Abstract
Objectives:
This study intended to understand the risk of developing temporomandibular disorder among Saudi women who experienced a miscarriage.
Materials and Methods:
Two hundred and eight Saudi women from several hospitals’ gynecologic clinics in two areas in Saudi Arabia were screened to fill out the Impact of Events Scale-Revised (self-reporting questionnaire) Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition diagnostic criteria for posttraumatic stress disorder and a structured temporomandibular joint disorder (TMD) Questionnaire (Research Diagnostic Criteria for Temporomandibular Disorders). A single examiner did the clinical examination for temporomandibular joint (TMJ). One-hundred and fifty-eight of the participants were divided into two groups. Group A (85 participants) included females who had had a previous miscarriage, whereas Group B (73 participants) included females who had not had a miscarriage. IBM SPSS version 22.0 was used to conduct a nonparametric Chi-square test to find the significance of any observed differences.
Results:
Almost 40% of the participants had symptoms that qualified for possible TMD. Around 73% of the miscarried Saudi women in Group A showed symptoms of TMD. Furthermore, approximately 38% of the participants in Group B developed significant symptoms of TMD. The Chi-square test (Chi-test = 22.03 with P = 0.0001) shows highly significant association between treatment groups (control and study) and temporomandibular joint disorder group and non temporomandibular joint disorder group.
Conclusion:
Women who suffer from spontaneous single or recurrent miscarriages are advised to seek a dental specialist for diagnosis and prevention devices such as a night guard.
KEYWORDS: Chronic pain, facial muscles, headaches, miscarriages, posttraumatic stress disorder, Saudi, stress, temporomandibular disorder
INTRODUCTION
One primary problem with the emotional and psychological impact of traumatic events on individual health and well-being is that it could be a risk for developing unconscious parafunctional habits such as teeth grinding, which is highly associated with temporomandibular joint disorder (TMD). As Mottaghi and Zamani revealed in their published research in 2014, patients with posttraumatic stress disorder (PTSD) showed a significant imperfect TMJ function in comparison to the control group,[1] orofacial pain, and tooth wear consequences such as tooth loss that affects the quality of life.[1,2,3,4] A gap in the literature is found between the prevalence of TMD in miscarried women with or without posttraumatic stress disorder.
TEMPOROMANDIBULAR DISORDER
TMD symptoms could manifest in the body as myofascial pain, joint noises, jaw locking and clicking, limitations in the mouth opening, deviation of the jaw to one side of the face, and tinnitus. TMD is influenced by multiple factors and usually associated with many complications such as parafunctional teeth grinding.[5] The peak of sleep bruxism onset is between 20 and 45 years of age. It commonly occurs in females, and it is positively related to a highly stressful lifestyle.[6] Many researchers advise the patient who has a tooth wear condition to release his emotional stress.[7] In addition to tooth tissue loss and damage, resultant chronic headaches may impact one’s health, especially when associated with stressful factors.[8]
POSTTRAUMATIC STRESS DISORDER
PTSD is a psychological reaction to a negative event. This disorder can last for many years and can affect the quality of life, if not treated. PTSD affects the pain threshold and has constant symptoms. Up to 25% of women with a positive history of chronic and persistent negative life events are more likely to develop PTSD 1 month following a miscarriage.[2,3,9]
EARLY PREGNANCY LOSS
Early pregnancy loss (EPL) complications could be dangerous enough to threaten human life if it includes uncontrollable hemorrhage.[10,11] EPL can be classified as (a) spontaneous abortion or (b) induced abortion. In comparison to the general population, researchers found that in the same year of having a miscarriage, women might develop a psychological disorder or PTSD, and they are more likely to develop a persistent TMD.[12,13,14]
AIMS OF THE STUDY
This study intended to understand the relationship between miscarriage and TMD as a result of stress-coping behavior among Saudi women with signs and symptoms of PTSD.
MATERIALS AND METHODS
Ethical approval for the study was approved from the research center of the Riyadh Elm University with registration number FUGRP/2018/74.
A convenient sample was collected from the several governmental hospitals’ gynecologic clinics from two areas in Saudi Arabia: Riyadh and the Eastern Province. Between February 2018 and November 2018, 208 Saudi females whose ages ranged from 18 to 45 years with a mean age of 31.15 years and with no history of injury to the head and neck were screened for PTSD according to the Impact of Events Scale-Revised (IES-R)[15] after signing informed consent. We excluded any female who is single, pregnant, younger than 18 years or older than 45 years, who had any trauma to the head and neck, and who had experienced a miscarriage during the second or third trimester of pregnancy and non-Saudi females. The G*Power 3.1.9.2 (Düsseldorf, Heinrich Heine University, Germany) for Windows used to calculate the sample size at large effect with a confidence interval of 95% and a = 0.05 based on the Chi-square test with 1 degree of freedom revealed the need for 123 samples.
For blinding, 208 females were asked by the researcher (screener) to fill out the IES-R (prevalidated self-report questionnaire).[15] An Arabic version was obtained from the Harvard Program in Refugee Trauma and modified according to our aim of the study. It consisted of 22 items based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition diagnostic criteria for PTSD,[16] and the participants scored as stated by Weiss. On this test, scores that exceed 24 can be quite meaningful.[17] The single examiner (a prosthodontic specialist with several years of experience) fulfilled the Diagnostic Criteria for Temporomandibular Disorders for clinical and research applications (revised, reliable, and valid Axis I diagnostic methods for both muscle pain and joint pain). A structured TMD questionnaire for the criterion protocol included all the measures specified in the Research Diagnostic Criteria for Temporomandibular Disorders,[18] which also included a clinical examination of the TMJ and facial muscles for all the participants [Table 1]. We cannot deny the presence of some sample selection biases due to the limited access of the hospitals’ records. For this reason, we tried to overcome this weakness by performing the clinical examination for the 208 participants by a single examiner who did not know if the participants fulfilled the diagnostic criteria for PTSD or if the participant had a previous miscarriage.
Table 1.
Clinical examination of the temporomandibular joint and facial muscles
| The most reported symptoms of TMD by the examiner | Participants (%) | Study group (64) (%) | Control group (28) (%) | P |
|---|---|---|---|---|
| Pain in the jaw, temple, in the ear, or front of the ear on either side | 85 (53.8) | 61 (71) | 21 (28) | 0.000* |
| Headache that included the temple areas of the head | 60 (38.0) | 39 (45) | 18 (24) | 0.000* |
| Jaw joint noise(s) when patient moved her jaw | 63 (39.8) | 44 (51) | 16 (21) | 0.000* |
| Pain on the lateral palpation of the joint | 59 (37.3) | 42 (49) | 14 (19) | 0.000* |
| Sound on the lateral palpation of the joint | 58 (36.7) | 44 (51) | 13 (17) | 0.000* |
| Pain and limitation in lateral movement | 40 (25.3) | 35 (41) | 5 (6) | 0.000* |
| Mandibular inclination of the mouth opening | 36 (22.8) | 31 (36) | 4 (5) | 0.000* |
| Limitations in protrusive movements | 40 (25.3) | 31 (36) | 8 (10) | 0.000* |
| Clicking noise during chewing | 58 (36.7) | 46 (54) | 11 (15) | 0.000* |
| Pain in the temporal muscle | 95 (60.1) | 63 (74) | 29 (39) | 0.000* |
| Pain in the masseter muscle | 47 (29.7) | 31 (36) | 15 (20) | 0.000* |
Data expressed as n (%). Study group suffered from PTSD and had experienced miscarriage, control group suffered from PTSD and did not experience miscarriage, *Chi-square test was used for P values. PTSD=Posttraumatic stress disorder, TMD=Temporomandibular joint disorder
Only 158 of the participants who were positive for PTSD [Table 2] were included in the statistical analysis. The selected sample was divided into two groups: group A (85 participants), the study group, included females who had had a previous miscarriage in the first trimester (before January 2018) and Group B (73 participants), the control group, included the females who had not had a miscarriage.
Table 2.
Relationship between treatment (control and study) with temporomandibular joint disorder
| Miscarriage | Total | ||
|---|---|---|---|
| Yes (study group) | No (control group) | ||
| TMD symptoms (%) | |||
| Yes | 64 (40.5) | 28 (17.7) | 92 (58.2) |
| No | 21 (13.3) | 45 (28.5) | 66 (41.8) |
| Total | 85 (53.8) | 73 (46.2) | 158 (100) |
| Chi-square test | Value | 22.03 | |
| P | 0.000**** | P≤0.0001**** | |
****P<0.05 is statistically significant. Cross-tabulation shows there was highly significant association between treatment groups (control group and study group) and TMD and non-TMD. Study group suffered from PTSD and had experienced miscarriage, control group suffered from PTSD and did not experience a miscarriage. PTSD=Posttraumatic stress disorder, TMD=Temporomandibular joint disorder
STATISTICAL ANALYSIS
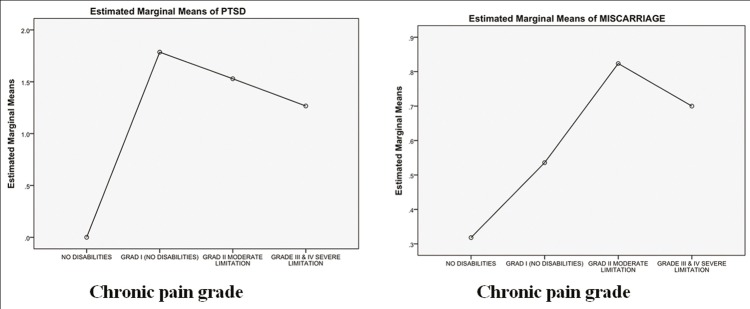
Descriptive statistics were calculated for all variables used for the demographic data and the most reported TMD symptoms by the participants in both the groups. Data from the 158 participants were typed into the statistical analysis software, IBM SPSS version 22.0. (IBM Corp, Armonk, NY, USA). The categorization of the variables and calculations was in percentages, and the numbers were done as shown in Table 1. For determining the difference and association between the two groups, the Chi-square test was utilized. Pearson’s Chi-square value = 22.03 and the difference between the groups were statistically significant at P < 0.0001. A high association exists between the TMD and miscarriage in the study group. Two-way cross-tabulation showed that patients with miscarriage were more likely to have TMD in comparison to the patients who did not experience a miscarriage. The difference between the groups was statistically significant at P < 0.0001 [Table 3]. Afterward, each group was divided into three subgroups depending on the intensity of TMD symptomatology (none, chronic pain grade (CPG) I, CPG II, and CPG III–IV). Testing of the differences between the variables was done by multivariate analysis of variance (MANOVA), with the dependent variable (CPG) and the independent variables (PTSD intensity and having a miscarriage).
Table 3.
Posttraumatic stress disorder scores on the Impact of Events Scale-Revised scale among the three subgroups in the miscarriage group and control group
| GCPS/PTSD | 24-32 points, n (%) | 32-36 points, n (%) | >37 points, n (%) | |
|---|---|---|---|---|
| Grade label | CPG | |||
| Study group (miscarriage) (n=85) | ||||
| None | 0 | 21 (24.7 | ||
| Low-intensity pain, without disability | I | 2 (2.3) | 13 (15.2) | |
| High-intensity pain, without disability | II | 12 (14.1) | 16 (18.8) | |
| Moderately limiting | III | 3 (3.5) | 7 (8.2) | 11 (12.9) |
| Control group (nonmiscarriage) (n=73) | ||||
| None | 0 | 45 (61.6) | ||
| Low-intensity pain, without disability | I | 4 (5.0 | 9 (12.0) | |
| High-intensity pain, without disability | II | 4 (5.0 | 2 (3.0) | |
| Moderately limiting | III | 3 (4.0) | 3 (4.0) | 3 (4.0) |
GCPS, CPG of TMD symptomatology scoring system of the RDC/TMD,[18] PTSD intensity scoring system of the IES-R scale.[16] PTSD=Posttraumatic stress disorder, GCPS=Graded Chronic Pain Scale, CPG=Chronic pain grade, RDC/TMD=Research Diagnostic Criteria for Temporomandibular Disorders, IES-R=Impact of Events Scale-Revised, TMD=Temporomandibular joint disorder
RESULTS
POSTTRAUMATIC STRESS DISORDER AMONG THE SAMPLE
One-hundred and fifty-eight females were included in the analysis. All the recruited women were nonsmokers, predominantly of primary school educational level (69%), and of moderate socioeconomic status, indicated by demographic data (65.2%). One-hundred and twelve of them reported an unemployment situation (70.9%) and 66 were forced to move house (41.8). The entire sample scored >24 points on the IES-R questionnaire: 72 women showed partial symptoms of PTSD, and their scores ranged between 24 and 32 points on the scale (15.18% of them had miscarriage, 1.9% of them experienced multiple miscarriages, and 30.37% of them had not experienced miscarriage). Thirty-two of them scored 33–36 points on the scale, and this is the cutoff point for a PTSD diagnosis (13.29% of them had a miscarriage, 12% of them experienced multiple miscarriages, and only 6.9% were from the control group). Fifty-four Saudi females had a high score which is >37 points on the scale (25.31% experienced a miscarriage, 17% of them had experienced multiple miscarriages, and 8.8% had not had a miscarriage). However, 49 members of the study group had suffered from miscarriage more than once (31% of the samples). More than half had a safe and stable marriage (48% of them scored 37 points and higher on the IES-R scale) [Table 3]. In addition, one-way MANOVA revealed in Table 4c that PTSD has a statistically significant effect on educational level (F = 3.127; P = 0.047; partial eta squared = 0.040), separation from partner (F = 30.276; P < 0.0001; partial eta squared = 0.288), being forced to move house (F = 14.588; P < 0.0001; partial eta squared = 0.658), and multiple miscarriages (F = 390.749; P < 0.0001; partial eta squared = 0.842), but there is no statistically significant effect of PTSD on employment status (F = 0.658; P = 520; partial eta squared = 0.009) and socioeconomics (F = 1.810; P = 0.167; partial eta squared = 0.024).
Table 4c.
Test of participants’ effectsa
| Source | Dependent variables | Type III SS | df | Mean square | F | P | Partial η2 |
|---|---|---|---|---|---|---|---|
| CPGb | PTSD | 92.898 | 3 | 30.966 | 153.575 | 0.000 | 0.749 |
| Miscarriage | 6.749 | 3 | 2.250 | 10.651 | 0.000 | 0.172 | |
| Multiple miscarriages | 11.188 | 3 | 3.729 | 25.394 | 0.000 | 0.331 | |
| Employment status | 17.323 | 3 | 5.774 | 58.178 | 0.000 | 0.531 | |
| Marital status | 4.070 | 3 | 1.357 | 6.455 | 0.000 | 0.112 | |
| Move house | 22.594 | 3 | 7.531 | 73.238 | 0.000 | 0.588 | |
| Socioeconomic | 1.258 | 3 | 0.419 | 1.306 | 0.275 | 0.025 | |
| Educational level | 4.209 | 3 | 1.403 | 7.211 | 0.000 | 0.123 | |
| PTSDc | Multiple miscarriages | 17.444 | 2 | 0.598 | 399.749 | 0.000 | 0.842 |
| Employment status | 0.133 | 2 | 0.066 | 0.658 | 0.520 | 0.009 | |
| Marital status | 8.973 | 2 | 4.486 | 30.276 | 0.000 | 0.288 | |
| Move house | 9.800 | 2 | 4.900 | 144.588 | 0.000 | 0.817 | |
| Socioeconomic | 1.128 | 2 | 0.564 | 1.810 | 0.167 | 0.024 | |
| Educational level | 0.13e | 2 | 0.066 | 0.658 | 0.520 | 0.009 |
aComputed using alpha=0.05, bCPG of TMD symptomatology scoring system of the RDC/TMD,[18] cPTSD intensity scoring system of the IES-R scale the sample categorized into three subgroups according to their IES-R scores.[16] RDC/TMD=Research Diagnostic Criteria for Temporomandibular Disorders, IES-R=Impact of Events Scale-Revised, PTSD=Posttraumatic stress disorder, TMD=Temporomandibular joint disorder
CLINICAL EXAMINATION OF THE TMJ AREA AMONG THE STUDY GROUP AND THE CONTROL GROUP
Eighty-one women described pain in the jaw, temple, in the ear, or front of the ear on either side (51.3%). Sixty-three of the participants had had jaw joint noises when they moved their jaw (39.8%). Myofascial pain persisted among 92 participants (58.2%). Pain on the lateral palpation of the joint was reported by 59 participants (37.3%) and sound on the lateral palpation of the joint was found in 36.7% of them. Pain in the temporal muscle was expressed by 95 women (60.1%). Fifty-eight females complained of clicking noise during mouth chewing (36.7%), limitation in protrusive and lateral movement noticed in 25.3% and 22.8% of them had an apparent inclination of the mandible during mouth opening. All the results were tested by the Chi-square test, and it was highly significant (P < 0.05). The results of Group A (85 participants), the study group, showed that 64 (40.5%) participants had TMD, whereas the remaining 21 (13.3%) participants did not have TMD. The results of Group B (73 participants), the control group, showed that only 28 (17.7%) of the participants had TMD, whereas the remaining 45 (28.5%) participants did not have TMD [Table 1].
The Chi-square test (Chi-test = 22.03 with P = 0.0001) shows a highly significant association between treatment groups (control and study) and TMD and non-TMD. However, 75.3% (64 out of 85) of the study groups had TMD, when only 38.4% of the control group had TMD (28 out of 73), which means that TMD is significantly higher within the study group (73.5%) than the control group (38.4%). On the other hand, the non-TMD was significantly higher (P = 0.0001) within the control group (61.6%) compared to the study group (24.7%) [Table 2].
THE GRADED CHRONIC PAIN SCALE AND THE CHARACTERISTIC PAIN INTENSITY
However, 92 included samples reported signs and symptoms of TMD according to the Graded Chronic Pain Scale. 32.6% (22.6% of the study group and 10% of the control group) of them showed very high scores (characteristic pain intensity [CPI] >50) and were considered as Grade III of the CPG, which means that most of them live with moderate limitations. 36.95% (30.43% of the study group and 6.52% of the control group) had CPI scores that ranged between 21 and 50 and were to have high-intensity pain without disability (Grade II of CPG). 30.43 % (16.29 percent of the study group And 14.14 percent of the control group) scored between 1 and 20 points of CPI and were considered to have low-intensity pain without disability (Grade I of CPG) [Table 4a]. On the other hand, the data underwent one-way MANOVA using the IBM SPSS Software version 22.0 with the dependent variable (CPG) and the independent variables (PTSD intensity and miscarriage). According to the multivariate test results, as shown in Table 4b, there was a statistically significant difference in the levels of the CPG (subgroup) on a linear combination the dependent variable (PTSD intensity, miscarriage or multiple miscarriages, employment status, marital status, forced to move house, and educational levels) (F = 25.5, P = 0.000, which is mean P < 0.0005; Wilk’s value = 0.076, partial eta squared = 0.577). We can see from Table 4c that CPG has a statistically significant effect on PTSD (F = 153.575; P < 0.0001; partial eta squared = 0.749), females who experienced spontaneous miscarriage (F = 10.651; P < 0.0001; partial eta squared = 0.172), multiple miscarriages (F = 25.394; P < 0.0001; partial eta squared = 0.331), employment status (F = 58.178; P < 0.0001; partial eta squared = 0.531), marital status (F = 6.455; P < 0.0001; partial eta squared = 0.112), and women who were forced to move house (F = 73.238; P < 0.0001; partial eta squared = 0.588). However, there is no statistically significant effect of CPG on the educational level of the participants (F = 1.306; P = 275; partial eta squared = 0.025). In addition, the mean scores of PTSD intensity displayed in Table 5 show a statistically significant difference between CPG 0 and CPG I (P < 0.0001), CPG 0 and CPG II (P < 0.0001), CPG 0 and CPG III/IV (P < 0.0001), and CPG I and CPG III/IV (P < 0.0001) but no statistically significant difference between CPG I and CPG II (P = 0.176) and between CPG II and CPG III/IV (P = 0.146). A statistically significant difference in mean miscarriage had been noticed between CPG 0 and CPG II (P < 0.0001) and CPG 0 and CPG III/IV (P = 0.003) but not between CPG 0 and CPG I (P = 0.225), CPG I and CPG II (P = 0.115), CPG I and CPG III/IV (P = 0.605), and CPG II and CPG III/IV (P = 0.765). These differences can be easily estimated by the plots in Figure 1a and b.[18] A statistically significant difference exists in mean multiple miscarriages and between CPG 0 and CPG I (P < 0.0001), CPG 0 and CPG II (P < 0.0001), and CPG 0 and CPG III/IV (P < 0.0001). Furthermore, there is a statistically significant difference in the mean employment status and between CPG 0 and CPG I (P < 0.0001), CPG 0 and CPG II (P < 0.0001), and CPG 0 and CPG III/IV (P < 0.0001). Regarding marital status, a statistically significant difference was noticed in the mean and between CPG 0 and CPG I (P = 0.010) and CPG II and CPG I (P < 0.002). Women who were forced to move house showed a statistically significant difference in the mean and between CPG 0 and CPG I (P < 0.0001), CPG 0 and CPG II (P < 0.0001), CPG 0 and CPG III/IV (P < 0.0001), and CPG II and CPG III/IV (<0.0001). A statistically significant difference was noticed as well in the mean educational level and between CPG 0 and CPG II (P = 0.042), CPG I and CPG II (P = 0.014), and CPG II and CPG III/IV (P < 0.0001).
Table 4a.
Descriptive statistics
| CPGa | Mean | SD | n |
|---|---|---|---|
| PTSDb | |||
| No disabilities | 0.00 | 0.000 | 66 |
| Grade I no disabilities | 1.79 | 0.418 | 28 |
| Grade II moderate limitation | 1.53 | 0.507 | 34 |
| Grade III and IV severe limitation | 1.27 | 0.785 | 30 |
| Total | 0.89 | 0.889 | 158 |
| Miscarriagec | |||
| No disabilities | 0.32 | 0.469 | 66 |
| Grade I no disabilities | 0.54 | 0.508 | 28 |
| Grade II moderate limitation | 0.82 | 0.387 | 34 |
| Grade III and IV severe limitation | 0.70 | 0.466 | 30 |
| Total | 0.54 | 0.500 | 158 |
aCPG of TMD symptomatology scoring system of RDC⁄TMD,[18] bPTSD intensity scoring system, the sample categorized into three subgroups according to their IES-R scores,[16] cStudy group and control group. RDC⁄TMD=Research Diagnostic Criteria for Temporomandibular Disorders, PTSD=Posttraumatic stress disorder, SD=Standard deviation, CPG=Chronic pain grade, IES-R=Impact of Events Scale-Revised, TMD=Temporomandibular joint disorder
Table 4b.
Multivariate testa
| Effect | Value | F | Hypothesis df | Error df | P | Partial η2 |
|---|---|---|---|---|---|---|
| CPG | ||||||
| Wilk’s lambda | 0.076 | 25.500 | 224.000 | 426.946 | 0.000 | 0.577 |
F tests the multivariate effect of CPG. This test is based on the linearly independent pairwise comparison among the estimated marginal mean because Wilk’s lambda is significant, so we have significant differences between the groups, aDesign: CPG of TMD symptomatology scoring system of the RDC⁄TMD.[18] RDC=Research Diagnostic Criteria for Temporomandibular Disorders, CPG=Chronic pain grade, TMD=Temporomandibular joint disorder
Table 5.
Multiple comparisons**
| Dependent variables | CPGa (I) | CPG (J) | Mean difference (I-J) | SE | Pb | 95% CI for differenceb | |
|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||||
| PTSD intensityb | No disabilities | Grade I (no disabilities) | -1.79-* | 0.101 | 0.000 | -2.07- | -1.50- |
| Grade II moderate limitation | -1.53-* | 0.095 | 0.000 | -1.80- | -1.26- | ||
| Grade III and IV severe limitation | -1.27-* | 0.099 | 0.000 | -1.55- | -0.99- | ||
| Grade I (no disabilities) | Grade III and IV severe limitation | 0.52* | 0.118 | 0.000 | 0.19 | 0.85 | |
| Spontaneous miscarriagec | No disabilities | Grade II moderate limitation | -0.51-* | 0.097 | 0.000 | -0.78- | -0.23- |
| Grade III and IV severe limitation | -0.38-* | 0.101 | 0.003 | -0.67- | -0.10- | ||
| Multiple niscarriages | No disabilities | Grade I (no disabilities) | -0.61-* | 0.086 | 0.000 | -0.85- | -0.36- |
| Grade II moderate limitation | -0.53-* | 0.081 | 0.000 | -0.76- | -0.30- | ||
| Grade III and IV severe limitation | -0.47-* | 0.084 | 0.000 | -0.71- | -0.23- | ||
| Employment status | No disabilities | Grade I (no disabilities) | 0.68* | 0.071 | 0.000 | 0.48 | 0.88 |
| Grade II moderate limitation | 0.68* | 0.067 | 0.000 | 0.49 | 0.87 | ||
| Grade III and IV severe limitation | 0.65* | 0.069 | 0.000 | 0.45 | 0.84 | ||
| Marital status | No disabilities | Grade I (no disabilities) | 0.35* | 0.103 | 0.010 | 0.06 | 0.65 |
| Grade II | Grade I (no disabilities) | -0.47-* | 0.117 | 0.002 | -0.80- | -0.14- | |
| Forced to move house | No disabilities | Grade I (no disabilities) | -0.86-* | 0.072 | 0.000 | -1.06- | -0.65- |
| Grade II moderate limitation | -0.82-* | 0.068 | 0.000 | -1.01- | -0.63- | ||
| Grade III and IV severe limitation | -0.47-* | 0.71 | 0.000 | -6.7- | -0.27- | ||
| Grade II | Grade III and IV severe limitation | 0.36 | 0.080 | 0.000 | 0.13 | 0.58 | |
| Educational level | No disabilities | Grade II moderate limitation | -0.27-* | 0.093 | 0.042 | -0.53- | -0.01- |
| Grade I (no disabilities) | Grade II moderate limitation | -0.37-* | 0.113 | 0.014 | -0.69- | -0.06- | |
| Grade II | Grade III and IV severe limitation | 0.49* | 0.110 | 0.000 | 0.18 | 0.80 | |
**Based on observed means, Scheffe HSD post hoc test. The error term is mean square (error)=0.202, *The mean difference is significant at the 0.05 level. aCPG of TMD symptomatology scoring system of RDC/TMD,[18] bPTSD intensity scoring system[16], cStudy group and control group, only statistically significant data are reported. RDC/TMD=Research Diagnostic Criteria for Temporomandibular Disorders, CPG=Chronic pain grade, TMD=Temporomandibular joint disorder, HSD=Honestly significant difference
Figure 1.
Based on observed means of multiple comparisons, the error term is mean square (error) =0.211, the mean difference is significant at the. 05 level, chronic pain grade of temporomandibular disorder symptomatology scoring system of the Research Diagnostic Criteria For Temporomandibular Disorders; posttraumatic stress disorder intensity in (a) and experiencing spontaneous miscarriage at first trimester in (b)
DISCUSSION
This study provides useful information about spontaneous miscarriage and its consequences, especially for Saudi women’s lifestyle and oral health. Furthermore, we establish the possibility of a large-scale study regarding the mental injury related to recurrent spontaneous pregnancy loss in our research. The 208 Saudi women were mostly pleased to be contacted and join in. Almost all women who participated completed all questions, except for 50 women whose data were not included in our sample because they did not fulfill the inclusion criteria completely. The dropout participants did not affect our sample to produce a large effect as it was calculated by the G-power software. However, about dropouts, while it is likely that the Saudi women with a more noteworthy passionate response to spontaneous pregnancy loss were more probable to answer, it is likewise possible that Saudi females with excessive trauma would avoid going through steps that might force them to relive the trauma. This might constitute a hypothesis of the probability of an unintentional, constraining remedial effect from participating in the study as Neugebauer et al. revealed in their study.[19]
Considering that EPLs are traumatic events because they involve many traumatizing aspects, especially when coupled with complications dangerous enough to threaten a human life such as uncontrollable hemorrhage, women with EPLs are significantly recognized to be more prone to develop symptoms of PTSD.[10,20,21]
Our study revealed an astonishing pervasiveness of PTSD symptoms among the selected sample. Significant symptom clusters advocated inclusion into the sample women who did not show the whole benchmark for PTSD, in addition to the deterioration among public and job-related territories. The prevalence of probable PTSD is higher than the earlier declared results by Farren et al. and Engelhard et al. Appropriately, the established diagnosis of PTSD may have confirmed the symptom clusters among the selected sample. Acute stress disorder may be manipulated at an early level for 1 month at least.[10,11,21]
In our study, the selected Saudi women were not limited to a certain early stage of pregnancy loss because of the lack of the specific sample, which is similar to another study by Engelhard et al. The candidates were women with or without miscarriage. In our community, some of the females preferred to stay at home and not visit the gynecologist after experiencing a spontaneous miscarriage. This may be due to a low level of education, inherited traditions, or lack of awareness regarding the side effects of EPL. Especially for the noneducated females and women who are at risk for having a miscarriage, we recommend focusing on the emotional negativity, and more attention should be given to the need for psychological awareness among our society.[11]
According to Giraki et al., stress-coping behaviors are significantly correlated with TMD symptoms. Although psychological and emotional factors are the most important factors of TMD, as revealed by Staniszewski et al. in their research, Bertoli et al. declared in their studies that PTSD symptoms were more frequent among patients who had orofacial pain. These results coincide with our findings: 58.2% of the women in our study reported myofascial pain. A strong relationship between PTSD signs and TMJ pain had been found by Oliveira et al. and Ahmad Mottaghi and Zamani. These findings are in line with our study as the prevalence of TMD was 53.8% among the selected sample (the study group and the control group). A longitudinal study would have been conducted to identify the long-term consequences of EPL on TMJ.[1,9,22,23,24]
Conclusively, we accept that this research depends on the usage of self-report questionnaires, as well as a quick examination of the TMJ and recording the obvious symptoms of TMD, while an established diagnosis of PTSD necessitates broader interviews with appropriately qualified people, and TMD requires an MRI and a CT scan to establish a definitive diagnosis and suitable treatment.[9,18]
The treatment approach for PTSD is limited and dependent on trauma-focused cognitive-behavioral therapy or reprocessing and desensitization of eye movement. Women who suffer from EPL are advised to seek a psychological screening for mental disorders because of harmful PTSD symptoms.[25,26]
LIMITATIONS
The sample was taken from only two areas of Saudi Arabia. Furthermore, the sample selection was conveniently made due to lack of cooperation from the gynecology clinics. However, inherited traditions might be a reason for some of the women who refused to participate in the research.
CONCLUSION
There is a statistically proven relation between miscarriage and TMD. Therefore, it is recommended that a gynecologist refers the patient to a dentist for early screening and prevention of TMD.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- 1.Mottaghi A, Zamani E. Temporomandibular joint health status in war veterans with post-traumatic stress disorder. J Educ Health Promot. 2014;3:60. doi: 10.4103/2277-9531.134765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taylor S, Kuch K, Koch WJ, Crockett DJ, Passey G. The structure of posttraumatic stress symptoms. J Abnorm Psychol. 1998;107:154–60. doi: 10.1037//0021-843x.107.1.154. [DOI] [PubMed] [Google Scholar]
- 3.Barros Vde M, Seraidarian PI, Côrtes MI, de Paula LV. The impact of orofacial pain on the quality of life of patients with temporomandibular disorder. J Orofac Pain. 2009;23:28–37. [PubMed] [Google Scholar]
- 4.de Oliveira Solis AC, Araújo ÁC, Corchs F, Bernik M, Duran ÉP, Silva C, et al. Impact of post-traumatic stress disorder on oral health. J Affect Disord. 2017;219:126–32. doi: 10.1016/j.jad.2017.05.033. [DOI] [PubMed] [Google Scholar]
- 5.Azuma K, Adachi Y, Hayashi H, Kubo KY. Chronic psychological stress as a risk factor of osteoporosis. J UOEH. 2015;37:245–53. doi: 10.7888/juoeh.37.245. [DOI] [PubMed] [Google Scholar]
- 6.Jung HD, Kim SY, Park HS, Jung YS. Orthognathic surgery and temporomandibular joint symptoms. Maxillofac Plast Reconstr Surg. 2015;37:14. doi: 10.1186/s40902-015-0014-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kubo KY, Iinuma M, Chen H. Mastication as a stress-coping behavior. Biomed Res Int 2015. 2015:876409. doi: 10.1155/2015/876409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bottiroli S, Galli F, Viana M, Sances G, Tassorelli C. Traumatic experiences, stressful events, and alexithymia in chronic migraine with medication overuse. Front Psychol. 2018;9:704. doi: 10.3389/fpsyg.2018.00704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bertoli E, de Leeuw R, Schmidt JE, Okeson JP, Carlson CR. Prevalence and impact of post-traumatic stress disorder symptoms in patients with masticatory muscle or temporomandibular joint pain: Differences and similarities. J Orofac Pain. 2007;21:107–19. [PubMed] [Google Scholar]
- 10.Farren J, Jalmbrant M, Ameye L, Joash K, Mitchell-Jones N, Tapp S, et al. Post-traumatic stress, anxiety and depression following miscarriage or ectopic pregnancy: A prospective cohort study. BMJ Open. 2016;6:e011864. doi: 10.1136/bmjopen-2016-011864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Engelhard IM, van den Hout MA, Arntz A. Posttraumatic stress disorder after pregnancy loss. Gen Hosp Psychiatry. 2001;23:62–6. doi: 10.1016/s0163-8343(01)00124-4. [DOI] [PubMed] [Google Scholar]
- 12.Reardon DC. The abortion and mental health controversy: A comprehensive literature review of common ground agreements, disagreements, actionable recommendations, and research opportunities. SAGE Open Med. 2018;6:2050312118807624. doi: 10.1177/2050312118807624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giannandrea SA, Cerulli C, Anson E, Chaudron LH. Increased risk for postpartum psychiatric disorders among women with past pregnancy loss. J Womens Health (Larchmt) 2013;22:760–8. doi: 10.1089/jwh.2012.4011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kindler S, Schwahn C, Bernhardt O, Söhnel A, Mksoud M, Biffar R, et al. Association between symptoms of posttraumatic stress disorder and signs of temporomandibular disorders in the general population. J Oral Facial Pain Headache. 2018;10:11607. doi: 10.11607/ofph.1905. [DOI] [PubMed] [Google Scholar]
- 15.Malinauskienė V, Bernotaitė L. The impact of event scale – Revised: Psychometric properties of the Lithuanian version in a sample of employees exposed to workplace bullying. Acta Med Litu. 2016;23:185–92. doi: 10.6001/actamedica.v23i3.3384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arnetz BB, Broadbridge CL, Jamil H, Lumley MA, Pole N, Barkho E, et al. Specific trauma subtypes improve the predictive validity of the Harvard trauma questionnaire in Iraqi refugees. J Immigr Minor Health. 2014;16:1055–61. doi: 10.1007/s10903-014-9995-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weiss DS. The impact of event scale: Revised. In: Wilson JP, Tang CS, editors. Cross-Cultural Assessment of Psychological Trauma and PTSD. New York: Springer; 2007. pp. 219–38. [Google Scholar]
- 18.Look JO, Schiffman EL, Truelove EL, Ahmad M. Reliability and validity of axis I of the research diagnostic criteria for temporomandibular disorders (RDC/TMD) with proposed revisions. J Oral Rehabil. 2010;37:744–59. doi: 10.1111/j.1365-2842.2010.02121.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Neugebauer R, Fisher PW, Turner JB, Yamabe S, Sarsfield JA, Stehling-Ariza T. Post-traumatic stress reactions among Rwandan children and adolescents in the early aftermath of genocide. Int J Epidemiol. 2009;38:1033–45. doi: 10.1093/ije/dyn375. [DOI] [PubMed] [Google Scholar]
- 20.Daugirdaitė V, van den Akker O, Purewal S. Posttraumatic stress and posttraumatic stress disorder after termination of pregnancy and reproductive loss: A systematic review. J Pregnancy 2015. 2015:646345. doi: 10.1155/2015/646345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kessler RC. Posttraumatic stress disorder: The burden to the individual and to society. J Clin Psychiatry. 2000;61(Suppl 5):4–12. [PubMed] [Google Scholar]
- 22.Staniszewski K, Lygre H, Bifulco E, Kvinnsland S, Willassen L, Helgeland E, et al. Temporomandibular disorders related to stress and HPA-axis regulation. Pain Res Manag. 2018;2018:7020751. doi: 10.1155/2018/7020751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Giraki M, Schneider C, Schäfer R, Singh P, Franz M, Raab WH, et al. Correlation between stress, stress-coping and current sleep bruxism. Head Face Med. 2010;6:2. doi: 10.1186/1746-160X-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oliveira FD, de Oliveira VC, Rodrigues CP. Post-traumatic stress disorder and temporomandibular dysfunction: A review and clinical implications. BRJP. 2018;1:55–9. [Google Scholar]
- 25.Furuta M, Horsch A, Ng ES, Bick D, Spain D, Sin J, et al. Effectiveness of trauma-focused psychological therapies for treating post-traumatic stress disorder symptoms in women following childbirth: A systematic review and meta-analysis. Front Psychiatry. 2018;9:591. doi: 10.3389/fpsyt.2018.00591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Horesh D, Nukrian M, Bialik Y. To lose an unborn child: Post-traumatic stress disorder and major depressive disorder following pregnancy loss among Israeli women. Gen Hosp Psychiatry. 2018;53:95–100. doi: 10.1016/j.genhosppsych.2018.02.003. [DOI] [PubMed] [Google Scholar]