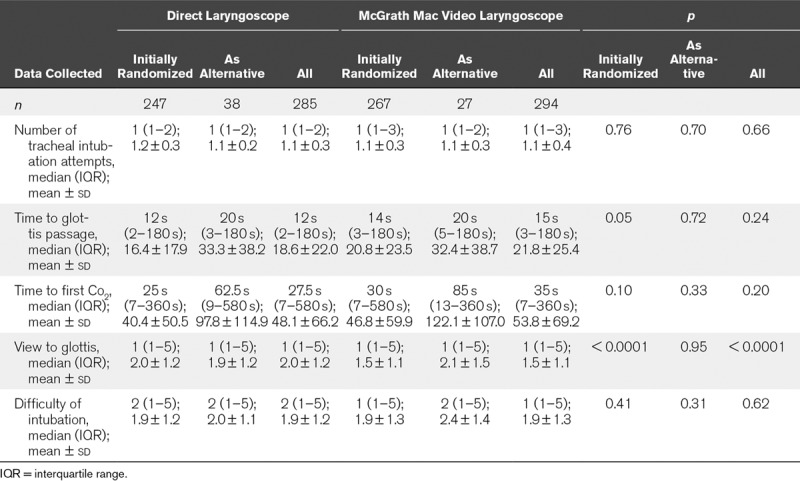
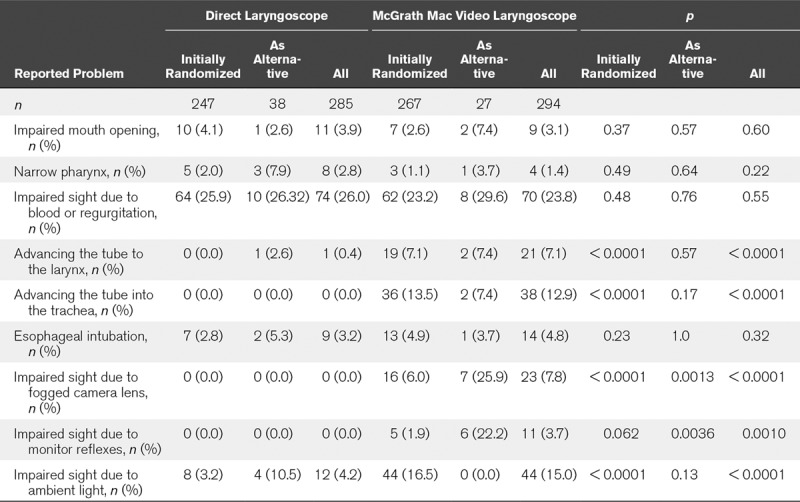
Despite better visualization of the glottis with the McGrathVL (p < 0.0001), the number of TI attempts, time to passage of the tracheal tube through the glottis and to first end-tidal Co2 measurement, as well as the category of HEMS physicians’ subjective assessment of TI performance were comparable (Table 3). This was caused by highly significantly more technical problems (impaired sight due to fogged camera lens, monitor reflexes, ambient light) with the McGrathVL (78/294, 26.5%) than with the DL (12/285, 4.2%; p < 0.0001). Although the view of the glottis improved with the McGrathVL, advancement of the tube into the larynx or the trachea was significantly impaired, but ultimately equally successful as with the DL (Tables 2, 3, and 4; and Supplemental Table 1, Supplemental Digital Content 1, http://links.lww.com/CCM/E834; Supplemental Table 2, Supplemental Digital Content 2, http://links.lww.com/CCM/E835; and Supplemental Table 3, Supplemental Digital Content 3, http://links.lww.com/CCM/E836).
TABLE 3.
Tracheal Intubation: Performance Data
Switching from the DL to the McGrathVL (success rate second attempt 15/25, 60% vs switching 15/17, 88.2%; p = 0.081) or vice versa (success rate second attempt 17/31, 54.8% vs 23/25, 92%; p = 0.002) following an unsuccessful first TI attempt was significantly more successful than switching following two attempts with the same device (Supplemental Fig. 1, Supplemental Digital Content 4, http://links.lww.com/CCM/E837; legend: flow diagram showing included patients, in whom TI attempts failed and the device was switched).
In trauma patients, especially those with cervical spine immobilization, and in patients undergoing CPR, the first TI attempt was more often successful with the DL. In patients with other reasons for TI (e.g., respiratory insufficiency, unconsciousness, stroke) the success rate showed no relevant difference. This did not reach statistical significance, but the subgroups were too small to draw a meaningful conclusion. These results are displayed in Supplemental Table 3 (Supplemental Digital Content 3, http://links.lww.com/CCM/E836).
Analyzing the potential reasons for TI failure, successful and unsuccessful attempts were compared: DL in trauma patients, impaired mouth opening (1/60, 1.7% vs 3/6, 50%;p = 0.002). In patients undergoing CPR: impaired glottic view (1 [1–5] vs 4 [1–5]; p < 0.0001); in nontrauma patients impaired glottic view (1 [1–5] vs 4 [3–5]; p = 0.0008); with McGrathVL: in trauma patients: advancing the tube into the larynx (0/52, 0% vs 4/15, 26.7%; p = 0.002) or trachea (5/52, 9.6% vs 8/15, 53.3%; p = 0.0007); disturbing bright ambient light (7/52, 13.5% vs 11/15, 73.3%; p < 0.0001); in patients undergoing CPR: advancing the tube into the larynx (5/123, 4.1% vs 7/19, 36.8%; p < 0.0001) or the trachea (11/123, 8.9% vs 10/19, 52.6%; p < 0.0001); impaired sight due to mirror reflexes (0/123, 0% vs 3/19, 15.9%; p < 0.0001); disturbing ambient light (14/123, 11.4% vs 9/19, 47.4%; p < 0.0001). These differences were not found in nontrauma, non-CPR patients (Supplemental Table 1, Supplemental Digital Content 1, http://links.lww.com/CCM/E834; Supplemental Table 2, Supplemental Digital Content 2, http://links.lww.com/CCM/E835; and Supplemental Table 3, Supplemental Digital Content 3, http://links.lww.com/CCM/E836).
The number of TI injuries was comparable between both groups: DL six of 285 patients (2.1%), McGrathVL eight of 294 patients (2.7%) (p = 0.63). In each group, there was one patient with a tooth injury (0.4% vs 0.3%); all other TI injuries were superficial dermal or mucosal abrasions.
DISCUSSION
In this nation-wide, multicenter RCT with more than 500 prehospital emergency patients with indication for prehospital TI, the McGrathVL and common DL were compared and both were found to be equally successful (98.1% vs 98.5%). These rates of successful prehospital TI were generally in line with those of other studies conducted in experienced users, even though at 83% (DL) and 79% (McGrathVL) the rate of first-pass success seems rather low. It is noteworthy that our strict protocol prompted immediate interruption of laryngoscopy when oxygen saturation dropped below 90%, thus proving that patient safety was given. The present study population equaled that of other prehospital airway trials (26–28). To our knowledge, this is the first proof of equivalence in a “real life” prehospital trial—despite frequent use of a wide range of VLs in prehospital airway management. In a variety of observational case series, cohort studies or retrospective analysis, products of numerous manufacturers (e.g., Pentax, Storz, Prodol) were investigated (29). However, their role in the prehospital environment remained unclear to date. Two recent meta-analyses conclude that VL has not been shown to improve TI outcomes in the EMS setting: Savino et al (30) and Jiang et al (31) identified eight of 470, and 12 of 826 trials, respectively discussing prehospital and emergency video-assisted TI. Both analyses came to comparable results: among physicians with significant DL experience, VL did not increase overall or first-pass success rates and may even lead to worsening performance or outcome (30, 31). Both authors urge that further studies be conducted in order to determine whether VL is beneficial in emergency patients. In light of these findings, we performed this trial comparing the McGrathVL and the DL for prehospital TI as used by HEMS physicians with sufficient experience in VL. VL was introduced in OEAMTC HEMS in 2015 following recommendations made by the German Society for Anesthesiology and Intensive Care Medicine (32) and the Difficult Airway Society (33). All HEMS physicians underwent compulsive manikin and clinical training.
Equivalence of TI success was also shown for subgroups like patients undergoing CPR or TI due to respiratory failure or unconsciousness as well as and, as a trend, also for trauma patients. Interestingly, in trauma patients, especially those with cervical spine immobilization, and in patients undergoing CPR, the first TI attempt was more often successful with the DL than with the McGrathVL. This may contradict results of previous in-hospital (34, 35) and manikin studies (15, 28, 36), but is in accordance with other prehospital investigations (1, 9, 19). The reasons for this unexpected finding are most likely related to the challenging environment at accident sites and the demanding CPR airway management during ongoing or only briefly interrupted chest compressions.
The advantage of better visualization of the glottis when using the McGrathVL is, however, offset by technical problems like fogged camera lens, monitor reflexes and disturbing ambient light and, in addition, by more difficult handling of the tube when using the VL (Table 4; and Supplemental Table 1, Supplemental Digital Content 1, http://links.lww.com/CCM/E834; Supplemental Table 2, Supplemental Digital Content 2, http://links.lww.com/CCM/E835; and Supplemental Table 3, Supplemental Digital Content 3, http://links.lww.com/CCM/E836). This obviously prolonged the TI process: time to first end-tidal Co2 was 48.1 ± 66.2 s for the DL versus 53.8 ± 69.2 s for the McGrathVL. This difference was found especially in trauma patients, but statistical significance was closely missed due to high variance in both groups. The main reasons for failed TI attempts with the McGrathVL were the impossibility to advance the tube into the larynx or trachea, or disturbances caused by ambient light, which was highly significant in trauma patients (in 13.5% of DL patients vs 73.3% of VL patients). Therefore, in outdoor situations with bright sunlight, a DL may be the better choice.
TABLE 4.
Reported Problems (Both Devices)
A prolonged TI time may be hazardous: the guidelines of the European Resuscitation Council recommend only brief interruptions in chest compressions for TI: these should not exceed 5 seconds (1). In patients undergoing CPR, we found a mean time from onset of the TI process to first end-tidal Co2 measurement of 50.0 ± 64.9 s with the DL and 56.0 ± 69.1 s with the McGrathVL (p = 0.28). Thus, it is of the utmost importance to precisely plan and communicate the TI process within the EMS team.
Another main result was found in patients who had a crossover after a first failed TI attempt. Here, the probability of successful TI was 88.2% (DL) or 92% (McGrathVL), whereas the likelihood of TI success for another attempt using the same device turned out to be only 60.0% and 54.8%, respectively (Supplemental Fig. 1, Supplemental Digital Content 4, http://links.lww.com/CCM/E837). The change of the TI method after a first failed attempt was made in all cases based on the clinical assessment of an (experienced) EMS physician, who judged continuation with the randomized device not to be promising when considering patient safety as the highest priority. We thus adopted our institutional airway algorithm and recommend changing the TI method after the first failed attempt in cases with a comparable setting, namely experienced users with equal extensive training with both devices. This could significantly reduce the total number of attempts and facilitate a second-pass success rate of at least 94% in the prehospital environment.
In our opinion, the two devices supplement each other. Advantages of DL can be seen in the greater experience of HEMS staff, and consequently in faster TI performance with the well-known device, even in difficult airway situations. In contrast, the advantages of the McGrathVL are a superior view to the glottis, which occasionally may be offset by technical problems such as fogged camera lens and, mainly, bright ambient light impairing identification of anatomical structures on the monitor. In indoor situations, there was no increase in technical problems as compared with DL (Supplemental Table 1, Supplemental Digital Content 1, http://links.lww.com/CCM/E834; Supplemental Table 2, Supplemental Digital Content 2, http://links.lww.com/CCM/E835; and Supplemental Table 3, Supplemental Digital Content 3, http://links.lww.com/CCM/E836). We therefore strongly recommend that both procedures and their particular pros and cons be taught accordingly during emergency physician training and also ongoing clinical training. If the technical monitor problems can be solved, the first-pass rate with the McGrathVL would be higher. This would presumably mean shorter intubation times and thus a possible advantage of VL in the prehospital setting.
Our study was discontinued following an interim analysis after enrollment of half of the originally targeted patients; this limits the statistical power of our findings within subgroups. Nevertheless, we were able to prove that the two methods are equivalent in all patients. High-quality studies such as RCTs are difficult to perform in the prehospital environment, where human resources are generally limited and patient care is absolutely paramount and often time-critical. In addition, a too long study period may be negative, as other influences such as a personnel change might obviously influence the results. Also, as the study progresses, there is a decrease in the willingness of HEMS physicians and technicians to exert the effort required for a RCT. Nevertheless, these studies are mandatory to examine the value of methods in the reality of prehospital care: the transferability of knowledge gained from hospital or manikin studies is very limited.
CONCLUSIONS
Both devices, the DL and the McGrathVL, are equivalently well suited for prehospital emergency TI of adult patients. Switching the device following a failed first TI attempt was more successful than another attempt with the same device.
ACKNOWLEDGMENTS
We thank all Helicopter Emergency Medical Service physicians and technicians of the OEAMTC Air Rescue for their devoted work, collecting this important data, and having contributed valuable feedback.
Supplementary Material
Footnotes
*See also p.1463.
Drs. Kreutziger and Trimmel drafted, initiated, and designed the study, analyzed and interpreted the data, and drafted the article. Drs. Hornung, Harrer, Urschl, and Doppler assisted in collecting the data and revised the article. Dr. Voelckel participated in concept and design of the study, data interpretation, and critically revised the article. All authors read and approved the final article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
Supported, in part, by OEAMTC Helicopter Emergency Medical Service, who paid patient insurance premiums.
Dr. Trimmel disclosed that the study was funded in part by Oesterreichischer Automobil- und Touring Club, the motorist association of Austria (OEAMTC) Helicopter Emergency Medical Service (patient insurance fees). The remaining authors have disclosed that they do not have any potential conflicts of interest.
Ethics Committee Approval: The study was approved by the Ethics Committee of the State of Lower Austria (GS1-EK-3/124–2016).
REFERENCES
- 1.Soar J, Nolan JP, Böttiger BW, et al. ; Adult advanced life support section Collaborators: European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation 2015; 95:100–147 [DOI] [PubMed] [Google Scholar]
- 2.Wang HE, Kupas DF, Hostler D, et al. Procedural experience with out-of-hospital endotracheal intubation. Crit Care Med 2005; 33:1718–1721 [DOI] [PubMed] [Google Scholar]
- 3.Rhode MG, Vandborg MP, Bladt V, et al. Video laryngoscopy in pre-hospital critical care - a quality improvement study. Scand J Trauma Resusc Emerg Med 2016; 24:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Trimmel H, Beywinkler C, Hornung S, et al. In-hospital airway management training for non-anesthesiologist EMS physicians: A descriptive quality control study. Scand J Trauma Resusc Emerg Med 2017; 25:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Breckwoldt J, Klemstein S, Brunne B, et al. Difficult prehospital endotracheal intubation - predisposing factors in a physician based EMS. Resuscitation 2011; 82:1519–1524 [DOI] [PubMed] [Google Scholar]
- 6.Caruana E, Duchateau FX, Cornaglia C, et al. Tracheal intubation related complications in the prehospital setting. Emerg Med J 2015; 32:882–887 [DOI] [PubMed] [Google Scholar]
- 7.Freund Y, Duchateau FX, Devaud ML, et al. Factors associated with difficult intubation in prehospital emergency medicine. Eur J Emerg Med 2012; 19:304–308 [DOI] [PubMed] [Google Scholar]
- 8.Benumof JL. Management of the difficult adult airway. With special emphasis on awake tracheal intubation. Anesthesiology 1991; 75:1087–1110 [DOI] [PubMed] [Google Scholar]
- 9.Crewdson K, Lockey DJ, Røislien J, et al. The success of pre-hospital tracheal intubation by different pre-hospital providers: A systematic literature review and meta-analysis. Crit Care 2017; 21:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang HE, Schmicker RH, Daya MR, et al. Effect of a strategy of initial laryngeal tube insertion vs endotracheal intubation on 72-hour survival in adults with out-of-hospital cardiac arrest: A randomized clinical trial. JAMA 2018; 320:769–778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Apfelbaum JL, Hagberg CA, Caplan RA, et al. ; American Society of Anesthesiologists Task Force on Management of the Difficult Airway: Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on management of the difficult airway. Anesthesiology 2013; 118:251–270 [DOI] [PubMed] [Google Scholar]
- 12.Lewis SR, Butler AR, Parker J, et al. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation. Cochrane Database Syst Rev 2016; 11:CD011136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Okamoto H, Goto T, Wong ZSY, et al. Comparison of video laryngoscopy versus direct laryngoscopy for intubation in emergency department patients with cardiac arrest: A multicentre study. Resuscitation 2019; 136:70–77 [DOI] [PubMed] [Google Scholar]
- 14.Aziz M, Dillman D, Kirsch JR, et al. Video laryngoscopy with the Macintosh video laryngoscope in simulated prehospital scenarios by paramedic students. Prehosp Emerg Care 2009; 13:251–255 [DOI] [PubMed] [Google Scholar]
- 15.Shippey B, McGuire B, Dalton A. A comparison of the McGRATH video laryngoscope and the Macintosh laryngoscope in patients with cervical spine immobilisation. Anaesthesia 2013; 68:883–886 [Google Scholar]
- 16.Arima T, Nagata O, Miura T, et al. Comparative analysis of airway scope and Macintosh laryngoscope for intubation primarily for cardiac arrest in prehospital setting. Am J Emerg Med 2014; 32:40–43 [DOI] [PubMed] [Google Scholar]
- 17.Trimmel H, Kreutziger J, Fertsak G, et al. Use of the Airtraq laryngoscope for emergency intubation in the prehospital setting: A randomized control trial. Crit Care Med 2011; 39:489–493 [DOI] [PubMed] [Google Scholar]
- 18.Trimmel H, Kreutziger J, Fitzka R, et al. Use of the Glidescope ranger video laryngoscope for emergency intubation in the prehospital setting: A randomized control trial. Crit Care Med 2016; 44:e470–e476 [DOI] [PubMed] [Google Scholar]
- 19.Cavus E, Neumann T, Doerges V, et al. First clinical evaluation of the C-MAC D-Blade videolaryngoscope during routine and difficult intubation. Anesth Analg 2011; 112:382–385 [DOI] [PubMed] [Google Scholar]
- 20.Guyette FX, Farrell K, Carlson JN, et al. Comparison of video laryngoscopy and direct laryngoscopy in a critical care transport service. Prehosp Emerg Care 2013; 17:149–154 [DOI] [PubMed] [Google Scholar]
- 21.Taylor AM, Peck M, Launcelott S, et al. The McGrath® Series 5 videolaryngoscope vs the Macintosh laryngoscope: A randomised, controlled trial in patients with a simulated difficult airway. Anaesthesia 2013; 68:142–147 [DOI] [PubMed] [Google Scholar]
- 22.Tryba M, Brüggemann H, Echtermeyer V. Classification of diseases and injuries in emergency medical services. Notfallmedizin 1980; 6:725–727 [Google Scholar]
- 23.De Jong A, Clavieras N, Conseil M, et al. Implementation of a combo videolaryngoscope for intubation in critically ill patients: A before-after comparative study. Intensive Care Med 2013; 39:2144–2152 [DOI] [PubMed] [Google Scholar]
- 24.Kleine-Brueggeney M, Greif R, Schoettker P, et al. Evaluation of six videolaryngoscopes in 720 patients with a simulated difficult airway: A multicentre randomized controlled trial. Br J Anaesth 2016; 116:670–679 [DOI] [PubMed] [Google Scholar]
- 25.Schulz KF, Altman DG, Moher D; for the CONSORT Group: CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010; 340:c332 [DOI] [PubMed] [Google Scholar]
- 26.Piegeler T, Neth P, Schlaepfer M, et al. Advanced airway management in an anaesthesiologist-staffed Helicopter Emergency Medical Service (HEMS): A retrospective analysis of 1047 out-of-hospital intubations. Resuscitation 2016; 105:66–69 [DOI] [PubMed] [Google Scholar]
- 27.Bernhard M, Hilger T, Sikinger M, et al. Patientenspektrum im Notarztdienst. Anaesthesist 2006; 55:1157–1165 [DOI] [PubMed] [Google Scholar]
- 28.Ruetzler K, Imach S, Weiss M, et al. [Comparison of five video laryngoscopes and conventional direct laryngoscopy: Investigations on simple and simulated difficult airways on the intubation trainer]. Anaesthesist 2015; 64:513–519 [DOI] [PubMed] [Google Scholar]
- 29.Healy DW, Maties O, Hovord D, et al. A systematic review of the role of videolaryngoscopy in successful orotracheal intubation. BMC Anesthesiol 2012; 12:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Savino PB, Reichelderfer S, Mercer MP, et al. Direct versus video laryngoscopy for prehospital intubation: A systematic review and meta-analysis. Acad Emerg Med 2017; 24:1018–1026 [DOI] [PubMed] [Google Scholar]
- 31.Jiang J, Ma D, Li B, et al. Video laryngoscopy does not improve the intubation outcomes in emergency and critical patients - a systematic review and meta-analysis of randomized controlled trials. Crit Care 2017; 21:288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bernhard M, Bein B, Böttiger BW, et al. Handlungsempfehlung zur prähospitalen notfallnarkose beim erwachsenen practice management guideline on prehospital emergency anaesthesia. Notfall+ Rettungsmedizin 2015; 18:395–412 [Google Scholar]
- 33.Frerk C, Mitchell VS, McNarry AF, et al. ; Difficult Airway Society Intubation Guidelines Working Group: Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth 2015; 115:827–848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Malik MA, Maharaj CH, Harte BH, et al. Comparison of Macintosh, Truview EVO2, Glidescope, and Airwayscope laryngoscope use in patients with cervical spine immobilization. Br J Anaesth 2008; 101:723–730 [DOI] [PubMed] [Google Scholar]
- 35.Suppan L, Tramèr MR, Niquille M, et al. Alternative intubation techniques vs Macintosh laryngoscopy in patients with cervical spine immobilization: Systematic review and meta-analysis of randomized controlled trials. Br J Anaesth 2016; 116:27–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Park SO, Shin DH, Lee KR, et al. Efficacy of the Disposcope endoscope, a new video laryngoscope, for endotracheal intubation in patients with cervical spine immobilisation by semirigid neck collar: Comparison with the Macintosh laryngoscope using a simulation study on a manikin. Emerg Med J 2013; 30:270–274 [DOI] [PubMed] [Google Scholar]


