Abstract
Objectives
To increase understanding of knowledge, attitudes, and preventative practices regarding ischemic heart disease (IHD) in sub-Saharan Africa in order to develop patient-centered interventions to improve care and outcomes.
Study Design
Prospective observational study.
Methods
Adult patients presenting with chest pain or shortness of breath to an emergency department in northern Tanzania were enrolled. A questionnaire was adapted from existing knowledge attitude and practice surveys regarding cardiovascular disease and the WHO STEPS instrument. Individual five-year risk of cardiovascular event was determined by validated models based on age, sex, systolic blood pressure, body mass index, diabetes, and smoking status. An IHD knowledge score was calculated by giving one point for each correct response to the knowledge-related items, with a maximum score of 10. Associations between IHD knowledge and patient characteristics were assessed by Welch’s t-test.
Results
A total of 349 patients were enrolled, with median (IQR) age 60 (45, 72) years. Of participants, 259 (74.2%) had hypertension, and 228 (65.3%) had greater than 10% five-year risk of cardiovascular event. The mean (sd) knowledge score was 4.8 (3.3). The majority of respondents (224, 64.2%) recognized obesity as a risk factor for heart attack, while a minority (34, 9.7%) knew that a daily aspirin could reduce the risk of cardiovascular event. Greater IHD knowledge was associated with younger age (p = 0.045) and higher levels of education (p < 0.001) but not higher risk of cardiovascular disease (p = 0.123). Most respondents expressed a willingness to diet to improve their health (322, 92.3%) and a preference for treatment from a physician rather than a traditional healer for a heart attack (321, 92.0%). A minority of patients reported exercising regularly (88, 25.2%) or seeing a doctor routinely for check-ups (100, 28.7%).
Conclusions
High-risk emergency department patients in northern Tanzania have moderate knowledge regarding IHD but do not consistently engage in healthy preventive practices. Patient-centered interventions are needed to improve IHD knowledge and practices in high-risk populations.
Keywords: Ischemic heart disease, knowledge, attitudes, practices, sub-Saharan Africa
Introduction
Ischemic heart disease (IHD) is the leading cause of death worldwide.1 Little is known about the epidemiology of IHD in sub-Saharan Africa (SSA), although the incidence of the disease is presumed to be increasing given the rapid rise in cardiovascular risk factors and metabolic changes such as hypertension and obesity across SSA.2, 3 In Tanzania, for example, IHD is currently estimated to be the fourth leading cause of mortality.4 Like many countries in SSA, Tanzania faces the dual burden of communicable diseases like HIV and malaria as well as a growing burden of noncommunicable diseases like hypertension: although HIV remains the leading cause of mortality in Tanzania,4 the community prevalence of hypertension in many parts of the country now exceeds levels seen in Europe and North America.5–7
Against this backdrop, a firm understanding of patient knowledge, attitudes, and practices towards IHD in SSA is lacking. Although several studies describe community awareness of stroke and other forms of cardiovascular disease in SSA,8–16 to our knowledge only one study regarding patient knowledge of IHD has been conducted in SSA to date.17 This study, conducted among HIV-infected outpatients in Kenya, found that most participants were unaware of IHD symptoms or risk factors.17 Beyond these findings, much remains to be learned about patient perceptions and behavior regarding IHD in SSA, particularly among those at greatest risk. In Tanzania, for example, little is known about patient knowledge of IHD risk factors or uptake of preventative practices like salt reduction and exercise.
Characterizing patient knowledge, attitudes, and practices towards IHD is essential to developing educational and health system interventions to reduce IHD-related morbidity and mortality across SSA. Although some have questioned whether physician failure to diagnosis IHD may contribute to under-detection of IHD in SSA,18, 19 the role of the patient in IHD diagnosis and outcomes has heretofore been relatively ignored. If patients at high risk for IHD in SSA have poor knowledge, inappropriate attitudes, and unhealthy practices regarding IHD, then IHD burden and outcomes will likely be refractory to improvement, despite physician-centered interventions. Indeed, studies from settings outside SSA have demonstrated that improvements in patient knowledge and attitudes regarding cardiovascular disease result in healthier preventative practices and better outcomes.20–22 For instance, studies from the United Sates have found that improved cardiovascular health literacy was associated with improved control of hypertension and diabetes, lower rates of cardiovascular readmissions, and increased medication adherence.22 Thus, understanding patient beliefs, perceptions, and behaviors is essential to develop interventions reducing IHD morbidity and mortality across SSA.
In the context of an existing prospective study of adults presenting to an emergency department (ED) in northern Tanzania, we characterized the knowledge, attitudes, and practices (KAP) towards IHD among a high-risk patient population and described the association between personal IHD risk and IHD-related awareness and behaviors.
Methods
Study location
This study was conducted at Kilimanjaro Christian Medical Centre (KCMC), a tertiary care center in the Kilimanjaro Region of northern Tanzania. In 2014, the prevalence of hypertension among adults in Kilimanjaro was 28%, and the prevalence of diabetes was 6%.5, 23 Patients were recruited from the KCMC ED, which receives all patients presenting for urgent unscheduled care.
Survey development
No locally validated KAP survey for IHD exists in Tanzania or SSA at large. Therefore, the survey used in the present study was derived from multiple existing KAP surveys related to cardiovascular disease from SSA and elsewhere.17, 24–28 Candidate questions from existing surveys were selected and reviewed by an interdisciplinary team consisting of cardiologists, emergency medicine physicians, and lay people from Tanzania and the United States. From this pool of questions, items were chosen for inclusion in the KAP survey based on cultural relevance, pertinence to IHD, and unique content. The draft KAP survey was then translated from English to Swahili and independently back-translated to confirm fidelity to the intended content and to flag any potential ambiguity. The modified KAP survey was then piloted with 10 Tanzanians, some with and some without medical backgrounds, to ensure content clarity and fidelity. The final version of the KAP survey used in this study consisted of 22 items, including 10 questions regarding IHD knowledge, 7 questions regarding IHD attitudes, and 5 questions regarding IHD practices.
Study procedures
A prospective observational study was conducted in the KCMC ED. As part of a parent study on patterns of care for patients with chest pain or shortness of breath, all adult (age > 18 years) patients presenting to the ED were screened by trained research assistants. Adult patients presenting with chest pain or shortness of breath were eligible for inclusion in the parent study. Exclusion criteria were inability to provide informed consent, chest pain secondary to trauma, and self-reported fever. Screening was conducted during one shift (morning, evening, overnight) per day and the total number of days assigned to each shift was proportional to patient volumes during those shifts. All patients enrolled into the parent study were co-enrolled into the KAP study. Research assistants administered the KAP survey and a medical questionnaire derived from the World Health Organization STEPS instrument (WHO) to each enrolled patient.29 The medical questionnaire collected information regarding sociodemographic background, medical history, and lifestyle behaviors. Surveys were administered using Samsung Galaxy Tab E tablets (Samsung, Seoul, South Korea). In addition, one-time measurements of weight, height, and blood pressure were obtained for each participant at time of enrollment. Blood pressure was measured using the Beurer BM40 automatic blood pressure monitor (Beurer, Ulm, Germany). The study was conducted from 20 August 2018 to 4 January 2019.
Study definitions
Hypertension was defined as a self-reported history of hypertension or a measured blood pressure ≥ 140/90 mmHg, as per JNC 8 definitions.30 Although guidelines generally require elevated blood pressure measurements on two separate occasions for a new diagnosis of hypertension,30 follow-up visits were not conducted during this study and so the study definition for hypertension relied on the single blood pressure measurement obtained at enrollment. History of diabetes, hyperlipidemia, HIV infection, tobacco use, and alcohol use were defined by self-report. Body mass index (BMI) was used to categorize patients as obese (BMI ≥ 30 kg/m2), overweight (25 kg/m2 ≤ BMI < 30 kg/m2), normal weight (18.5 kg/m2 ≤ BMI < 25 kg/m2), and underweight (BMI < 18.5 kg/m2). Individual five-year cardiovascular risk was calculated using the Harvard NHANES (National Health and Nutrition Examination Survey) risk score based on age, sex, systolic blood pressure, diabetes, current smoking, and BMI.31, 32 This risk score has been internationally validated, including in SSA.32 Patients were categorized as low-risk if they had less than a 10% five-year risk of cardiovascular event; those with greater than 10% five-year risk of cardiovascular event were categorized as high-risk.
Statistical analyses
All statistical analyses were performed in RStudio (RStudio, Boston, MA). Categorical variables are presented as proportions and continuous variables are presented as means (standard deviations) or medians (interquartile ranges). An individual knowledge score was calculated for each participant. Participants were given one point for each correct answer to the knowledge-related questions (“yes” for all items except item 2 for which the correct answer was “no”), with a minimum possible score of 0 and a maximum possible score of 10. Responses of “do not know” did not receive any points. A higher knowledge score indicated better knowledge of IHD. Associations between IHD knowledge score and various sociodemographic and health characteristics were assessed using Welch’s t test. For purposes of data analysis, education was treated as a binary variable whereby those with any post-primary education (secondary school or post-secondary education) were compared to participants with no education or primary school education only. All analyses were performed at a 5% threshold for statistical significance. As this was an exploratory, descriptive study, no sample size calculations were performed in advance; sample size was dictated by the length of enrollment feasible within the study budget.
Ethical approval
This study received ethics approval from the Duke Health Institutional Review Board, the Kilimanjaro Christian Medical Centre Research Ethics Committee, and the Tanzania National Institutes for Medical Research Ethics Coordinating Committee. All participants provided written informed consent prior to enrollment.
Results
A total of 360 adult ED patients were eligible for study inclusion, of whom 349 (96.9%) consented to participate. Table 1 presents the sociodemographic characteristics and cardiovascular risk profiles of enrolled patients. The median (IQR) age of participants was 60 (45, 72) years, and 259 (74.2%) met the study definition for hypertension. A total of 162 (46.4%) participants were overweight or obese, and 228 (65.3%) had greater than 10% five-year risk of cardiovascular event.
Table 1.
Characteristics of emergency department patients with chest pain or shortness of breath participating in KAP survey, northern Tanzania, 2018 (N = 349)
| Patient characteristics | Number of patients (%) |
|---|---|
| Male sex | 148 (42.4) |
| Age, median (IQR), years | 60 (45, 72) |
| Education | |
| None | 27 (7.7) |
| Primary | 221 (63.3) |
| Secondary | 55 (15.8) |
| Post-secondary | 46 (13.2) |
| Medical comorbidities | |
| Hypertension | 259 (74.2) |
| Diabetes | 45 (12.9) |
| Hyperlipidemia | 40 (11.5) |
| HIV infected | 6 (1.7) |
| History of tobacco use | 114 (32.7) |
| History of alcohol use | 238 (68.2) |
| Body mass index | |
| Underweight | 28 (8.0) |
| Normal weight | 159 (45.6) |
| Overweight | 90 (25.8) |
| Obese | 72 (20.6) |
| 5-year cardiovascular risk | |
| Low risk (<10%) | 121 (34.7) |
| High risk (>10%) | 228 (65.3) |
Figure 1 presents participants’ responses to questions regarding knowledge of IHD. The majority of patients (224, 64.2%) knew that obesity increases the chance of having a heart attack. Similarly, a majority of participants recognized high blood pressure, a salt-heavy diet, a sedentary lifestyle, high cholesterol, and old age as risk factors for a heart attack. However, only a minority of enrolled patients knew that taking a daily aspirin could reduce the chances of a second heart attack or stroke, that diabetes increases the chances of a heart attack, or that a heart attack is not the same thing as a stroke. The mean (sd) knowledge score was 4.8 (3.3).
Figure 1.
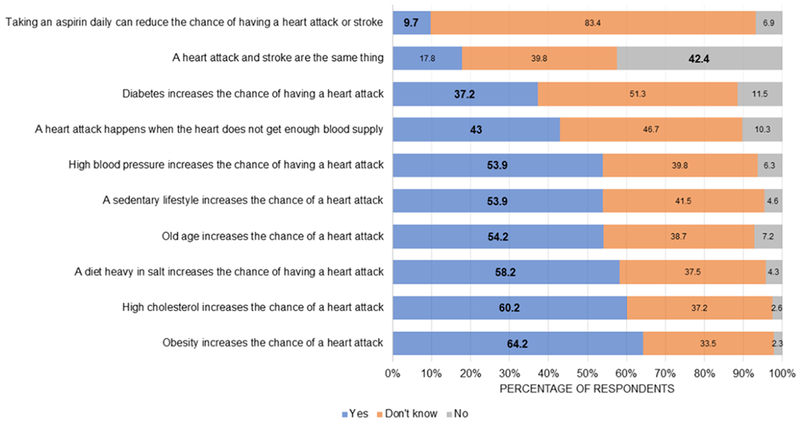
Responses to questions regarding knowledge of ischemic heart disease among emergency department patients with chest pain and shortness of breath, northern Tanzania, 2018 (N = 349)
*Correct answers in bold
Table 2 presents associations between participant characteristics and knowledge score. On bivariate analysis, higher knowledge score was associated with younger age and postprimary education. There was no association between IHD knowledge and cardiovascular risk.
Table 2.
Association between participant characteristics and knowledge of ischemic heart disease among emergency department patients with chest pain and shortness of breath, northern Tanzania, 2018 (N = 349)
| Participant characteristic | Knowledge score, mean (sd) | p |
|---|---|---|
| Sex | ||
| Female | 4.7 (3.3) | 0.755 |
| Male | 4.8 (3.2) | |
| Age | ||
| Age ≥ 55 years | 4.5 (3.3) | 0.045* |
| Age < 55 years | 5.2 (3.1) | |
| Education | ||
| Primary or none | 4.3 (3.3) | <0.001* |
| Post-primary | 6.0 (2.7) | |
| 5-year cardiovascular risk | ||
| Low risk (<10%) | 5.1 (3.1) | 0.123 |
| High risk (>10%) | 4.6 (3.3) |
With regard to participants’ attitudes toward IHD, the majority (322 patients, 92.3%) expressed a willingness to reduce the amount they ate to improve their health (Table 3). Similarly, the majority of participants viewed obesity as bad for one’s health, preferred treatment from a doctor over a traditional healer for a heart attack, and believed that hospital physicians can diagnose and treat heart attacks. Of participants, 117 (33.5%) felt that heart attacks were common in their community and 263 (75.4%) stated they would not be scared if a doctor told them they were having a heart attack.
Table 3.
Responses to questions regarding attitudes towards ischemic heart disease among emergency department patients with chest pain and shortness of breath, northern Tanzania, 2018 (N = 349)
| Question | Yes, n (%) | No, n (%) | Don’t Know, n (%) |
|---|---|---|---|
| 1. Heart attacks are common in my community | |||
| 117 (33.5) | 164 (47.0) | 68 (19.5) | |
| 2. Obesity is bad for one’s health | |||
| 297 (85.1) | 19 (5.4) | 33 (9.5) | |
| 3. If a doctor told me I was having a heart attack, I would be scared | |||
| 79 (22.6) | 263 (75.4) | 7 (2.0) | |
| 4. I would prefer to use medicines from a doctor more than traditional medicines from a traditional healer for a heart attack | |||
| 321 (92.0) | 8 (2.3) | 20 (5.7) | |
| 5. There are things I can do to reduce my chances of having a heart attack | |||
| 188 (53.9) | 19 (5.4) | 142 (40.7) | |
| 6. Doctors here can diagnose and treat heart attacks | |||
| 262 (75.1) | 8 (2.3) | 79 (22.6) | |
| 7. I am ready to reduce the amount that I eat to improve my health | |||
| 322 (92.3) | 16 (4.6) | 11 (3.2) | |
With regard to participants’ practices surrounding IHD, most reported that they take medicines daily as instructed by their doctor and that they limit their salt intake (Table 4). Only a minority of patients reported exercising more than twice weekly, seeing a doctor regularly for health checkups, or trying to lose weight. Figure 2 summarizes the knowledge, attitudes, and preventative practices regarding IHD among participants.
Table 4.
Responses to questions regarding practices towards ischemic heart disease among emergency department patients with chest pain and shortness of breath, northern Tanzania, 2018 (N = 349)
| Question | Yes, n (%) | No, n (%) | Don’t Know, n (%) |
|---|---|---|---|
| 1. Do you currently take medicines every day as instructed by your doctor? | |||
| 282 (80.8) | 67 (19.2) | 0 (0) | |
| 2. Do you exercise more than twice weekly? | |||
| 88 (25.2) | 244 (69.9) | 17 (4.9) | |
| 3. Do you go to the doctor regularly for health check-ups? | |||
| 100 (28.7) | 247 (70.8) | 2 (0.6) | |
| 4. Do you limit the amount of salt you use in your food so you don’t develop health problems? | |||
| 277 (79.4) | 62 (17.8) | 10 (2.9) | |
| 5. Do you try to lose weight? | |||
| 121 (34.7) | 191 (54.7) | 37 (10.6) | |
Figure 2.
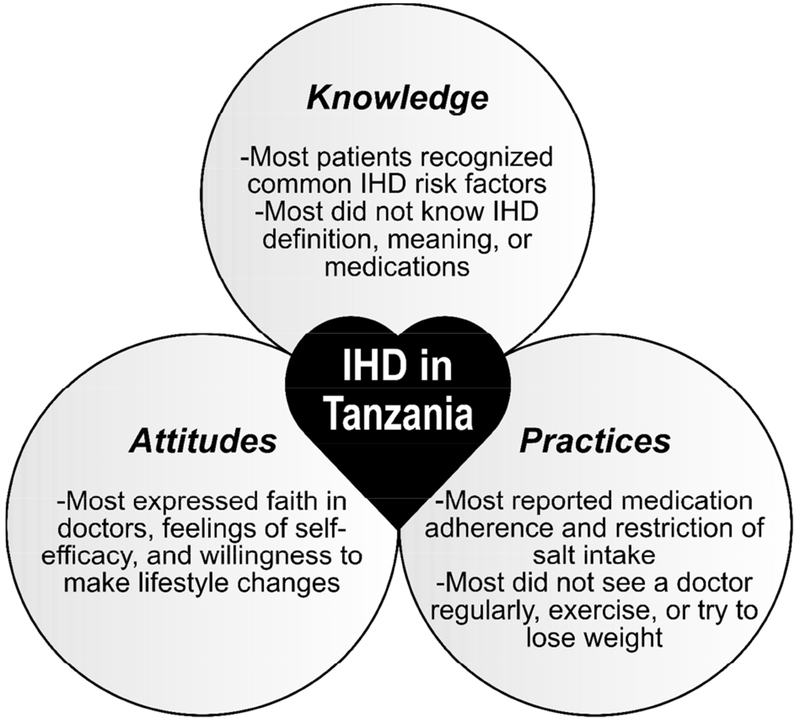
Summary of knowledge, attitudes, and preventative practices regarding ischemic heart disease (IHD) among emergency department patients in northern Tanzania
Discussion
This study is one of the first to investigate patient knowledge, attitudes, and practices regarding IHD in SSA. To our knowledge, this is the first published IHD KAP survey from Tanzania and the first from SSA among patients with acute chest pain or shortness of breath. Among a patient population at high-risk for IHD, knowledge of IHD was associated with younger age and higher education but not associated with personal cardiovascular risk. Although patients generally expressed trust in the healthcare system and a willingness to make lifestyle changes, less than a third received regular health check-ups or exercised more than twice weekly. This study found many high-risk patients with inadequate knowledge of IHD and unhealthy practices towards IHD, highlighting the need for patient-centered educational interventions in northern Tanzania, particularly among high risk populations.
A majority of participants recognized obesity, hypertension, age, high cholesterol, sedentary lifestyle, and a high-salt diet as risk factors for heart attack. Overall knowledge of IHD risk factors among our study population was better than knowledge of stroke risk factors among patients and community members elsewhere in SSA.12–16 For example, fewer than half of participants in studies published from SSA in the past 7 years recognized hypertension, obesity, age, high cholesterol, or sedentary lifestyle as risk factors for stroke.12–15 Similarly, a study of IHD knowledge among HIV infected patients in Kenya found that only small minorities of patients recognized sedentary lifestyle, obesity, hypertension, diabetes, hyperlipidemia, or age as IHD risk factors.17 These comparisons suggest that knowledge of cardiovascular disease among ED patients in northern Tanzania may be better than in other patient populations in SSA. However, this study identified several areas where patient knowledge was poor, including the difference between heart attacks and strokes, the physiologic meaning of a heart attack, the role of aspirin in secondary prevention of cardiovascular events, and the association between diabetes and IHD. Such topics should be emphasized in patient-based educational interventions in Tanzania. Although knowledge of heart attack symptoms was not assessed in this study, a recent community survey conducted in northern Tanzania found that knowledge of IHD symptoms among adults was very poor,33 suggesting that information regarding IHD symptoms should also be included in patient educational programming.
Unfortunately, higher personal cardiovascular risk was not associated with better IHD knowledge in this study. However, younger age and higher educational status were associated with better knowledge of IHD. This finding is consistent with results of other studies in SSA which found that higher level of education was associated with better stroke knowledge.11–13, 16 This suggests that educational efforts regarding IHD in northern Tanzania should target older high-risk populations.
With regard to attitudes towards IHD, patients in this study generally expressed willingness to make lifestyle changes to improve their cardiovascular health and reported high levels of trust in the formal healthcare system. However, given that this study included only patients who had chosen to present to the ED for their symptoms, such positive attitudes may not reflect community-wide perspectives. A recent study found that fewer than half of adults in northern Tanzania would present to the ED for chest pain,34 suggesting that the attitudes of patients in this study may not be representative of the general population.
Despite having generally positive attitudes towards lifestyle modifications and IHD prevention, participants’ self-reported IHD practices were not uniformly positive. This finding is unsurprising, as discordance between self-reported ideals and actual health practices has been widely reported across many settings.35, 36 In our study, only a minority endorsed regular exercise or regular visits to a doctor. This discrepancy suggests that adequate knowledge and positive attitudes may not be sufficient to produce desired preventive practices regarding IHD in Tanzania, as noted in many other venues.35, 36 Identifying barriers to healthy practices and developing patient-centered interventions that address such barriers will be essential to reducing the burden of IHD locally.
This study had several limitations. First, patient self-report was used to identify some cardiovascular risk factors like diabetes, HIV, and hyperlipidemia. Given that many adults in SSA with chronic diseases such as diabetes are unaware of their diagnosis,37, 38 this likely resulted in an underestimation of the level of cardiovascular risk among the study population. Furthermore, concerns about stigma may have resulted in under-reporting of HIV infection and other comorbidities, resulting in further underestimation of cardiovascular risk. Obtaining lipid panels, hemoglobin A1c levels, and HIV serostatuses would have led to a more accurate description of the IHD risk profile of our participants. Secondly, like other KAP surveys, this study was potentially subject to social desirability bias. If participants perceived certain attitudes or practices to be more acceptable in a hospital setting, this may have biased their responses. This may have resulted in an overestimation of, for example, the proportion of patients who take their medications regularly or who view hospital physicians as competent. Fourthly, as described above, the participants in this study may not be representative of the general community, as most Tanzanian adults reported in a recent community survey that they would not present to the ED for chest pain.34 Thus, the findings of this study may not be generalizable to Tanzania or SSA at large. Finally, as there are no existing KAP surveys regarding IHD validated in Swahili in SSA, this study utilized a survey adapted from KAP surveys validated in other settings and other languages. Therefore, the psychometric properties of the tool used in this investigation are unknown.
In conclusion, among ED patients with chest pain and shortness of breath in northern Tanzania, knowledge of IHD was moderate but several key areas of knowledge deficits were identified. Although attitudes towards IHD prevention and formal healthcare were generally positive, patients did not report consistently healthy practices regarding IHD prevention. Patient-centered interventions are needed to improve IHD knowledge and practices, particularly for high-risk populations.
Highlights.
Less than half of patients knew that a heart attack and stroke are not the same thing
Better IHD knowledge was not associated with personal cardiovascular risk
Less than a third of patients reported exercising or getting health check-ups regularly
Acknowledgments
Funding
This work was supported by the US National Institutes of Health [grant number D43TW009337].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing interests
None declared
References
- 1.Global Naghavi M., regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet (London, England). 2017; 390:1151–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tibazarwa K, Ntyintyane L, Sliwa K, Gerntholtz T, Carrington M, Wilkinson D, et al. A time bomb of cardiovascular risk factors in South Africa: results from the Heart of Soweto Study “Heart Awareness Days”. International journal of cardiology. 2009; 132:233–9. [DOI] [PubMed] [Google Scholar]
- 3.Campbell NR, Lemogoum D. Hypertension in sub-Saharan Africa: a massive and increasing health disaster awaiting solution. Cardiovascular journal of Africa. 2015; 26:152–4. [PMC free article] [PubMed] [Google Scholar]
- 4.IHME. Tanzania. Seattle, WA: University of Washington; 2016. [cited 2018 8 August]; Available from: http://www.healthdata.org/tanzania. [Google Scholar]
- 5.Galson SW, Staton CA, Karia F, Kilonzo K, Lunyera J, Patel UD, et al. Epidemiology of hypertension in Northern Tanzania: a community-based mixed-methods study. BMJ open. 2017; 7:e018829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muhamedhussein MS, Nagri ZI, Manji KP. Prevalence, Risk Factors, Awareness, and Treatment and Control of Hypertension in Mafia Island, Tanzania. International journal of hypertension. 2016; 2016:1281384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Katalambula LK, Meyer DN, Ngoma T, Buza J, Mpolya E, Mtumwa AH, et al. Dietary pattern and other lifestyle factors as potential contributors to hypertension prevalence in Arusha City, Tanzania: a population-based descriptive study. BMC public health. 2017; 17:659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boateng D, Wekesah F, Browne JL, Agyemang C, Agyei-Baffour P, Aikins AD, et al. Knowledge and awareness of and perception towards cardiovascular disease risk in sub-Saharan Africa: A systematic review. PloS one. 2017; 12:e0189264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Obembe AO, Olaogun MO, Bamikole AA, Komolafe MA, Odetunde MO. Awareness of risk factors and warning signs of stroke in a Nigeria university. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association. 2014; 23:749–58. [DOI] [PubMed] [Google Scholar]
- 10.Nansseu JR, Atangana CP, Petnga SN, Kamtchum-Tatuene J, Noubiap JJ. Assessment of the general public’s knowledge of stroke: A cross-sectional study in Yaounde, Cameroon. Journal of the neurological sciences. 2017; 378:123–9. [DOI] [PubMed] [Google Scholar]
- 11.Ajayi AO, Ojo OO. Knowledge and perception of stroke among at risk medical outpatients in a tertiary health institution in Nigeria. Annals of African medicine. 2007; 6:51–3. [DOI] [PubMed] [Google Scholar]
- 12.Wahab KW, Kayode OO, Musa OI. Knowledge of stroke risk factors among Nigerians at high risk. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association. 2015; 24:125–9. [DOI] [PubMed] [Google Scholar]
- 13.Cossi MJ, Preux PM, Chabriat H, Gobron C, Houinato D. Knowledge of stroke among an urban population in Cotonou (Benin). Neuroepidemiology. 2012; 38:172–8. [DOI] [PubMed] [Google Scholar]
- 14.Donkor ES, Owolabi MO, Bampoh P, Aspelund T, Gudnason V. Community awareness of stroke in Accra, Ghana. BMC public health. 2014; 14:196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaddumukasa M, Kayima J, Kaddumukasa MN, Ddumba E, Mugenyi L, Pundik S, et al. Knowledge, attitudes and perceptions of stroke: a cross-sectional survey in rural and urban Uganda. BMC research notes. 2015; 8:819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nakibuuka J, Sajatovic M, Katabira E, Ddumba E, Byakika-Tusiime J, Furlan AJ. Knowledge and Perception of Stroke: A Population-Based Survey in Uganda. ISRN stroke. 2014; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Temu TM, Kirui N, Wanjalla C, Ndungu AM, Kamano JH, Inui TS, et al. Cardiovascular health knowledge and preventive practices in people living with HIV in Kenya. BMC infectious diseases. 2015; 15:421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nkoke C, Luchuo EB. Coronary heart disease in sub-Saharan Africa: still rare, misdiagnosed or underdiagnosed? Cardiovascular diagnosis and therapy. 2016; 6:64–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hertz JT, Reardon JM, Rodrigues CG, de Andrade L, Limkakeng AT, Bloomfield GS, et al. Acute myocardial infarction in sub-Saharan Africa: the need for data. PloS one. 2014; 9:e96688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abbott LS, Slate EH. Improving Cardiovascular Disease Knowledge among Rural Participants: The Results of a Cluster Randomized Trial. Healthcare (Basel, Switzerland). 2018; 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee TW, Lee SH, Kim HH, Kang SJ. Effective intervention strategies to improve health outcomes for cardiovascular disease patients with low health literacy skills: a systematic review. Asian nursing research. 2012; 6:128–36. [DOI] [PubMed] [Google Scholar]
- 22.Magnani JW, Mujahid MS, Aronow HD, Cene CW, Dickson VV, Havranek E, et al. Health Literacy and Cardiovascular Disease: Fundamental Relevance to Primary and Secondary Prevention: A Scientific Statement From the American Heart Association. Circulation. 2018; 138:e48–e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stanifer JW, Cleland CR, Makuka GJ, Egger JR, Maro V, Maro H, et al. Prevalence, Risk Factors, and Complications of Diabetes in the Kilimanjaro Region: A Population-Based Study from Tanzania. PloS one. 2016; 11:e0164428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vaidya A, Aryal UR, Krettek A. Cardiovascular health knowledge, attitude and practice/behaviour in an urbanising community of Nepal: a population-based cross-sectional study from Jhaukhel-Duwakot Health Demographic Surveillance Site. BMJ open. 2013; 3:e002976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mosca L, Jones WK, King KB, Ouyang P, Redberg RF, Hill MN. Awareness, perception, and knowledge of heart disease risk and prevention among women in the United States. American Heart Association Women’s Heart Disease and Stroke Campaign Task Force. Archives of family medicine. 2000; 9:506–15. [DOI] [PubMed] [Google Scholar]
- 26.Gill R, Chow CM. Knowledge of heart disease and stroke among cardiology inpatients and outpatients in a Canadian inner-city urban hospital. The Canadian journal of cardiology. 2010; 26:537–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aminde LN, Takah N, Ngwasiri C, Noubiap JJ, Tindong M, Dzudie A, et al. Population awareness of cardiovascular disease and its risk factors in Buea, Cameroon. BMC public health. 2017; 17:545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Muhamad R, Yahya R, Yusoff H, Rao B, Rao D. Knowledge, Attitude and Practice on Cardiovascular Disease among Women in North-Eastcoast Malaysia. International Journal of Collaborative Research on Internal Medicine & Public Health. 2012; 4:85–98. [Google Scholar]
- 29.WHO. WHO STEPS Instrument: The WHO STEPwise approach to noncommunicable disease risk factor surveillance (STEPS). Geneva: World Health Organization; 2003. [Google Scholar]
- 30.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). Jama. 2014; 311:507–20. [DOI] [PubMed] [Google Scholar]
- 31.Gaziano TA, Young CR, Fitzmaurice G, Atwood S, Gaziano JM. Laboratory-based versus non-laboratory-based method for assessment of cardiovascular disease risk: the NHANES I Follow-up Study cohort. Lancet (London, England). 2008; 371:923–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gaziano TA, Abrahams-Gessel S, Alam S, Alam D, Ali M, Bloomfield G, et al. Comparison of Nonblood-Based and Blood-Based Total CV Risk Scores in Global Populations. Global heart. 2016; 11:37–46.e2. [DOI] [PubMed] [Google Scholar]
- 33.Hertz JT, Madut DB, Tesha RA, William G, Simmons RA, Galson SW, et al. Knowledge of myocardial infarction symptoms and perceptions of self-risk in Tanzania. American heart journal. 2019; 210:69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hertz JT, Madut DB, Tesha RA, William G, Simmons RA, Galson SW, et al. Perceptions of chest pain and healthcare seeking behavior for chest pain in northern Tanzania: A community-based survey. PloS one. 2019; 14:e0212139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Larsen JK, Hermans RCJ, Sleddens EFC, Vink JM, Kremers SPJ, Ruiter ELM, et al. How to bridge the intention-behavior gap in food parenting: Automatic constructs and underlying techniques. Appetite. 2018; 123:191–200. [DOI] [PubMed] [Google Scholar]
- 36.Rhodes RE, Yao CA. Models accounting for intention-behavior discordance in the physical activity domain: a user’s guide, content overview, and review of current evidence. The international journal of behavioral nutrition and physical activity. 2015; 12:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Manne-Goehler J, Atun R, Stokes A, Goehler A, Houinato D, Houehanou C, et al. Diabetes diagnosis and care in sub-Saharan Africa: pooled analysis of individual data from 12 countries. The lancet Diabetes & endocrinology. 2016; 4:903–12. [DOI] [PubMed] [Google Scholar]
- 38.Hall V, Thomsen RW, Henriksen O, Lohse N. Diabetes in Sub Saharan Africa 1999-2011: epidemiology and public health implications. A systematic review. BMC public health. 2011; 11:564. [DOI] [PMC free article] [PubMed] [Google Scholar]


