Background:
Pain catastrophizing has been identified as a prognostic indicator of poor outcome following knee arthroplasty. Interventions to address pain catastrophizing, to our knowledge, have not been tested in patients undergoing knee arthroplasty. The purpose of this study was to determine whether pain coping skills training in persons with moderate to high pain catastrophizing undergoing knee arthroplasty improves outcomes 12 months postoperatively compared with usual care or arthritis education.
Methods:
A multicenter, 3-arm, single-blinded, randomized comparative effectiveness trial was performed involving 5 university-based medical centers in the United States. There were 402 randomized participants. The primary outcome was the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Pain Scale, measured at baseline, 2 months, 6 months, and 12 months following the surgical procedure.
Results:
Participants were recruited from January 2013 to June 2016. In 402 participants, 66% were women and the mean age of the participants (and standard deviation) was 63.2 ± 8.0 years. Three hundred and forty-six participants (90% of those who underwent a surgical procedure) completed a 12-month follow-up. All 3 treatment groups had large improvements in 12-month WOMAC pain scores with no significant differences (p > 0.05) among the 3 treatment arms. No differences were found between WOMAC pain scores at 12 months for the pain coping skills and arthritis education groups (adjusted mean difference, 0.3 [95% confidence interval (CI), −0.9 to 1.5]) or between the pain coping and usual-care groups (adjusted mean difference, 0.4 [95% CI, −0.7 to 1.5]). Secondary outcomes also showed no significant differences (p > 0.05) among the 3 groups.
Conclusions:
Among adults with pain catastrophizing undergoing knee arthroplasty, cognitive behaviorally based pain coping skills training did not confer pain or functional benefit beyond the large improvements achieved with usual surgical and postoperative care. Future research should develop interventions for the approximately 20% of patients undergoing knee arthroplasty who experience persistent function-limiting pain.
Level of Evidence:
Therapeutic Level I. See Instructions for Authors for a complete description of levels of evidence.
Knee arthroplasty is the most common major orthopaedic procedure conducted in the United States1, with an estimated 1 million procedures performed in 20152. Although knee arthroplasty is effective at reducing pain and improving function, approximately 20% (that is, approximately 200,000 patients in 2015) report persistent function-limiting pain following recovery from a technically sound procedure3. Persistent pain following knee arthroplasty is associated with patient dissatisfaction3,4 and an increased health-care and socioeconomic burden5.
Prognostic research in knee arthroplasty has focused on modifiable variables associated with poor pain and function outcomes and among the most powerful of these are psychological health indicators, including pain catastrophizing6,7. Pain catastrophizing is a maladaptive approach to coping with pain and is characterized by negative thoughts about pain, rumination about pain, and helplessness in coping with pain8. Many trials of cognitive behavioral treatments for pain have been conducted on patients with a variety of chronic musculoskeletal pain conditions9,10 including knee osteoarthritis11. Although some trials have shown benefits associated with the delivery of pain coping skills training for medically treated knee osteoarthritis12,13, to our knowledge, no study has examined patients who catastrophize about the pain prior to knee arthroplasty.
The primary aim of this randomized controlled trial (RCT) was to compare the effectiveness of pain coping skills training with arthritis education and usual surgical care in patients who were scheduled for knee arthroplasty and reported moderate to high levels of pain catastrophizing. We hypothesized that pain coping skills training would lead to better pain and function outcomes relative to arthritis education or usual surgical care.
Materials and Methods
Study Design, Setting, and Participants
The protocol for our Knee Arthroplasty Pain Coping Skills Training (KASTPain) trial has been published14. The study was a 3-arm RCT conducted at 5 sites (Duke University, New York University Medical Center, Virginia Commonwealth University, Wake Forest University, and Southern Illinois University). The institutional review boards from all sites approved the study. The study was registered at clinicaltrials.gov (NCT01620983).
Potential participants were ≥45 years of age, were diagnosed with osteoarthritis by the treating surgeon, had a knee arthroplasty scheduled 1 to 8 weeks after their consent, scored ≥16 points on the Pain Catastrophizing Scale (PCS)15, and read and spoke English. Patients were excluded if they were scheduled for a revision surgical procedure, had undergone hip or knee arthroplasty within 6 months of the surgical procedure of interest, had a self-reported diagnosis of inflammatory arthritis (for example, rheumatoid arthritis), were scheduled for bilateral knee arthroplasty, planned to undergo hip or knee arthroplasty within 6 months after the currently planned knee arthroplasty, scored ≥20 points on a depression screener (indicating severe clinical depression)16, or scored ≤2 points on a cognitive screener (indicating cognitive deficit)17.
Randomization and Blinding
Following consent and baseline data collection, participants were randomized to usual care, pain coping skills training, or arthritis education. A study statistician generated a random numbers table to permit randomization in permuted block sizes of 3 or 6, stratified by surgeon. This randomization approach ensures that variation attributed to surgeon and site in a variety of known and unknown factors (for example, operative and postoperative anesthesia, pain control, and surgical technique) and not easily controlled would not bias the estimated treatment effects. To avoid potential selection bias, site coordinators used a REDCap (Research Electronic Data Capture) web interface18 to reveal randomized group assignments after baseline data collection. Participants and interventionists were not blinded, but data collectors, surgeons, and investigators were blinded to group assignment.
Interventions
Participants randomized to either pain coping skills training or arthritis education received eight 50-minute sessions of 1-on-1 instruction delivered over an approximate 2-month period beginning approximately 2 weeks preoperatively and ending approximately 6 weeks postoperatively. The first session was an in-person appointment and the remaining sessions occurred via telephone. Behavioral interventions for pain management via telephone have been effective19,20. Pain coping skills training was delivered by local physical therapists with at least 2 years of clinical experience treating patients with knee arthroplasty. Physical therapists attended a 2-day training session conducted by clinical psychologists highly experienced in the delivery of pain coping skills training. Additionally, physical therapists received a detailed training manual to guide treatment delivery, and all treatment sessions were audio-recorded. Local clinical psychologists held monthly conference calls with physical therapists and monitored treatment delivery by listening to audiotapes throughout the study.
Arthritis education was taught by registered nurses with at least 2 years of experience in the care of patients with osteoarthritis. One author trained all nurses using a detailed manual. This treatment arm accounts for treatment effects attributable to substantial time and attention from a caring provider21. By comparing treatment effects in the arthritis education arm with those in the pain coping arm, we were able to determine effects attributable to the presumed active ingredient under study, pain coping skills. All arthritis education treatment sessions were audiotaped and were assessed to confirm fidelity. The arthritis education sessions used a presentation-and-discussion format similar to the approach used by Lorig et al. in their early work on arthritis education22. The usual-care arm was used to estimate real-world effects of knee arthroplasty. For more details, see the protocol14 and the participant and interventionist pain coping and arthritis education training manuals (see Appendix).
Follow-up
Trained data collectors, blinded to treatment group, obtained follow-up data by telephone (using up to 8 attempts) at 2, 6, and 12 months following the surgical procedure; the 12-month data collection session was the primary end point. Participants were compensated $50 at baseline and $80 for completing all follow-up assessments.
Outcome Measures
The primary outcome was the highly reliable and valid Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Pain Scale, 3.1 Likert version, ranging from 0 (no pain with activity) to 20 (extreme pain with activity)23. Secondary outcome measures were the WOMAC Physical Function Scale (ranging from 0 to 68, with higher scores indicating greater functional difficulty), the Pain Catastrophizing Scale (PCS, ranging from 0, indicating no catastrophizing, to 52, indicating high catastrophizing)15, a 4-item knee pain intensity scale ranging from 0 to 1024, and a global rating-of-change scale from −5 (vastly worse) to +5 (completely recovered)25. Performance-based outcome measures were the Short Physical Performance Battery (SPPB) and the 6-minute walk test. The SPPB is a composite measure (ranging from 0 to 12, with higher scores equating to better physical performance)26, and the 6-minute walk test assesses walking endurance and speed27.
Adverse Events
Adverse events were identified either during data collection or via medical record review completed at 12 months postoperatively. Emphasis was placed on psychologically based adverse events because of the cognitive behavioral emphasis of the pain coping skills training.
Sample Size
The required sample size of 321 participants (107 per arm) with 12-month follow-up provided adequate power to detect meaningful differences between pain coping skills training and arthritis education or usual care. Calculations were based on a difference of ≥2 points in the 20-point WOMAC Pain Scale indicating a clinically important difference between groups28. Recruiting a sample size of 107 in each group provided 91% power to detect this difference, assuming an alpha of 0.05 and a common standard deviation of 4.34 (based on pilot work). This effect corresponds to a moderate effect size of 0.46, consistent with the effect of other behavioral interventions for knee arthritis12,29. Accounting for a 20% loss to follow-up, 402 participants were enrolled.
Statistical Analysis
Statistical analyses were completed using an intention-to-treat approach, including all participants14. To test for differences between study groups on each outcome, linear mixed effects models were used. For each outcome, a Gaussian link function was used for all outcomes with the exception of the dichotomous outcome of ≥50% change in WOMAC pain scores, which used a logistic link. These models include the between-subjects group effect, the within-subjects time effect, the group-by-time interaction, and a random intercept term. These models account for the nesting of patients within surgeon and surgeons within site, as well as the within-subjects nature of the data. To account for missing data when analyzing the binary outcome, multiple imputation was used. Predictive mean matching was used to generate 5 imputed data sets whose estimates were combined to provide final model results via the mice package in R (R Foundation for Statistical Computing)30. Imputed variables used in the logistic model were sex, race, age, and baseline WOMAC pain. Both methods account for data missing at random31. An alpha of 0.05 was used for all tests.
Prespecified moderators (depressive symptoms, surgical expectations, self-efficacy, social support) and a post hoc moderator (pain catastrophizing) of the treatment effect on the primary outcome were examined by testing for a moderator by treatment interaction in individual models. To control for the familywise type-I error, follow-up comparisons of treatment differences were only made if appropriate omnibus tests were significant. The lme4 package in the R statistical software was used to fit all models32.
Results
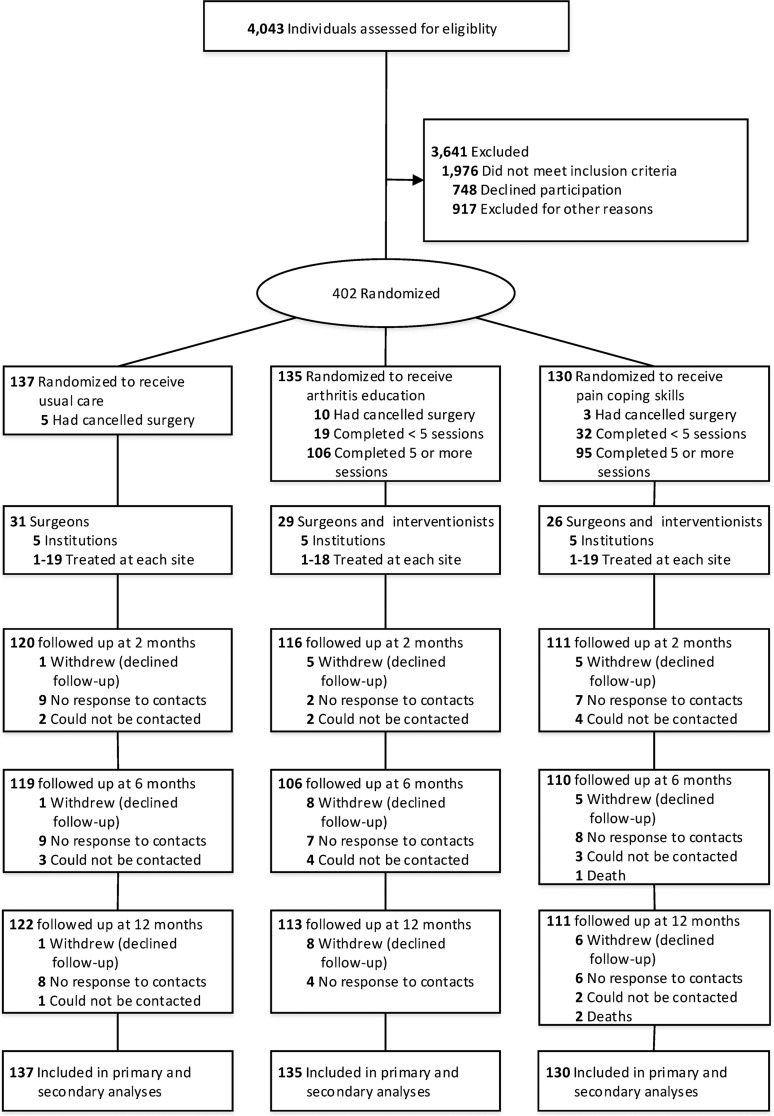
Participant flow is reported in Figure 1. From January 2013 to June 2016, 4,043 patients were considered for screening. Of 402 participants who consented, 18 had the surgical procedure canceled. A total of 367 participants underwent total knee arthroplasty, and 17 participants had unicompartmental knee arthroplasty. Thirty-two surgeons performed knee arthroplasties, with the number of patients treated by each surgeon ranging from 1 to 54. Unicompartmental knee arthroplasty was added to the protocol approximately 6 months after recruitment began.
Fig. 1.
CONSORT (Consolidated Standards of Reporting Trials) flowchart of participants comparing pain coping skills training with arthritis education and usual surgical care for recovery following knee arthroplasty.
Four sites each received consent from 94 to 108 participants, and 1 site received consent from 5 participants. Of the 130 participants assigned to pain coping skills training, 73% (95 participants) received ≥5 of 8 treatment sessions, an a priori indicator of good adherence. Of the 135 participants randomized to the arthritis education arm, 79% (106 participants) received ≥5 treatment sessions. The overall follow-up response rates were 86% (347 participants) at 2 months, 83% (335 participants) at 6 months, and 86% (346 participants) at 12 months. Among the 384 participants who had knee arthroplasty, the 12-month follow-up was 90%.
The median knee pain duration was 6 years (interquartile range, 3 to 12 years), and the mean WOMAC pain score (and standard deviation) was 11.4 ± 3.4 points, indicating moderate to severe function-limiting knee pain (Table I). Surgical methods and implant type were similar across sites (see Appendix). No significant differences between baseline characteristics were found (all p > 0.05), allowing for the linear mixed effects models to be fit without covariates.
TABLE I.
Baseline Sample Characteristics (N = 402)
| Baseline Characteristics | All (N = 402) | Usual Care (N = 137) | Arthritis Education (N = 135) | Pain Coping Skills (N = 130) |
| Age* (yr) | 63.2 ± 8.0 | 62.7 ± 7.7 | 64.2 ± 8.5 | 62.6 ± 7.9 |
| Female sex† | 267 (66%) | 88 (64%) | 85 (63%) | 94 (72%) |
| Body mass index* (kg/m2) | 32.3 ± 6.2 | 32.6 ± 6.5 | 31.7 ± 6.0 | 32.4 ± 6.1 |
| Race or ethnic group†‡ | ||||
| White | 249 (59%) | 86 (60%) | 83 (59%) | 80 (59%) |
| African American | 143 (34%) | 48 (34%) | 45 (32%) | 50 (37%) |
| Hispanic | 13 (3%) | 5 (3%) | 5 (4%) | 3 (2%) |
| Asian | 8 (2%) | 2 (1%) | 4 (3%) | 2 (1%) |
| Declined to answer§ | 6 (1%) | 2 (1%) | 4 (3%) | — |
| Current income† | ||||
| <$10,000 | 42 (10%) | 14 (10%) | 12 (9%) | 16 (12%) |
| $10,000 to $24,999 | 84 (21%) | 28 (20%) | 30 (22%) | 26 (20%) |
| $25,000 to $49,999 | 91 (23%) | 27 (20%) | 31 (23%) | 33 (25%) |
| $50,000 to $99,999 | 94 (23%) | 35 (26%) | 33 (24%) | 26 (20%) |
| ≥$100,000 | 53 (13%) | 18 (13%) | 16 (12%) | 19 (15%) |
| Declined to answer§ | 38 (10%) | 15 (11%) | 13 (10%) | 10 (8%) |
| Current work status† | ||||
| Employed | 132 (33%) | 45 (33%) | 42 (31%) | 45 (35%) |
| Not working in part due to health problems | 102 (25%) | 36 (26%) | 32 (24%) | 34 (26%) |
| Not working for other reasons | 167 (42%) | 56 (41%) | 60 (44%) | 51 (39%) |
| Declined to answer§ | 1 (0.2%) | — | 1 (1%) | — |
| Education† | ||||
| Less than high school | 26 (7%) | 10 (7%) | 8 (6%) | 8 (6%) |
| High school graduate | 91 (23%) | 35 (26%) | 33 (24%) | 23 (18%) |
| Some college | 103 (26%) | 40 (29%) | 31 (23%) | 32 (25%) |
| College degree or higher | 182 (45%) | 52 (38%) | 63 (47%) | 67 (52%) |
| Marital status† | ||||
| Married | 197 (49%) | 70 (51%) | 64 (47%) | 63 (49%) |
| Divorced | 80 (20%) | 26 (19%) | 26 (19%) | 28 (22%) |
| Never married | 49 (12%) | 19 (14%) | 10 (7%) | 20 (15%) |
| Widowed | 47 (12%) | 15 (11%) | 18 (13%) | 14 (11%) |
| Separated | 20 (5%) | 5 (4%) | 13 (10%) | 2 (2%) |
| Member of an unmarried couple | 7 (2%) | 1 (1%) | 3 (2%) | 3 (2%) |
| Declined to answer§ | 2 (1%) | 1 (1%) | 1 (1%) | — |
| Current smoker (yes)† | 47 (12%) | 19 (14%) | 12 (9%) | 16 (12%) |
| Health history | ||||
| Modified Charlson Comorbidity Index*# | 8.7 ± 4.1 | 8.8 ± 4.2 | 8.7 ± 4.0 | 8.7 ± 4.1 |
| Knee pain duration** (yr) | 6 (3 to 15) | 8 (3 to 20) | 6 (3 to 12) | 6 (3 to 12) |
| Opioid use at baseline† | 121 (30%) | 48 (35%) | 37 (27%) | 36 (28%) |
| Unicompartmental knee arthroplasty (yes)† | 17 (4%) | 8 (6%) | 5 (4%) | 4 (3%) |
| Psychological health* | ||||
| Patient Health Questionnaire (PHQ-8)†† | 6.0 ± 5.0 | 5.9 ± 5.2 | 6.1 ± 5.0 | 5.8 ± 4.8 |
| Generalized Anxiety Disorder Scale (GAD-7)‡‡ | 5.4 ± 4.9 | 5.6 ± 4.9 | 5.2 ± 5.1 | 5.3 ± 4.8 |
| Arthritis Self-Efficacy Scale*§§ | 49.1 ± 17.8 | 51.6 ± 18.5 | 50.4 ± 17.7 | 45.1 ± 16.7 |
| Primary outcome scores* | ||||
| WOMAC Pain Scale## (points) | 11.4 ± 3.4 | 11.4 ± 3.5 | 11.3 ± 3.5 | 11.6 ± 3.1 |
| Secondary outcome scores* | ||||
| WOMAC physical function*** | 37.2 ± 11.6 | 36.0 ± 11.1 | 37.1 ± 11.8 | 38.6 ± 11.8 |
| Numeric pain rating* | 6.1 ± 1.9 | 6.2 ± 1.9 | 6.0 ± 2.0 | 6.0 ± 1.8 |
| SPPB††† | 9.3 ± 2.9 | 9.7 ± 2.6 | 9.1 ± 2.9 | 9.1 ± 3.2 |
| 6-minute walk test (m) | 297 ± 120 | 309 ± 106 | 279 ± 132 | 305 ± 121 |
| PCS‡‡‡ (points) | 30.0 ± 9.3 | 29.7 ± 9.2 | 30.0 ± 9.2 | 30.4 ± 9.6 |
The values are given as the mean and the standard deviation.
The values are given as the number of patients, with the percentage in parentheses.
In the race or ethnic group category, the sums are greater than the total sample (n = 402) because some subjects marked >1 category. The sum may equal >100% because of multiple categories.
This category indicates not specified or missing.
The modified Charlson Comorbidity Index score range is 0 to 45 points; higher scores indicate greater comorbidity burden.
The values are given as the median, with the interquartile range in parentheses.
The PHQ-8 score range is 0 to 24 points; higher scores indicate more depressive symptoms.
The GAD-7 score range is 0 to 21 points; higher scores indicate more anxiety.
The Arthritis Self-Efficacy Scale score range is 0 to 80 points; higher scores indicate more self-efficacy.
The WOMAC Pain Scale score range is 0 to 20 points; higher scores indicate more function-limiting pain.
The WOMAC Physical Function Scale range is 0 to 68 points; higher scores indicate more difficulty with functional activities.
The Short Physical Performance Battery (SPPB) score range is 0 to 12 points; higher scores indicate better performance.
The Pain Catastrophizing Scale (PCS) range is 0 to 52 points; higher scores indicate more pain catastrophizing.
Effects on Primary Outcome
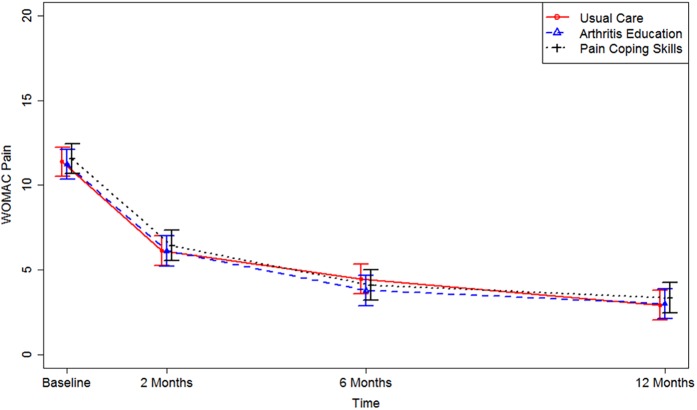
No significant treatment (p = 0.60) or group-by-time interaction (p = 0.73) was found, indicating no significant difference between groups (collapsed over time) or in the trajectories of the WOMAC pain score over time (Fig. 2). There was a significant effect of time (p < 0.001) indicating improvement in pain for each group. Notably, the effect size ([pooled baseline – 12-month WOMAC pain score]/pooled baseline standard deviation of the difference score) was very large (2.0). The adjusted mean WOMAC pain scores for the 3 groups at the primary end point of 12 months postoperatively were not significantly different (p > 0.05) (adjusted score of 3.4 points for the pain coping group, 3.1 points for the arthritis education group, and 2.9 points for the usual care group). The adjusted mean differences were 0.3 (95% confidence interval [CI], −0.9 to 1.5) between pain coping skills and arthritis education and 0.4 (95% CI, −0.7 to 1.5) between pain coping skills and usual surgical care. As stated in our protocol14, we compared the results for the full analysis with those for patients who actually underwent the surgical procedure, and no differences were found (data not shown). Likewise, when WOMAC pain scores were dichotomized on the basis of whether improvement at 12 months was ≥50% or <50%, the analysis revealed no significant differences (p > 0.05) (see Appendix).
Fig. 2.
Adjusted mean WOMAC pain scores for the 3 treatment groups over the study period. The bars for each line indicate the 95% CIs.
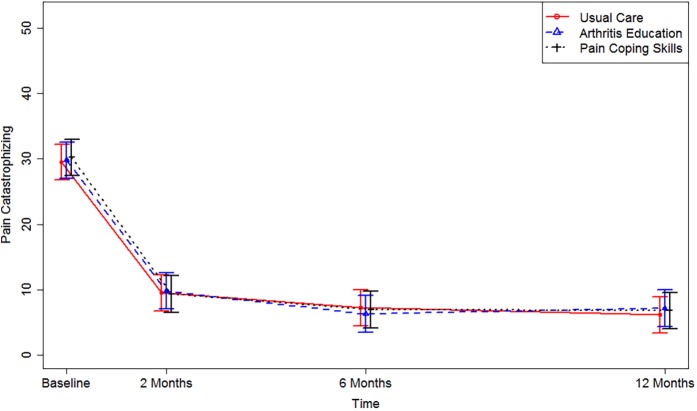
Effects on Secondary Outcomes and Potential Moderators
No significant group or group-by-time interactions (p > 0.05) were found among WOMAC physical function, pain catastrophizing, composite pain, or SPPB scores (Table II). Substantial improvements over 12 months were noted for WOMAC physical function scores (pooled effect size, 1.8) and pain catastrophizing (pooled effect size, 2.0) (Fig. 3). There was a significant group effect on 6-minute walk scores (p = 0.04) but no significant interaction (p = 0.96). Prespecified and post hoc potential moderators (that is, treatment expectations, self-efficacy, social support, depressive symptoms, and pain catastrophizing, all measured at baseline)14 were not significant predictors (p > 0.05) of treatment effect for 1-year WOMAC pain (data not shown).
Fig. 3.
Adjusted mean PCS scores for the 3 treatment groups over the study period. The bars for each line indicate the 95% CIs.
TABLE II.
Outcomes for the 3 Treatment Conditions for All Time Points
| Outcome | Usual Care* | Arthritis Education* | Pain Coping Skills* |
| Primary outcome | |||
| WOMAC Pain Scale | |||
| Baseline | 11.4 (10.5 to 12.2) | 11.2 (10.4 to 12.1) | 11.6 (10.7 to 12.4) |
| 2 months | 6.1 (5.3 to 7.0) | 6.1 (5.2 to 7.0) | 6.4 (5.5 to 7.3) |
| 6 months | 4.4 (3.6 to 5.3) | 3.8 (2.9 to 4.7) | 4.1 (3.2 to 5.0) |
| 12 months | 2.9 (2.0 to 3.8) | 3.0 (2.1 to 3.8) | 3.3 (2.5 to 4.2) |
| Secondary outcomes | |||
| WOMAC physical function | |||
| Baseline | 36.0 (32.9 to 39.1) | 37.1 (34.0 to 40.2) | 38.6 (35.5 to 41.7) |
| 2 months | 21.2 (18.1 to 24.4) | 19.5 (16.3 to 22.7) | 22.5 (19.2 to 25.7) |
| 6 months | 15.4 (12.3 to 18.6) | 14.7 (11.5 to 17.9) | 15.2 (12.0 to 18.4) |
| 12 months | 10.5 (7.4 to 13.6) | 11.7 (8.6 to 14.9) | 12.2 (9.0 to 15.4) |
| Numeric pain rating | |||
| Baseline | 6.1 (5.6 to 6.7) | 5.9 (5.4 to 6.5) | 6.0 (5.4 to 6.6) |
| 2 months | 3.4 (2.8 to 4.0) | 3.1 (2.5 to 3.7) | 3.1 (2.6 to 3.7) |
| 6 months | 2.3 (1.8 to 2.9) | 2.2 (1.6 to 2.8) | 2.2 (1.6 to 2.8) |
| 12 months | 1.7 (1.1 to 2.2) | 2.0 (1.3 to 2.6) | 1.8 (1.2 to 2.4) |
| SPPB | |||
| Baseline | 7.9 (7.0 to 8.9) | 7.5 (6.6 to 8.5) | 7.6 (6.7 to 8.5) |
| 12 months | 8.6 (7.8 to 9.4) | 8.0 (7.2 to 8.7) | 8.4 (7.6 to 9.1) |
| 6-minute walk test (m) | |||
| Baseline | 304 (282 to 325) | 274 (252 to 296) | 301 (279 to 324) |
| 12 months | 363 (340 to 387) | 337 (313 to 362) | 366 (341 to 391) |
| Pain catastrophizing | |||
| Baseline | 29.5 (26.7 to 32.2) | 29.8 (27.1 to 32.6) | 30.2 (27.5 to 33.0) |
| 2 months | 9.5 (6.8 to 12.3) | 9.8 (7.0 to 12.6) | 9.3 (6.5 to 12.1) |
| 6 months | 7.2 (4.5 to 10.0) | 6.3 (3.5 to 9.1) | 6.9 (4.1 to 9.7) |
| 12 months | 6.1 (3.4 to 8.9) | 7.2 (4.4 to 10.0) | 6.8 (4.0 to 9.6) |
| Global rating of change | |||
| 2 months | 2.9 (2.3 to 3.4) | 2.9 (2.4 to 3.5) | 2.8 (2.3 to 3.3) |
| 6 months | 3.6 (3.0 to 4.1) | 3.7 (3.1 to 4.2) | 3.0 (2.5 to 3.6) |
| 12 months | 4.1 (3.6 to 4.6) | 3.8 (3.3 to 4.3) | 3.6 (3.1 to 4.2) |
The values are given as the mean estimate (from the linear mixed effect model), with the 95% CI in parentheses.
Intervention Fidelity
After study completion, a pain psychologist not involved with the study reviewed a random set of 5% of pain coping skills training audiotapes and rated proficiency of care delivery, based on the treatment manual, on a 5-point scale (1 = poor to 5 = excellent). A joint arthroplasty nurse not affiliated with the study used a similar rating for arthritis education audiotapes. The mean quality rating was 4.0 (range, 3.5 to 4.5) for pain coping skills training and 3.8 (range, 2.0 to 5.0) for arthritis education training. These data support intervention treatment fidelity.
Adverse Events
Serious adverse events and other adverse events associated with knee replacement and other hospitalizations were not significantly different (p > 0.05) across treatment arms (Table III). Two deaths occurred in participants assigned to the pain coping skills group. In 1 case, the cause of death was reported by the family to be due to natural causes, and in the other case, the cause of death could not be determined. The National Institutes of Health (NIH)-appointed Data and Safety Monitoring Board adjudicated these deaths and found them to be unrelated to the intervention.
TABLE III.
Serious Adverse Events and Adverse Events at 12 Months Postoperatively in Participants Who Underwent Knee Arthroplasty (N = 384)
| All* (N = 384) | Usual Care* (N = 132) | Arthritis Education* (N = 125) | Pain Coping Skills* (N = 127) | |
| Serious adverse events† | 100 | 28 | 36 | 36 |
| Venous thromboembolism | 8 | 3 | 2 | 3 |
| Infection of index knee | 4 | 1 | 1 | 2 |
| Other non-knee orthopaedic surgery‡ | 7 | 5 | 2 | 0 |
| Hospitalization (psychological distress) | 2 | 1 | 1 | 0 |
| Hospitalization (other)§ | 20 | 7 | 6 | 7 |
| Urinary tract infection | 1 | 0 | 1 | 0 |
| Revision or other surgery of index knee | 7 | 1 | 3 | 3 |
| Manipulation of index knee | 17 | 3 | 7 | 7 |
| Contralateral knee replacement | 32 | 7 | 13 | 12 |
| Death | 2 | 0 | 0 | 2 |
| Adverse events# | 20 | 9 | 3 | 8 |
| Patient Health Questionnaire (PHQ-8) score >19 | 10 | 6 | 1 | 3 |
| Verbal report of psychological distress | 5 | 2 | 1 | 2 |
| Shortness of breath | 1 | 0 | 0 | 1 |
| Twisted knee | 1 | 1 | 0 | 0 |
| Fractured patella | 1 | 0 | 0 | 1 |
| Emergency room visit for knee pain | 2 | 0 | 1 | 1 |
The values are given as the number of participants.
These values were not significant at p = 0.330, determined with use of the Fisher exact test.
Other orthopaedic surgical procedures were lumbar fusion (n = 1) and to treat hip fracture (n = 1), malleolar fracture (n = 1), tibial fracture (n = 1), and shoulder injury (n = 1).
Other hospitalization reasons included heart failure, anemia, cellulitis, angioplasty, pacemaker, and cyst removal, among others.
These values were not significant at p = 0.190, determined with use of the Fisher exact test.
Discussion
No significant differences between treatment groups were found for any outcome. The unadjusted mean WOMAC pain scores at 12 months following the surgical procedure for all participants were 73% lower (improved) compared with preoperative scores, indicating that knee arthroplasty was associated with a substantial reduction in function-limiting pain. Beneficial effects associated with a surgical procedure were so substantial (effect sizes of 2.0 for WOMAC pain scores and 1.8 for WOMAC physical function scores) that, despite several hours of contact with a caring practitioner in both treatment groups and, in the case of pain coping skills, an intervention with known beneficial effects for patients with chronic pain12, these treatment groups demonstrated no beneficial effects beyond those experienced by the usual care group. Beneficial effects attributed to knee arthroplasty appeared to preclude even placebo responses associated with treatment delivery and caring-practitioner interaction21.
Approximately 20% of patients who undergo knee arthroplasty experience poor outcome3, and some of these cases are attributed to preoperative psychological distress including pain catastrophizing7. In our study, all groups improved on the WOMAC Pain Scale to the extent that, at 12 months following the surgical procedure, the mean score for all 3 groups was 3.1 ± 3.7 points. A score of 3 on the WOMAC Pain Scale is equivalent to a report of mild pain with standing, walking, and climbing steps and is consistent with 12-month outcomes from several large U.S.-based and international cohort studies of patients undergoing knee arthroplasty33-35. Our data run counter to prior evidence6,7,36,37 and suggest that preoperative knee arthroplasty pain catastrophizing, using PCS cutoff scores of ≥16, is likely not a viable therapeutic target for improving knee arthroplasty outcomes. Alternatively, all 3 groups had such large improvements in pain catastrophizing that the cognitive behaviorally based intervention could not generate further benefits beyond that provided by the surgical procedure and usual care.
In 2 post hoc analyses, we compared 12-month outcomes of the 3 treatment groups for participants completing >4 treatment sessions (that is, per-protocol analysis) and with unicompartmental arthroplasty excluded (n = 17). No differences in the primary outcome were found for either analysis (see Appendix). Adverse events occurred at a rate that was expected38, with no significant differences among the 3 treatment groups.
The limitations of our study warrant discussion. First, our participants had moderate to high levels of pain catastrophizing and were recruited from academic medical centers. Results may not generalize to individuals with low levels of pain catastrophizing or patients treated by community-based orthopaedic surgeons. Second, pain coping skills treatment sessions were delivered primarily by telephone. Although telephone-based delivery of cognitive behavioral treatment has been shown to be effective12,39, study findings may not generalize to in-person pain coping skills training. Third, pain coping skills training was not delivered by the same physical therapists providing physical therapy following participants’ surgical procedures. It is possible that physical therapists providing physical rehabilitation following knee arthroplasty will more effectively deliver pain coping skills. Finally, interventionists were not blinded to treatment group.
In conclusion, we found that pain coping skills training was not an effective perioperative treatment for patients who are undergoing knee arthroplasty and catastrophize about pain. Pain catastrophizing scores of ≥16 points, as measured with the PCS, are not prognostic of poor outcome following knee arthroplasty. Future study is needed both to identify prognostic variables that predict poor outcome following knee arthroplasty and to design and test interventions to improve outcomes for those at risk for poor outcome.
Appendix
Tables showing the summary of surgical data from the KASTPain sample, the dichotomous outcome of ≥50% improvement in WOMAC pain scores over the study period, post hoc analysis comparing the 3 treatment groups after excluding participants with ≤4 treatment sessions (per-protocol analysis), and post hoc analysis comparing the 3 treatment groups after excluding participants with unicompartmental arthroplasty are available with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/F122). Arthritis education manuals for nurses and patients are also available with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/F123).
Acknowledgments
Note: The authors thank the participants who enrolled in this study. They also thank the physical therapists and nurses for their role in providing the interventions under study, as well as study staff and study psychologists, at Duke University, New York University, Southern Illinois University, Virginia Commonwealth University, and Wake Forest University.
Footnotes
Disclosure: This study was funded by grants from the National Institutes of Health (NIH) National Center for Advancing Translational Sciences (UL1TR000058) and the National Institute of Arthritis Musculoskeletal and Skin Diseases (NIAMS) (UM1AR062800). One author of this study (S.D.R.) also received personal fees as a consultant for Virginia Commonwealth University to conduct an economic evaluation of the intervention. The NIH or NIAMS had no role in the design, conduct, or presentation of study findings. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJS/F121).
References
- 1.Steiner CA, Karaca Z, Moore BJ, Imshaug MC, Pickens G. Surgeries in hospital-based ambulatory surgery and hospital inpatient settings, 2014: statistical brief #223. 2017. February https://hcup-us.ahrq.gov/reports/statbriefs/sb223-Ambulatory-Inpatient-Surgeries-2014.pdf. Accessed 2018 Sep 24. [PubMed]
- 2.Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014. April 16;96(8):624-30. [DOI] [PubMed] [Google Scholar]
- 3.Wylde V, Bruce J, Beswick A, Elvers K, Gooberman-Hill R. Assessment of chronic postsurgical pain after knee replacement: a systematic review. Arthritis Care Res (Hoboken). 2013. November;65(11):1795-803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baker PN, van der Meulen JH, Lewsey J, Gregg PJ; National Joint Registry for England and Wales; Data from the National Joint Registry for England and Wales. The role of pain and function in determining patient satisfaction after total knee replacement. J Bone Joint Surg Br. 2007. July;89(7):893-900. [DOI] [PubMed] [Google Scholar]
- 5.Jeffery AE, Wylde V, Blom AW, Horwood JP. “It’s there and I’m stuck with it”: patients’ experiences of chronic pain following total knee replacement surgery. Arthritis Care Res (Hoboken). 2011. February;63(2):286-92. [DOI] [PubMed] [Google Scholar]
- 6.Dave AJ, Selzer F, Losina E, Usiskin I, Collins JE, Lee YC, Band P, Dalury DF, Iorio R, Kindsfater K, Katz JN. The association of pre-operative body pain diagram scores with pain outcomes following total knee arthroplasty. Osteoarthritis Cartilage. 2017. May;25(5):667-75. Epub 2016 Dec 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vissers MM, Bussmann JB, Verhaar JA, Busschbach JJ, Bierma-Zeinstra SM, Reijman M. Psychological factors affecting the outcome of total hip and knee arthroplasty: a systematic review. Semin Arthritis Rheum. 2012. February;41(4):576-88. Epub 2011 Oct 28. [DOI] [PubMed] [Google Scholar]
- 8.Turner JA, Aaron LA. Pain-related catastrophizing: what is it? Clin J Pain. 2001. March;17(1):65-71. [DOI] [PubMed] [Google Scholar]
- 9.Dixon KE, Keefe FJ, Scipio CD, Perri LM, Abernethy AP. Psychological interventions for arthritis pain management in adults: a meta-analysis. Health Psychol. 2007. May;26(3):241-50. [DOI] [PubMed] [Google Scholar]
- 10.Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2012. November 14;11:CD007407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Somers TJ, Blumenthal JA, Guilak F, Kraus VB, Schmitt DO, Babyak MA, Craighead LW, Caldwell DS, Rice JR, McKee DC, Shelby RA, Campbell LC, Pells JJ, Sims EL, Queen R, Carson JW, Connelly M, Dixon KE, Lacaille LJ, Huebner JL, Rejeski WJ, Keefe FJ. Pain coping skills training and lifestyle behavioral weight management in patients with knee osteoarthritis: a randomized controlled study. Pain. 2012. June;153(6):1199-209. Epub 2012 Apr 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Broderick JE, Keefe FJ, Bruckenthal P, Junghaenel DU, Schneider S, Schwartz JE, Kaell AT, Caldwell DS, McKee D, Reed S, Gould E. Nurse practitioners can effectively deliver pain coping skills training to osteoarthritis patients with chronic pain: a randomized, controlled trial. Pain. 2014. September;155(9):1743-54. Epub 2014 May 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rini C, Porter LS, Somers TJ, McKee DC, DeVellis RF, Smith M, Winkel G, Ahern DK, Goldman R, Stiller JL, Mariani C, Patterson C, Jordan JM, Caldwell DS, Keefe FJ. Automated internet-based pain coping skills training to manage osteoarthritis pain: a randomized controlled trial. Pain. 2015. May;156(5):837-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Riddle DL, Keefe FJ, Ang D, J K, Dumenci L, Jensen MP, Bair MJ, Reed SD, Kroenke K. A phase III randomized three-arm trial of physical therapist delivered pain coping skills training for patients with total knee arthroplasty: the KASTPain protocol. BMC Musculoskelet Disord. 2012. August 20;13:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1996;7(4):524-32. [Google Scholar]
- 16.Kroenke K, Spitzer RL, Williams JB, Löwe B. The Patient Health Questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010. Jul-Aug;32(4):345-59. Epub 2010 May 7. [DOI] [PubMed] [Google Scholar]
- 17.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002. September;40(9):771-81. [DOI] [PubMed] [Google Scholar]
- 18.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009. April;42(2):377-81. Epub 2008 Sep 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Allen KD, Oddone EZ, Coffman CJ, Datta SK, Juntilla KA, Lindquist JH, Walker TA, Weinberger M, Bosworth HB. Telephone-based self-management of osteoarthritis: a randomized trial. Ann Intern Med. 2010. November 2;153(9):570-9. [DOI] [PubMed] [Google Scholar]
- 20.McBeth J, Prescott G, Scotland G, Lovell K, Keeley P, Hannaford P, McNamee P, Symmons DP, Woby S, Gkazinou C, Beasley M, Macfarlane GJ. Cognitive behavior therapy, exercise, or both for treating chronic widespread pain. Arch Intern Med. 2012. January 9;172(1):48-57. Epub 2011 Nov 14. [DOI] [PubMed] [Google Scholar]
- 21.Kaptchuk TJ, Kelley JM, Conboy LA, Davis RB, Kerr CE, Jacobson EE, Kirsch I, Schyner RN, Nam BH, Nguyen LT, Park M, Rivers AL, McManus C, Kokkotou E, Drossman DA, Goldman P, Lembo AJ. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ. 2008. May 3;336(7651):999-1003. Epub 2008 Apr 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lorig K, Konkol L, Gonzalez V. Arthritis patient education: a review of the literature. Patient Educ Couns. 1987. December;10(3):207-52. [DOI] [PubMed] [Google Scholar]
- 23.McConnell S, Kolopack P, Davis AM. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC): a review of its utility and measurement properties. Arthritis Rheum. 2001. October;45(5):453-61. [DOI] [PubMed] [Google Scholar]
- 24.Jensen MP, Turner JA, Romano JM, Fisher LD. Comparative reliability and validity of chronic pain intensity measures. Pain. 1999. November;83(2):157-62. [DOI] [PubMed] [Google Scholar]
- 25.Kamper SJ, Maher CG, Mackay G. Global rating of change scales: a review of strengths and weaknesses and considerations for design. J Man Manip Ther. 2009;17(3):163-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994. March;49(2):M85-94. [DOI] [PubMed] [Google Scholar]
- 27.Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, Berman LB. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985. April 15;132(8):919-23. [PMC free article] [PubMed] [Google Scholar]
- 28.Angst F, Aeschlimann A, Steiner W, Stucki G. Responsiveness of the WOMAC Osteoarthritis Index as compared with the SF-36 in patients with osteoarthritis of the legs undergoing a comprehensive rehabilitation intervention. Ann Rheum Dis. 2001. September;60(9):834-40. [PMC free article] [PubMed] [Google Scholar]
- 29.Nuñez M, Nuñez E, Segur JM, Macule F, Quinto L, Hernandez MV, Vilalta C. The effect of an educational program to improve health-related quality of life in patients with osteoarthritis on waiting list for total knee replacement: a randomized study. Osteoarthritis Cartilage. 2006. March;14(3):279-85. Epub 2005 Nov 23. [DOI] [PubMed] [Google Scholar]
- 30.van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained qquations in R. J Stat Softw. 2011;45(3). [Google Scholar]
- 31.Wothke W. Longitudinal and multigroup modeling with missing data. In: Little TD, Schnabel KU, Baumert J, editors. Modeling longitudinal and multilevel data: practical issues, applied approaches, and specific examples. Mahwah: Lawrence Erlbaum Associates; 2000. p 219-40. [Google Scholar]
- 32.Bates D, Machler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67(1):1-48. [Google Scholar]
- 33.Collins JE, Donnell-Fink LA, Yang HY, Usiskin IM, Lape EC, Wright J, Katz JN, Losina E. Effect of obesity on pain and functional recovery following total knee arthroplasty. J Bone Joint Surg Am. 2017. November 1;99(21):1812-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dowsey MM, Robertsson O, Sundberg M, Lohmander LS, Choong PFM, W-Dahl A Variations in pain and function before and after total knee arthroplasty: a comparison between Swedish and Australian cohorts. Osteoarthritis Cartilage. 2017. June;25(6):885-91. Epub 2016 Dec 20. [DOI] [PubMed] [Google Scholar]
- 35.Lingard EA, Katz JN, Wright EA, Sledge CB; Kinemax Outcomes Group. Predicting the outcome of total knee arthroplasty. J Bone Joint Surg Am. 2004. October;86(10):2179-86. [DOI] [PubMed] [Google Scholar]
- 36.Riddle DL, Wade JB, Jiranek WA, Kong X. Preoperative pain catastrophizing predicts pain outcome after knee arthroplasty. Clin Orthop Relat Res. 2010. March;468(3):798-806. Epub 2009 Jul 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sullivan M, Tanzer M, Stanish W, Fallaha M, Keefe FJ, Simmonds M, Dunbar M. Psychological determinants of problematic outcomes following total knee arthroplasty. Pain. 2009. May;143(1-2):123-9. Epub 2009 Mar 21. [DOI] [PubMed] [Google Scholar]
- 38.Siracuse BL, Ippolito JA, Gibson PD, Ohman-Strickland PA, Beebe KS. A preoperative scale for determining surgical readmission risk after total knee arthroplasty. J Bone Joint Surg Am. 2017. November 1;99(21):e112. [DOI] [PubMed] [Google Scholar]
- 39.Moore JE, Von Korff M, Cherkin D, Saunders K, Lorig K. A randomized trial of a cognitive-behavioral program for enhancing back pain self care in a primary care setting. Pain. 2000. November;88(2):145-53. [DOI] [PubMed] [Google Scholar]