Abstract
Background:
Black women disproportionately suffer from violence and its subsequent mental health outcomes. Increasing levels of perceived stress are associated with greater symptoms of depression and PTSD. Social support and resilience can potentially mediate the negative consequences of perceived stress on women’s mental health. This study assesses the association between perceived stress and mental health outcomes among Black women. In addition, this study examines social support and resilience as mediators of association between perceived stress and mental health.
Methods:
Black women residing in Baltimore, MD (n=310) were recruited from STD clinics into a retrospective cohort study (2013-2018) on sexual assault and HIV risk. Social support and resilience served as coping variables and were assessed as mediators in the associations between perceived stress and mental health. Analyses were stratified by exposure to sexual violence in adulthood.
Results:
Almost half of our sample (46%) experienced severe depression and about one-third (27%) experienced severe PTSD. Resilience partially mediated the association between perceived stress and severe depressive symptoms among exposed women. Social support partially mediated the association between perceived stress and severe PTSD symptoms among exposed women.
Limitations:
Since this is a cross-sectional analysis, we are unable to determine the temporal relationship between outcome and exposure variables. The CES-D-10 and NSESSS are scales that measure the severity of depressive and PTSD symptoms, respectively, and are not clinical diagnoses
Conclusion:
There is a critical need to develop interventions focused on reducing the burden of stress on mental health.
Keywords: depression, PTSD, perceived stress, social support, resilience, violence
INTRODUCTION
Mental health disparities in the United States (US) are persistent among women, especially women of color. In the US, women are nearly twice as likely to experience depression and two to three times as likely to develop post-traumatic stress disorder (PTSD) as men (Brody et al., 2018; Olff, 2017). Black women experience comparable prevalence of depression and PTSD as the general population, but are less likely to utilize mental health services than their white counterparts (Sabri et al., 2013). If left untreated, mental health problems can worsen and lead to additional adverse health outcomes and consequences, including substance use and suicide (Chesney et al., 2014; Prasad, 2016).
These mental health disparities among racial minorities can be understood in the context of stress and coping. The Theory of Stress and Coping (Lazarus and Folkman, 1984) posits that stress is a dynamic process where an individual’s perception of a stressful experience defines their response to the stressor. The ability to cope with stress depends on whether an individual believes they possess sufficient resources to mitigate or eliminate the stressor. In the context of Black women, the theory of stress and coping can additionally be viewed through the lens of the Minority Stress Model. The minority stress model posits that racial and ethnic minorities experience heightened stress and unique minority stressors arising from a hostile environment (Meyer, 2003). These additional chronic stressors demand more coping among racial minorities, likely causing additional stress, and potentially more adverse effects on mental health (Meyer, 2003).
Stress is consistently related to mental health problems, with increasing levels of perceived stress associated with greater symptoms of depression and PTSD (Qu et al., 2012). Research finds that socially disadvantaged individuals experience more stressful life events (Almeida et al., 2005) and tend to perceive these events as more stressful, perhaps due to limited coping resources (Adler et al., 1994). In addition, issues related to gender and ethnicity influence the stress experiences of Black women (Woods-Giscombé and Lobel, 2008). Specifically, Black women are disproportionately affected by gender-based violence (Cunradi et al., 2002) and the negative consequences of violence on mental conditions (Lacey et al., 2015). Therefore, it is imperative to understand the underlying mechanism between perceived stress and mental health among Black women exposed to violence. In particular, it is critical to identify the factors that may enhance coping strategies such as social support and resilience.
Social support is the process of social interaction in relationships, which enhances belonging, coping, and esteem through the exchange of physical or psychosocial resources (Gottlieb, 2000). Social support helps people cope with traumatic experiences and is highly correlated with good mental health. People who report low levels of social support are found to have higher levels of stress, increased mental health morbidity in depression, PTSD, and increased mortality than people with high levels social support (Southwick et al., 2005). Black women who have social networks with high social support report better mental health and greater well-being. (Hood et al., 2017; Talwar, 2017; Thorsteinsson et al., 2013). Furthermore, social support has been found to mediate the association between stress and depression among samples of adolescents and undergraduate students (Talwar, 2017; Thorsteinsson et al., 2013).
Resilience is defined as the process of successfully adapting to adversity, trauma, or significant stressors (Southwick et al., 2014). Resilience may strengthen resistance to stress by allowing greater access to positive emotional resources. Increased resilience can enhance coping strategies and is highly correlated to mental health (Gheshlagh et al., 2017; Mary and Dolbier, 2008). Strengthening resilience among Black women at risk for depression and PTSD may serve as a protective factor against mental health problem symptom severity (Holden et al., 2017). Social support may also help to enhance resilience, particularly among abused Black women (Howell et al., 2017). Hence, social support and resilience can potentially improve coping strategies to avoid the negative effects of stress on mental health among Black women.
Despite this, few studies have explored the roles of social support and resilience in the association between stress and mental health problems among Black women who are survivors of abuse. The primary objective of this study is to examine the association between perceived stress and mental health problems (depressive and PTSD symptoms) among Black women. The secondary objective of this study is to examine the roles of social support and resilience as mediators of the association between perceived stress and mental health problems. We hypothesize that women with greater perceived stress will have an increased likelihood of mental health problems. We further hypothesize that social support and resilience will attenuate (mediate) the association between mental health problems among Black women.
METHODS
The data analyzed is from The ESSENCE Project: Examining Stress, Sexual Experiences, and Neighborhood Correlates of HIV Risk among Black Women (NICHD R01HD077891). The ESSENCE Project is a retrospective cohort study (2015-2018) examining the association between the neighborhood and social environment, sexual assault, and HIV risk factors among Black women in Baltimore, MD. Black women seeking health services were recruited in the waiting rooms of two Baltimore City public STD clinics. After providing informed consent, participants were screened for eligibility using the following inclusion criteria: biologically female, between ages 18-44, self-identified as Black, reported having sex with a man in the past 6-months, and reported having either two or more sexual partners in the past year or a high HIV risk sexual partner (i.e., used injection/non-injection drugs, had sex with men, been to prison, had concurrent sex partner, had an STD, was HIV-positive, or did not know if their sexual partners had any of these characteristics). Due to the study design, at least one-third of women in our sample reported exposure to sexual violence since the age of 18 (referred to as “exposed” from herein out). Exposure to sexual violence was determined by asking women, “Since you turned 18, has a male sex partner used force (like hitting, holding down, or using a weapon) to make you have sex?” Eligible women proceeded to full survey completion (60-90 minutes), which was administered via audio computer-assisted self-interview (ACASI). Each participant received $45 of remuneration and a list of local community resources. The ethical review boards of Johns Hopkins University and the University of California, San Diego approved the study design and procedures. An NIH Certificate of Confidentiality was issued to protect the privacy of research participants involved in our study.
Measures
The outcome variables were depressive symptoms and PTSD symptoms. The primary independent variable was perceived stress. Mediators were social support and resilience. Cronbach’s alpha was calculated to determine the reliability for each of the scales used.
Depressive symptoms were measured using the Center for Epidemiologic Studies Short Depression (CES-D-10) scale, a 10-item, self-reported measure of an individual’s past-week depressive feelings and behaviors (Andresen et al., 1994). Items included being bothered by things not usually bothersome, having trouble concentrating, feeling depressed, and feeling lonely. The CES-D-10 has a 4-point response format ranging from “rarely or none of the time (less than 1 day)” to “all of the time (5-7 days)”. This measure was calculated by summing the respondent’s scores across all 10 items, with scores ranging from 0 to 30. A cut-off score ≥10 denoted having severe depressive symptoms vs. not having severe depressive symptoms (<10). This cut-off has been established as optimal to identify individuals at risk of depression (Andresen et al.,1994). The scale demonstrated good reliability among exposed (α=0.82) and unexposed women ((α=0.77).
Post-traumatic Stress Disorder (PTSD) symptoms were measured using the National Stressful Events Survey PTSD Short Scale (NSESSS), a 9-item, self-reported measure that determines the severity of an individual’s PTSD during the past month (LeBeau et al., 2014). Responses for each item were measured on a 5-point scale ranging from 0 “never” to 4 “extremely”. The PTSD symptoms score was calculated by taking the average across all 9 items, with higher scores indicating greater severity of PTSD. According to the American Psychiatric Association (APA), the average total score reduces the overall score to a scale: mild (1), moderate (2), severe (3), or extreme (4) (Kilpatrick et al., 2013). The binary outcome of PTSD, a cut-off score of ≥3 denoted severe/extreme PTSD symptoms vs. not having severe/extreme PTSD symptoms (<3). The scale demonstrated excellent reliability among exposed (α=0.91) and unexposed women ((α=0.93).
Perceived stress was measured using the Perceived Stress Scale (PSS), a 14-item scale, self-reported measure of the degree to which situations are considered stressful, unpredictable or uncontrollable in the past month (Cohen et al., 1983). Items included how often they felt unable to control important things in their life, how often they felt nervous and “stressed,” and how often they have been able to control irritations in their life. Responses followed a 5-point Likert scale ranging from “strongly disagree” to “strongly agree.” This measure was calculated by summing the respondent’s score across all 14 items, with scores ranging from 0 to 40. For solely descriptive purposes, scale scores were categorized by tertiles (≤18, 19-22, ≥23). The scale demonstrated good reliability among exposed (α=0.80) and unexposed women (α=0.82).
Social support was measured using the Multidimensional Scale of Perceived Social Support (MSPSS), a 12-item scale, self-reported measure of an individual’s perception of social support quality (Zimet et al., 1988). Items assessed included having a special person who is around when in need, having a family that really tries to help, and being able to count on my friends when things go wrong. Responses followed a 5-point Likert scale ranging from “strongly disagree” to “strongly agree.” This measure was calculated by summing the respondent’s score across all 12 items, with scores ranging from 12 to 60. For solely descriptive purposes, scale scores were categorized by tertiles (≤42, 43-50, ≥51). The scale demonstrated excellent reliability among exposed (α=0.91) and unexposed (α=0.93) women.
Resilience was measured using the Connor-Davidson Resilience Scale (CD-RISC 10), a 10-item scale, self-reported measure of the ability to cope with adversity in the past month (Campbell-Sills and Stein, 2007). Items included the ability to adapt to change, dealing with whatever comes, seeing the humorous side of things, and achieving goals. Responses followed a 5-point Likert scale ranging from 0 “not true at all” to 4 “true nearly all the time”. This measure was calculated by summing the respondent’s score across all 10 items, with scores ranging from 0 to 40. For solely descriptive purposes, scale scores were categorized by tertiles (≤19, 20-27, ≥28). The scale demonstrated excellent reliability among exposed (α=0.93) and unexposed women (α=0.94).
Analyses
All statistical analyses were conducted using Stata, version 15.2. Of the 310 women recruited in the ESSENCE Project, we excluded 78 women with missing data on depressive symptoms, PTSD symptoms, perceived stress, social support, and resilience, bringing the analytic sample to 232. Analyses began with univariate descriptive statistics of sociodemographic characteristics, mental health problems, perceived stress, social support, and resilience. Pearson correlation coefficients were conducted to examine the associations between these variables. Logistic regression models estimated the bivariate associations between perceived stress, social support, and resilience on the mental health problem outcomes of severe depressive symptoms and severe PTSD symptoms, respectively. Finally, generalized structural equation modeling tested whether social support and resilience mediated the association between perceived stress and mental health using. Akaike’s Information Criterion (AIC) and Bayesian Information Criterion (BIC) were used to assess model fit. All analyses were stratified by exposure to sexual violence since the age of 18 (referred to as “exposed” in tables, figures, and text).
RESULTS
Table 1 reports the socio-demographic, mental health, stress, and coping characteristics of our total sample and stratified sample (stratified by exposure to sexual violence since the age of 18). Of the total sample, the average age was 26.22 (±6.35) years, the majority of women received a high school education or more (85%), were formally employed (60%), had an individual annual income of less than $10,000 (59%), and reported being single for their relationship status (69%). In regards to mental health, 46% had depressive symptoms and 27% had severe PTSD symptoms. In regards to stress and coping variables, 68% reported a medium level of perceived stress, 35% a high level of social support, and 72% medium or high levels of resilience.
Table 1.
Characteristics of sample of Black women in Baltimore, Maryland, 2015-2018 (N=232)
| Total (n=232) | Exposed (n=94) | Unexposed (n=138) | |
|---|---|---|---|
| Variables | n (%) | n (%) | n (%) |
| SOCIO-DEMOGRAPHICS | |||
| Agea ** | 26.22 ± 6.35 | 28.26 ± 7.10 | 24.83 ± 5.38 |
| 18-24*** | 101 (44) | 29 (31) | 72 (52) |
| 25-34 | 105 (45) | 46 (49) | 59 (43) |
| 35-44 | 26 (11) | 19 (20) | 7 (5) |
| High school education or more* | 198 (85) | 75 (80) | 123 (89) |
| Formally employed* | 139 (60) | 47 (50) | 92 (67) |
| Unstable Housing* | 14 (6) | 10 (11) | 4 (3) |
| Individual Income | |||
| <$10,000 | 136 (59) | 59 ( 63) | 77 (56) |
| $10,000 - 29,999 | 75 (32) | 28 (30) | 47 (34) |
| >$30,000 | 21 (9) | 7 (7) | 14 (10) |
| Relationship Status | |||
| Single | 160 (69) | 64 ( 68) | 96 (70) |
| In Relationship | 63 (27) | 25 (27) | 38 (28) |
| Separated/Divorced/Widowed | 6 (3) | 3 (3) | 3 (2) |
| Other | 3 (1) | 2 (2) | 1 (1) |
| MENTAL HEALTH | |||
| Depressive symptomsa, c *** | 10.29 ± 6.46 | 13.28 ± 6.91 | 8.25 ± 5.25 |
| Severe Depressive symptoms*** | 106 (46) | 62 (66) | 44 (32) |
| PTSD symptomsa, b *** | 1.62 ± 1.12 | 2.19 ± 1.07 | 1.23 ± 0.99 |
| Severe/Extreme PTSD symptoms*** | 62 (27) | 40 (43) | 22 (16) |
| STRESS AND COPING | |||
| Perceived Stressa, b *** | 19.24 ± 7.13 | 22.03 ± 5.77 | 17.33 ± 7.36 |
| Low*** | 43 (19) | 7 (7) | 36 (26) |
| Medium | 157 (68) | 68 (72) | 89 (64) |
| High | 32 (14) | 19 (20) | 13 (9) |
| Social Supporta ** | 46.15 ± 10.34 | 42.99 ± 10.61 | 48.30 ± 9.61 |
| Low** | 75 (32) | 39 (41) | 36 (26) |
| Medium | 75 (32) | 33 (35) | 42 (30) |
| High | 82 (35) | 22 (23) | 60 (43) |
| Resiliencea, b ** | 24.38 ± 7.96 | 22.20 ± 8.40 | 25.86 ± 7.32 |
| Low** | 65 (28) | 37 (39) | 28 (20) |
| Medium | 84 (36) | 30 (32) | 54 (39) |
| High | 83 (36) | 27 (29) | 56 (41) |
Source: The ESSENCE Project 2015-2017;
[mean ± std dev.];
Past month;
Past week;
a p-value for statistical difference between Exposed/Unexposed using 2 for comparisons among categorical variables & F-statistic for comparison of means among continuous variables;
p-value≤0.05,
p-value≤0.01,
p-value≤0.001
Compared to unexposed women (Table 1), exposed women were significantly older, less likely to have at least a high school education, and more likely to be unemployed and unstably housed. In regards to mental health, exposed women were significantly more likely to have depressive symptoms and severe PTSD symptoms than unexposed women. In regards to stress and coping variables, exposed women reported significantly more perceived stress, less social support, and less resilience than unexposed women.
Table 2 displays the correlation matrix of depressive symptoms, PTSD symptoms, perceived stress, social support, and resilience. Among exposed women, greater social support and resilience were correlated with less depressive symptoms (r=−0.35, p≤0.01 and r=−0.26, p≤0.05, respectively) and less PTSD symptoms (r=−0.39, p≤0.05 and r=−0.18, p≤0.01, respectively). Among unexposed women, greater social support and resilience were correlated with less depressive symptoms (r=−0.19, p≤0.05 and r=−0.32, p≤0.01, respectively), whereas greater resilience was correlated with less PTSD symptoms (r=−0.30, p≤0.01).
Table 2.
Correlation Matrix of Mental Health, Perceived Stress and Coping of Black women in Baltimore, Maryland, 2015-2018
| Exposed (n=94) | Unexposed (n=138) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | 1 | 2 | 3 | 4 | 5 | Variables | 1 | 2 | 3 | 4 | 5 |
| 1: Depressive Symptoms | - | 1: Depressive Symptoms | - | ||||||||
| 2: PTSD Symptoms | 0.67*** | - | 2: PTSD Symptoms | 0.62*** | - | ||||||
| 3: Perceived Stress Score | 0.63*** | 0.50*** | - | 3: Perceived Stress Score | 0.61*** | 0.63*** | - | ||||
| 4: Social Support Score | −0.26* | −0.39** | −0.24* | - | 4: Social Support Score | −0.19* | −0.08 | −0.09 | - | ||
| 5: Resilience Score | −0.29** | −0.18 | −0.35** | 0.25* | - | 5: Resilience Score | −0.32** | −0.30** | −0.43*** | 0.21* | - |
Source: The ESSENCE Project 2015-2018;
p-value≤0.05,
p-value≤0.01,
p-value≤0.001
Table 3 reports the odds ratios of the associations between perceived stress, social support, and resilience on mental health problems. Among exposed women, for each point increase in perceived stress score, there is an increase in odds of having severe depressive symptoms (OR=1.26; 95%CI: 1.12-1.43). For each point increase in social support score (OR= 0.95; 95%CI: 0.91-1.00) and resilience score (OR=0.91; 95%CI: 0.85-0.97), there is a decrease in odds of having severe depressive symptoms, respectively. For every point increase in perceived stress score (OR=1.22; 95%CI: 1.10-1.35), the odds of having severe/extreme PTSD symptoms increases. For every point increase in social support score, the odds of having severe/extreme PTSD symptoms decreases (OR=0.94; 95%CI: 0.90-0.98). Among unexposed women, for each point increase in perceived stress score, there is a significant increase in odds of having severe depressive symptoms (OR=1.31; 95%CI: 1.18-1.46). For each point increase in resilience score, there is a decrease in odds of having severe depressive symptoms (OR=0.92; 95%CI: 0.88-0.97). For every point increase in perceived stress score, the odds of having severe/extreme PTSD symptoms increases (OR=1.38; 95% CI: 1.21-1.58).
Table 3.
Logistic Regression Models of Perceived Stress and Coping Variables on Depressive and Severe PTSD Symptoms among Black women in Baltimore, Maryland, 2015-2018 (N=232)
| Depressive Symptoms | Severe PTSD Symptoms | |||||||
|---|---|---|---|---|---|---|---|---|
| Exposed (n=94) |
Unexposed (n=138) |
Exposed (n =94) |
Unexposed (n=138) |
|||||
| Models 1-3: Bivariate | Models 1-3: Bivariate | Models 1-3: Bivariate | Models 1-3: Bivariate | |||||
| Variables | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Perceived Stress Score | 1.26*** | (1.12, 1.43) | 1.31*** | (1.18, 1.46) | 1.22*** | (1.10, 1.35) | 1.38*** | (1.21, 1.58) |
| Social Support Score | 0.95* | (0.91, 1.00) | 0.98 | (0.95, 1.02) | 0.94** | (0.90, 0.98) | 1.01 | (0.96, 1.07) |
| Resilience Score | 0.91** | (0.85, 0.97) | 0.92** | (0.88, 0.97) | 0.97 | (0.92, 1.02) | 0.95 | (0.89, 1.00) |
Source: The ESSENCE Project 2015-2018; OR=odds ratio; 95% CI=95% Confidence Interval;
p-value≤0.05,
p-value≤0.01,
p-value≤0.001
Figure 1 displays the pathway of mediation models of perceived stress and depressive symptoms via social support and resilience among (A) exposed and (B) unexposed women. Among exposed women, resilience partially mediated the association between perceived stress and depressive symptoms (Model 1c), attenuating the odds of perceived stress on depressive symptoms (OR=1.23, p≤0.01, compared to the bivariate association in Table 3 – OR=1.26, p≤0.01). The strength of the association between resilience and depressive symptoms slightly decreased between these models. Figure 2 displays the pathway of mediation model of perceived stress and severe PTSD symptoms through social support and resilience among (A) exposed and (B) unexposed women. Among exposed women, social support partially mediated the association between perceived stress and PTSD symptoms (Model 2a), attenuating the odds of perceived stress on PTSD symptoms (OR=1.20, p≤0.001, compared to the bivariate association in Table 3 – OR=1.22, p≤0.01). The strength of the association between perceived stress and PTSD symptoms slightly decreased between these models. Among unexposed women, social support and/or resilience did not significantly mediate the association between perceived stress and mental health problems.
Figure 1.
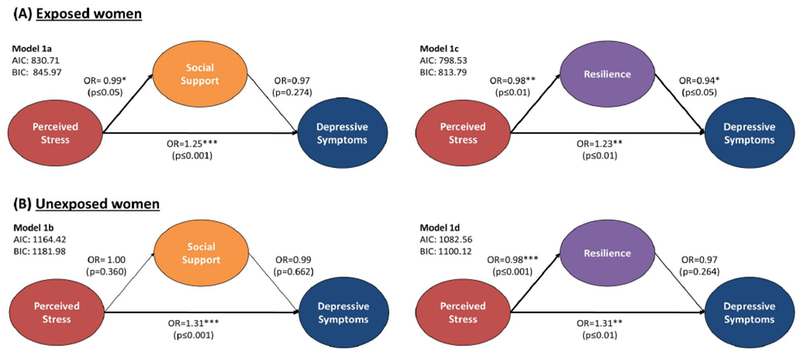
Pathway of mediation models of perceived stress and depressive symptoms through social support and resilience
Figure 2.
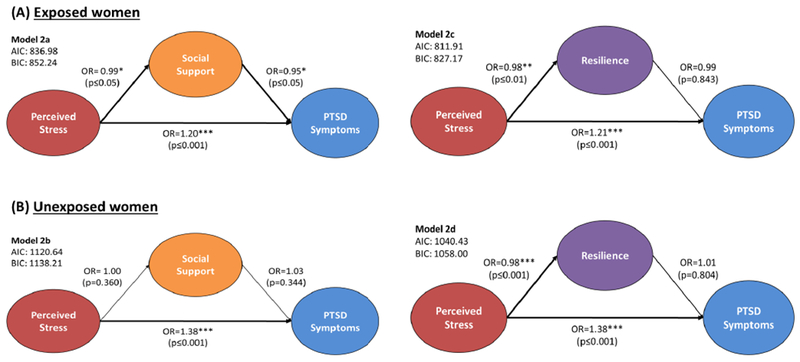
Pathway of mediation models of perceived stress and PTSD symptoms through social support and resilience
DISCUSSION
This study examined the relationship between perceived stress and mental health problems, as well as examined social support and resilience as mediators of this association among Black women in Baltimore, MD. We had three main findings. First, we found that perceived stress is very strongly associated with poor mental health, severely increasing depressive and PTSD symptomology. Second, we found that, among exposed women, the negative influences of perceived stress on mental health were partially mediated by resilience (depression) and social support (PTSD). Third, among unexposed women, we found that neither social support nor resilience mediated the association between perceived stress and mental health problems. These findings are discussed below in the context of public health implications.
We found that perceived stress is very strongly associated with poor mental health and severity of depressive and PTSD symptomology. It is imperative to acknowledge that Black women may perceive more stress due to their intersecting minority statuses as both racial and gender minorities. Previous findings assert that Black women experience a unique form of stress and discrimination that is specific to their race-gender subpopulation, supporting the minority stress model. Racial and gender discrimination may also give rise to additional stressors through the denial of opportunities and being systematically placed into stressful social contexts (Brown, 2003), indirectly increasing the risk for mental health problems (Perry et al., 2013). Experiencing these chronic stressors may trigger socio-psychological processes that reduce Black women’s ability to cope with stress and increase their vulnerability to mental health problems. Future interventions should address the race-gender specific stress experienced by Black women and enhance their coping resources to mitigate the adverse influence of stress on mental health.
Resilience partially mediated the association between perceived stress and depressive symptoms among exposed women. This is noteworthy as exposed women reported significantly less resilience compared to unexposed women in our sample. Therefore, resilience may serve as an effective form of coping against the robust negative effects of perceived stress on depression in this population. This supports previous research that found that women who experienced intimate partner violence but had relatively strong resilience were not significantly suffering from depression or other interpersonal difficulties (Anderson et al., 2012). However, there are relatively few studies and reviews to guide the development of interventions that promote resilience among women who experienced sexual violence (Herrman et al., 2011). Research studies and interventions that leverage resilience in order to reduce depression among abused women are needed.
Social support partially mediated the association between perceived stress and severe PTSD symptoms among our sample of exposed women. As exposed women also reported significantly less social support than unexposed women in our sample, social support can serve as an effective coping strategy against perceived stress and PTSD. This is consistent with a previous study that found greater social support was associated with lower PTSD severity among women who experienced child abuse and adult sexual violence (Ozbay et al., 2007; Schumm et al., 2006). High quality social support may reduce PTSD by buffering against trauma-related psychopathology (Ozbay et al., 2007). Perhaps, engaging with a social network with more diverse perspectives on violence provides greater access to coping resources like social support for abused women (Platt et al., 2014). Interventions that engage women exposed to trauma in social support-based activities may improve coping strategies and mitigate the risk of developing PTSD.
Neither social support nor resilience mediated the association between perceived stress and mental health among unexposed women. Our findings highlight the intersectionality of minority stress and coping among Black women, indicating that coping resources of social support and resilience may be salient in buffering stress effects on mental health among women who experienced sexual violence since age 18. It is possible that unabused women in our study experience forms of minority stress that require nuanced coping resources to avoid mental health problems. In terms of the role of abuse and trauma in the association between perceived stress and mental health, our findings indicate that abused women experience higher levels of perceived stress, but lower levels of social support and resilience. Abused women may be more vulnerable to the negative effects of perceived stress on mental health problems than unabused women, a conclusion supported by a review of previous studies (Schneiderman et al., 2005). This warrants further study among samples of Black women with diverse experiences of abuse, trauma and stress (racial and gender discrimination and stigma). Future research should aim to better understand what factors influence coping strategies and mitigate mental health problems among this population.
These findings should be considered in light of several limitations. First, mental health problems are especially stigmatized in the Black community, and it is possible that women in our sample devalued their mental health symptoms as a result (Ward et al., 2013). Therefore, the reported associations between perceived stress and mental health reported may be an underestimate. Nevertheless our measures of depressive and PTSD symptoms (CES-D-10 and NSESSS) demonstrated reasonable scores on Cronbach’s alpha measure of internal consistency (acceptable to good [0.7≤α<0.9] for CES-D-10 and excellent [0.9≤α] for NSESSS). Although our measure of depressive symptomology has been validated in samples of women who experienced sexual assault (Bryant-Davis et al., 2010), qualitative research would provide a richer data on the mechanisms linking stress and mental health problems in Black women. Second, as this is a cross-sectional analysis, we are unable to determine the temporal relationship between the outcome and exposure variables. Longitudinal research designs would allow us to examine the potentially causal effects of perceived stress and social-psychological resources on mental health problems among Black women, in particular those who have experienced violence. Finally, stress coping measures such as social support and resilience are dynamic and complex, containing multiple dimensions and changing in strength with the nature and context of the stressor. For example, resilience may change over time, thus measures of resilience should reflect this dynamic process of adapting to adversity and trauma (Southwick et al., 2014). Future research on these associations should consider more comprehensive and dynamic measures of social support and resilience to capture these theoretical and substantive shortcomings. Despite these limitations, this study emphasizes the importance of leveraging social support and resilience to address stress and improve mental health problems among Black women survivors of sexual violence.
This study finds support for leveraging social support and resilience to reduce the negative mental health effects of sexual violence among Black women. Both are targetable social factors, and our findings indicate that both social support and resilience are much lower among women exposed to sexual violence. As findings are consistent with the theory of stress and coping through the lens of the minority stress model, it is crucial to bolster social support and resilience among abused women to improve their health outcomes. For instance, the early aftermath of sexual violence may offer a critical period for enhancing social support and resilience. Social support interventions occurring after recent assault that incorporate engaging natural supports (i.e., family members, friends, current romantic partners) have been found to prevent avoidance symptoms and impart coping skills, as they ensure survivors have support and reminders to implement these skills in their daily lives (Dworkin and Schumacher, 2018). Additionally, studies find that incorporating socio-cultural elements may facilitate better intervention outcomes and likely leverages resilience in coping after sexual violence (Alim et al., 2008; Williams et al., 2014). Interventions that employ strategies that help increase social support and enhance resilience may improve the mental health of abused women.
Highlights.
In our sample, 46% experienced depression and 27% experienced severe PTSD.
Resilience partially mediated association between perceived stress and depressive symptoms among women exposed to sexual violence.
Social support partially mediated the association between perceived stress and severe PTSD symptoms among women exposed to sexual violence.
Neither social support nor resilience mediated association between perceived stress and mental health among women not exposed to sexual violence.
ACKNOWLEDGMENTS
The authors would like to thank the participants and those involved with data collection for the ESSENCE Project.
FUNDING
This research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD077891), the National Institute of Drug Abuse (K01DA031593; T32DA023356), the National Institute on Minority Health and Health Disparities (L60MD003701; L60MD011184), and the National Institute of Alcohol Abuse and Alcoholism (K01AA025009). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST
There is no conflict of interest to declare.
REFERENCES
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL, Syme SL, 1994. Socioeconomic status and health: the challenge of the gradient. American psychologist 49, 15. [DOI] [PubMed] [Google Scholar]
- Alim TN, Feder A, Graves RE, Wang Y, Weaver J, Westphal M, Alonso A, Aigbogun NU, Smith BW, Doucette JT, 2008. Trauma, resilience, and recovery in a high-risk African-American population. American Journal of Psychiatry 165, 1566–1575. [DOI] [PubMed] [Google Scholar]
- Almeida DM, Neupert SD, Banks SR, Serido J, 2005. Do daily stress processes account for socioeconomic health disparities? The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 60, S34–S39. [DOI] [PubMed] [Google Scholar]
- Anderson KM, Renner LM, Danis FS, 2012. Recovery: Resilience and growth in the aftermath of domestic violence. Violence against women 18, 1279–1299. [DOI] [PubMed] [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL, 1994. Screening for depression in well older adults: Evaluation of a short form of the CES-D. American journal of preventive medicine 10, 77–84. [PubMed] [Google Scholar]
- Brody DJ, Pratt LA, Hughes JP, 2018. Prevalence of Depression Among Adults Aged 20 and Over: United States, 2013-2016. NCHS data brief, 1–8. [PubMed] [Google Scholar]
- Brown DR, 2003. A conceptual model of mental well-being for African American women. In and out of our right minds: The mental health of African American women 15, 301. [Google Scholar]
- Bryant-Davis T, Ullman SE, Tsong Y, Tillman S, Smith K, 2010. Struggling to survive: Sexual assault, poverty, and mental health outcomes of African American women. American Journal of Orthopsychiatry 80, 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell-Sills L, Stein MB, 2007. Psychometric analysis and refinement of the Connor-Davidson resilience scale (CD-RISC): validation of a 10-item measure of resilience. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies 20, 1019–1028. [DOI] [PubMed] [Google Scholar]
- Chesney E, Goodwin GM, Fazel S, 2014. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World psychiatry 13, 153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R, 1983. A global measure of perceived stress. Journal of health and social behavior, 385–396. [PubMed] [Google Scholar]
- Cunradi CB, Caetano R, Schafer J, 2002. Socioeconomic predictors of intimate partner violence among White, Black, and Hispanic couples in the United States. Journal of family violence 17, 377–389. [Google Scholar]
- Dworkin ER, Schumacher JA, 2018. Preventing posttraumatic stress related to sexual assault through early intervention: A systematic review. Trauma, Violence, & Abuse 19, 459–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gheshlagh RG, Sayehmiri K, Ebadi A, Dalvandi A, Dalvand S, Maddah SSB, Tabrizi KN, 2017. The relationship between mental health and resilience: A systematic review and meta-analysis. Iranian Red Crescent Medical Journal 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb BH, 2000. Selecting and planning support interventions. Social support measurement and intervention: A guide for health and social scientists, 195–220. [Google Scholar]
- Herrman H, Stewart DE, Diaz-Granados N, Berger EL, Jackson B, Yuen T, 2011. What is resilience? The Canadian Journal of Psychiatry 56, 258–265. [DOI] [PubMed] [Google Scholar]
- Holden K, Hernandez N, Wrenn G, Belton A, 2017. Resilience: Protective Factors for Depression and Post Traumatic Stress Disorder among African American Women? Health, Culture and Society 9, 12–29. [Google Scholar]
- Hood S, Golembiewski E, Benbow K, Sow H, Sanders Thompson V, 2017. Who Can I Turn To? Emotional Support Availability in African American Social Networks. Social Sciences 6, 104. [Google Scholar]
- Howell KH, Thurston IB, Schwartz LE, Jamison LE, Hasselle AJ, 2017. Protective factors associated with resilience in women exposed to intimate partner violence. [DOI] [PMC free article] [PubMed]
- Kilpatrick D, Resnick H, Friedman M, 2013. National Stressful Events Survey PTSD Short Scale (NSESS-PTSD).
- Lacey KK, Parnell R, Mouzon DM, Matusko N, Head D, Abelson JM, Jackson JS, 2015. The mental health of US Black women: the roles of social context and severe intimate partner violence. BMJ open 5, e008415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S, 1984. Stress, Appraisal, and Coping. Springer, New York. [Google Scholar]
- LeBeau R, Mischel E, Resnick H, Kilpatrick D, Friedman M, Craske M, 2014. Dimensional assessment of posttraumatic stress disorder in DSM-5. Psychiatry research 218, 143–147. [DOI] [PubMed] [Google Scholar]
- Mary S, Dolbier C, 2008. Evaluation of a Resilience Intervention to Enhance Coping Strategies and Protective Factors and Decrease Symptomatology. Journal of American College Health 56, 445–453. [DOI] [PubMed] [Google Scholar]
- Meyer IH, 2003. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin 129, 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olff M, 2017. Sex and gender differences in post-traumatic stress disorder: an update. European Journal of Psychotraumatology 8, 1351204. [Google Scholar]
- Ozbay F, Johnson DC, Dimoulas E, Morgan C III., Charney D, Southwick S, 2007. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry (Edgmont) 4, 35. [PMC free article] [PubMed] [Google Scholar]
- Perry BL, Harp KL, Oser CB, 2013. Racial and gender discrimination in the stress process: Implications for African American women’s health and well-being. Sociological Perspectives 56, 25–48. [PMC free article] [PubMed] [Google Scholar]
- Platt J, Keyes KM, Koenen KC, 2014. Size of the social network versus quality of social support: which is more protective against PTSD? Social psychiatry and psychiatric epidemiology 49, 1279–1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasad BV, 2016. Chronic Mental Illness and the Changing Scope of Intervention Strategies, Diagnosis, and Treatment (Advances in Psychology, Mental Health, and Behavioral Studies). IGI Global. [Google Scholar]
- Qu Z, Tian D, Zhang Q, Wang X, He H, Zhang X, Huang L, Xu F, 2012. The impact of the catastrophic earthquake in China’s Sichuan province on the mental health of pregnant women. Journal of affective disorders 136, 117–123. [DOI] [PubMed] [Google Scholar]
- Sabri B, Bolyard R, McFadgion AL, Stockman JK, Lucea MB, Callwood GB, Coverston CR, Campbell JC, 2013. Intimate partner violence, depression, PTSD, and use of mental health resources among ethnically diverse black women. Social work in health care 52, 351–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneiderman N, Ironson G, Siegel SD, 2005. Stress and health: psychological, behavioral, and biological determinants. Annu. Rev. Clin. Psychol 1, 607–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumm JA, Briggs-Phillips M, Hobfoll SE, 2006. Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among inner-city women. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies 19, 825–836. [DOI] [PubMed] [Google Scholar]
- Southwick SM, Bonanno GA, Masten AS, Panter-Brick C, Yehuda R, 2014. Resilience definitions, theory, and challenges: Interdisciplinary perspectives. European journal of psychotraumatology 5, 25338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southwick SM, Vythilingam M, Charney DS, 2005. The psychobiology of depression and resilience to stress: implications for prevention and treatment. Annu. Rev. Clin. Psychol 1, 255–291. [DOI] [PubMed] [Google Scholar]
- Talwar P, 2017. The Role of Social Support in Mediating Stress and Depression. Online Journal of Health and Allied Sciences 16. [Google Scholar]
- Thorsteinsson EB, Ryan S, Sveinbjornsdottir S, 2013. The mediating effects of social support and coping on the stress-depression relationship in rural and urban adolescents. Open Journal of Depression 2, 1–6. [Google Scholar]
- Ward E, Wiltshire JC, Detry MA, Brown RL, 2013. African American men and women’s attitude toward mental illness, perceptions of stigma, and preferred coping behaviors. Nursing Research 62, 185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams M, Malcoun E, Sawyer B, Davis D, Nouri L, Bruce S, 2014. Cultural adaptations of prolonged exposure therapy for treatment and prevention of posttraumatic stress disorder in African Americans. Behavioral Sciences 4, 102–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods-Giscombé CL, Lobel M, 2008. Race and gender matter: A multidimensional approach to conceptualizing and measuring stress in African American women. Cultural Diversity and Ethnic Minority Psychology 14, 173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet GD, Dahlem NW, Zimet SG, Farley GK, 1988. The multidimensional scale of perceived social support. Journal of personality assessment 52, 30–41. [DOI] [PubMed] [Google Scholar]


