Abstract
Introduction:
Oral health is a complex interaction that contains factors such as disease status and physiological and psychosocial properties. Because of complexity of the health system, policymakers should find some ways to simplify the relations to increase the chance of understanding the conditions, values, and ideas behind it. Policy learning could be built on the appropriate policy models application corn stone. The aim of this study was to answer this question that what policy models were applied in oral health policy studies and what oral health policy issues were analyzed by policy models.
Materials and Methods:
A systematic review was conducted across international electronic databases (PubMed, ISI Web of Knowledge, and Scopus) with no time limitation and using prearranged keywords. All publications such as articles and thesis were included. Searched terms were selected based on frequent health policy model components and an initial search. Search strategy based on each data base instruction was applied.
Results:
Eight models or frameworks were applied in total. Most of these models were focused on process stage of oral health policy making. Five main themes such as the role of stakeholders in oral health policy making, assessment of oral health system, oral health policy development, the process of oral health policy making, and oral health policy learning and capacity building were synthesized.
Conclusion:
Oral health policy issues could be analyzed more comprehensively, and researchers could be guided by applying policy models and frameworks to answer policy-learning questions. Application of models and frameworks should be based on the nature of problem and issue, and the level of problem screening is a critical point in applying appropriate model.
KEYWORDS: Dentistry, oral health, policy analysis, policy model, policy process
INTRODUCTION
Oral health is recognized by the latest definition as one of the most important factors in public health.[1] From a comprehensive point of view, oral health is a complex interaction that contains factors such as disease status and physiological and psychosocial factors as the core elements of oral health, which together with a range of driving and moderating factors lead to overall health and well-being.[2]
Many people in the world are having oral and dental diseases, and dental treatments cost a lot to patients. Direct and indirect costs of dental disease amounted to US$356.80 billion and US$187.61 billion, respectively, and dental disease costs a total of US$544.41 billion in the world in 2015.[3]
For the aforementioned reasons, the improvement of oral health in the public could be very beneficial and useful, which could lead to social well-being improvement. Oral health could be promoted through appropriate policy making, and “policy analysis” can play a key role in this area.[4,5]
The analysis of health policy aims to understand the relationships between actors, processes, policy content, and the conditions underlying the implementation of health policy.[6] A comprehensive analysis of health policy is a prelude to major changes and developments in health policy, and it is therefore important to understand the relationships between actors in the political environment.[4]
Owing to the complexity of the health system, policymakers, health managers, and policy analysts should find some ways to simplify the relations to increase the chance of understanding the conditions, values, and ideas behind it. This usually involves compiling a theoretical framework or model that determines which factors are important and which relationships can be ignored. Utilizing concepts, approaches, and policy analysis patterns is useful in understanding the policies.[5,6,7,8]
Utilizing the theoretical models and frameworks of policy analysis provides a platform for discussion in order to provide individuals with the important topics of their frameworks, evaluate empirical evidence, and propose research guidelines.[5] Policy models also provide a practical manner of describing, explaining, understanding and planning future policy activities, and more extensive policy learning in one word.[9]
A key subject of public policy analysis is learning and its connection with convictions, policy development, and change.[10] So, policy learning could be achieved by applying appropriate policy models and then, policy-learning questions could be answered.[10]
The aim of this study was to answer this question that what policy models were applied in oral health policy studies, what oral health policy issues were analyzed by policy models, and what policy-learning questions were answered by application of these models. In other words, this study tried to provide a comprehensive overview of studies that applied health policy models/frameworks in analyzing oral health policy issues or to suggest a conceptual model in this area.
MATERIALS AND METHODS
SEARCH STRATEGY AND DATA SOURCES
To make a comprehensive search, the systematic review question was developed based on the modified form of PICO (population, intervention, compromised, output), which was used in qualitative systematic reviews. This modified form addressed population, context, and outcome (PCO) in qualitative studies.[11] The components of PCO in our review are shown in Table 1. In our study, different types of oral health issues were considered as population that in context of policy making stages were analyzed by models and led to policy learning. So the systematic review question was: “What policy models were applied in different oral health policy making stages to answer the policy-learning questions?” Searches were conducted across three international electronic databases (PubMed, ISI Web of Knowledge, and Scopus) with no time limitation and using prearranged keywords. All publications, such as articles, thesis, and reference articles, were included. Searched terms were selected based on PCO framework and an initial search [Table 2]. Different search strings have been created and tested. Search strategy based on each data base instruction was applied. The time of the last search was May 4, 2019. Keywords are shown in Table 2. This systematic review was submitted in International Prospective Register of Systematic Reviews (PROSPERO) with the ID code: 140274.
Table 1.
Components of population, context, and outcome in systematic review question
| Population | Oral health issues |
|---|---|
| Context | Policy making stages, policy models |
| Outcome | Policy learning |
Table 2.
Keywords and search strategy
| # | Keywords | * | Search strategy | |
|---|---|---|---|---|
| 1 | Model | 21 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR # 16 OR #17 OR #18 |
#21 AND #22 |
| 2 | Frame | |||
| 3 | Framework | |||
| 4 | Content | |||
| 5 | Context | |||
| 6 | Process | |||
| 7 | Formulation | |||
| 8 | Kingdon | |||
| 9 | Stage heuristic | |||
| 10 | Advocacy coalition | |||
| 11 | Triangle | |||
| 12 | Analysis | |||
| 13 | Evaluation | |||
| 14 | Assessment | |||
| 15 | Actors | |||
| 16 | Political priority | |||
| 17 | Shiffman and Smith | |||
| 18 | Power | |||
| 19 | Oral health | 22 | #19AND #20 | |
| 20 | Policy making | |||
STUDY SELECTION
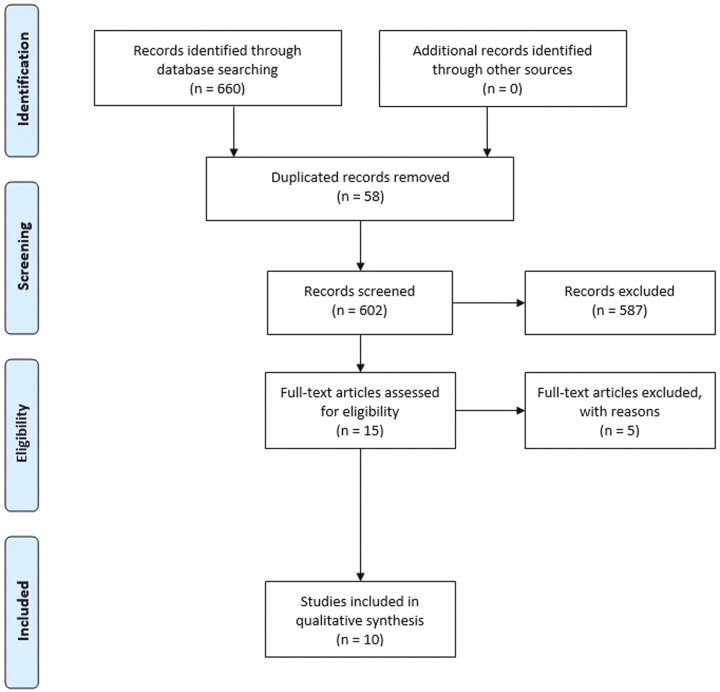
In this review, publications in electronic databases and libraries were reviewed. Furthermore, relevant scientific journals were explored. The including criterion in our systematic review was as follows: including all the publications, which have been conducted on oral health policy issues using policy models and which answered the policy-learning questions. The exclusion criteria were as follows: publications in which original papers have not been published in English language and publications not available in electronic full texts. To find more published articles, some journals were used after searching databases. The research protocol that is shown in Figure 1, was based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Guidelines[12] in line with excellent practice for systematic reviews.
Figure 1.
Review stages based on PRISMA flow diagram
Quality assessment and data synthesis
Full-text papers were obtained and evaluated for the quality of studies, which met the requirements for inclusion. Methodological quality was evaluated by using the critical appraisal skills program critical assessment of qualitative research tool.[13] High-quality papers scored 9–10, moderate-quality papers scored 7.5–9, low-quality papers scored 6–7.5, and papers less than score 6 were excluded. To assess the quality, two researchers evaluated the quality of the research and a third researcher was consulted in case of doubt.
In qualitative systematic reviews, various techniques of information synthesis are used.[14] In this study, after categorizing main themes of applied policy models, oral health issues, and policy stages, a code tree was drafted. Research team discussed about codes and categorized them into themes.
RESULTS
In the primary search, 660 publications were obtained from three valid databases (65 from PubMed, 225 from Web of Knowledge, and 370 from Scopus). After identifying duplicated ones by EndNote X7 software, the number of publications was reduced to 602. After that, titles and abstracts were investigated based on study subjects, and 525 articles were excluded. These publications were investigated by full text and finally 10 studies obtained the required credits to include in the review.
A total of 10 studies were finally included in our review [Table 3]. Of them, three were conducted in Nigeria and the other nine were conducted in the United States, Canada, England, India, Italy, and Australia. The latest and the oldest studies were published in 2018 and 2010, respectively. Moreover, nine of these studies were qualitative and one was mixed method. No systematic review was present in the included studies. The general characteristics of included studies are shown in Table 3.
Table 3.
Quality assessment results and general characteristics of the included studies
| No. | Title | First author | Year | Methodology | Country | Score |
|---|---|---|---|---|---|---|
| 1 | Political priority of oral health in India: analysis of the reasons for neglect[15] | Janakiram | 2018 | Qualitative document review | India | 7 |
| 2 | Can conditional health policies be justified? A policy analysis of the new NHS dental contract reforms[16] | Laverty | 2018 | Qualitative document review | England | 7.5 |
| 3 | The rise and fall of dental therapy in Canada: a policy analysis and assessment of equity of access to oral health care for Inuit and First Nations communities[17] | Leck | 2017 | Qualitative document review | Canada | 8.5 |
| 4 | Role and use of evidence in policymaking: an analysis of case studies from the health sector in Nigeria[18] | Onwujekwe | 2015 | Qualitative document review | Nigeria | 7 |
| In-depth interview | ||||||
| 5 | Development of oral health policy in Nigeria: an analysis of the role of context, actors and policy process[19] | Etiaba | 2015 | Qualitative document review | Nigeria | 9 |
| In-depth interview | ||||||
| 6 | Political priority of oral health in Italy: an analysis of reasons for national neglect[20] | Benedetti | 2015 | Qualitative document review | Italy | 8.5 |
| 7 | The origins of Minnesota’s mid-level dental practitioner: alignment of problem, political and policy streams[21] | Gwozdek | 2014 | Qualitative document review | USA | 7.5 |
| 8 | An appraisal of the oral health-care system in Nigeria[22] | Adeniyi | 2012 | Qualitative document review | Nigeria | 8 |
| 9 | Influencing public policy on oral health[23] | Lewis | 2012 | Qualitative in-depth interview | Australia | 7.5 |
| 10 | Policy analysis of oral health promotion in South Africa[24] | Singh | 2010 | Mixed method | South Africa | 6.5 |
| Literature review | ||||||
| Document review | ||||||
| In-depth interview |
In our review, nine studies used available models and one study proposed a new conceptual framework in oral health policy analysis. Eight models or frameworks were applied totally. Models or frameworks were used in these studies, they clarified events around oral health policy cycle. Most of these models were focused on process stage of oral health policy making that included problem identification, agenda setting, formulation, implementation, and evaluation. Furthermore, in process stage, agenda setting was analyzed by various models such as triple streams model and social network model.
Table 4 showed the prevalence of issues, policy making stages, and models applied in the reviewed articles. On the basis of results, oral health policy development was the most frequent issue that was analyzed by policy models. Multiple-streams model and political power framework also was the most frequent model that was applied in the studies. Moreover, agenda setting was the most notable stage of oral health policy making that was studied by the researchers.
Table 4.
Prevalence of issues, models, and policy making stage were applied in reviewed studies
| Oral health policy issue | Frequency | Model/framework | Frequency | Policy making stage | Frequency |
|---|---|---|---|---|---|
| Mid-level dental practitioner | 2 (20%) | Multiple-streams model | 2 (20%) | Agenda setting | 6 (60%) |
| Political power in oral health | 2 (20%) | Political power framework | 2 (20%) | Evaluation | 2 (20%) |
| Oral health policy development | 3 (30%) | Triangle model | 1 (10%) | Formulation | 1 (10%) |
| Oral health priority in agenda | 1 (10%) | Advocacy Coalition Framework | 1 (10%) | Holistic view (content, context, process) | 1 (10%) |
| Dental contract reforms | 1 (10%) | Evidence-based policy analysis model | 1 (10%) | ||
| Oral health-care system | 1 (10%) | Political discourse analysis model | 1 (10%) | ||
| Maxwell model and Beazoglou model | 1 (10%) | ||||
| Social network model | 1 (10%) | ||||
One of the objectives of this study was to clarify what policy learnings were achieved by using the models. To show this, the main questions that were answered in these studies were reflected. In the reviewed articles, various policy-learning questions were answered by using policy models that most of them were the questions of why and how. The special characteristics of applied models and the specific questions of the studies are shown in Table 5.
Table 5.
Special characteristics of applied models and the policy learning questions
| Article number | Applied model | Model provider | Main themes of model | The focus of model based on health policy cycle | Oral health policy issue | Policy-learning questions |
|---|---|---|---|---|---|---|
| 3, 7 | Multiple-streams model | John W. Kingdon | Policy stream | Process(agenda setting) | Mid-level dental practitioner | How “access need” becomes a part of political agenda? And what was the main and determinant interest groups? And what was the leading factors that induce achievement in legislation process in Minnesota? |
| Problem stream | ||||||
| Politic stream | ||||||
| Why dental therapy in Canada was proposed and implemented as a policy to reduce inequity in access to oral health services and why this policy has now been abandoned? | ||||||
| 1, 6 | Political power framework | Shiffman and Smith | Power of ideas | Process(agenda setting) | Political power of oral health | What factors (ideas, issue characteristics, actor, and context) are shaping the political power of oral health in Italy and India? |
| Power of issue | ||||||
| Power of actors | ||||||
| Power of political context | ||||||
| 5 | Triangle model | Walt and Gilson | Content | Holistic view of policy influential factors | National oral health policy development | How context, content, process, and actors affected oral health policy development in Nigeria? |
| Context | ||||||
| Process | ||||||
| Actors | ||||||
| 4 | Evidence usage in policymaking model | Proposed by author | Policy | Formulation | National oral health policy development | What is the role of evidence in policy development? And what are the interactions between evidence, policy actors, policy, and evidence use? How interactions of evidence outputs and policy process such as problem identification, formulation, and implementation are determined by policy actors? |
| Evidence | ||||||
| Actors | ||||||
| Evidence use | ||||||
| 10 | Advocacy Coalition Framework | Sabatier and Jenkins | Stable parameters | Agenda setting | Oral health promotion development | How oral health issue had been placed on policy agenda through coordination and collaboration between different role players? And what are indicated contradictions of all examined areas in oral health promotion-related policy and decision-making? And what is the most influential elements in oral health promotion in South Africa? |
| Policy subsystem | ||||||
| Potential external threats | ||||||
| 2 | Political discourse analysis model | Fairclough | Identified problem | Evaluation | Dental contract reforms in UK | How policy arguments comprise an identified problem or claim for actions, the specific means and desired goals proposed to achieve a proposed action, and contextualizing circumstances and values? |
| Specific means | ||||||
| Desired goals | ||||||
| Circumstances | ||||||
| Values | ||||||
| How arguments in the related policy documents frame and justify conditionality? How language and discourses influence in which policy formation gets enacted and how policies are interpreted by the public and policymakers? | ||||||
| 8 | Two models: | (1) Beazoglou | Structure (education and training) | Evaluation | Oral health-care system in Nigeria | What is the situation of oral health-care system in Nigeria in respect to critical appraisal? And what are the strengths and weaknesses, opportunities, and threats affecting the achievement of good oral health in Nigerians? |
| Structure measurement model | (2) Maxwell | Process (services and access) | ||||
| Quality assessment model | Outcome (oral health status) | |||||
| Efficiency effectiveness accessibility | ||||||
| Equity | ||||||
| Social acceptability | ||||||
| Relevance to need | ||||||
| 9 | Social network model | Wasserman and Faust | Social actors (such as individuals or organizations) and their relations | Predecision stage of policy making | Oral health priority in agenda | What is the position of oral health on the broader health policy agenda? |
| What is the network of interests, actors and interpersonal connections? And who is regarded as influential by others in the same policy sector that exercises control within the network? |
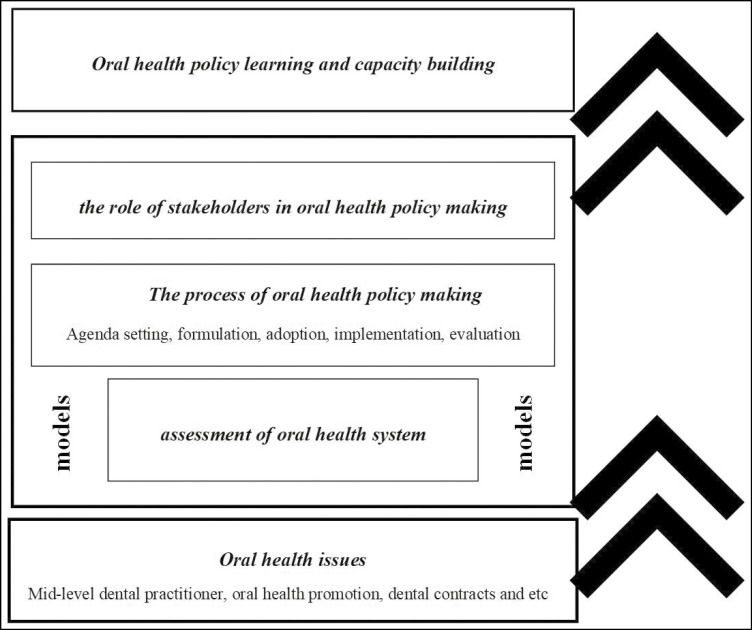
Overall findings from the data synthesis: Five main themes were identified in the qualitative analysis on the application of health policy analysis in oral health. The themes were as follows:
The role of stakeholders in oral health policy making
Assessment of oral health system
Oral health policy development
The process of oral health policy making
Oral health policy learning and capacity building
The themes are presented in Figure 2.
Figure 2.
Thematic schema: oral health issues are analyzed by policy models in different process stages and the results lead to policy learning and oral health policy capacity building
THEME ONE: THE ROLE OF STAKEHOLDERS IN ORAL HEALTH POLICY MAKING
In many studies, actors and stakeholders had a crucial role in directing policy making.[15,17,18,19,20,21,23] So, stakeholders should be identified and analyzed based on their power and interest. According to the results, stakeholders are important in the use of evidence, setting the agenda, emphasizing the importance of oral health, and mobilizing resources and activities.
The power of actors also is one of the components of political power framework that could influence on political stream. Furthermore, actors are placed on the center of oral health policy making. So identifying oral health stakeholders and analyzing them would lead to identify engagement strategies.
In some studies, political power was highlighted as one of the most important factors in neglecting oral health as a national priority,[15,20] which reflected the role of stakeholders and players. Though, the stakeholder power and interest is so important but it should be mentioned that the power of ideas, issues, and political context would be considered.
In another study, identification of stakeholders networkwas highlighted because they can access external resources through their links with other actors.[23] Mapping interpersonal social networks generates an image of people-to-people connections, showing who exercises power within the network.
THEME TWO: ASSESSMENT OF ORAL HEALTH SYSTEM
In many studies, oral health assessment was taken into account by modeling analysis.[16,22] The assessment of oral health system is a neglected area and assessing the system and its performance could improve dentistry and oral health functions and outputs.
Applying models in assessment of oral health system could guide the researcher to highlight the main factors such as quality, structure, efficiency, and public oral health as the main output.
THEME THREE: ORAL HEALTH POLICY DEVELOPMENT
In our review, six main issues were addressed, of which oral health policy development was the most frequent issue. Oral health policy development is also the center of many studies, and models were applied to clarify the challenges and highlight the main influential factors in oral health policy development.
THEME FOUR: THE PROCESS OF ORAL HEALTH POLICY MAKING
The process of oral health policy making was pointed in all of the studies. In oral health policy process, five stages such as agenda setting, policy formulation, adoption (or decision-making), implementation, and evaluation could be named. All models applied in our review were pointed to one or more than one stage of policy process. The oral health policy process is the main stage where all of policy-making efforts are focused in.
THEME FIVE: ORAL HEALTH POLICY LEARNING AND CAPACITY BUILDING
The application of policy models guides researchers to answer more in-depth questions. All of the papers in our review had the how and why questions, of whose the answers would lead to policy learning. By analyzing oral health issues and obtaining results, oral health policy builds capacity-building capabilities that could improve the oral health system over time.
The five main themes are presented in Figure 2 as thematic schema.
DISCUSSION
This study revealed that studying oral health issues is a new topic that is expanding, and oral health issues could be analyzed more in-depth. Different models and frameworks have been applied at different policy levels, and oral health policy issues have been investigated. Oral health policy development was the most frequent issue that was analyzed by policy models. Multiple-streams model also was the most frequent model that was applied in the articles, and agenda setting was the most notable stage of oral health policy making that was studied by researchers. There was no article in implementation stage and context analysis.
In our review, six main issues were addressed, of which oral health policy development was the most frequent issue. It may be because of the need for a comprehensive oral health policy and the emphasis on oral health policy development of international institutions such as the World Health Organization (WHO).[25,26,27,28] Development of oral health policy is a common issue in oral health policy and it may be influenced by different factors. Political power was also addressed in 20% of reviewed articles. It could be because the political support is so important in setting the oral health in agenda.[29] Evidences showed that inequalities in oral health and oral health promotion could occur when it did not find the way on the agenda.[30,31] On the basis of WHO priority action areas, issues such as effective use of fluoride, healthy diet and nutrition, tobacco control, oral health systems, oral health information systems, evidence for oral health policy, and formulation of goals were the most important global oral health issues. But some of these issues such as oral health system and evidence usage were addressed, whereas the rest of global issues were abandoned.
The second frequent issue was the problem of mid-level dental providers. They are non-dentists working outside the direct or indirect supervision of the dentist, diagnosing, and treating the dental patient in some cases. Addressing this issue in our reviewed article could be because this kind of oral health workforces are expanding in the world and are also facing some challenges.[32,33]
In reviewed studies, various models/frameworks have been used and a conceptual framework has been proposed. Each researcher selected a study-based framework or model that shows focus points in analysis. In other words, model/frameworks for policy analysis were used as a theoretical lens to guide and to highlight important components in analysis.
Triangle model by considering three main components, such as content, context, and process, made a comprehensive view of oral health policy development.[19] Recent calls for strengthening the field of health policy analysis in low- and middle-income countries through the use of a wide range of tools in the form of theories, models, and frameworks could be the reason why.[5]
The development of oral health policy has been analyzed from a different perspective in an adapted form of the coalition advocacy framework (ACF).[24] The main components of this framework were “stable parameters” and “potential external threats,” including changes in policy focus, public opinion, and political environment, as a belief in this “oral health promotion” framework. In the adapted form of ACF, “oral health promotion” was considered as “shared beliefs,” whereas in the triangle model and other frameworks reviewed, it was considered to be the interest of stakeholders. Oral health as “shared beliefs” could make coalitions, and these coalitions could remain stable until external threats such as political changes have taken place.[34]
In Kingdon’s model, three streams such as problem, politics, and policy could be discovered. Political power is one of the most important determinant factors in politic stream.[35] Although triple stream only referred to the political dimension, power relations and their specifics have not been mentioned. To fill this gap, specific framework was offered by Shiffman and Smith.[36] This framework made a guidance to assess the power of ideas, the power of actors, and the power of issue, and also the power of political context as the main determinants of political power.
Furthermore, social network model explained who has been seen as influential in health policy, how these people are connected, and what problems are of interest. Though this model is a kind of behavioral sciences,[37] it could highlight prioritizing oral health issue in the background of networks of interests and players.
On the basis of oral health evidence usage framework,[18] actors and players also had a significant role in evidence usage. In this framework, interactions of evidence outputs and policy process, such as problem identification, formulation, and implementation, are determined by policy.
In structure measurement model and quality assessment model, structure (education and training), process (services and access), and outcome (oral health status) were evaluated. Moreover, qualitative indicators such as social acceptance, efficiency, and equity were assessed by Maxwell model. On the basis of evidences, quality is an important part of health policies that could be addressed as a function in health-care system.[38,39]
The content of oral health policy was evaluated based on discourse analysis model[40] to examine how policy arguments represent recognized needs or demands for action, the appropriate means and specific objectives proposed to achieve the proposed action and contextualize situations and values.[16] Discourse analysis is an interdisciplinary approach, applied less by researchers in public health.[41] Though this model is about oral health content evaluation, it seems that social values and desired goals were mentioned in this model that could be categorized in context topic.
On the basis of results of this study, agenda setting was the most notable stage of oral health policy making (60%) that was studied by researchers. It could be because of neglecting oral health priority in the countries[15,20,32,42] The researchers tried to solve the problem at agenda setting step. In reviewed studies, three models were applied in agenda setting stage. Triple stream model, political power framework, and advocacy coalition framework were the applied models.
Formulation and evaluation stages were also addressed. On the basis of policy cycle, implementation and problem identification stage were not addressed in reviewed articles. In implementation stage, some approaches such as top-down or bottom-up could be helpful in analysis.[43]
Oral health policy evaluation stage applies principles and methods of assessment to investigate a policy’s content, execution, or effect. Evaluation is the activity by which we develop an awareness of a policy’s merit, value, and usefulness.[44] Evidences showed the importance of this policy level[15,45,46] that confirmed our results. Though there are many articles focused on evaluation stage, the researches guided by policy models are scarce.
The policy-making process, which is influenced by the step-by-step policy-making approach, shows the policy development and formulation process. The process of policy making is a good way for society to decide on the allocation of resources to solve social issues; such decisions are made by policymakers and what is best for themselves and the community.[47]
CONCLUSION
Because of the importance of oral health promotion and the influence of policy analysis in the improvement of programs and policies, oral health policy issues could be analyzed more comprehensively, and the application of policy models and frameworks could guide researchers. Application of models and frameworks should be based on the nature of problem and issue, and the level of problem screening should be a critical point in applying appropriate model.
FINANCIAL SUPPORT AND SPONSORSHIP
This study was supported by Iran University of Medical Sciences.
CONFLICTS OF INTEREST
There are no conflicts of interest.
ACKNOWLEDGEMENT
This article was a part of the PhD dissertation approved and supported by the School of Health Management and Information Sciences, Iran University of Medical Sciences, with the code of IUMS/SHMIS_1395/9323557002.
REFERENCES
- 1.Satcher D, Nottingham JH. Revisiting oral health in America: A report of the surgeon general. Am J Public Health. 2017;107:32–3. doi: 10.2105/AJPH.2017.303687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee J, Watt R, Williams D, Giannobile W. Los Angeles, CA: SAGE Publications; 2017. A new definition for oral health: Implications for clinical practice, policy, and research. [DOI] [PubMed] [Google Scholar]
- 3.Righolt AJ, Jevdjevic M, Marcenes W, Listl S. Global-, regional-, and country-level economic impacts of dental diseases in 2015. J Dent Res. 2018;98:501–7. doi: 10.1177/0022034517750572. [DOI] [PubMed] [Google Scholar]
- 4.Walt G, Gilson L. Reforming the health sector in developing countries: The central role of policy analysis. Health Policy Plan. 1994;9:353–70. doi: 10.1093/heapol/9.4.353. [DOI] [PubMed] [Google Scholar]
- 5.Walt G, Shiffman J, Schneider H, Murray SF, Brugha R, Gilson L. ‘Doing’ health policy analysis: Methodological and conceptual reflections and challenges. Health Policy Plan. 2008;23:308–17. doi: 10.1093/heapol/czn024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buse K, Mays N, Walt G. Maidenhead, McGraw-Hill Education (UK): 2012. Making Health Policy. [Google Scholar]
- 7.Araújo Jr JLCd, Maciel Filho R. Developing an operational framework for health policy analysis. Revista Brasileira de Saúde Materno Infantil. 2001;1:203–21. [Google Scholar]
- 8.Cheung KK, Mirzaei M, Leeder S. Health policy analysis: A tool to evaluate in policy documents the alignment between policy statements and intended outcomes. Aust Health Rev. 2010;34:405–13. doi: 10.1071/AH09767. [DOI] [PubMed] [Google Scholar]
- 9.Kaplan RM, Anderson JP. The general health policy model: An integrated approach. Q Life Pharmacoeconomics Clin Trials. 1996;2:302–22. [Google Scholar]
- 10.Dunlop CA, Radaelli CM. Does policy learning meet the standards of an analytical framework of the policy process? Policy Stud J. 2018;46:48–68. doi: 10.1111/psj.12250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Butler A, Hall H, Copnell B. A guide to writing a qualitative systematic review protocol to enhance evidence-based practice in nursing and health care. Worldviews Evid Based Nurs. 2016;13:241–9. doi: 10.1111/wvn.12134. [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med. 2009;151:264–9, W64. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 13.Dixon-Woods M, Sutton A, Shaw R, Miller T, Smith J, Young B, et al. Appraising qualitative research for inclusion in systematic reviews: A quantitative and qualitative comparison of three methods. J Health Serv Res Policy. 2007;12:42–7. doi: 10.1258/135581907779497486. [DOI] [PubMed] [Google Scholar]
- 14.Suri H. Purposeful sampling in qualitative research synthesis. Qualitative Res J. 2011;11:63–75. [Google Scholar]
- 15.Janakiram C, Sanjeevan V, Br R, Joseph J, Stauf N, Benzian H. Political priority of oral health in India: Analysis of the reasons for neglect. J Public Health Dent. 2018;78:144–53. doi: 10.1111/jphd.12254. [DOI] [PubMed] [Google Scholar]
- 16.Laverty L, Harris R. Can conditional health policies be justified? A policy analysis of the new NHS dental contract reforms. Soc Sci Med. 2018;207:46–54. doi: 10.1016/j.socscimed.2018.04.041. [DOI] [PubMed] [Google Scholar]
- 17.Leck V, Randall GE. The rise and fall of dental therapy in Canada: A policy analysis and assessment of equity of access to oral health care for Inuit and First Nations communities. Int J Equity Health. 2017;16:131. doi: 10.1186/s12939-017-0631-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Onwujekwe O, Uguru N, Russo G, Etiaba E, Mbachu C, Mirzoev T, et al. Role and use of evidence in policymaking: An analysis of case studies from the health sector in Nigeria. Health Res Policy Syst. 2015;13:46. doi: 10.1186/s12961-015-0049-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Etiaba E, Uguru N, Ebenso B, Russo G, Ezumah N, Uzochukwu B, et al. Development of oral health policy in Nigeria: An analysis of the role of context, actors and policy process. BMC Oral Health. 2015;15:56. doi: 10.1186/s12903-015-0040-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Benedetti G, Stauf N, Strohmenger L, Campus G, Benzian H. Political priority of oral health in Italy: An analysis of reasons for national neglect. Int Dent J. 2015;65:89–95. doi: 10.1111/idj.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gwozdek AE, Tetrick R, Shaefer HL. The origins of Minnesota’s mid-level dental practitioner: Alignment of problem, political and policy streams. J Dent Hyg. 2014;88:292–301. [PubMed] [Google Scholar]
- 22.Adeniyi AA, Sofola OO, Kalliecharan RV. An appraisal of the oral health care system in Nigeria. Int Dent J. 2012;62:292–300. doi: 10.1111/j.1875-595X.2012.00122.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lewis JM. Influencing public policy on oral health. Community Dent Oral Epidemiol. 2012;40:148–53. doi: 10.1111/j.1600-0528.2012.00735.x. [DOI] [PubMed] [Google Scholar]
- 24.Singh S, Myburgh NG, Lalloo R. Policy analysis of oral health promotion in South Africa. Glob Health Promot. 2010;17:16–24. doi: 10.1177/1757975909356631. [DOI] [PubMed] [Google Scholar]
- 25.Watt R, Fuller S, Harnett R, Treasure E, Stillman-Lowe C. Oral health promotion evaluation–time for development. Community Dent Oral Epidemiol. 2001;29:161–6. doi: 10.1034/j.1600-0528.2001.290301.x. [DOI] [PubMed] [Google Scholar]
- 26.Petersen PE. World Health Organization global policy for improvement of oral health–World Health Assembly 2007. Int Dent J. 2008;58:115–21. doi: 10.1111/j.1875-595x.2008.tb00185.x. [DOI] [PubMed] [Google Scholar]
- 27.Petersen PE, Estupinan-Day S, Ndiaye C. WHO's action for continuous improvement in oral health. SciELO Public Health. 2005 [PMC free article] [PubMed] [Google Scholar]
- 28.Petersen PE. Improvement of global oral health—The leadership role of the World Health Organization. Community Dent Health. 2010;27:194–8. [PubMed] [Google Scholar]
- 29.McDonough JE. Might oral health be the next big thing? Milbank Q. 2016;94:720–3. doi: 10.1111/1468-0009.12225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pitts N, Amaechi B, Niederman R, Acevedo AM, Vianna R, Ganss C, et al. Global oral health inequalities: Dental caries task group–research agenda. Adv Dent Res. 2011;23:211–20. doi: 10.1177/0022034511402016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Petersen PE. Global policy for improvement of oral health in the 21st century—Implications to oral health research of World Health Assembly 2007, World Health Organization. Community Dent Oral Epidemiol. 2009;37:1–8. doi: 10.1111/j.1600-0528.2008.00448.x. [DOI] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. Preventing and controlling oral and Pharyngeal cancer. Recommendations from a national strategic planning conference. MMWR. 1998;47(No. RR-14):1–14. [PubMed] [Google Scholar]
- 33.Nash DA, Mathu-Muju KR, Friedman JW. The dental therapist movement in the United States: A critique of current trends. J Public Health Dent. 2018;78:127–33. doi: 10.1111/jphd.12252. [DOI] [PubMed] [Google Scholar]
- 34.Sabatier PA, Weible CM. The advocacy coalition framework. Theories Policy Proc. 2007;2:189–220. [Google Scholar]
- 35.Mokken RJ, Stokman FN. Power and In?uence as Political Phenomena. Amsterdam, University of Amsterdam, Institute for Political Science. 1974 [Google Scholar]
- 36.Shiffman J, Smith S. Generation of political priority for global health initiatives: A framework and case study of maternal mortality. Lancet. 2007;370:1370–9. doi: 10.1016/S0140-6736(07)61579-7. [DOI] [PubMed] [Google Scholar]
- 37.Wasserman S, Faust K. Cambridge: Cambridge University Press; 1994. Social Network Analysis: Methods and Applications. [Google Scholar]
- 38.Maxwell RJ. Quality assessment in health. Br Med J (Clin Res Ed) 1984;288:1470–2. doi: 10.1136/bmj.288.6428.1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kalaja R, Myshketa R, Scalera F. Service quality assessment in health care sector: The case of Durres public hospital. Procedia-Soc Behav Sci. 2016;235:557–65. [Google Scholar]
- 40.Fairclough I, Fairclough N. London, Routledge: 2012. Political Discourse Analysis, a Method forAdvanced Students. [Google Scholar]
- 41.Lupton D. Discourse analysis: A new methodology for understanding the ideologies of health and illness. Aust J Public Health. 1992;16:145–50. doi: 10.1111/j.1753-6405.1992.tb00043.x. [DOI] [PubMed] [Google Scholar]
- 42.Lee H, Lomazzi M, Lee A, Bedi R. Global oral health in the framework of the global charter for the public’s health. J Public Health Policy. 2018;39:245–53. doi: 10.1057/s41271-018-0121-4. [DOI] [PubMed] [Google Scholar]
- 43.Sabatier PA. Top-down and bottom-up approaches to implementation research: A critical analysis and suggested synthesis. J Public Policy. 1986;6:21–48. [Google Scholar]
- 44.Vedung E. Public Policy and Program Evaluation. New York: Routledge; 2017. [Google Scholar]
- 45.Slade GD. Measuring Oral Health and Quality of Life. North Carolina, Department of Dental Ecology, School of Dentistry, Universityof North Carolina. 1997 [Google Scholar]
- 46.Petersen PE, Kwan S. Evaluation of community-based oral health promotion and oral disease prevention—WHO recommendations for improved evidence in public health practice. Community Dent Health. 2004;21:319–29. [PubMed] [Google Scholar]
- 47.Buchholz RA, Rosenthal SB. Stakeholder theory and public policy: How governments matter. J Business Ethics. 2004;51:143–53. [Google Scholar]