Abstract
Background:
Evidence on the association between road traffic noise and diabetes risk is sparse and inconsistent with respect to how confounding by air pollution was treated.
Objectives:
In this study, we aimed to examine whether long-term exposure to road traffic noise over 25 years is associated with incidence of diabetes, independent of air pollution.
Methods:
A total of 28,731 female nurses from the Danish Nurse cohort ( at recruitment in 1993 or 1999) were linked to the Danish National Diabetes Register with information on incidence of diabetes from 1995 until 2013. The annual mean weighted levels of 24-h average road traffic noise () at nurses’ residences from 1970 until 2013 were estimated with the Nord2000 method and annual mean levels of particulate matter (PM) with diameter and ( and ), nitrogen dioxide (), and nitrogen oxide () with the Danish AirGIS modeling system. Cox proportional hazards regression models were used to examine the association between residential in four different exposure windows (1-, 5-, 10-, and 25-years) and the incidence of diabetes, adjusted for lifestyle factors and air pollutants.
Results:
Of 23,762 nurses free of diabetes at the cohort baseline, 1,158 developed diabetes during a mean follow-up of 15.2 years. We found weak positive associations between 5-y mean exposure to (per increase) and diabetes incidence in a crude model [hazard ratio (HR): 1.07; 95% confidence interval (CI): 0.99, 1.12], which attenuated in a model adjusted for lifestyle factors (HR:1.04; 95% CI: 0.97, 1.12), and reached unity after additional adjustment for (HR: 0.99; 0.91, 1.08). In analyses by level of urbanization, we found a positive association between noise and diabetes in urban areas (HR:1.27; 95% CI: 0.98, 1.63) that was unchanged after adjusting for (HR: 1.25; 95% CI: 0.97, 1.62), but we found no apparent association in provincial (HR: 1.02; 95% CI: 0.88, 1.18) or rural areas (HR: 0.97; 95% CI: 0.87, 1.08).
Conclusion:
In the nationwide cohort of Danish nurses 44 years of age and older, we found no association between long-term exposure to road traffic noise and diabetes incidence after adjustment for but found suggestive evidence of an association limited to urban areas. https://doi.org/10.1289/EHP4389
Introduction
Well-established risk factors for type 2 diabetes include poor dietary habits, physical inactivity, being overweight, and obesity, all of which are individually modifiable factors. Recent evidence suggests that environmental exposures, including air pollution (Hansen et al. 2016; Weinmayr et al. 2015) and transport-related (road traffic, railway, aircraft) noise (Eze et al. 2017a; Roswall et al. 2018; Sørensen et al. 2013) may also be risk factors, but epidemiological evidence, especially on noise, is limited. Air pollution and road traffic noise are often highly correlated, and few studies have sought to quantitatively disentangle the possible effects of traffic noise and traffic-related air pollution. Therefore, the question to what extent the reported associations of traffic noise are confounded by traffic-related air pollution is still largely unanswered and potentially relevant to implementing adequate abatement policies.
Three cohort studies examined the association of road traffic noise and diabetes incidence (Clark et al. 2017; Eze et al. 2017a; Sørensen et al. 2013), all suggesting positive association. Sørensen et al. reported an 8% increased risk of diabetes per increase in road traffic noise levels, which was enhanced (11%) after adjustment for nitrogen oxide () in 50,187 members of the Danish Diet, Cancer and Health Cohort (Sørensen et al. 2013), and researchers reproduced this finding in the recent re-analyses with prolonged follow-up (Roswall et al. 2018). However, they did not have data on particulate matter with a diameter (), an air pollutant which is also relevant for development of diabetes, as suggested by experimental (Sun et al. 2009) and epidemiological (Eze et al. 2015; Hansen et al. 2016) studies. In a Swiss Cohort Study on Air Pollution and Lung and Heart Diseases in Adults (SAPALDIA) of 2,631 participants, Eze et al. found a 20% increase in diabetes risk per increase in road traffic noise levels, which was enhanced to 35% and reached statistical significance only in a model with air pollutants, and nitrogen dioxide () (Eze et al. 2017a). In a population-based cohort from Vancouver, Canada, Clark et al. have detected an 8% increase in diabetes risk per increase in transportation (mainly road traffic) noise, in a model with air pollutants [, , and black carbon (BC)], greenness, and neighborhood walkability (Clark et al. 2017). However, Clark et al., in contrast with Eze et al. and Sørensen et al., did not adjust for major diabetes risk factors, including physical activity, smoking, diet, and body mass index (BMI), etc. Finally, studies examining other sources of environmental noise, including railway noise (Eze et al. 2015, 2017a; Roswall et al. 2018; Sørensen et al. 2013) and wind turbines noise (Poulsen et al. 2018), found no evidence of association with diabetes, whereas the results on aircraft noise are conflicting (Eriksson et al. 2014; Eze et al. 2017a).
Here, we examine whether long-term exposure to residential road traffic noise over 25 years is associated with diabetes incidence in the nationwide Danish Nurse Cohort study, while accounting for a number of air pollutants.
Methods
The Danish Nurse Cohort
The Danish Nurse Cohort (Hundrup et al. 2012) was established in 1993 and includes a total of 28,731 female members of the Danish Nurse Organization who were 44 years of age or older at recruitment in 1993 or 1999. Inspired by the American Nurses’ Health Study, the Danish Nurse Cohort aimed to provide the basis for research into the potential health effects related to use of hormone replacement therapy. In 1993, 19,898 nurses accepted an invitation and answered a comprehensive questionnaire on lifestyle (smoking, alcohol consumption, leisure time physical activity, diet, BMI, etc.), occupational characteristics (shift work, work environment, etc.), health, reproductive factors, and other factors. The cohort was reinvestigated in 1999, adding 8,833 nurses (8,344 new nurses who turned 44 in the period 1993–1999 and 489 nonresponders from the 1993 who were reinvited). In this study, we used the data from the earliest available questionnaire (1993 or 1999) for the 28,731 nurses for following characteristics: smoking status (never, previous, current), leisure time physical activity (low, medium, high), alcohol consumption (none/0 drinks per week, moderate/0–15 drinks per week, ), avoidance of fatty meat (no, yes), consumption of fruit and vegetables (daily/several times a day, a few times a week, rarely), marital status (married, separated, divorced, single, widow), night-shift work as a typical work schedule in nurses who were employed at the time of recruitment (yes, no), hypertension (yes, no), myocardial infarction (MI) (yes, no), use of sleep medication (yes, no), use of sedatives (yes, no), hormone replacement therapy (ever, never), menopausal status (yes, no), and level of urbanization, defined by population density at the municipality of residence at the cohort baseline in 1993 or 1999 (rural areas: ; provincial areas: ; and urban areas: ). Questions on sleep disturbances, perceived noise annoyance, and indicators of mental health or sources of chronic stress were not assessed in the questionnaire, so adjustments for the use of sleeping medication and sedatives were used as a proxy for women who may be particularly sensitive to noise.
Definition of Diabetes Incidence
To obtain information on type 2 diabetes incidence, the 28,731 nurses were linked to the National Diabetes Register (NDR) (Carstensen et al. 2011). The NDR was established in 2006 and has complete information on diabetes incidence in Denmark beginning 1 January 1995; therefore, the start of follow-up for nurses who were recruited in 1993 was moved to 1 January 1995. The NDR collects information on diabetes diagnosis from four different national registries: the National Patient Register (NPR), the National Health Service Register (NHSR), the Danish National Prescription Registry (DNPR), and the Danish Civil Registration System (DCRS). Date of diagnosis is defined as the date of inclusion into the NDR when any of the following six inclusion criteria are met: a) registration in NPR with diabetes diagnosis (ICD10: DE10–14, DH36.0, DO24 (excluding DO24.4), and ICD8: 249, 250); b) NHSR registration of provided chiropody services for patients with diabetes; c) five blood-glucose measurements in a 1-y period in NHSR; d) two blood-glucose measurements per year in 5 consecutive years in NHSR; e) DNPR registration of more than one purchase of oral antidiabetic drugs (OAD) within six months; and f) DNPR registration of more than one purchase of prescribed insulin within six months (Carstensen et al. 2011). The register is unable to distinguish between type 1 and type 2 diabetes; however, because cohort inclusion was restricted to nurses age 44 years or older, we find it reasonable to assume that the majority of incident diabetes cases are type 2 diabetes, as type 1 diabetes typically occurs before age 30. Results from a validation of the NDR suggests that the probability of false positive cases will be reduced by not considering participants who were included in the NDR solely based on blood-glucose measurements as diabetes cases (Green et al. 2014), the definition that we applied in this cohort. Furthermore, the definition of diabetes incidence that we used is exactly the same as the diabetes definition used in earlier Danish studies on diabetes and air pollution (Andersen et al. 2012; Hansen et al. 2016) and diabetes and road traffic noise (Roswall et al. 2018; Sørensen et al. 2013).
Exposure assessment.
All cohort participants were linked to the Danish Civil Registration System (Pedersen 2011) to extract information on the nurses’ residential addresses, historically since 1970, including exact date of address changes (moving date), and vital status until the end of follow-up on the 31 December 2012. We retrieved information on geographical coordinates of the nurses’ residential addresses throughout the study period from the Danish Address Database.
Assessment of residential road traffic noise.
The residential road traffic noise contribution at the nurses’ residential addresses was calculated using the Nord2000 method, an accurate and validated method for calculating noise contributions from road traffic and wind turbines (DELTA 2001). The Nord2000 method is considered the most accurate method for estimating sound pressure levels, as this method, unlike many others, considers meteorology’s influence on the sound propagation. The model used the following input variables: geocodes of the addresses, the height of apartments above street level, road lines with information on yearly average daily traffic, traffic composition and speed, road type and properties (e.g., motorway, rural highway, roads wider than , and other roads), building polygons for all surrounding buildings, and meteorology, including wind speed and direction, air temperature, and cloud cover. The propagation model is based on geometrical ray theory, computing the one-third octave band sound attenuation along the path from the source to the receiver. It accounts for properties of the terrain (shape, ground type, including impedance and roughness) and variations in weather conditions, which are appropriate when estimating yearly average noise levels. Various weather conditions have been predefined and respective noise levels computed. The Nord2000 method has been validated by more than 500 propagation cases, 9 of them involving road traffic noise (DELTA Acoustics & Electronics 2006), and validation of the method has furthermore been conducted for noise originating from higher sources, e.g., wind turbines (DELTA Acoustics 2009). However, validation is not possible for historical values, and it is reasonable to assume that estimation of noise further back in time is less precise than more recent estimations. The annual mean road traffic noise levels were calculated for the 28,731 nurses’ residential addresses from 1970 until 2013, estimating noise contributions from roads within a radius from the addresses. Because we had exact date of moving, we calculated annual mean of at the year of address change as the mean of levels at two addresses (the old address and the new one). The annual road traffic noise levels were estimated as the equivalent continuous A-weighted sound pressure level () at the most exposed façade of the dwelling for the day (; from 07:00 hours to 19:00 hours), evening (; from 19:00 hours to 22:00 hours) and night (; from 22:00 hours to 07:00 hours), and expressed as (the annual weighted levels of 24-h average during the day, evening, and night), adding a penalty to the estimated noise level in evening hours and penalty in the nighttime hours. Addresses located in remote areas secluded from traffic noise contributions were returned by the Nord2000 model as . However, because noise levels of never occur, in reality, due to noise contributions from sources other than traffic (e.g., vegetation), the noise levels with no road traffic noise contributions were set to , which was the case for < 2% of total addresses. The level of was selected based on a presumption that this level would roughly be equivalent to the average background noise contribution. Validation of the Nord2000 model showed, on average, small differences in A-weighted levels between the predictions and the measurements, with higher predicted noise levels than measurements, in the order of at the worst (DELTA Acoustics & Electronics 2006). The nine cases with calculation of the yearly average from a road, covering propagation distances up to show an average difference less than and a standard uncertainty less than .
Assessment of residential air pollution concentrations.
Outdoor air pollution exposure levels were estimated using the newly updated, high-resolution Danish air pollution dispersion modeling system, AirGIS (http://envs.au.dk/en/knowledge/air/models/airgis/), (Jensen et al. 2001). The necessary input data for carrying out the exposure modeling were established for the first time in Denmark for and particulate matter with diameter () beginning in 1990, whereas input data necessary for the gaseous and have been available since 1970. AirGIS uses three air pollution models in the integrated air pollution model system THOR (Brandt 2001). For the long-range transport components, the Danish Eulerian Hemispheric Model (DEHM) (Brandt et al. 2012; Frohn et al. 2002) is applied with a nested grid set-up covering the northern hemisphere, with increasing resolution over Denmark and other regions of Europe ( for the northern hemisphere, for Europe, for northern Europe, and for Denmark and nearby surroundings). The local background is calculated using the Urban Background Model (UBM) (Brandt et al. 2003; Brandt 2001) on a resolution grid covering Denmark. Finally, the residential address front door concentration is estimated by the Operational Street Pollution Model (OSPM) (Berkowicz 2000; Ketzel et al. 2013). For the generation of the OSMP input parameters, a semiautomatic system has been constructed using the Geographic Information System (GIS) and available Danish registers (Hertel et al. 2013). The AirGIS is considered a state-of-the-art modeling system in this field, and the OSPM applied for the street pollution component is applied in > 20 countries worldwide (Hvidtfeldt et al. 2018; Kakosimos et al. 2010). The OSPM model has recently been validated for , by comparing model estimates of monthly averages to measured values from fixed-site monitoring stations in Copenhagen (Hvidtfeldt et al. 2018). Hvidtfeldt et al. reported correlation coefficients of 0.82 between predicted and measured at the background monitor and 0.85 at the street measurement site and found that the model underestimated concentrations by 7–13% (Hvidtfeldt et al. 2018). In this study, we had available annual mean concentrations of and since 1990, and of and since 1970, all until 2013.
Statistical analysis.
Cox proportional hazards regression model with age as underlying time was used to examine the association between residential road traffic noise and the incidence of diabetes. The start of follow-up was age at the start of follow-up (1 January 1995 or 1 April 1999), and the end of follow-up was age at the time of diabetes diagnoses (event), death, emigration, or 31 December 2012 (censoring times), whichever came first. We modeled the association in crude models adjusted for age (underlying time scale) and calendar year, and in fully adjusted models, we further adjusted for established risk factors for diabetes, smoking status, leisure time physical activity, alcohol consumption, avoidance of fatty meat, consumption of fruit and vegetables, and marital status, all assessed at cohort baseline in 1993 or 1999. Additionally, we modeled the association between and diabetes incidence while taking residential air pollution exposure into account, by adding four different pollutants (, , , and ) one at a time in mutually adjusted models. The association was modeled using four different exposure time windows: 1-, 5-, 10-, and 25-y running means of at the year prior to diabetes diagnosis (calculated as geometric means), as the maximum available exposure window since the follow-up start in 1995 and first available data on road traffic noise in 1970, and compared with the same exposure windows for all other participants at the same age. was additionally categorized into low, medium, and high, defined as , percentile of exposure range, respectively, for each exposure window. Concentrations of the different air pollutants were added to the model using the time varying exposure windows equivalent to the exposure window of road traffic noise (described above) with exception of and , for which the longest possible exposure window was 5 y (between 1990, when modeling of PM began, and the start of follow-up in 1995). For this reason, analyses with 5-y mean of were considered main analyses.
We further assessed potential mediation of the association between and incident diabetes by BMI, MI, or hypertension, by examining changes in the effect estimates after adding these factors into the model. Road traffic noise has been linked to higher BMI and increased risk of MI and hypertension, and thus BMI, MI and hypertension may mediate the effect of road traffic noise on diabetes incidence. We also performed sensitivity analyses adjusting for neighborhood socioeconomic status (SES) in terms of mean income at the municipality level at the cohort baseline. Lastly, in exploratory analyses without a priori hypothesis, we examined whether (5-y mean, categorized as , percentile of exposure range) (25-y mean, categorized as , percentile of exposure range) obesity (), night-shift work, hypertension, MI, use of sleep medication, use of sedatives, level of urbanization, physical activity, and use of hormone replacement therapy modified the association between road traffic noise and incident diabetes. Effect modification was evaluated by introducing interaction terms to the fully adjusted model and assessed by likelihood ratio tests. Results are presented as hazard ratios (HR) with 95% confidence interval (CI), per interquartile range (IQR) increase for continuous exposures. In addition, p-value of was used to define statistical significance in main and effect modification analyses. Statistical analyses were conducted in Stata (version 14.2; StataCorp) and R (version 3.3.2; R Core Development Team). The graphical presentation of a functional form of an association between 5-y mean and diabetes incidence was produced using restricted cubic spline in the design library in R, and linearity assumption was tested using log-likelihood test.
Results
Of the 28,731 cohort participants, we excluded 192 who died or emigrated between 1 April 1993 and start of follow-up on 1 January 1995, 588 who were identified as patients with diabetes either by self-reported diabetes diagnosis or use of antidiabetic medications, and 31 who were identified in the NDR with a diabetes diagnosis prior to cohort baseline in 1995. We further excluded 1,319 participants with missing road traffic noise information at the year of the cohort baseline (1993 and 1999) and 3,056 participants with missing information on one or more potentially confounding, mediating, or modifying factors, which left 23,762 participants for the final study population. The 23,762 participants were followed from 1995 or 1999, until diabetes diagnosis, death, emigration, or end of follow-up on 31 December 2012, whichever came first, resulting in a total of 367,619 person-years of follow-up. During a mean follow-up time of 15.2 y, and median of 18 y, 1,158 nurses developed diabetes, resulting in an incidence rate of 315 per 100,000 person-years. Furthermore, 4,969 nurses who were excluded from analyses were more likely to have been recruited in 1993 (1995), were older, had higher BMI, were more likely to be current smokers, were less physically active and drank less alcohol, were more likely to be married, were more likely to have hypertension, were more likely to have MI, were more likely to use sleep medications or sedatives, were more likely to work night shifts, and were more likely to live in rural areas than the 23,762 nurses who were included in the analyses were (see Table S1), but two groups had comparable road traffic noise levels at residence (see Table S2).
Mean age at start of follow-up was 53.5 [], which was higher among those who developed diabetes (mean ± SD ) (Table 1). Nurses who developed diabetes were more likely to be overweight and obese, to be current smokers, never drinkers, divorced, single, or widowed, have hypertension and MI, use sleeping medication and sedatives, and live in urban areas; however, they were less likely to be physically active and avoid fatty meat than were the women who remained free of diabetes during the study period. Mean () residential road traffic noise level () was () at the baseline year in 1995 or 1999, ranging from to . and all air pollutant levels were slightly higher among nurses who developed diabetes than among the rest of the cohort (Table 2). At the baseline, 25.8% of the cohort participants lived in areas where the noise levels exceeded the Danish Environmental Protection Agency’s current limit from guidelines for road traffic noise of (Table 2). Nurses from The Danish Nurse Cohort resided throughout Denmark, with 15.3% residing in urban areas (), 43.6% in provincial towns (), and 41.1% in rural areas () at the cohort baseline, a distribution that corresponds closely to the distribution of Danish population. The estimated air pollution levels at baseline varied greatly. Levels of and , proxies of road traffic pollution, were high in urban areas, provincial areas, and small towns. Levels of and were also high in urban areas (traffic), as well as in southeastern Denmark due to long-range transported secondary pollution. Furthermore, levels of were high on the west coast, indicating strong influence of sea spray. Although is the proxy of traffic related air pollution, in Denmark is only partially originating from road traffic, whereas biomass burning for heating and long-range transported from central and eastern Europe present important sources.
Table 1.
Descriptive statistics for 23,762 female nurses from the Danish Nurse Cohort, at the cohort baseline in 1993 or 1999, two recruitment rounds, by diabetes status during follow-up until 2013.
| Total | No diabetes | Incident diabetes | p-Value | |
|---|---|---|---|---|
| Age at study start (1995/1999), | ||||
| Year of cohort enrollment, (%) | ||||
| 1995 | 15,484 (65.2) | 14,558 (64.4) | 926 (80.0) | |
| 1999 | 8,278 (34.8) | 8,046 (35.6) | 232 (20.0) | |
| Body mass index (BMI) (), | ||||
| BMI, (%) | ||||
| Underweight () | 571 (2.4) | 556 (2.5) | 15 (1.3) | |
| Normal weight () | 16,568 (69.7) | 16,093 (71.2) | 475 (41.0) | |
| Overweight () | 5,344 (22.5) | 4,902 (21.7) | 442 (38.2) | |
| Obese () | 1,279 (5.4) | 1,053 (4.7) | 226 (19.5) | |
| Smoking status, (%) | ||||
| Never | 8,231 (34.6) | 7,864 (34.8) | 367 (31.7) | |
| Previous | 7,327 (30.8) | 6,990 (30.9) | 337 (29.1) | |
| Current | 8,204 (34.5) | 7,750 (34.3) | 454 (39.2) | |
| Leisure time physical activity, (%) | ||||
| Low | 1,500 (6.3) | 1,380 (6.1) | 120 (10.4) | |
| Medium | 15,820 (66.6) | 15,017 (66.4) | 803 (69.3) | |
| High | 6,442 (27.1) | 6,207 (27.5) | 235 (20.3) | |
| Avoids fatty meat, (%) | 21,552 (90.7) | 20,540 (90.9) | 1,012 (87.4) | |
| Fruit intake, (%) | ||||
| Daily | 866 (3.6) | 825 (3.6) | 41 (3.5) | 0.94 |
| Weekly | 6,794 (28.6) | 6,467 (28.6) | 327 (28.2) | |
| Rarely | 16,102 (67.8) | 15,312 (67.7) | 790 (68.2) | |
| Vegetables intake, (%) | ||||
| Daily | 350 (1.5) | 327 (1.4) | 23 (2.0) | |
| Weekly | 5,822 (24.5) | 5,488 (24.3) | 334 (28.8) | |
| Rarely | 17,590 (74.0%) | 16,789 (74.3) | 801 (69.2) | |
| Alcohol consumption, (%) | ||||
| None (0 drinks/week) | 3,540 (14.9) | 3,294 (14.6) | 246 (21.2) | |
| Moderate (1–15 drinks/week) | 14,717 (61.9) | 14,058 (62.2) | 659 (56.9) | |
| Heavy () | 5,505 (23.2) | 5,252 (23.2) | 253 (21.8) | |
| Hypertension | ||||
| Yes, (%) | 2,916 (12.3) | 2,594 (11.5) | 322 (27.8) | |
| No, (%) | 20,846 (87.7) | 20,010 (88.5) | 836 (72.2) | |
| MI | ||||
| Yes, (%) | 154 (0.6) | 138 (0.6) | 16 (1.4) | 0.00 |
| No, (%) | 23,608 (99.4) | 22,466 (99.4) | 1,142 (98.6) | |
| Use of sleep medication | ||||
| Yes, (%) | 2,154 (9.3) | 2,027 (9.2) | 127 (11.3) | 0.02 |
| No, (%) | 21,002 (90.7) | 20,010 (90.8) | 992 (88.7) | |
| Missing, (%) | 606 (2.6) | 567 (2.5) | 39 (3.4) | |
| Use of sedatives | ||||
| Yes, (%) | 1,176 (5.1) | 1,095 (5.0) | 81 (7.2) | |
| No, (%) | 21,957 (94.9) | 20,920 (95.0) | 1,037 (92.8) | |
| Missing, (%) | 629 (2.6) | 589 (2.6) | 40 (3.5) | |
| Night shift work | ||||
| Yes, (%) | 1,010 (5.4) | 933 (5.2) | 77 (9.4) | |
| No, (%) | 17,712 (94.6) | 16974 (94.8) | 738 (90.6) | |
| Missing (not active in labor force), n (%) | 5,040 (21.2) | 4697 (20.8) | 343 (29.6) | |
| Marital status, (%) | ||||
| Married | 16,877 (71.0) | 16,117 (71.3) | 760 (65.6) | |
| Separated | 398 (1.7) | 380 (1.7) | 18 (1.6) | |
| Divorced | 2,685 (11.3) | 2,538 (11.2) | 147 (12.7) | |
| Single | 2,299 (9.7) | 2,165 (9.6) | 134 (11.6) | |
| Widow | 1,503 (6.3) | 1,404 (6.2) | 99 (8.5) | |
| Urbanization level, (%) | ||||
| Urban | 3,627 (15.3) | 3,418 (15.1) | 209 (18.0) | 0.02 |
| Provincial | 10,365 (43.6) | 9,864 (43.6) | 501 (43.3) | |
| Rural | 9,770 (41.1) | 9,322 (41.2) | 448 (38.7) | |
Note: p-Values obtained from ANOVA and Pearson’s chi-square test. MI, myocardial infarction.
Table 2.
Residential road traffic noise and air pollution levels (annual mean) at the beginning of the study in 1995 or 1999 (two recruitment rounds) for 23,786 female nurses from the Danish Nurse Cohort.
| Total | No diabetes | Incident diabetes | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Median (IQR) | 25th–75th | Median (IQR) | 25th–75th | Median (IQR) | 25th–75th | ||||
| 53.2 (9.4) | 48.8–58.2 | 53.2 (9.3) | 48.8–58.1 | 53.3 (9.9) | 49.2–59.1 | ||||
| in categories, (%) | |||||||||
| Low () | 5,117 (21.5) | — | — | 4,889 (21.6) | — | — | 228 (19.7) | — | — |
| Medium () | 12,563 (52.9) | — | — | 11,978 (53.0) | — | — | 585 (50.5) | — | — |
| High () | 6,082 (25.6) | — | — | 5,737 (25.4) | — | — | 345 (29.8) | — | — |
| 49.1 (9.5) | 44.6–54.1 | 49.1 (9.4) | 44.6–54.0 | 49.2 (10.1) | 45.0–55.1 | ||||
| 50.9 (9.5) | 46.4–55.9 | 50.9 (9.5) | 46.4–55.9 | 51.0 (10.1) | 46.9–57.0 | ||||
| 48.6 (9.5) | 44.1–53.6 | 48.6 (9.4) | 44.1–53.5 | 48.7 (10.0) | 44.5–54.5 | ||||
| 45.1 (9.4) | 40.6–50.0 | 45.1 (9.4) | 40.5–49.9 | 45.2 (9.9) | 41.0–50.9 | ||||
| * | 18.0 (3.9) | 16.1–20.0 | 18.0 (3.9) | 16.1–20.0 | 18.9 (3.5) | 16.9–20.4 | |||
| * | 21.4 (3.3) | 19.7–23.0 | 21.4 (3.3) | 19.7–23.0 | 22.0 (3.5) | 20.4–23.9 | |||
| * | 11.9 (11.0) | 8.3–19.3 | 11.9 (11.0) | 8.3–19.3 | 12.4 (11.3) | 8.7–19.9 | |||
| * | 10.3 (8.0) | 7.6–15.6 | 10.3 (8.0) | 7.5–15.5 | 10.6 (8.5) | 7.8–16.4 | |||
Note: is the current (2018) Danish guideline limit value for exposure to outdoor road traffic noise. *Available for only 22,242 nurses. —, not applicable.
The five modeled noise exposures (, , , , and ) were highly correlated with Spearman’s rank correlation coefficient () varying between 0.92 and 0.99 (Table 3). We found low correlation between and () and () and moderate with () and (). We observed lower correlation between and air pollutants in provincial and rural areas than we observed in urban areas (see Table S3). Correlation between different exposure windows was high (0.73 between 1-y and 25-y mean , see Table S4).
Table 3.
Correlation between road traffic noise and air pollutants (annual mean) at the cohort baseline in 1995 or 1999, two recruitment rounds.
| 1.0000 | |||||||||
| 0.99 | 1.0000 | ||||||||
| 0.98 | 0.98 | 1.0000 | |||||||
| 0.99 | 0.99 | 0.98 | 1.0000 | ||||||
| 0.96 | 0.94 | 0.92 | 0.94 | 1.0000 | |||||
| 0.46 | 0.44 | 0.44 | 0.44 | 0.44 | 1.0000 | ||||
| 0.34 | 0.32 | 0.33 | 0.32 | 0.31 | 0.793 | 1.0000 | |||
| 0.66 | 0.64 | 0.64 | 0.64 | 0.63 | 0.73 | 0.59 | 1.0000 | ||
| 0.56 | 0.54 | 0.534 | 0.54 | 0.53 | 0.65 | 0.64 | 0.92 | 1.0000 |
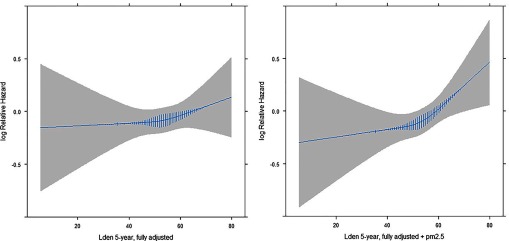
We found statistically significant positive associations between and diabetes incidence in crude models, strongest for the longest exposure window of 25 y (HR 1.10; 95% CI: 1.01, 1.19 per increase in ) and weaker for shorter exposure windows of 10 y (HR 1.08; 95% CI: 1.00, 1.16), 5 y (HR 1.07; 95% CI: 0.99, 1.15), and 1 y (HR 1.07; 95% CI: 1.00, 1.16) (Table 4). These associations attenuated in fully adjusted models to HRs of 1.06 (95% CI: 0.98, 1.16), 1.05 (95% CI: 0.97, 1.14), 1.04 (95% CI: 0.97, 1.12), and 1.05 (95% CI: 0.98, 1.13) for 25-, 10-, 5- and 1-y mean, respectively. The HRs attenuated further and reached unity in the model with , to HR of 1.01 in the model with and to 1.02 in the model with . In contrast, risk estimates attenuated only slightly or remained unchanged when models were adjusted for . Association between and diabetes incidence did not deviate from linearity (Figure 1). We detected statistically significant positive associations of and with diabetes incidence, which remained robust in the model with . Results were almost identical for , , and (see Table S6). HRs in the fully adjusted models remained largely unchanged after adjustment for the potential mediators BMI, hypertension, and MI, as well as after adjustment for mean income at the municipality level (see Table S7). We found similar results when noise exposure was modeled categorically, showing a dose–response relationship between diabetes incidence and increasing levels of ; however, the relationship attenuated after adjustment for , and , but not for (Table 4).
Table 4.
Association between road traffic noise (modeled as continuous variable, estimates presented per interquartile range increase and categorical) and incidence of diabetes in the Danish Nurse Cohort.
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
|---|---|---|---|---|---|---|
| Crudea | Fully adjustedb | Fully adjustedb | Fully adjustedb | Fully adjustedb | Fully adjustedb | |
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| 1-year mean | ||||||
| per | 1.07 (0.99, 1.15) | 1.05 (0.98, 1.13) | 1.00 (0.92, 1.08) | 1.02 (0.94, 1.10) | 1.02 (0.93, 1.13) | 1.04 (0.95, 1.14) |
| Low () | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Medium () | 1.03 (0.88, 1.20) | 1.02 (0.87, 1.20) | 1.00 (0.85, 1.17) | 1.02 (0.87, 1.20) | 1.02 (0.87, 1.20) | 1.03 (0.87, 1.21) |
| High () | 1.20 (1.01, 1.42) | 1.15 (0.97, 1.37) | 1.06 (0.88, 1.28) | 1.10 (0.92, 1.32) | 1.14 (0.92, 1.40) | 1.16 (0.96, 1.41) |
| 5-year mean | ||||||
| per | 1.07 (0.99, 1.15) | 1.04 (0.97, 1.12) | 0.99 (0.91, 1.08) | 1.01 (0.93, 1.10) | 1.01 (0.91, 1.11) | 1.03 (0.94,1.13) |
| Low () | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Medium () | 1.06 (0.90, 1.25) | 1.05 (0.89, 1.23) | 1.03 (0.87, 1.22) | 1.05 (0.89, 1.24) | 1.05 (0.89, 1.24) | 1.06 (0.89, 1.25) |
| High () | 1.22 (1.03, 1.45) | 1.17 (0.98, 1.40) | 1.08 (0.89, 1.31) | 1.12 (0.93, 1.35) | 1.14 (0.93, 1.41) | 1.17 (0.96, 1.43) |
| 10-year mean | ||||||
| per | 1.08 (1.00. 1,17) | 1.05 (0.97, 1.14) | — | — | 1.01 (0.91,1.12) | 1.04 (0.95,1.14) |
| Low () | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Medium () | 1.07 (0.91, 1.27) | 1.06 (0.90, 1.25) | — | — | 1.05 (0.89, 1.25) | 1.07 (0.90, 1.26) |
| High () | 1.24 (1.04, 1.48) | 1.18 (0.99, 1.41) | — | — | 1.13 (0.92, 1.40) | 1.18 (0.96, 1.44) |
| 25-year mean | ||||||
| per | 1.10 (1.01, 1.19) | 1.06 (0.98, 1.16) | — | — | 1.01 (0.91,1.13) | 1.05 (0.95,1.16) |
| Low () | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Medium () | 1.05 (0.89, 1.24) | 1.03 (0.87, 1.23) | — | — | 1.01 (0.85, 1.21) | 1.02 (0.86, 1.22) |
| High () | 1.23 (1.02, 1.47) | 1.16 (0.96, 1.40) | — | — | 1.09 (0.88, 1.36) | 1.15 (0.93, 1.41) |
Note: P and were available from 1990 onward and are thus only included in 5- and 1-y mean analyses. —, not applicable.
Crude model, adjusted for age and calendar time.
Fully adjusted model, adjusted for age, calendar time, leisure time physical activity, alcohol consumption, smoking status, marital status, diet (fruit, vegetables, and fatty meat).
Figure 1.
Association (log-relative hazard) between residential exposure to road traffic noise (5-y mean modeled with restricted cubic splines with 3 knots) and diabetes incidence among 22,233 members of the Danish Nurse Cohort in Denmark. Analyses were adjusted for age, calendar time, physical activity, alcohol consumption, smoking status, and marital status, and diet (fruit, vegetables and fatty meat). Vertical lines intersecting regression line represent density of the population.
Differences in the association between and diabetes incidence among strata of potential effect modifiers were small or difficult to interpret, given small numbers of incident cases within subgroups, with interaction for , , obesity, night-shift work, hypertension, MI, use of sleeping medication, physical activity, and hormone replacement therapy (Table 5). The association between and diabetes was inverse among those who used sedatives (HR 0.87; 95% CI: 0.65, 1.15) and positive among nonusers (HR 1.06; 95% CI: 0.98, 1.15 for nonusers), but there were only 81 incident cases among the sedative users (). The association between and diabetes was positive among urban women (1.27; 95% CI: 0.98, 1.63), but close to the null for provincial women (HR 1.02; 95% CI: 0.88, 1.18) and rural women (0.97; 95% CI: 0.87, 1.08) () (Table 5). Associations were similar after additional adjustment for (urban HR 1.26; 95% CI: 0.97, 1.62; provincial HR 0.99; 95% CI: 0.85, 1.15; and rural HR 0.93; 95% CI: 0.83, 1.05, ).
Table 5.
Effect modification of the association between residential road traffic noise (modeled as continuous variable, 5-year mean, per increase) and incidence of diabetes in the Danish Nurse Cohort. Analyses were adjusted for age, calendar time, physical activity, alcohol consumption, smoking status, marital status, and diet (fruit, vegetables, and fatty meat).
| cases | Person-years | HR (95% CI) | p-Valuea | |
|---|---|---|---|---|
| (5-year mean) | ||||
| Low () | 622 | 163,196 | 0.99 (0.89, 1.10) | |
| Medium () | 419 | 132,472 | 1.01 (0.88, 1.16) | |
| High () | 79 | 51,811 | 1.10 (0.76, 1.59) | 0.57 |
| (10-year mean) | ||||
| Low () | 274 | 83,871 | 1.05 (0.89, 1.24) | |
| Medium () | 572 | 180,149 | 0.97 (0.84, 1.13) | |
| High () | 276 | 84,080 | 1.18 (0.91, 1.52) | 0.29 |
| Obesity | ||||
| Not obese | 932 | 342,793 | 1.02 (0.94, 1.11) | |
| Obese | 226 | 17,930 | 1.12 (0.96, 1.32) | 0.38 |
| Night workb | ||||
| No | 738 | 272,649 | 1.00 (0.91, 1.10) | |
| Yes | 77 | 15,670 | 1.09 (0.82, 1.46) | 0.84 |
| Hypertension | ||||
| No | 836 | 318,673 | 1.05 (0.96, 1.15) | |
| Yes | 322 | 42,051 | 1.00 (0.87, 1.16) | 0.27 |
| MI | ||||
| No | 1,142 | 358,874 | 1.03 (0.96, 1.12) | |
| Yes | 16 | 1,849 | 1.49 (0.59, 3.77) | 0.46 |
| Use of sleep medicationc | ||||
| No | 992 | 321,182 | 1.04 (0.96, 1.13) | |
| Yes | 127 | 30,919 | 1.06 (0.83, 1.34) | 0.98 |
| Use of sedativesd | ||||
| No | 1,037 | 335,431 | 1.06 (0.98, 1.15) | |
| Yes | 81 | 16,346 | 0.87 (0.65, 1.15) | 0.15 |
| Urbanizatione | ||||
| Rural | 448 | 148,479 | 0.97 (0.87, 1.08) | |
| Provincial | 501 | 157,754 | 1.02 (0.88, 1.18) | |
| Urban | 209 | 54,489 | 1.27 (0.98, 1.63) | 0.14 |
| Physical activity | ||||
| Low | 120 | 20,355 | 1.28 (1.00, 1.64) | |
| Medium | 235 | 99,744 | 1.02 (0.87, 1.20) | |
| High | 803 | 240,623 | 1.02 (0.93, 1.12) | 0.60 |
| Hormone replacement therapy | ||||
| Never | 756 | 257,235 | 1.04 (0.94, 1.14) | |
| Previous | 162 | 34,671 | 1.06 (0.82, 1.31) | |
| Current | 226 | 63,810 | 1.04 (0.87, 1.24) | 0.97 |
Note: .
From likelihood ratio test for interaction.
Available for only a subset of the cohort, .
Available for only a subset of the cohort .
Available for only a subset of the cohort .
Estimates for urban, provincial, and rural areas after additional adjustment for : 1.26 (95% CI: 0.97, 1.62), 0.99 (95% CI: 0.85, 1.15), and 0.93 (95% CI: 0.83, 1.05), respectively.
Discussion
In the nationwide cohort of Danish nurses 44 years of age and older, we found no association between long-term exposure to road traffic noise and diabetes incidence after adjustment for . We also present a novel finding of a suggestive association between road traffic noise and diabetes in urban, but not in provincial and rural, areas in a nationwide Danish cohort of female nurses 44 years of age and older. Our findings agree with existing prospective cohort studies on diabetes incidence and road traffic noise, all suggesting positive associations (Clark et al. 2017; Eze et al. 2017a; Roswall et al. 2018; Sørensen et al. 2013), and all but one (Eze et al. 2017a) conducted in urban areas.
One of the differences between studies on road traffic noise and diabetes incidence is in treatment of possible confounding by air pollution and lifestyle factors (risk factors for diabetes), making estimates difficult to compare directly. Our study is most comparable to a study by Sørensen et al. in 57,053 Danish men and women from the Diet, Cancer and Health cohort, which found an 8% increased risk of diabetes per increase in 5-y mean exposure to , after adjusting for (Sørensen et al. 2013). Results by Sørensen et al. were recently reinvestigated and confirmed in an update of the original study with a longer follow-up period and an updated exposure of railway noise (Roswall et al. 2018). A major difference between our study and studies by Sørensen et al. and Roswall et al. is that they did not have data on exposure, which may be the more relevant pollutant for diabetes risk than nitrogen oxides (Clark et al. 2017; Hansen et al. 2016; Sun et al. 2009) and a confounder of an association between road traffic noise and diabetes risk. We previously found a strong association between and diabetes risk in this cohort (Hansen et al. 2016) and no association with , likely explaining the unchanged effect estimate of in the model with (Table 4). These findings are in line with a previous study in the Diet, Cancer and Health cohort where was also shown to be of less importance for diabetes development than was , but was not available and not yet studied with respect to diabetes in this cohort (Andersen et al. 2012). Similarly, Eze et al., in a Swiss SAPALDIA study of 2,631 participants, did not adjust for , reporting that they found no association between and incident diabetes, but they did adjust for despite lack of association between and diabetes incidence (Eze et al. 2017a). Eze et al. did not detect an association between and diabetes incidence in a single-exposure model (HR 1.20; 95% CI: 0.92, 1.56), but reported as their main result a strong and statistically significant association with in a multiexposure model (; 95% CI:1.02, 1.78), adjusted for , and even aircraft and railway traffic noise (although no association was found with railway traffic noise). Clark et al. has detected in 380,738 inhabitants from Vancouver, Canada, an association between and diabetes risk (HR: 1.08; 95% CI: 1.05, 1.10 per ) and found little evidence of confounding by , NO, , BC, greenness, or neighborhood walkability. The study by Clark et al., however, was based solely on administrative data, resulting in limited adjustment for potentially confounding variables, which included only age, gender and area-level household income, whereas information on known diabetes risk factors was unavailable (Clark et al. 2017). Roswall et al. and Sørensen et al. both showed considerable confounding of an association between road traffic noise and diabetes by lifestyle factors with HR for 5-y exposure to (per ) changing from 1.17 in crude to 1.10 in the fully adjusted model (for smoking, alcohol, fruit and vegetable consumption, physical activity, education, and calendar time). This finding is in line with our results (Table 4) and with Eze et al., where crude estimates for association between diabetes incidence and changed from 1.29 to 1.20 after adjustment for age, sex, education, smoking, alcohol, and diet. Thus, it is almost certain that associations reported by Clark et al. (1.05–1.07, per , depending on which pollutants were included in the model) are overestimated. Besides differences in treatment of cofounding in literature on noise and diabetes, there are other plausible differences, including natural variability of the association, as well as differences in study populations and in the nature of the confounding exposure, such as composition of , which differs between regions, and differences in modeling methods of noise and air pollution, etc.
Inconsistencies between our results and those of Sørensen et al. and Roswall et al. may be explained by differences in the study populations. The Diet, Cancer and Health cohort is based on men and women recruited from general populations living in the two largest and most polluted Danish cities (Copenhagen and Aarhus), whereas the Danish Nurse Cohort is an occupational cohort consisting of female nurses recruited from throughout Denmark, mainly from rural and provincial areas, with larger variations and lower mean levels in road traffic noise and air pollutant levels. When our results in sensitivity analyses were restricted to participants living in urban areas, in the same municipalities as the Diet, Cancer and Health cohort participants (), we found a positive association (HR:1.27; 05% CI: 0.98, 1.63) per increase in (5-y mean) (Table 5), which did not change after adjustment for (HR: 1.26; 95% CI: 0.97, 1.62) indicating that an association between road traffic noise and diabetes risk may be limited to urban areas (Table 5). A study by Clark et al. is also based on the urban population of Vancouver, Canada, whereas Eze et al. included populations from different regions of Switzerland but did not explored whether association between road traffic noise and diabetes incidence may differ by level of urbanization. We cannot exclude the possibility that our observation of a stronger association in urban areas may be due to exposure measurement error, as the exposure models’ performance may be different in urban and rural areas, and the Danish modeling system validation has been performed only in the urban area of Copenhagen (Hvidtfeldt et al. 2018). Other reasons may also include other differences between urban and rural areas, such as differences in access to health care or confounding by SES, among other factors.
Eze et al. examined potential effect modification by gender and found indication of a stronger association in males (HR: 1.66; 95% CI: 1.08, 2.55) than in females (HR: 1.17; 95% CI: 0.77, 1.77) and these findings may explain why we did not detect any association between and diabetes incidence in this study population of female nurses. On the contrary, Sørensen et al. found a stronger association between road traffic noise and diabetes risk in female cohort participants (Sørensen et al. 2013), whereas Clark et al. did not explore effect modification by gender.
Mechanisms linking road traffic noise exposure to the development of diabetes remain unclear. However, stress responses induced by exposure to noise, consequently leading to overproduction of glucocorticoids, inhibition of insulin secretion in the pancreas, and decreased insulin sensitivity in the liver, adipose tissue, and skeletal muscles are all suspected to play an important role in the development of diabetes (Recio et al. 2016). Besides initiation of stress responses, exposure to environmental noise has been associated with sleep disturbances (Muzet 2007), which may promote the development of type 2 diabetes (Medic et al. 2017). Recent results by Eze et al. furthermore suggest that exposure to nighttime road traffic noise () was associated with impaired glucose control (measured by changes in glycosylated hemoglobin (HbA1c)) in individuals with diabetes and that this association was significantly modified by genetic risk score of circadian-related variants (Eze et al. 2017b). Existing epidemiological studies are supported by results from a small experimental study showing that chronic exposure to noise induced persistent abnormalities in blood glucose regulation, a strong risk factor for type 2 diabetes, in 64 rats (Cui et al. 2016).
Strengths and Limitations
A strength of this study lies in the validated state-of-the-art exposure-assessment methods for modeling of individual-level noise and air pollution exposures (DELTA Acoustics & Electronics 2006; Kakosimos et al. 2010; Ketzel et al. 2011). Another strength is, furthermore, the use of Danish registry data to obtain information on individual residential address history since 1970, facilitating the longest exposure window to road traffic noise (25 y) to date. We also benefited from having access to NDR, with an objective, validated, and standardized definition of diabetes incidence (Carstensen et al. 2011; Green et al. 2014). A weakness of our study is the lack of data on noise sensitivity and annoyance, sleep quality, occupational noise exposure, and bedroom orientation, which may be important confounders or modifiers. Another weakness is the high correlation between different exposure windows (0.73 between 1-y and 25-y mean see Table S4) limiting our ability to distinguish whether long-term chronic or more recent exposures are most relevant for diabetes development. Information on covariates, e.g., dietary factors, were collected at one point in time (at cohort baseline in 1993 or 1999), and reflect the current behaviors at the cohort baseline, with no additional follow-up assessment on potentially confounding, mediating, or modifying factors.
We lacked data on individual income and education, but nurses represent a homogenous group with similar education and income. Furthermore, adjusting for mean income at the municipality level, as a proxy for neighborhood SES made no difference in noise estimates. Another limitation was limited power to explore a joint effect of air pollution and road traffic noise on diabetes incidence. We further lacked information on railway and aircraft noise exposure; however, these sources of transportation noise account for only a very small proportion of the total exposure from transportation noise in Denmark. Additionally, results by Roswall et al. found no association between railway noise and diabetes incidence in the Danish Diet, Cancer and Health cohort (Roswall et al. 2018), and similarly, no clear association was reported for aircraft noise in a cohort study from Sweden (Eriksson et al. 2014). Finally, our cohort of female nurses presents the population of health professionals, who are healthier than other Danish women. Indeed, nurses were found to have in general a healthier lifestyle than a representative sample of Danish women have, as the nurses smoked less and were more physically active, although they consumed more alcohol (Hundrup et al. 2012). We found that diabetes incidence of 315 new cases per 100,000 person-years in our cohort of female Danish nurses was somewhat lower than that observed in women from Danish Diet, Cancer and Health cohort, recruited from the general population (Roswall et al. 2018), of over 400 new cases per 100,000 person-years. This difference is likely explained by lower mean age at baseline (54 y) and BMI () in the nurses, than in the Diet, Cancer and Health cohort women, who were 56 years of age at baseline (1993–1997) and had a mean BMI of .
In the nationwide cohort of Danish nurses 44 years of age and older, we found no evidence of an association between long-term exposure to road traffic noise and incidence of diabetes in the total study population, where moderate positive associations detected in the crude models seemed to be explained by confounding factors, including lifestyle and air pollution, specifically . However, we found suggestive evidence that an association between noise and diabetes may be limited to residents of urban areas.
Supplementary Material
Acknowledgments
This work was funded by a grant from The Danish Council for Independent Research (DFF-4183-00353).
Footnotes
Supplemental Material is available online (https://doi.org/10.1289/EHP4389).
The authors declare they have no actual or potential competing financial interests.
Note to readers with disabilities: EHP strives to ensure that all journal content is accessible to all readers. However, some figures and Supplemental Material published in EHP articles may not conform to 508 standards due to the complexity of the information being presented. If you need assistance accessing journal content, please contact ehponline@niehs.nih.gov. Our staff will work with you to assess and meet your accessibility needs within 3 working days.
References
- Andersen ZJ, Raaschou-Nielsen O, Ketzel M, Jensen SS, Hvidberg M, Loft S, et al. 2012. Diabetes incidence and long-term exposure to air pollution: a cohort study. Diabetes Care 35(1):92–98, PMID: 22074722, 10.2337/dc11-1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkowicz R. 2000. OSPM - a parameterised street pollution model. Environ Monit Assess 65(1/2):323–331, 10.1023/A:1006448321977. [DOI] [Google Scholar]
- Brandt J. 2001. Operational air pollution forecasts from European to local scale. Atmos Environ 35:91–98, 10.1016/S1352-2310(00)00415-5. [DOI] [Google Scholar]
- Brandt J, Christensen JH, Frohn LM, Berkowicz R. 2003. Air pollution forecasting from regional to urban street scale––implementation and validation for two cities in Denmark. Phys Chem Earth, Parts A/B/C 28(8):335–344, 10.1016/S1474-7065(03)00054-8. [DOI] [Google Scholar]
- Brandt J, Silver JD, Frohn LM, Geels C, Gross A, Hansen AB, et al. 2012. An integrated model study for Europe and North America using the Danish Eulerian Hemispheric Model with focus on intercontinental transport of air pollution. Atmos Environ 53:156–176, 10.1016/j.atmosenv.2012.01.011. [DOI] [Google Scholar]
- Carstensen B, Kristensen JK, Marcussen MM, Borch-Johnsen K. 2011. The National Diabetes Register. Scand J Public Health 39(7 Suppl):58–61, PMID: 21775353, 10.1177/1403494811404278. [DOI] [PubMed] [Google Scholar]
- Clark C, Sbihi H, Tamburic L, Brauer M, Frank LD, Davies HW. 2017. Association of long-term exposure to transportation noise and traffic-related air pollution with the incidence of diabetes: a prospective cohort study. Environ Health Perspect 125(8):87025, PMID: 28934721, 10.1289/EHP1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui B, Gai Z, She X, Wang R, Xi Z. 2016. Effects of chronic noise on glucose metabolism and gut microbiota-host inflammatory homeostasis in rats. Sci Rep 6: 36693, PMID: 27811997, 10.1038/srep36693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DELTA Acoustics & Electronics. 2006. Nord2000. Validation of the Propagation Model. https://assets.madebydelta.com/assets/docs/share/Akustik/Nord2000_Validation_of_the_Propagation_Model_AV_1117_06.pdf [accessed 10 May 2019].
- DELTA Acoustics. 2009. Validation of the Nord2000 Propagation Model for Use on Wind Turbine Noise. https://assets.madebydelta.com/assets/docs/share/Akustik/Noise_and_energy_optimization_of_wind_farms.pdf [accessed 10 May 2019].
- DELTA. 2001. Nordic Environmental Noise Prediction Methods: Nord2000 Summary Report. https://assets.madebydelta.com/assets/docs/share/Akustik/Nordic_Environmental_Noise_Prediction_Methods_Nord2000_Summary_Report_-_Prediction_Methods.pdf [accessed 10 May 2019].
- Eriksson C, Hilding A, Pyko A, Bluhm G, Pershagen G, Östenson C-G. 2014. Long-term aircraft noise exposure and body mass index, waist circumference, and type 2 diabetes: a prospective study. Environ Health Perspect 122(7):687–694, PMID: 24800763, 10.1289/ehp.1307115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eze IC, Foraster M, Schaffner E, Vienneau D, Héritier H, Rudzik F, et al. 2017a. Long-term exposure to transportation noise and air pollution in relation to incident diabetes in the SAPALDIA study. Int J Epidemiol 46(4):1115.– , PMID: 28338949, 10.1093/ije/dyx020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eze IC, Hemkens LG, Bucher HC, Hoffmann B, Schindler C, Künzli N, et al. 2015. Association between ambient air pollution and diabetes mellitus in Europe and North America: systematic review and meta-analysis. Environ Health Perspect 123(5):381–389, PMID: 25625876, 10.1289/ehp.1307823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eze IC, Imboden M, Foraster M, Schaffner E, Kumar A, Vienneau D, et al. 2017b. Exposure to night-time traffic noise, melatonin-regulating gene variants and change in glycemia in adults. Int J Environ Res Public Health 14(12):1492, PMID: 29194408, 10.3390/ijerph14121492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frohn LM, Christensen JH, Brandt J. 2002. Development of a high-resolution nested air pollution model. J Comput Phys 179(1):68–94, 10.1006/jcph.2002.7036. [DOI] [Google Scholar]
- Green A, Sortsø C, Jensen PB, Emneus M. 2014. Validation of the Danish National Diabetes Register. Clin Epidemiol 7:5–15, PMID: 25565889, 10.2147/CLEP.S72768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen AB, Ravnskjær L, Loft S, Andersen KK, Bräuner EV, Baastrup R, et al. 2016. Long-term exposure to fine particulate matter and incidence of diabetes in the Danish Nurse Cohort. Environ Int 91:243–250, PMID: 26989812, 10.1016/j.envint.2016.02.036. [DOI] [PubMed] [Google Scholar]
- Hertel O, Jensen SS, Ketzel M, Becker T, Peel R, Ørby P, et al. 2013. Chapter 6: Utilizing monitoring data and spatial analysis tools for exposure assessment of atmospheric pollutants in Denmark. In: Occurrence, Fate and Impact of Atmospheric Pollutants on Environmental and Human Health, ACS Symposium Series Vol. 1149. American Chemical Society, 95–122, 10.1021/bk-2013-1149.ch006. [DOI] [Google Scholar]
- Hundrup YA, Simonsen MK, Jørgensen T, Obel EB. 2012. Cohort profile: the Danish nurse cohort. Int J Epidemiol 41(5):1241–1247, PMID: 21421694, 10.1093/ije/dyr042. [DOI] [PubMed] [Google Scholar]
- Hvidtfeldt UA, Ketzel M, Sørensen M, Hertel O, Khan J, Brandt J, et al. 2018. Evaluation of the Danish AirGIS air pollution modeling system against measured concentrations of PM2.5, PM10, and black carbon. Environ Epidemiol 2:e014, 10.1097/EE9.0000000000000014. [DOI] [Google Scholar]
- Jensen SS, Berkowicz R, Sten Hansen H, Hertel O. 2001. A Danish decision-support GIS tool for management of urban air quality and human exposures. Transp Res Part D Transp Environ 6(4):229–241, 10.1016/S1361-9209(00)00026-2. [DOI] [Google Scholar]
- Kakosimos KE, Hertel O, Ketzel M, Berkowicz R. 2010. Operational Street Pollution Model (OSPM) – a review of performed application and validation studies, and future prospects. Environ Chem 7(6):485, 10.1071/EN10070. [DOI] [Google Scholar]
- Ketzel M, Berkowicz R, Hvidberg M, Jensen SS, Nielsen OR. 2011. Evaluation of AirGIS: a GIS-based air pollution and human exposure modelling system. IJEP 47(1/2/3/4):226, 10.1504/IJEP.2011.047337. [DOI] [Google Scholar]
- Ketzel M, Jensen S, Brandt J, Ellermann T, Olesen H, Berkowicz R, et al. 2013. Evaluation of the street pollution model OSPM for measurements at 12 streets stations using a newly developed and freely available evaluation tool. J Civ Environ Eng S1:004, 10.4172/2165-784X.S1-004. [DOI] [Google Scholar]
- Medic G, Wille M, Hemels M. 2017. Short- and long-term health consequences of sleep disruption. Nat Sci Sleep 9:151–161, PMID: 28579842, 10.2147/NSS.S134864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzet A. 2007. Environmental noise, sleep and health. Sleep Med Rev 11(2):135–142, PMID: 17317241, 10.1016/j.smrv.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Pedersen CB. 2011. The Danish Civil Registration System. Scand J Public Health 39(7_suppl):22–25, PMID: 21775345, 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- Poulsen AH, Raaschou-Nielsen O, Peña A, Hahmann AN, Nordsborg RB, Ketzel M, et al. 2018. Long-term exposure to wind turbine noise at night and risk for diabetes: a nationwide cohort study. Environ Res 165:40–45, PMID: 29665463, 10.1016/j.envres.2018.03.040. [DOI] [PubMed] [Google Scholar]
- Recio A, Linares C, Banegas JR, Díaz J. 2016. Road traffic noise effects on cardiovascular, respiratory, and metabolic health: an integrative model of biological mechanisms. Environ Res 146:359–370, PMID: 26803214, 10.1016/j.envres.2015.12.036. [DOI] [PubMed] [Google Scholar]
- Roswall N, Raaschou-Nielsen O, Jensen SS, Tjønneland A, Sørensen M. 2018. Long-term exposure to residential railway and road traffic noise and risk for diabetes in a Danish cohort. Environ Res 160:292–297, PMID: 29045908, 10.1016/j.envres.2017.10.008. [DOI] [PubMed] [Google Scholar]
- Sørensen M, Andersen ZJ, Nordsborg RB, Becker T, Tjønneland A, Overvad K, et al. 2013. Long-term exposure to road traffic noise and incident diabetes: a cohort study. Environ Health Perspect 121(2):217–222, PMID: 23229017, 10.1289/ehp.1205503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Q, Yue P, Deiuliis JA, Lumeng CN, Kampfrath T, Mikolaj MB, et al. 2009. Ambient air pollution exaggerates adipose inflammation and insulin resistance in a mouse model of diet-induced obesity. Circulation 119(4):538–546, PMID: 19153269, 10.1161/CIRCULATIONAHA.108.799015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinmayr G, Hennig F, Fuks K, Nonnemacher M, Jakobs H, Möhlenkamp S, et al. 2015. Long-term exposure to fine particulate matter and incidence of type 2 diabetes mellitus in a cohort study: effects of total and traffic-specific air pollution. Environ Heal 14:53, , 10.1186/s12940-015-0031-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.