ABSTRACT
A 75-year-old man presented to our facility with a 5-day history of hematemesis. He reported a left inguinoscrotal hernia that had been present since 1990. Physical examination demonstrated an incarcerated inguinoscrotal hernia. Abdominal computed tomography revealed the stomach, small, and large bowel in the hernia. Esophagogastroduodenoscopy revealed food and brownish liquid in the stomach. Neither the antrum nor the pylorus could be identified during the esophagogastroduodenoscopy, consistent with an incarcerated portion of the stomach. Blood was not seen in the examined portion of the gastrointestinal tract. He was emergently treated with surgical intervention.
INTRODUCTION
Inguinal hernias are common but often only present in the setting of complications. Strangulation is uncommon but risks significant morbidity and mortality.1 Strangulation is due to trapping of hernia contents causing reduced venous/lymphatic flow and eventually reduced arterial flow, leading to ischemia and necrosis.1 Complicated inguinal hernias may present with pain and symptoms of intestinal obstruction. Patients should undergo early elective repair of hernias to prevent future complications. We report a case of a 75-year-old man presenting with a complicated inguinal hernia containing the stomach, small intestine, and large intestine. Inguinal hernias with contents including portions of the stomach have scarcely been described in the literature with most cases reported before 1980.2,3
CASE REPORT
A 75-year-old man was transferred to our facility with hematemesis of “coffee-ground” appearance. His medical history was significant for coronary artery disease, paroxysmal atrial fibrillation, chronic kidney disease, hyperlipidemia, hypertension, and left inguinoscrotal hernia. He reported that the inguinoscrotal hernia had been present since 1990. Physical examination revealed a large incarcerated inguinoscrotal hernia (Figure 1). A nasogastric tube was placed, which drained brownish material. Abdominal computed tomography revealed a large left inguinal hernia that contained portions of the stomach, small intestine, and large intestine (Figure 2).
Figure 1.

Gross examination of the scrotum with inguinoscrotal hernia.
Figure 2.
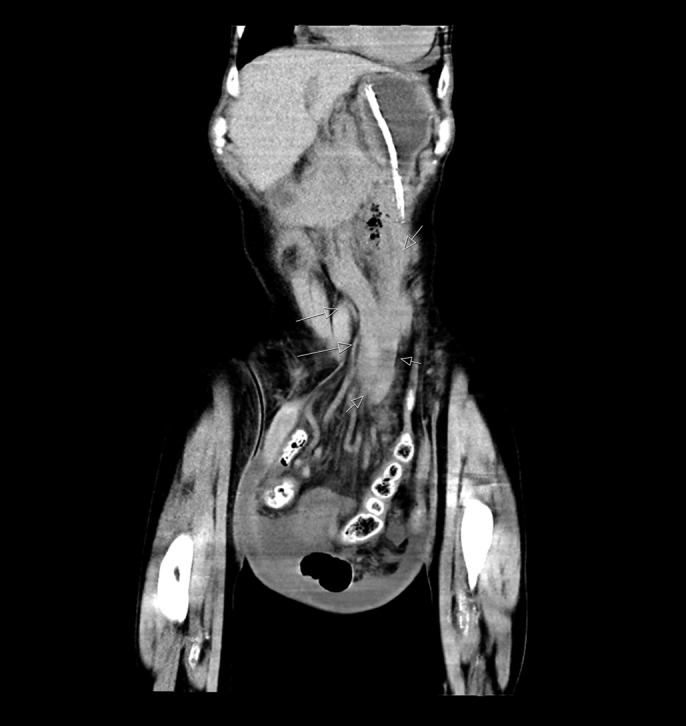
Coronal computed tomography demonstrating incarcerated inguinoscrotal hernia contents. White arrows denote the path of herniated contents.
Esophagogastroduodenoscopy revealed a large amount of semisolid food and brown, possibly feculent, liquid material in the body of the stomach. Neither the antrum nor the pylorus could be identified during the esophagogastroduodenoscopy. This was consistent with the incarcerated portion of the stomach within the left inguinal hernia based on the computed tomography findings. Blood was not seen in the examined upper gastrointestinal tract. It was determined that the inguinoscrotal hernia was causing gastric outlet obstruction by incarcerating the pylorus. He underwent emergent, laparoscopic surgical repair requiring resection of part of the small bowel. The remaining gastrointestinal contents were successfully returned to the abdomen. However, he developed aspiration pneumonia postoperatively and suffered anoxic brain injury.
DISCUSSION
Herniations of the abdominal wall are among the most common pathologies worldwide with a prevalence of 1.7% overall and 4% among those older than 45 years.4 Inguinal hernias account for most abdominal wall hernias, with a predilection toward men (lifetime risk among males of 27%).4 A complication of hernias, incarceration, refers to the trapping of hernia contents without the possibility of reduction and may lead to reduced venous and/or lymphatic flow.1 Left untreated, this may reduce arterial flow and cause strangulation (ischemia and necrosis of the hernia contents).1 The risk of strangulation has been estimated at 0.3%–3% per year.5
Inguinal hernias containing stomach contents have scarcely been described in the literature; approximately 60 cases have been reported, most of which occurred before 1980. Patients with this condition commonly present with pain, sequelae of intestinal obstruction, gastric outlet obstruction, and dyspeptic symptoms.2,3,6 It has been hypothesized that the emphasis on early, elective repair has reduced the number of patients presenting with this specific pathology.6 In this case, the inguinal hernia caused gastric outlet obstruction, a serious medical condition wherein a mechanical impediment preventing gastric emptying into the small bowel.
It has been postulated that long-standing traction on the greater omentum in the setting of a long-standing hernia may draw the stomach into the hernial sac.7 Chronic obstructive pulmonary disease has also been implicated in the pathogenesis of gastric pylorus containing inguinal hernias secondary to gastrointestinal ptosis.2 Little direct evidence supports this theory; however, chronic obstructive pulmonary disease has been an associated factor in at least 3 other cases of this pathology.2,6
Inguinal hernias may present with a wide range of symptoms; however, most cases are asymptomatic. Emphasis on early, elective treatment with open or laparoscopic surgery can reduce complications associated with inguinal hernias. Left untreated, inguinal hernias may grow in size and contents, increasing potential morbidity and mortality.
DISCLOSURES
Author contributions: T. Mehta wrote and edited the manuscript, searched the literature, and is the article guarantor. S. Weissman wrote and edited the manuscript and searched the literature. A. Vash and O. Serrano acquired and interpreted the imaging. D. Yim revised the manuscript.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
REFERENCES
- 1.Gallegos NC, Dawson J, Jarvis M, Hobsley M. Risk of strangulation in groin hernias. Br J Surg. 1991;78(10):1171–3. [DOI] [PubMed] [Google Scholar]
- 2.Diaz Oller J, Medina Dominguez MT, Arcos Navarro A, et al. Stomach in inguinal-scrotal hernia. Rev Esp Enferm Dig. 1997;89(4):325–8. [Spanish.] [PubMed] [Google Scholar]
- 3.Patel K, Francis L, Fazekas B, Panthagani J. Unusual contents of a large incarcerated inguinal hernia. BMJ Case Rep. 2014;2014:bcr2014207886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jenkins JT, O'Dwyer PJ. Inguinal hernias. BMJ. 2008;336(7638):269–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leubner KD, Chop WM, Jr, Ewigman B, Loven B, Park MK. Clinical inquiries. What is the risk of bowel strangulation in an adult with an untreated inguinal hernia? J Fam Pract. 2007;56(12):1039–41. [PubMed] [Google Scholar]
- 6.Creedon L, Peacock O, Singh R, Awan A. Gastric outlet obstruction secondary to incarcerated pylorus in an inguinal hernia. Ann R Coll Surg Engl. 2014;96(5):e26–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Padmanabhan AI, Lowenfels AB. Letter: An unusual hernia. JAMA. 1976;235(26):2813. [DOI] [PubMed] [Google Scholar]


