Abstract
Purpose
To evaluate the protective effect of applying an ophthalmic viscosurgical device (OVD) to the ocular surface during cataract surgery and its ability to prevent dry eye syndrome.
Methods
Twenty-four patients aged 50 to 75 years who underwent cataract surgery at Seoul National University Bundang Hospital and agreed to participate in the study were included and divided into two groups: a study group who underwent cataract surgery after application of an OVD to the ocular surface, and a control group who underwent cataract surgery without application of an OVD. DisCoVisc was used as the OVD in the study group, while other factors including surgical techniques and administration of anesthetic agents were performed in both groups in the same manner. Indicators of dry eye syndrome including ocular staining score, tear break-up time, and tear osmolality were analyzed. Ocular surface disease index and a visual analog scale were analyzed for dry eye symptoms, and the amount of balanced salt solution used during surface irrigation and operation time were also analyzed.
Results
Significant improvement in the tear break-up time, corneal ocular staining score, and ocular surface disease index score in the study group compared with the control group one week after operation (by the Mann-Whitney test). Use of OVD was associated with longer operating time.
Conclusions
OVD applied to the ocular surface during cataract surgery had a protective effect on the ocular surface one week after surgery.
Keywords: Cataract extraction, Dry eye syndromes, Ophthalmic viscosurgical device
Several studies have reported that, after cataract surgery, patients suffer from newly developed ocular dryness or those with preoperative diagnosis of dry eye syndrome had worsened dry eye symptoms [1,2,3]. Despite successful vision improvement after uneventful cataract surgery, ocular dryness causes visual impairment due to foreign body sensation, dryness, and instability of the tear layer, and is considered as the main factor for lowering patient satisfaction after surgery [4,5].
The causes of dry eye syndrome after cataract surgery include corneal nerve damage due to corneal incision [1], eye surface damage due to application of ophthalmic solutions such as local anesthesia during surgery, pH change due to persistent ocular surface irrigation during surgery, conjunctival goblet cell damage [6,7], ocular surface dryness during surgery, free radical release due to ultrasound energy [8], surgical microscope-light exposure during surgery [9], femtosecond laser application [10], and suction speculum use [11]. Still, the exact cause remains unclear.
Based on these mechanisms, methods to reduce the extent of corneal incision, operation time, exposure to causal factors listed above, and manipulation of the cornea during surgery have been proposed [12]. Reports have indicated that common treatments of dry eye syndrome such as ocular surface anti-inflammatory treatment [13], artificial tears, and omega-3 fatty acid ingestion [14] improve symptoms to a certain extent [15], but a confirmed treatment method that prevents and improves patient discomfort is not yet known.
An ophthalmic viscosurgical device (OVD) used to maintain anterior chamber space and prevent damage to intraocular tissue during cataract surgery is excellent for protection of corneal endothelial cells [16]. Reports have indicated that OVD applied to the ocular surface during cataract surgery results in less ocular surface damage 2 hours and 24 hours after operation than balanced salt solution (BSS) irrigation on the surface [17]. Therefore, an OVD thinly coated on the corneal surface during cataract surgery is expected to greatly reduce corneal epithelial damage from continuous intraoperative perfusion of the ocular surface without interfering with the visual field.
The purpose of this study was to evaluate the protective effect on the ocular surface and ability to prevent dry eye syndrome of an OVD applied to the ocular surface during cataract surgery.
Materials and Methods
This prospective study was conducted from August 2014 to December 2015. A total of 24 eyes from 24 patients aged 50 to 75 years who were diagnosed with level 2 dry eye syndrome [18] or less at the time of diagnosis and who agreed to participate in this study were enrolled. As difficulty in corneal surface evaluation was expected in patients with dry eye syndrome more severe than level 2, we enrolled patients with mild dry eye syndrome of level 2 or less. The patients were divided into two groups: a study group, consisting of 13 eyes of 13 patients, in which the ocular surface area exposed during cataract surgery was coated with a single application of the OVD at the beginning of surgery, and cataract surgery was performed without BSS perfusion on the ocular surface; and a control group, consisting of 11 eyes of 11 patients, in which cataract surgery was performed without OVD application to the ocular surface. The protective effect of the OVD on the ocular surface was evaluated by comparing the signs and symptoms of dry eye syndrome between the two groups after cataract surgery. All patients were given an explanation of the aims of the study, and informed consent was obtained before the study. The study was conducted in accordance with tenets of the Helsinki Declaration and under approval of the institutional review board of Seoul National University Bundang Hospital (B-1110/138-009).
Systemic and ocular history of the patients, ocular staining score (OSS), tear break-up time (BUT), and tear osmolality, which are indicators of dry eye syndrome, were analyzed. Ocular surface disease index (OSDI) and visual analog scale (VAS) were analyzed for dry eye symptoms. The amount of BSS used during surface irrigation and operation time were also analyzed.
Exclusion criteria included previous ocular surgery including refractive surgery, severe dry eye syndrome of level 3 or higher, infectious ocular diseases, severe ocular surface disease, other systemic diseases that can affect the eye, and anticholinergic medication that may cause dry eye syndrome or eye drops that may affect the ocular surface.
OSDI and VAS questionnaires were used to evaluate subjective symptoms of dry eye syndrome preoperatively and at 1 week and 1 month after surgery. The OSDI questionnaire consists of five questions related to dry eye symptoms, four questions to assess the degree of disability in daily life, and three questions related to environmental stimuli [19].
The VAS questionnaire comprises self-assessment of ocular discomfort for 2 weeks based on the time the questionnaire was received. Ocular symptoms related to dry eye such as ocular itching, foreign body sensation, burning, pain and dryness, blurred vision, sensation of photophobia, ocular redness, and sensations of tearing were quantified and summarized using the VAS scale.
Objective ophthalmic examination such as BUT, ocular surface staining, and tear osmolality were performed preoperatively, and 1 week and 1 month postoperatively. Differences between the two groups were analyzed. BUT was measured by dropping 0.25% fluorescein solution in each eye, allowing eye blinks for a few seconds, and recording the time of a tear-film defect under slit-lamp biomicroscopy with blue filter. After staining with fluorescein solution, the OSS of each eye based on the Sjögren's International Collaborative Clinical Alliance OSS form was evaluated. Degree of corneal epithelial damage was evaluated using a numerical point scale as follows: 0, absence of surface punctate epithelial erosion (PEE); 1, presence of 1–5 of PEEs; 2, presence of 5–30 PEEs; and 3, presence of >30 PEEs. Degree of conjunctival epithelial damage was graded with the lesions on the medial and lateral sides of the conjunctiva as follows: grade 0, absence of lesion; grade 1, presence of 10–32 lesions; grade 3, presence of 33–100 lesions; and grade 4, presence of over 100 lesions. An additional point is added if (1) PEE occurred in the central 4-mm diameter portion of the cornea; (2) 1 or more filaments were seen anywhere on the cornea; or (3) 1 or more patches of confluent staining, including linear stains, were found anywhere on the cornea [20]. Tear osmolality was measured using Tearlab (TearLab Corp., San Diego, CA, USA) with 50-nL tear samples obtained from the lower conjunctival sac of patient's bilateral eyes.
In the study group, a commercial OVD, DisCoVisc (Alcon Laboratories, Fort Worth, TX, USA) was applied evenly on the ocular surface before performing surgery, and irrigation of the ocular surface with BSS was withheld during the operation; whereas in the control group, corneal surface irrigation was performed without applying OVD. The surgical procedure was performed after applying topical anesthetic, Alcaine (Alcon, Irvine, CA, USA), to the target eye. Subsequently, a 2.2-mm clear corneal incision was made. The OVD (DisCoVisc) was infused into the anterior chamber, and the lens was removed by inserting a phacoemulsification device through the corneal incision. Intraocular lens was inserted through the incision, and the previously injected OVD was aspirated. At the end of surgery, hydro-sealing of the corneal incision was performed. After phacoemulsification and aspiration of the lens, and aspiration of the OVD were performed, partial leakage of BSS occurred through the corneal wound to the ocular surface. Surgical techniques except BSS irrigation and OVD surface application were carried out in the same way in both groups. In all cases, a suction speculum was used, and the total operation time and amount of BSS used for ocular surface irrigation were recorded.
Objective ocular dryness index and subjective symptom index at 1 week and 1 month after surgery were compared, and the degree of dry eye syndrome between the two groups was evaluated to confirm the effect of OVD application.
Statistical analysis was performed using IBM SPSS Statistics ver. 22.0 (IBM Corp., Armonk, NY, USA) and the Mann-Whitney test was performed to compare preoperative and postoperative data in each group. The Mann-Whitney test adjusted with Bonferroni's correction was used to compare the values between the two groups at each time point. The Friedman test was used to compare changes after cataract surgery in both groups, and p-values <0.05 were considered statistically significant.
Results
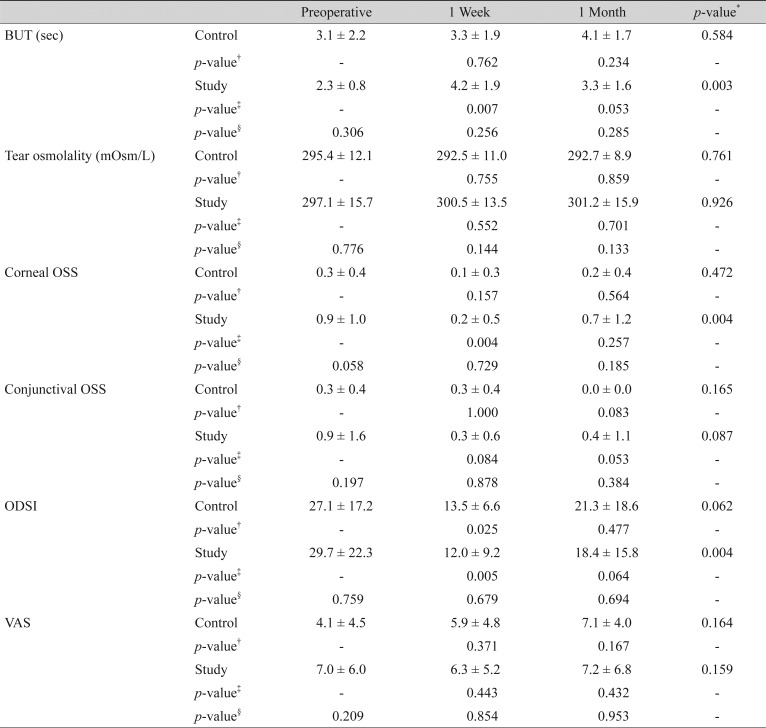
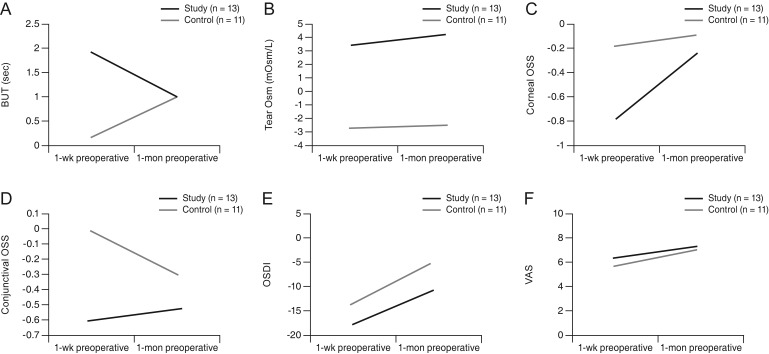
BUT at the preoperative time-point was 2.3 ± 0.8 seconds in the study group and 3.1 ± 2.2 seconds in the control group, which was not significantly different between the two groups. BUT at 1 week after surgery was 4.2 ± 1.9 seconds in the study group and 3.3 ± 1.9 seconds in the control group, and BUT at 1 month after surgery was 3.3 ± 1.6 seconds in the study group and 4.1 ± 1.7 seconds in the control group, which was not significantly different between the two groups at either period. In the comparison of BUT between preoperative, postoperative 1-week, and 1-month follow-up in each group, a statistically significant difference was seen for the study group (p = 0.003, Friedman test) (Table 1). Analysis of the differences in BUT 1-week postoperation compared to the preoperative value showed there was a statistically significant increase in BUT in the study group (p = 0.007, Mann-Whitney test) (Fig. 1A).
Table 1. Changes in BUT, tear osmolality, corneal and conjunctival OSS, OSDI, and VAS after cataract surgery.
Values are presented as mean ± standard deviation; Control group: cataract surgery without application of ophthalmic viscosurgical device to the ocular surface; Study group: cataract surgery with application of ophthalmic viscosurgical device to the ocular surface.
BUT = tear break-up time; OSS = ocular staining score; OSDI = ocular surface disease index; VAS = visual analog scale.
*Comparison between parameters at each period, repeated-measures ANOVA test; †Comparison with pretreatment data in control group, Mann-Whitney test; ‡Comparison with pretreatment data in study group, Mann-Whitney test; §Comparison between the two groups, Mann-Whitney test.
Fig. 1. Differences between preoperative and postoperative dry eye evaluation values at 1 week and 1 month after cataract. (A) Tear break-up time (BUT), (B) tear osmolality (Osm), (C) corneal ocular staining score (OSS), (D) conjunctival ocular staining score, (E) ocular surface disease index (OSDI), and (F) visual analog scale (VAS).
Preoperative tear osmolality was 297.1 ± 15.7 mOsm/L in the study group and 295.4 ± 12.1 mOsm/L in the control group. Tear osmolality values of 300.5 ± 13.5 mOsm/L in the study group and 292.5 ± 11.0 mOsm/L in the control group 1 week after operation, and those of 301.2 ± 15.9 mOsm/L in the study group and 292.7 ± 8.9 mOsm/L in the control group 1 month after surgery were obtained, without significant difference between the two groups (Table 1). There was no statistically significant difference in tear osmolality before and after surgery in the study and control groups (p = 0.761 and p = 0.926, respectively; Friedman test) (Fig. 1B).
The preoperative corneal staining score was 0.9 ± 1.0 in the study group and 0.3 ± 0.4 in the control group, with no statistically significant difference. Corneal staining score at 1 week after surgery was 0.2 ± 0.5 in the study group and 0.1 ± 0.3 in the control group, and after 1 month was 0.7 ± 1.2 in the study group and 0.2 ± 0.4 in the control group, with no significant difference. In the comparison of corneal OSS between preoperative, postoperative 1-week, and 1-month period in each group, statistically significant difference was seen in the study group (p = 0.004, Friedman test) (Table 1). In the analysis of the differences in corneal OSS as compared to preoperative value, there was a statistically significant decrease in the study group 1 week after operation (p = 0.004, Mann-Whitney test) (Fig. 1C).
The preoperative conjunctival staining score was 0.9 ± 1.6 in the study group and 0.3 ± 0.4 in the control group with no statistically significant difference. Corneal staining score at 1 week after surgery was 0.3 ± 0.6 in the study group, 0.3 ± 0.4 in the control group, and after 1 month was 0.4 ± 1.1 in the study group and 0.0 ± 0.0 in the control group with no significant difference (Table 1). The conjunctival staining score was not significantly different between the study group and control group before and after surgery (p = 0.165 and p = 0.087, respectively; Friedman test) (Fig. 1D).
The preoperative OSDI score was 29.7 ± 22.3 in the study group and 27.1 ± 17.2 in the control group with no significant difference. OSDI score at 1 week after surgery was 12.0 ± 9.2 in the study group, 13.5 ± 6.6 in the control group, and after 1 month was 18.4 ± 15.8 in the study group and 21.3 ± 18.6 in the control group, with no significant difference. In comparison of OSDI between preoperative, postoperative 1-week, and 1-month period in each group, statistically significant difference was seen in the study group (p = 0.004, Friedman test) (Table 1). In analysis of differences in OSDI as compared to preoperative value, there was a statistically significant decrease in OSDI in the control and study groups 1-week postoperation (p = 0.025, p = 0.005, respectively; Mann-Whitney test) (Fig. 1E).
The preoperative VAS score was 7.0 ± 6.0 in the study group and 4.1 ± 4.5 in the control group and there was no statistically significant difference. VAS score at 1 week after surgery of 6.3 ± 5.2 in the study group and 5.9 ± 4.8 in the control group, and after 1 month of 7.2 ± 6.8 in the study group and 7.1 ± 4.0 in the control group were seen, with no significant difference (Table 1). The VAS score was not significantly different between the study group and control group before and after surgery (p = 0.164, p = 0.159, respectively; Friedman test) (Fig. 1F).
The amount of BSS applied to the eye surface during surgery was 0 mL in the experimental group and 7.6 ± 3.0 mL in the control group. The amount of BSS used in the total operation was 35.8 ± 6.8 mL in the study group and 33.9 ± 10.0 mL in the control group, and there was no significant difference between the two groups (p = 0.622). The total operation time was 502.8 ± 164.1 seconds in the study group and 412.0 ± 123.3 seconds in the control group, and there was also no statistically significant difference between the two groups (p = 0.168).
Discussion
Several reports have indicated that dry eye syndrome after cataract surgery occurs in about 10 to 35% of cases [3,21,22,23]. Patients suffering from dry eye syndrome after cataract surgery complain of symptoms such as foreign body sensation, ocular pain, blurred vision, and experience persistent discomfort despite improved vision after surgery [5].
Newly developed dry eye syndrome or worsened previous dry eye symptoms after cataract surgery involves several potential mechanisms. The benzalkonium chloride-component of eye drops is toxic to the eye surface [24], and exposure to the surgical microscope's light source affects dry eye symptoms [25,26]. In cataract surgery, corneal incision may damage normal corneal nerves resulting in decreased corneal sensitivity and dry eye symptoms [27]. Studies have demonstrated elevated postoperative levels of inflammatory cytokines, and decrease of postoperative Meibomian gland function as contributing factors in ocular dryness [28,29]. Moreover, existing symptoms of dry eye syndrome before cataract surgery worsen after surgery.
The purpose of this study was to investigate the effectiveness of OVD in terms of index change of dry eye syndrome by ocular surface irrigation performed to minimize ocular surface damage due to cataract surgery, which is considered as a mechanism for developing dry eye syndrome after surgery.
Previous reports have indicated rapid aggravation of dry eye symptom indicators including BUT immediately after surgery [3], which is in contrast to our results showing absence of significant deterioration in dry eye syndrome indicators in the control and study groups after surgery. Worsening of OSDI and VAS scores postoperatively occurred in about 30% of patients, which is similar to the findings of previous studies. In a previous study including 149 patients with a similar design as our study, the study group including patients with an OVD applied to the ocular surface showed significant improvement in the Schirmer test performed 1 week later, while the male patients of the study group who were previously diagnosed with dry eye syndrome showed significant improvement at 1 month after surgery. Surgery time showed greater inverse relationship with ocular surface staining index in the study group than the control group [30]. Similar to the findings of several studies, Yusufu et al. [31] have shown that in patients diagnosed with diabetes mellitus, at 1 and 3 days after the operation, the control group showed worsened dry eye symptoms while the study group showed significantly higher noninvasive BUT.
A previous study reported that corneal erosion occurred in 60% of the eyes with an OVD applied to the ocular surface during surgery but in 90% of control eyes at 2 hours after surgery. At postoperative 2 and 24 hours, the study group showed significantly improved foreign body sensation [17]. In previous studies, some indicators of dry eye syndrome showed improvement in a short time-period of 2 to 3 days after surgery in the group with OVD applied to the ocular surface. However, results of improved symptoms and signs of dry eye syndrome at a longer follow-up period were not available.
In our study, improvements in BUT, corneal staining score, and OSDI score over baseline preoperative data were maintained until 1 week after surgery, with statistical significance in the study group. OSDI or VAS showed no consistent change, indicating that subjective visual improvement and the dry eye symptoms of patients did not correlate with objective indicators, and correlated with patient satisfaction after surgery as previously shown in other studies [5]. Patient satisfaction after surgery can be assessed and correlated with postoperative dry eye symptoms in subsequent follow-up studies. In a previous study, tear osmolality showed no significant differences between treated and untreated eyes before cataract surgery, 1 month after surgery, and 3 months after surgery, and patients with tear osmolality of >312 mOsm/L were more likely to suffer from severe ocular discomfort after surgery [32]. In our study, although we did not evaluate the contralateral eye, tear osmolality was higher postoperatively in the group with relatively high tear osmolality before surgery, and lower than that before surgery in the control group. However, the results were not statistically significant, and the difference may be due to uneven distribution of patients with tear osmolality of >300 mOsm/L before surgery (study group, seven eyes; control group, four eyes).
Our results suggest that BUT, corneal staining scores, and OSDI score improved up to 1 week postoperatively, so that ocular surface damage due to corneal surface irrigation may contribute more to immediate postoperative dry eye symptoms than other proposed mechanisms.
In patients with an OVD applied to the ocular surface, despite lack of data supporting long-term improvement in dry eye syndrome, the approach was successful to prevent ocular surface damage caused by persistent intraoperative ocular surface perfusion and provided the advantage of a clear surgical view with no difference in surgical time.
Our study was limited by small sample sizes and uneven sex ratios for a limited age group, and a short operation time of about 10 minutes. Hence, this study did not have enough power to detect the effect of ocular surface perfusion. Dry eye symptoms and signs were evaluated at postoperative 1 week and 1 month, however previous studies have shown that dry eye syndrome significantly deteriorated for 1 month after surgery and gradually improved over 6 months. We consider that evaluation for a longer follow-up period may yield more accurate results [33]. In addition, the evaluation of dry eye symptoms and signs according to presence or absence of preoperative dry eye syndrome could be assessed by further studies.
In conclusion, an OVD applied to the ocular surface during cataract surgery was effective for improving BUT, corneal staining score, and OSDI score until 1 week. This suggests that surface damage due to corneal surface irrigation may contribute more to immediate postoperative dry eye symptoms than other proposed mechanisms and may be prevented by applying an OVD to the corneal surface instead of corneal surface irrigation during cataract surgery.
Acknowledgements
This work was supported by grant no 02-2011-023 from the SNUBH Research Fund.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Costigan M, Scholz J, Woolf CJ. Neuropathic pain: a maladaptive response of the nervous system to damage. Annu Rev Neurosci. 2009;32:1–32. doi: 10.1146/annurev.neuro.051508.135531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khanal S, Tomlinson A, Esakowitz L, et al. Changes in corneal sensitivity and tear physiology after phacoemulsification. Ophthalmic Physiol Opt. 2008;28:127–134. doi: 10.1111/j.1475-1313.2008.00539.x. [DOI] [PubMed] [Google Scholar]
- 3.Li XM, Hu L, Hu J, Wang W. Investigation of dry eye disease and analysis of the pathogenic factors in patients after cataract surgery. Cornea. 2007;26(9 Suppl 1):S16–S20. doi: 10.1097/ICO.0b013e31812f67ca. [DOI] [PubMed] [Google Scholar]
- 4.Hardten DR. Dry eye disease in patients after cataract surgery. Cornea. 2008;27:855. doi: 10.1097/ICO.0b013e31816f6854. [DOI] [PubMed] [Google Scholar]
- 5.Szakats I, Sebestyen M, Toth E, Purebl G. Dry eye symptoms, patient-reported visual functioning, and health anxiety influencing patient satisfaction after cataract surgery. Curr Eye Res. 2017;42:832–836. doi: 10.1080/02713683.2016.1262429. [DOI] [PubMed] [Google Scholar]
- 6.Oh T, Jung Y, Chang D, et al. Changes in the tear film and ocular surface after cataract surgery. Jpn J Ophthalmol. 2012;56:113–118. doi: 10.1007/s10384-012-0117-8. [DOI] [PubMed] [Google Scholar]
- 7.Kato K, Miyake K, Kondo N, et al. Conjunctival goblet cell density following cataract surgery with diclofenac versus diclofenac and rebamipide: a randomized trial. Am J Ophthalmol. 2017;181:26–36. doi: 10.1016/j.ajo.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 8.Sahu PK, Das GK, Malik A, Biakthangi L. Dry eye following phacoemulsification surgery and its relation to associated intraoperative risk factors. Middle East Afr J Ophthalmol. 2015;22:472–477. doi: 10.4103/0974-9233.151871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cho YK, Kim MS. Dry eye after cataract surgery and associated intraoperative risk factors. Korean J Ophthalmol. 2009;23:65–73. doi: 10.3341/kjo.2009.23.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shao D, Zhu X, Sun W, et al. Effects of femtosecond laser-assisted cataract surgery on dry eye. Exp Ther Med. 2018;16:5073–5078. doi: 10.3892/etm.2018.6862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moon H, Yoon JH, Hyun SH, Kim KH. Short-term influence of aspirating speculum use on dry eye after cataract surgery: a prospective study. Cornea. 2014;33:373–375. doi: 10.1097/ICO.0000000000000072. [DOI] [PubMed] [Google Scholar]
- 12.Ram J, Gupta A, Brar G, et al. Outcomes of phacoemulsification in patients with dry eye. J Cataract Refract Surg. 2002;28:1386–1389. doi: 10.1016/s0886-3350(02)01387-1. [DOI] [PubMed] [Google Scholar]
- 13.Kawahara A, Utsunomiya T, Kato Y, Takayanagi Y. Comparison of effect of nepafenac and diclofenac ophthalmic solutions on cornea, tear film, and ocular surface after cataract surgery: the results of a randomized trial. Clin Ophthalmol. 2016;10:385–391. doi: 10.2147/OPTH.S101836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mohammadpour M, Mehrabi S, Hassanpoor N, Mirshahi R. Effects of adjuvant omega-3 fatty acid supplementation on dry eye syndrome following cataract surgery: a randomized clinical trial. J Curr Ophthalmol. 2016;29:33–38. doi: 10.1016/j.joco.2016.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhao X, Xia S, Chen Y. Comparison of the efficacy between topical diquafosol and artificial tears in the treatment of dry eye following cataract surgery: a meta-analysis of randomized controlled trials. Medicine (Baltimore) 2017;96:e8174. doi: 10.1097/MD.0000000000008174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ho JW, Afshari NA. Advances in cataract surgery: preserving the corneal endothelium. Curr Opin Ophthalmol. 2015;26:22–27. doi: 10.1097/ICU.0000000000000121. [DOI] [PubMed] [Google Scholar]
- 17.Giardini P, Hauranieh N, Gatto C, et al. Tripolymeric corneal coating gel versus balanced salt solution irrigation during cataract surgery: a retrospective analysis. Cornea. 2018;37:431–435. doi: 10.1097/ICO.0000000000001480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hyon JY, Kim HM, Lee D, et al. Korean guidelines for the diagnosis and management of dry eye: development and validation of clinical efficacy. Korean J Ophthalmol. 2014;28:197–206. doi: 10.3341/kjo.2014.28.3.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pflugfelder SC, Tseng SC, Sanabria O, et al. Evaluation of subjective assessments and objective diagnostic tests for diagnosing tear-film disorders known to cause ocular irritation. Cornea. 1998;17:38–56. doi: 10.1097/00003226-199801000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Whitcher JP, Shiboski CH, Shiboski SC, et al. A simplified quantitative method for assessing keratoconjunctivitis SICCA from the Sjogren’s Syndrome International Registry. Am J Ophthalmol. 2010;149:405–415. doi: 10.1016/j.ajo.2009.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu Z, Luo L, Zhang Z, et al. Tear film changes after phacoemulsification. Zhonghua Yan Ke Za Zhi. 2002;38:274–277. [PubMed] [Google Scholar]
- 22.Kasetsuwan N, Satitpitakul V, Changul T, Jariyakosol S. Incidence and pattern of dry eye after cataract surgery. PLoS One. 2013;8:e78657. doi: 10.1371/journal.pone.0078657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sajnani R, Raia S, Gibbons A, et al. Epidemiology of persistent postsurgical pain manifesting as dry eye-like symptoms after cataract surgery. Cornea. 2018;37:1535–1541. doi: 10.1097/ICO.0000000000001741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walker TD. Benzalkonium toxicity. Clin Exp Ophthalmol. 2004;32:657. doi: 10.1111/j.1442-9071.2004.00922.x. [DOI] [PubMed] [Google Scholar]
- 25.Hwang HB, Kim HS. Phototoxic effects of an operating microscope on the ocular surface and tear film. Cornea. 2014;33:82–90. doi: 10.1097/ICO.0000000000000001. [DOI] [PubMed] [Google Scholar]
- 26.Ipek T, Hanga MP, Hartwig A, et al. Dry eye following cataract surgery: the effect of light exposure using an in-vitro model. Cont Lens Anterior Eye. 2018;41:128–131. doi: 10.1016/j.clae.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 27.Kohlhaas M. Corneal sensation after cataract and refractive surgery. J Cataract Refract Surg. 1998;24:1399–1409. doi: 10.1016/s0886-3350(98)80237-x. [DOI] [PubMed] [Google Scholar]
- 28.El Ameen A, Majzoub S, Vandermeer G, Pisella PJ. Influence of cataract surgery on Meibomian gland dysfunction. J Fr Ophtalmol. 2018;41:e173–e180. doi: 10.1016/j.jfo.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 29.Han KE, Yoon SC, Ahn JM, et al. Evaluation of dry eye and meibomian gland dysfunction after cataract surgery. Am J Ophthalmol. 2014;157:1144–1150. doi: 10.1016/j.ajo.2014.02.036. [DOI] [PubMed] [Google Scholar]
- 30.He Y, Li J, Zhu J, et al. The improvement of dry eye after cataract surgery by intraoperative using ophthalmic viscosurgical devices on the surface of cornea: the results of a consort-compliant randomized controlled trial. Medicine (Baltimore) 2017;96:e8940. doi: 10.1097/MD.0000000000008940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yusufu M, Liu X, Zheng T, et al. Hydroxypropyl methylcellulose 2% for dry eye prevention during phacoemulsification in senile and diabetic patients. Int Ophthalmol. 2018;38:1261–1273. doi: 10.1007/s10792-017-0590-7. [DOI] [PubMed] [Google Scholar]
- 32.Gonzalez-Mesa A, Moreno-Arrones JP, Ferrari D, Teus MA. Role of tear osmolarity in dry eye symptoms after cataract surgery. Am J Ophthalmol. 2016;170:128–132. doi: 10.1016/j.ajo.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 33.Xue W, Zhu MM, Zhu BJ, et al. Long-term impact of dry eye symptoms on vision-related quality of life after phacoemulsification surgery. Int Ophthalmol. 2019;39:419–429. doi: 10.1007/s10792-018-0828-z. [DOI] [PubMed] [Google Scholar]