Abstract
Background:
Surrounding green, air pollution, and noise have been associated with cardiometabolic diseases, but most studies have assessed only one of these correlated exposures.
Objectives:
We aimed to evaluate associations of combined exposures to green, air pollution, and road traffic noise with cardiometabolic diseases.
Methods:
In this cross-sectional study, we studied associations between self-reported physician-diagnosed diabetes, hypertension, heart attack, and stroke from a Dutch national health survey of 387,195 adults and residential surrounding green, annual average air pollutant concentrations [including particulate matter with aerodynamic diameter (), PM with aerodynamic diameter (), nitrogen dioxide (), and oxidative potential (OP) with the dithiothreitol (DTT) assay ()] and road traffic noise. Logistic regression models were used to analyze confounding and interaction of surrounding green, air pollution, and noise exposure.
Results:
In single-exposure models, surrounding green was inversely associated with diabetes, while air pollutants (, ) and road traffic noise were positively associated with diabetes. In two-exposure analyses, associations with green and air pollution were attenuated but remained. The association between road traffic noise and diabetes was reduced to unity when adjusted for surrounding green or air pollution. Air pollution and surrounding green, but not road traffic noise, were associated with hypertension in single-exposure models. The weak inverse association of surrounding green with hypertension attenuated and lost significance when adjusted for air pollution. Only was associated with stroke and heart attack.
Conclusions:
Studies including only one of the correlated exposures surrounding green, air pollution, and road traffic noise may overestimate the association of diabetes and hypertension attributed to the studied exposure. https://doi.org/10.1289/EHP3857
Introduction
In daily life, humans are exposed to a mixture of environmental exposures that can affect health. Exposure to air pollution and road traffic noise, for example, have both been associated with increased risks of diabetes and hypertension (Wang et al. 2014a; Balti et al. 2014; Eze et al. 2015; Dzhambov 2015; Fuks et al. 2014, Van Kempen and Babisch 2012). Air pollution and road traffic noise may induce inflammation, oxidative stress, vascular dysfunction, and autonomic nervous system imbalance, thereby contributing to the development of cardiometabolic diseases (Münzel et al. 2016b). On the other hand, research suggests that exposure to surrounding green is associated with reduced risks of cardiometabolic disease (Dalton et al. 2016; Astell-Burt, et al. 2014; Ngom et al. 2016; Maas et al. 2009). Surrounding green has been hypothesized to benefit health via several pathways, including promoting physical activity and social cohesion and decreasing psychological stress (Hartig et al. 2014; Nieuwenhuijsen et al. 2017).
Long-term exposures to surrounding green, air pollution, and road traffic noise are, to a certain extent, related to each other. Higher levels of surrounding green, for example, tend to go together with lower levels of air pollution and traffic noise because of absence of air pollution and noise sources in green areas or removal of air pollutants from the air (Markevych et al. 2017). Road traffic noise is related to traffic intensity, which also affects traffic related air pollutants such as nitrogen dioxide () and black carbon [ ()], which can lead to spatial correlation between air pollution and road traffic noise (Münzel et al. 2016a; Tétreault et al. 2013). Correlations between surrounding green, air pollution, and road traffic noise depend on the study setting but are typically moderate (Boogaard et al. 2009; Fecht et al. 2016, Hystad et al. 2014, Thiering et al. 2016; Dadvand et al. 2012).
The large majority of studies on the associations of long-term exposure to surrounding green, air pollution, or road traffic noise have evaluated single-exposure associations of one of these environmental exposures, ignoring potential confounding by and interaction with the other two environmental exposures. Therefore, it is difficult to interpret the results of studies that only evaluated single exposures. Only a few studies investigated the combined effects of these environmental exposures with cardiometabolic diseases. Some of these studies suggest that exposure to air pollution confounds associations with exposure to road traffic noise and vice versa (Balti et al. 2014; Eze et al. 2017; Floud et al. 2013; Bodin et al. 2016; Selander et al. 2009; Sørensen et al. 2013), while there are also indications for interaction effects between air pollution and road traffic noise (Sørensen et al. 2014).
Studies that evaluated associations of surrounding green with health have treated air pollution and traffic noise as confounders (Hystad et al. 2014; Crouse et al. 2017; Thiering et al. 2016; Villeneuve et al. 2012) or as mediators (James et al. 2016; Gascon et al. 2018; Dzhambov et al. 2018). The difference between treating them as confounders or mediator is the assumption of causality of the relationships of surrounding green with air pollution and road traffic noise. If air pollution and road traffic noise are on the causal pathway from surrounding green to health, mediation analysis is appropriate. Such a causal relationship is supported by the fact that more surrounding green may lead to lower road traffic noise and air pollution concentrations by limiting dispersion of noise and air pollution through green barriers or by scavenging of air pollution. These mechanisms, however, explain only part of the empirical correlations of surrounding green with air pollution and road traffic noise. More important is the fact that in a greener area, there are fewer sources of air pollution and road traffic noise and, consequently, lower air pollution and noise levels. This reflects a common source (or lack thereof) and thus not a causal pathway from surrounding green to health. Hence, air pollution and road traffic noise can be considered both as confounders and as mediators in the analysis of the relationship between surrounding green and health.
Strak et al. (2017) previously reported associations between exposure to air pollution and diabetes in a large national health survey of 387,195 citizens . For the current study, surrounding green and road traffic noise were also added to the health survey data. Further, besides diabetes, we also included hypertension, stroke, and heart attack. For all these health end points, there is some evidence for associations with surrounding green, air pollution, and road traffic noise from typically single-exposure studies. The aim of this study was to evaluate associations of combined long-term exposure to surrounding green, air pollution, and road traffic noise with prevalence of diabetes, hypertension, stroke, and heart attack.
Methods
We specifically analyzed potential confounding and interaction of long-term exposure to surrounding green, air pollution, and road traffic noise. In addition, we analyzed mediation to evaluate whether decreased levels of air pollution and road traffic noise are possible mechanisms underlying potential beneficial associations of surrounding green with cardiometabolic outcomes. For the mediation analyses, we thus assumed that air pollution and road traffic noise would be on the causal pathway from surrounding green to health, while for the confounding analyses, we assumed that air pollution and road traffic noise were not on the causal pathway from surrounding green to health. Figure 1 provides a graphical representation of the four approaches (single exposure, confounding, interaction, and mediation). Air pollution and road traffic noise were treated as mutual confounders, because one exposure is not on the causal pathway of the other exposure to health.
Figure 1.
Schematic overview of the analyses performed for two exposures and one health outcome. The black solid lines represent hypothesized causal relationships; the black dashed line represents a noncausal relationship. Note: NDVI, Normalized Difference Vegetation Index; OPDTT, oxidative potential (OP) metric with dithiothreitol (DTT).
Study Design and Study Population
We used cross-sectional data from a national health survey [Dutch Public Health Monitor 2012 (PHM) (Gezondheidsmonitor Volwassenen GGD-en, CBS en RIVM)] that covered issues related to personal characteristics, lifestyle, socioeconomic status (SES), and physical and mental health. The PHM was conducted by 28 public health services (GGD-en), Statistics Netherlands (CBS), and the National Institute for Public Health and the Environment (RIVM) in 2012. The elderly () were oversampled as part of the design of the PHM. The PHM includes information on 387,195 citizens aged ; the response rate was 45–50%. The home address of each subject was geocoded; hence, no individuals were excluded due to missing geocodes.
Statistics Netherlands enriched the PHM with information on standardized household income and country of origin. Standardized household income was adjusted for differences in household size and composition. The PHM was also linked with information on SES at the neighborhood level (four-digit postal code area). This indicator represents the educational, occupational, and economical status of the neighborhood and is derived by the Netherlands Institute for Social Research (Knol 1998). A high SES neighborhood score indicates a high SES of the neighborhood. We used the 2002 SES score. The 2002 SES correlated highly with the 2010 SES score, which became available in a late phase of the study ().
Outcome Definition
The PHM included questions on diabetes, hypertension, stroke, and heart attack. The main questions were: “Do you have diabetes?”, “Do you have hypertension?”, “Have you ever had a stroke?” and “Have you ever had a heart attack?”. These questions were followed by a question “In the last 12 months, have you been treated for … by a physician or a specialist?”. Strak et al. (2017) previously showed that 92% of positive answers to the main question for diabetes were also positive in the question about treatment by a physician or specialist in this study population. Moreover, nearly 85% of the population with self-reported physician-diagnosed diabetes in the past 12 months have also been prescribed diabetes medication, based on an external database (Strak et al. 2017). For hypertension, 91% of the positive answers for the main question were also positive in the question about treatment by a physician or specialist. For heart attack, 70% of the people who ever had a heart attack reported that they have been treated by a physician or a specialist within the last 12 months. For stroke, this was 49%.
Self-reports from questionnaires have been found to agree moderately to very well with medical records for diabetes, hypertension, and heart attack; kappa coefficients ranged from 0.76 to 0.80 for diabetes, from 0.56 to 0.75 for hypertension, and from 0.48 to 0.80 for heart attack (Okura et al. 2004; Schneider et al. 2012; Hansen et al. 2014; Muggah et al. 2013; Machón et al. 2013). Agreements for stroke varied per study; kappa statistics ranged from 0.35 to 0.71 (Okura et al. 2004; Schneider et al. 2012; Muggah et al. 2013; Machón et al. 2013; Hansen et al. 2014).
We used the questions about treatment by a physician or specialist to define health outcomes. As agreements between the main question and the question about treatment were moderate for heart attack and stroke, the first question (“Have you ever had a heart attack/stroke”) was used as the health outcome in sensitivity analyses.
Exposure Assessment
Surrounding green.
We used two green metrics to assess exposure to surrounding green that have been described previously (Klompmaker et al. 2017). In brief, the Normalized Difference Vegetation Index (NDVI) was used to assess surrounding greenness, i.e., average density of green vegetation within a circular buffer around the participant’s residential address. The NDVI was derived from LANDSAT 5 TM and captures the density of green vegetation at a spatial resolution of based on land surface reflectance of visible (red) and near-infrared parts of spectrum (https://earthobservatory.nasa.gov). NDVI values range between and 1, with higher numbers indicating more photosynthetically active greenness and thus a higher density of green vegetation. Negative NDVI values were set to zero (Klompmaker et al. 2017). We combined cloud-free images from the summer of 2010 to create a map that covers (almost) the whole country.
A highly detailed national land-use database of the Netherlands of 2010 [TOP10NL, CC-BY Kadaster, https://www.kadaster.com/automatic-generalisation (Kadaster 2010)] was used to assess surrounding green space, i.e., the proportion of green space within a buffer around the participant’s residential address. TOP10NL divides the Netherlands into polygons with different classes of land use (water, road, and terrain). The terrain class is divided in 21 subclasses; 11 of these classes correspond to green areas. TOP10NL does, in contrast to the NDVI, not include private green property (such as gardens) and street greenery.
Surrounding greenness and surrounding green space were assessed in buffers with radii of 100; 300; 500; 1,000; and for all addresses in the Netherlands. Analyses to assess surrounding green were performed in ArcGIS (version 10.2.2; Esri).
Air pollution.
For each home address, long-term average concentrations of particulate matter [PM with aerodynamic diameter (), , PM with aerodynamic diameter (), ] and were assessed by land-use regression (LUR) models developed within the framework of the European Study of Cohorts for Air Pollution Effects (ESCAPE) project (Beelen et al. 2013; Eeftens et al. 2012). levels higher than () were set to , as these values are probably due to an unrealistic combination of explanatory variables. Further, we used long-term average concentrations of two oxidative potential (OP) metrics: electron spin resonance () and dithiothreitol () (Yang et al. 2015). OP is an intrinsic measure of PM to oxidize target molecules, and thus, it effectively incorporates biologically relevant properties of PM (Yang et al. 2015). Performances of LUR models were evaluated using leave-one-out cross validation (R2LOOCV) and ranged from 0.38 for to 0.89 for (Table S1). Models were based on air pollution measurements conducted in 2009, 3 y prior to the health survey. There were no LUR models available for 2012. Previous studies have shown that the spatial variation of air pollution and traffic noise exposure levels remain stable over periods of about 10 y in Western countries (Eeftens et al. 2011; Fecht et al. 2016).
Road traffic noise.
Residential road traffic noise levels were assessed by the Standard Model Instrumentation for Noise Assessments (STAMINA). STAMINA is a model to map environmental noise in the Netherlands. This model was developed at the Dutch National Institute for Public Health and the Environment (RIVM) and uses the standard Dutch calculation method for traffic and industrial noise (Schreurs et al. 2010). The spatial resolution of the noise maps depends on the distance between source and observation point. The lowest resolution is , and close to the source the level of detail is the highest, with a resolution of (Schreurs et al. 2010). This method is used in the Netherlands to implement the European Environmental Noise Directive (EU Directive 2002).
Daily average (24 h, Lden) and nighttime average (2300–0700 hours, Lnight) road traffic noise exposures were assessed for 2011. Because Lden and Lnight were highly correlated [Spearman’s rank order correlation coefficient ], we only used Lden in our analyses.
Exclusion of Subjects
Since we did not have land-use data across the border of the Netherlands, subjects with residential addresses within (largest buffer) of the border of the Netherlands were excluded from our analyses (8.4%).
Statistical Analyses
We calculated Spearman correlations to evaluate relations between the exposure variables at PHM subject addresses. We developed logistic regression models to study whether the exposure variables were associated with cardiometabolic diseases (diabetes, hypertension, stroke, and heart attack). We performed single-exposure, multi-exposure (confounding and interaction), and mediation analyses. An example of the different analyses performed for surrounding greenness (NDVI ), air pollution (), and diabetes is shown in Figure 1. Further, we calculated Spearman correlations between surrounding green, road traffic noise, and measured air pollution at the Dutch ESCAPE measurement sites to evaluate whether correlations between modeled and measured exposures differed.
All analyses were performed with R (version 3.3.1; R Development Core Team).
Single-exposure regression models.
We used single-exposure regression models to analyze individual associations of exposures. We specified a priori several regression models with increasing degree of covariate adjustment. Model 1 included age and sex. Model 2 was additionally adjusted for individual SES variables (marital status, country of origin, work, standardized household income, level of education). Model 3 further included smoking habits (current, former, never), number of cigarettes/day, alcohol consumption (current, former, never), number of alcohol glasses/week, physical activity, and body mass index. Model 4 was additionally adjusted for area-level SES (main model). Categories of covariates in the regression analyses were identical to the categories presented in Table 1, except for age (12 categories: 19–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–74, 75–84, ).
Table 1.
Characteristics of the population ().
| Characteristic | Category | (%) |
|---|---|---|
| Sex | Female | 193,782 (54.6) |
| Age (years) | 19–39 | 68,940 (19.4) |
| 40–64 | 134,161 (37.8) | |
| 151,726 (42.8) | ||
| Marital status | Married, living together | 246,775 (70.6) |
| Unmarried/never married | 42,233 (12.1) | |
| Divorced | 22,509 (6.4) | |
| Widowed | 38,089 (10.9) | |
| Country of origin | Dutch | 308,167 (86.8) |
| Other, Westerna | 29,215 (8.2) | |
| Other, non-Westernb | 6,543 (1.8) | |
| Netherlands Antilles | 1,500 (0.4) | |
| Suriname | 3,820 (1.1) | |
| Turkey | 3,284 (0.9) | |
| Morocco | 2,298 (0.6) | |
| Education | Primary or less | 33,679 (9.8) |
| Lower secondary | 119,549 (34.9) | |
| Higher secondary | 97,005 (28.3) | |
| University | 92,733 (27.0) | |
| Work | Yes | 158,704 (48.1) |
| Standardized household incomec | 35,539 (10.1) | |
| 67,391 (19.1) | ||
| 74,677 (21.2) | ||
| 83,916 (23.8) | ||
| 91,224 (25.9) | ||
| Smoking habits | Current | 65,702 (19.7) |
| Former | 133,267 (39.9) | |
| Never | 134,794 (40.4) | |
| Number of cigarettes/day for current smokers [mean (SD)] | — | 10.2 (8.3) |
| Alcohol consumption | Current | 280,311 (82.2) |
| Former | 20,564 (6.0) | |
| Never | 40,007 (11.7) | |
| Number of alcohol glasses/week for current consumers [mean (SD)] | — | 8.5 (9.6) |
| BMI | 4,628 (1.3) | |
| 154,595 (44.3) | ||
| 130,058 (37.2) | ||
| 59,987 (17.2) | ||
| Physical activity | 83,340 (25.1) | |
| 86,401 (26.0) | ||
| 80,470 (24.2) | ||
| 81,634 (24.6) | ||
| SES neighborhoodd | 75,223 (21.3) | |
| 30–34 | 78,723 (22.3) | |
| 35–38 | 73,947 (20.9) | |
| 38–43 | 58,521 (16.5) | |
| 67,342 (19.0) | ||
| Self-reported physician-diagnosed diabetes | Yes | 28,312 (8.0) |
| Self-reported physician-diagnosed hypertension | Yes | 65,407 (21.6) |
| Self-reported physician-diagnosed stroke | Yes | 6,975 (2.1) |
| Self-reported physician-diagnosed heart attack | Yes | 11,866 (3.5) |
| NDVI [median (IQR)] | — | 0.52 (0.13) |
| NDVI [median (IQR)] | — | 0.56 (0.14) |
| TOP10NL [median (IQR)]e | — | 0.24 (0.24) |
| TOP10NL [median (IQR)]f | — | 0.40 (0.32) |
| [median (IQR)] | 24.4 (1.24) | |
| [median (IQR)] | 8.1 (0.82) | |
| [median (IQR)] | 16.7 (0.83) | |
| [median (IQR)] | 1.2 (0.25) | |
| [median (IQR)]g | 23.4 (7.85) | |
| [median (IQR)] | 1.19 (0.27) | |
| [median (IQR)] | 0.89 (0.18) | |
| Road traffic noise [median (IQR)] | Lden (dB) | 53.3 (7.5) |
Note: —, no data; BMI, body mass index; CI, confidence interval, IQR, interquartile range, NDVI, Normalized Difference Vegetation Index; , nitrogen dioxide; , oxidative potential (OP) metric with dithiothreitol (DTT); , oxidative potential (OP) metric with electron spin resonance; , PM with aerodynamic diameter ; , black carbon (); , particulate matter with aerodynamic diameter ; SD, standard deviation; SES, socioeconomic status; A.U., arbitrary unit.
Other Western: Europe, North America, Oceania, Indonesia, Japan.
Other non-Western: Africa, Latin America, Asia (excluding Indonesia and Japan).
Standardized household income is adjusted for differences in household size and composition.
SES neighborhood represents the educational, occupational, and economical status of the neighborhood.
Surrounding green space in a buffer based on TOP10NL.
Surrounding green space in a buffer based on TOP10NL.
values higher than were set at .
For each exposure variable, we specified a regression model with the exposure variable as linear term [1 degree of freedom (df)]. Additionally, we used natural splines (3 df) to determine the linearity of exposure–response relationships (only for the main model). To test whether the goodness of fit of the models with splines was significantly better than the goodness of fit of the linear models, we used the likelihood ratio test and defined statistical significance by a two-sided alpha level of . Exposure–response curves showed a nonsignificant or small to moderate deviation from linearity for most associations (Figure S1). Deviations from linearity primarily occurred in areas with very few data, as evidenced by the wide confidence intervals (CIs) of the nonlinear part of most curves. We considered the deviations from linearity to be sufficiently large to present both linear and quintile analyses in the paper, but not large enough to make the linear analysis uninformative. We a priori decided to use quintiles instead of tertiles or quartiles to obtainer a finer assessment, which was made possible by the large study population. We presented the linear effect estimate of exposure to surrounding green and air pollution per interquartile range (IQR) and for road traffic noise per . We used instead of the IQR, as this is the standard for reporting of noise effect estimates.
Surrounding green in different buffer sizes was highly correlated, and associations between closely related buffer sizes, such as 1,000 and , barely differed (data not shown). Hence, we decided to only report associations of the 300- and buffers and focus on these buffers in the multi-exposure models to limit the number of reported analyses.
As sensitivity analyses, we evaluated associations of surrounding green, air pollution, and road traffic noise with cardiometabolic diseases in the elderly population (, ). Further, we evaluated the associations of exposures with heart attack and stroke by the questions if participants ever had a heart attack () or stroke () instead of if they have been treated by a physician or a specialist within the last 12 months for a heart attack or stroke.
Multi-exposure regression models.
We used multi-exposure models to analyze whether a potential association of one of the environmental exposures with cardiometabolic health was confounded by other environmental exposures. Here, we specified surrounding green, air pollution, and road traffic noise as mutual confounders in the analyses with cardiometabolic health and thus assumed a noncausal relationship between surrounding green and air pollution and road traffic noise.
To evaluate potential mutual confounding of exposures, we specified two-exposure models. We performed multi-exposure regression analyses with combinations of surrounding green, air pollutants, and road traffic noise exposures. We used generalized variance inflation factors to quantify multicollinearity between the exposures (Fox and Monette 1992).
Joint odds ratio.
In epidemiological studies, it can be difficult to disentangle individual effects of correlated exposures, as exposure estimates share overlapping information. Hence, in exposure–health models, the estimated coefficient for one exposure based on a single-exposure model could be partly or fully explained (confounded) by the overlapping information with another exposure, depending on the extent of overlap and the associations with the outcome. Therefore, the estimated coefficient for an exposure from a single-exposure model could be an overestimation of the true coefficient of that exposure. However, because no adjustment for the overlapping information with the other exposure is made in a single-exposure model, the coefficient of the single-exposure model could be a good indication for the joint coefficient of both exposures.
A joint coefficient of co-occurring exposures can be assessed using the cumulative risk index (CRI) method (Crouse et al. 2015; Jerrett et al. 2013; Lippmann et al. 2013). Previous studies used the CRI to find out which combinations of air pollutants are required to fully capture the toxicity of the mix of air pollutants (Jerrett et al. 2013; Crouse et al. 2015). We used the CRI to investigate which combination of exposures is needed to assess the joint impact of surrounding green, air pollution, and road traffic noise on cardiometabolic diseases. As we found negative correlations between surrounding green, air pollution, and road traffic noise, exposure to a combination of low levels of surrounding green and high levels of air pollution and road traffic noise or the other way around seems to occur more frequently than exposure to high or low levels of all three exposures. Hence, we estimated the association of a combination of increased air pollution and road traffic noise and decreased surrounding green. The joint odds ratio (JOR) represents the odds for a 1-unit (IQR) increase in air pollution and road traffic noise and a 1-unit decrease in surrounding green exposure relative to the odds for no increase (no decrease in surrounding green) in any of the exposures. The direction of the associations of surrounding green in the JORs are opposite to the direction used to describe associations of surrounding green in single- and multi-exposure models.
We denote the JOR based on the combination of the p exposures evaluated at x as the CRI and define it as
where are the estimates of the log odds ratio (OR) for the p exposures estimated in a logistic regression model consisting of all p exposures together, are the levels at which each exposure-specific OR is evaluated, and denotes the JOR for the exposure in a multiexposure model. JORs were estimated assuming additive effect estimates (log ORs) of joint exposures. The 95% CI of CRI is defined by: . This definition of the CI is similar to that described by Crouse et al. (2015) and Jerrett et al. (2013). Interactions are not formally incorporated in the CRI method, as only main terms of exposures are included in the regression model used to calculate the CRI.
Interaction analyses.
To evaluate potential interactions of combined exposures, we specified interaction terms in two-exposure models. To be able to observe patterns of interactions, we assessed interactions by combining a continuous exposure with quintiles of another exposure and vice versa, and by continuous exposure terms. Interactions were assessed on the multiplicative scale, the extent to which, on the OR scale, the effect estimate of being exposed to both exposures together exceeds the product of the effect estimates of the two exposures considered separately. We hypothesized that the association with exposure to air pollution is strongest (increased odds) in the highest road traffic noise quintile and vice versa. Further, we hypothesized that the association with air pollution and road traffic noise is strongest (increased odds) in the lowest surrounding green quintile and that the association with surrounding green is strongest (decreased odds) in the lowest air pollution or road traffic noise quintile. The rationale for this is that there is some evidence that associations of air pollution are stronger for people with psychological distress (Hicken et al. 2014) and that people who live in greener areas generally report less psychological distress (Gascon et al. 2015).
Mediation analyses.
We performed mediation analyses to evaluate whether decreased levels of air pollution and road traffic noise are possible mechanisms underlying potential beneficial associations of surrounding green on cardiometabolic outcomes. We think that the application of mediation analyses in our cross-sectional study is reasonable because we assess mediation between environmental factors where the relationship is immediate. Mediation analysis does not add to the general limitation of our cross-sectional study. Previous mediation analyses in a cohort study have also applied green and air pollution from the same study period (James et al. 2016). Here, we specified air pollution and road traffic noise as mediators in the surrounding green–health association and thus assumed a causal effect between surrounding green, air pollution, and road traffic noise. Mediation analyses were only performed when surrounding green was significantly associated (decreased OR) with a cardiometabolic outcome in a single-exposure model. Of the potential mediator variables (air pollutants and road traffic noise), we only selected the exposures that were significantly associated (increased ORs) with the cardiometabolic outcome for the mediation analyses.
We used the mediation package to estimate the direct, indirect, and total effects and the proportion mediated (Imai et al. 2010; Tingley et al. 2014). The mediation package uses the counterfactual framework to clarify the assumptions needed for causal mediation. Briefly, we specified mediator models () and outcome models (). Both models were adjusted for SES indicators and lifestyle factors (Model 4). Next, we included the model objects (mediator model and outcome model) in the mediate function and specified the “treat” (surrounding green) and “mediator” variables. We used continuous terms for the treat and mediator variables in the mediation analyses. Exposure–response curves of associations between surrounding green and the mediators showed small deviations from linearity. We assessed CIs by 300 nonparametric bootstrap simulations. Due to computational limitations, we were not able to run the recommended 1,000 bootstrap simulations (Tingley et al. 2014).
Four important underlying confounding assumptions are required for the mediation analyses: no unmeasured exposure–outcome confounding, no unmeasured exposure–mediator confounding, no unmeasured mediator–outcome confounding, and no mediator–outcome confounder is affected by the exposure (VanderWeele 2016). While we were not able to verify these assumptions, we included major confounders in our mediation analyses and hence believe these assumptions are reasonable.
Results
Public Health Monitor Statistics
Our study population consisted of 354,827 persons aged 19 y or older (Table 1). Due to oversampling of the elderly, almost 43% of the subjects were 65 y or older. Further, people of Dutch origin (86.8% compared with 78% in the general population) were overrepresented in the PHM. More information on the study population can be found elsewhere (Statistics Netherlands 2015).
Of our study population, 8.0% reported physician-diagnosed diabetes. Treatment in the past 12 months by a physician for hypertension was reported by 21.6% of the population, and treatment by a physician for heart attack and stroke was reported by 3.5% and 2.1% of the population, respectively. The degree of overlap between the cardiometabolic diseases was moderate to low. Of all subjects, 20.8% reported only one cardiometabolic disease. Two, three, and four cardiometabolic diseases were reported by 5.3%, 0.6%, and of the subjects, respectively. Agreements between the outcomes were low; kappa values ranged from 0.05 to 0.18.
Exposure Distribution and Correlations
The variability of TOP10NL surrounding green space [expressed as median (IQR)] was larger compared with NDVI surrounding greenness (Table 1). The variability of and was substantially lower than the variability of the other pollutants, particularly and . Road traffic noise varied less than but more than and (Table 1).
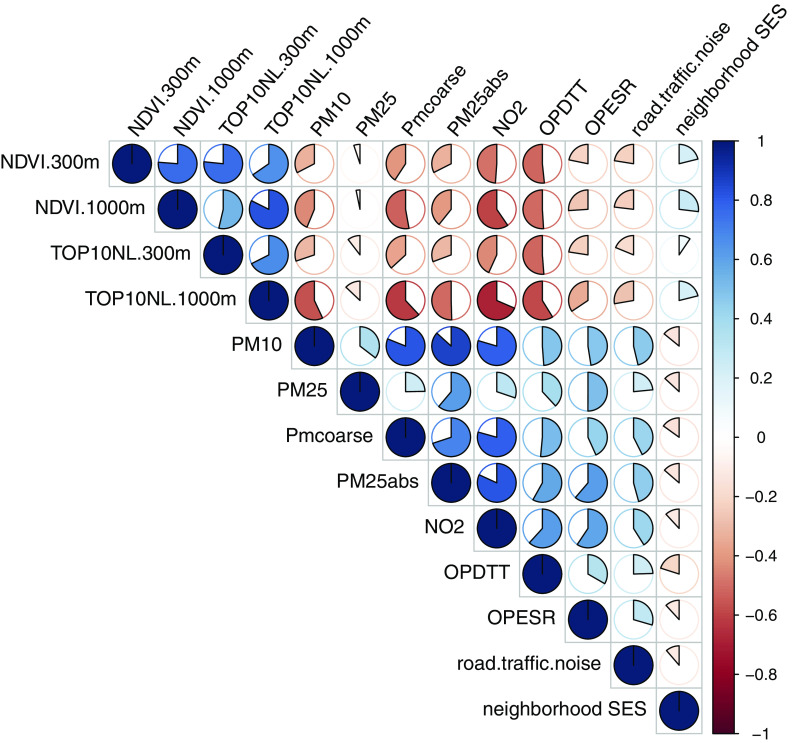
Surrounding green, air pollution, and road traffic noise exposures at the study participants’ home addresses were overall moderately correlated. In general, surrounding green (both NDVI and TOP10NL) in a buffer was slightly more strongly negatively correlated with concentrations of air pollutants and road traffic noise compared with surrounding green in a buffer (Figure 2). There was no correlation between NDVI surrounding greenness and (). Road traffic noise correlated weak to moderately with concentrations of air pollutants (, Figure 2). Surrounding green was weakly positively correlated with neighborhood SES (more green in higher SES neighborhoods), while air pollution and road traffic noise were weakly negatively correlated with neighborhood SES (Figure 2). Spatial collinearity was therefore not a concern in our analyses.
Figure 2.
Spearman correlations between surrounding green, air pollution, road traffic noise, and neighborhood socioeconomic status (SES). Clockwise pies denote positive correlations, and counterclockwise pies denote negative correlations. Note: All correlations are statistically significant, different from 0.0 (). Surrounding green space in a buffer based on TOP10NL; surrounding green space in a buffer based on TOP10NL. NDVI, Normalized Difference Vegetation Index; , nitrogen dioxide; , oxidative potential (OP) metric with dithiothreitol (DTT); , oxidative potential (OP) metric with electron spin resonance; , PM with aerodynamic diameter ; , particulate matter with aerodynamic diameter .
Single-Exposure Regression Models
Analyses with surrounding green as continuous terms and quintiles of surrounding green indicated a significant inverse association between surrounding green and diabetes in our main models (Table 2 for continuous term, Table S2 for quintiles). We found a weak inverse association between surrounding green and the odds of hypertension, which was significant in the analysis with surrounding green as continuous term and for the fifth quintile (Tables 2 and S2). We found no association between surrounding green and the odds of stroke or heart attack (Tables 2 and S2).
Table 2.
Results of single-exposure regression models.
| Exposure variable (increment) | OR (95% CI) | |||
|---|---|---|---|---|
| Diabetes | Hypertension | Stroke | Heart attack | |
| NDVI (0.13) | 0.91 (0.89, 0.93) | 0.97 (0.96, 0.99) | 1.00 (0.96, 1.04) | 1.00 (0.97, 1.03) |
| NDVI (0.14) | 0.92 (0.90, 0.94) | 0.99 (0.97, 1.01) | 1.00 (0.96, 1.04) | 1.04 (1.00, 1.07) |
| TOP10NL (0.24)a | 0.93 (0.91, 0.95) | 0.97 (0.95, 0.98) | 1.00 (0.96, 1.04) | 0.97 (0.94, 1.00) |
| TOP10NL (0.32)b | 0.91 (0.88, 0.93) | 0.98 (0.96, 0.99) | 0.98 (0.93, 1.03) | 0.99 (0.95, 1.03) |
| (7.85) | 1.06 (1.04, 1.09) | 1.02 (1.00, 1.03) | 1.00 (0.96, 1.04) | 0.98 (0.95, 1.02) |
| (0.27) | 1.09 (1.07, 1.12) | 1.06 (1.04, 1.07) | 1.02 (0.97, 1.06) | 1.03 (0.99, 1.06) |
| (0.18) | 1.02 (1.00, 1.04) | 1.01 (1.00, 1.03) | 1.02 (0.99, 1.06) | 1.00 (0.97, 1.02) |
| (1.24) | 1.03 (1.01, 1.05) | 1.00 (0.99, 1.01) | 1.00 (0.96, 1.03) | 0.97 (0.95, 1.00) |
| (0.83) | 1.01 (0.99, 1.03) | 1.01 (1.00, 1.02) | 1.05 (1.01, 1.09) | 1.07 (1.05, 1.10) |
| (0.25) | 1.03 (1.01, 1.05) | 1.01 (1.00, 1.02) | 1.02 (0.98, 1.05) | 1.01 (0.99, 1.04) |
| (0.82) | 1.03 (1.01, 1.05) | 1.00 (0.99, 1.01) | 1.01 (0.98, 1.05) | 0.96 (0.94, 0.99) |
| Road traffic noise, Lden (5) | 1.02 (1.00, 1.03) | 1.00 (0.99, 1.01) | 1.01 (0.98, 1.03) | 1.00 (0.98, 1.02) |
Note: Results are presented as OR (95% CI) per interquartile range increase (surrounding green and air pollution) or per (road traffic noise). Models were adjusted for sex, age, marital status, region of origin, education, work, standardized household income, smoking habits, number of cigarettes/day, alcohol consumption, number of alcohol glasses/week, physical activity, body mass index, and neighborhood socioeconomic status (SES). CI, confidence interval; Lden, daily average noise level; NDVI, Normalized Difference Vegetation Index; , nitrogen dioxide; , oxidative potential (OP) metric with dithiothreitol (DTT) assay; , oxidative potential (OP) metric with electron spin resonance; OR, odds ratio; , PM with aerodynamic diameter ; , black carbon (); , particulate matter with aerodynamic diameter .
Surrounding green space in a buffer based on TOP10NL.
Surrounding green space in a buffer based on TOP10NL.
For most air pollutants, analyses with quintiles and with continuous terms showed a significant positive association with diabetes, especially for and (Tables 2 and S2). , , , and were significantly associated with higher odds of hypertension (Tables 2 and S2). ORs for stroke and heart attack were increased for but not for other air pollutants (Tables 2 and S2).
Road traffic noise was positively associated with the odds of diabetes [; 95% CI: 1.00, 1.03) per ], but not with the odds of hypertension, stroke, or heart attack (Tables 2 and S2). Estimated exposure–response curves for diabetes and hypertension are shown in Figure S1.
Associations of surrounding green, air pollution, and road traffic noise with cardiometabolic outcomes were affected by the adjustment for covariates. In crude models, surrounding green, air pollution, and road traffic noise were significantly associated with diabetes, hypertension, stroke, and heart attack morbidity (Figure S2). Adjustment for individual SES and lifestyle factors attenuated the associations substantially ().
Sensitivity analyses showed similar associations with diabetes and hypertension in the elderly population () compared with the full population. Associations of with stroke and heart attack, on the other hand, were somewhat stronger for the elderly population compared with the full population (Table S3). In analyses with heart attack ever and stroke ever, no significant associations were found with surrounding green or road traffic noise (Table S4). For air pollution, only was significantly associated with stroke ever (; 95% CI: 1.01, 1.06 per IQR increase) and heart attack ever (; 95% CI: 1.01, 1.06 per IQR increase), similar to the analyses of our main (doctor-diagnosed) end points. Associations of were similar to associations of when values above were not set to (Table S5).
Multi-exposure Regression Models
Based on the findings of the single-exposure models, we decided to focus on diabetes and hypertension in multi-exposure models. We only used NDVI surrounding greenness exposure variables, as this is a commonly used green exposure measure in epidemiological studies. For air pollution, we used , , and , as these variables were most strongly associated with at least one cardiometabolic disease among the air pollutants.
Potential for confounding.
The association of NDVI surrounding greenness with diabetes attenuated slightly when adjusted for and vice versa (Table 3 for a buffer; Table S6 for a buffer). The effect estimate (OR) of NDVI attenuated from 0.91 (95% CI: 0.89, 0.93) per IQR increase to 0.93 (95% CI: 0.91, 0.96) and the effect estimate (OR) of attenuated from 1.09 (95% CI: 1.07, 1.12) per IQR increase to 1.05 (95% CI: 1.03, 1.08). Adjustment for road traffic noise hardly affected the associations of NDVI or with diabetes. Associations of road traffic noise with diabetes attenuated and lost significance when adjusted for NDVI of or .
Table 3.
Associations of surrounding green (NDVI ), air pollution (), and road traffic noise (Lden) with diabetes from single- and two-exposure models.
| Exposure variable | Exposure metrica | Two exposure (adj. for)b | |||
|---|---|---|---|---|---|
| OR (95% CI) | |||||
| Single exposure | NDVI | Road traffic noise (Lden) | |||
| NDVI | Continuous (per IQR) | 0.91 (0.89, 0.93) | — | 0.93 (0.91, 0.96) | 0.91 (0.89, 0.93) |
| Q1 () | 1.00 | — | 1.00 | 1.00 | |
| Q2 () | 0.98 (0.93, 1.03) | — | 0.99 (0.94, 1.04) | 0.98 (0.93, 1.03) | |
| Q3 () | 0.97 (0.93, 1.02) | — | 0.99 (0.94, 1.04) | 0.97 (0.93, 1.02) | |
| Q4 () | 0.91 (0.87, 0.96) | — | 0.95 (0.90, 0.99) | 0.92 (0.87, 0.96) | |
| Q5 () | 0.80 (0.76, 0.84) | — | 0.84 (0.79, 0.89) | 0.80 (0.76, 0.85) | |
| Continuous (per IQR) | 1.09 (1.07, 1.12) | 1.05 (1.03, 1.08) | — | 1.09 (1.07, 1.12) | |
| Q1 () | 1.00 | 1.00 | — | 1.00 | |
| Q2 () | 1.04 (0.99, 1.09) | 0.99 (0.94, 1.05) | — | 1.04 (0.98, 1.09) | |
| Q3 () | 1.07 (1.02, 1.13) | 1.00 (0.95, 1.06) | — | 1.07 (1.01, 1.12) | |
| Q4 () | 1.17 (1.11, 1.23) | 1.08 (1.02, 1.14) | — | 1.16 (1.11, 1.22) | |
| Q5 () | 1.20 (1.14, 1.26) | 1.10 (1.04, 1.16) | — | 1.19 (1.13, 1.25) | |
| Road traffic noise (Lden) | Continuous (per ) | 1.02 (1.00, 1.03) | 1.00 (0.99, 1.02) | 1.00 (0.99, 1.02) | — |
| Q1 () | 1.00 | 1.00 | 1.00 | — | |
| Q2 () | 1.05 (1.00, 1.11) | 1.03 (0.98, 1.08) | 1.04 (0.98, 1.09) | — | |
| Q3 () | 1.07 (1.01, 1.12) | 1.03 (0.98, 1.09) | 1.04 (0.99, 1.09) | — | |
| Q4 () | 1.08 (1.03, 1.13) | 1.04 (0.99, 1.10) | 1.05 (1.00, 1.10) | — | |
| Q5 () | 1.06 (1.01, 1.12) | 1.03 (0.98, 1.08) | 1.02 (0.97, 1.08) | — | |
Note: Results are presented as OR (95% CI) relative to the reference category for the quintile analyses () or per continuous increase in the linear model. Models were adjusted for sex, age, marital status, region of origin, education, work, standardized household income, smoking habits, number of cigarettes/day, alcohol consumption, number of alcohol glasses/week, physical activity, body mass index, and neighborhood socioeconomic status (SES). —, no data; CI, confidence interval; IQR, interquartile range; Lden, daily average noise level; NDVI, Normalized Difference Vegetation Index; , oxidative potential (OP) metric with dithiothreitol (DTT) assay; OR, odds ratio.
IQR for NDVI : 0.13, : .
In all two-exposure models, generalized variance inflation factor (GVIF) values were below 1.8.
Associations of with hypertension slightly attenuated after adjustment for NDVI (Table 4). The weak associations of NDVI with hypertension became insignificant when adjusted for ; the OR decreased from 0.97 (95% CI: 0.96, 0.99) to 0.99 (95% CI: 0.98, 1.01). Adjustments for road traffic noise did not affect the associations of or NDVI with hypertension.
Table 4.
Associations of surrounding green (NDVI ), air pollution (), and road traffic noise (Lden) with hypertension in single- and two-exposure models.
| Exposure variable | Exposure metrica | Two exposure (adj. for)b | |||
|---|---|---|---|---|---|
| OR (95% CI) | |||||
| Single exposure | NDVI | Road traffic noise (Lden) | |||
| NDVI | Continuous (per IQR) | 0.97 (0.96, 0.99) | — | 0.99 (0.98, 1.01) | 0.97 (0.96, 0.98) |
| Q1 () | 1.00 | — | 1.00 | 1.00 | |
| Q2 () | 1.03 (1.00, 1.07) | — | 1.04 (1.00, 1.07) | 1.03 (0.99, 1.07) | |
| Q3 () | 1.02 (0.99, 1.06) | — | 1.03 (1.00, 1.07) | 1.02 (0.99, 1.06) | |
| Q4 () | 1.00 (0.96, 1.03) | — | 1.02 (0.98, 1.05) | 0.99 (0.96, 1.03) | |
| Q5 () | 0.95 (0.91, 0.98) | — | 0.99 (0.95, 1.03) | 0.94 (0.91, 0.98) | |
| Continuous (per IQR) | 1.06 (1.04, 1.07) | 1.05 (1.04, 1.07) | — | 1.06 (1.04, 1.08) | |
| Q1 () | 1.00 | 1.00 | — | 1.00 | |
| Q2 () | 1.07 (1.03, 1.10) | 1.06 (1.02, 1.09) | — | 1.07 (1.03, 1.10) | |
| Q3 () | 1.06 (1.02, 1.09) | 1.04 (1.00, 1.08) | — | 1.06 (1.02, 1.09) | |
| Q4 () | 1.10 (1.07, 1.14) | 1.08 (1.04, 1.13) | — | 1.11 (1.07, 1.15) | |
| Q5 () | 1.12 (1.08, 1.16) | 1.10 (1.06, 1.14) | — | 1.12 (1.08, 1.16) | |
| Road traffic noise (Lden) | Continuous (per ) | 1.00 (0.99, 1.01) | 0.99 (0.98, 1.00) | 0.99 (0.98, 1.00) | — |
| Q1 () | 1.00 | 1.00 | 1.00 | — | |
| Q2 () | 1.04 (1.01, 1.08) | 1.03 (1.00, 1.07) | 1.03 (1.00, 1.07) | — | |
| Q3 () | 1.00 (0.97, 1.03) | 0.99 (0.95, 1.02) | 0.98 (0.95, 1.02) | — | |
| Q4 () | 1.00 (0.97, 1.04) | 0.99 (0.96, 1.03) | 0.99 (0.95, 1.02) | — | |
| Q5 () | 1.00 (0.96, 1.03) | 0.99 (0.95, 1.02) | 0.98 (0.94, 1.01) | — | |
Note: Results are presented as OR (95% CI) relative to the reference category () or per continuous increase. Models were adjusted for sex, age, marital status, region of origin, education, work, standardized household income, smoking habits, number of cigarettes/day, alcohol consumption, number of alcohol glasses/week, physical activity, body mass index, and neighborhood socioeconomic status (SES). —, no data; CI, confidence interval, IQR, interquartile range; Lden, daily average noise level; NDVI, Normalized Difference Vegetation Index; , oxidative potential (OP) metric with dithiothreitol (DTT) assay; OR, odds ratio.
IQR for NDVI : 0.13, : .
In all two-exposure models, generalized variance inflation factor (GVIF) values were below 1.8.
Associations of with stroke and heart attack were not affected by adjustment for surrounding green and traffic noise (Table S6), consistent with the lack of associations of these exposures with stroke and heart attack.
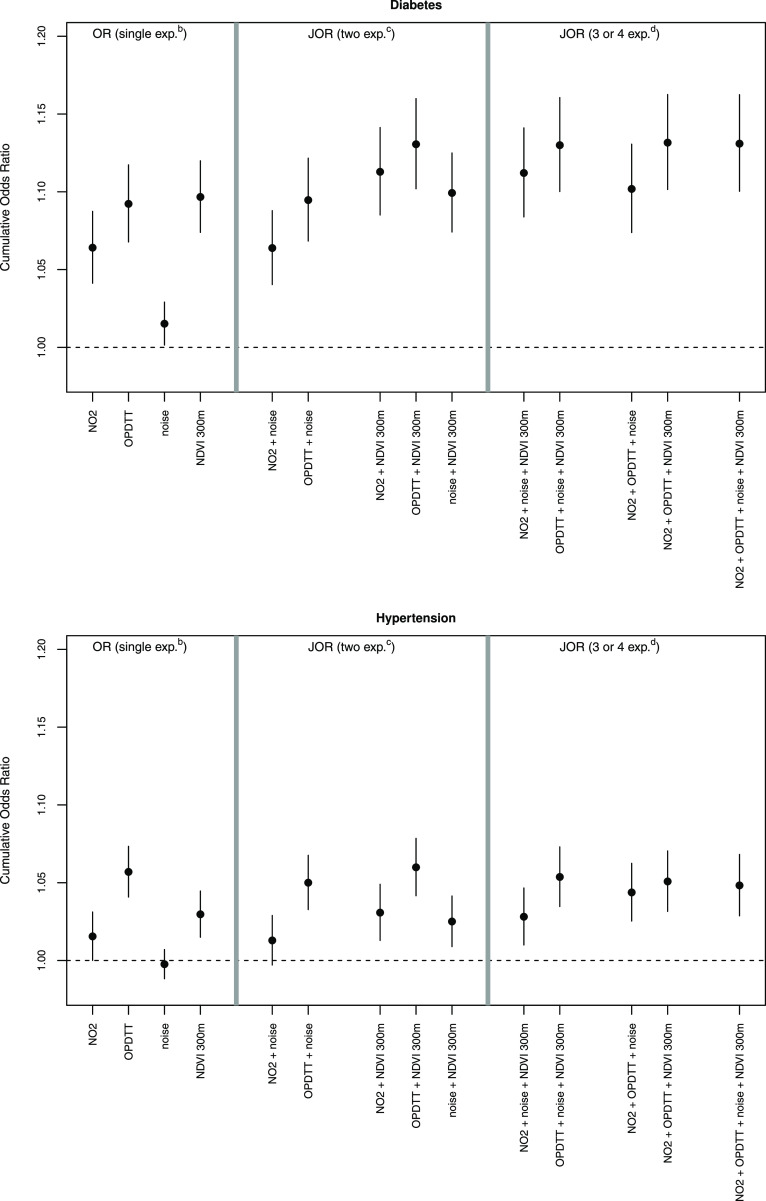
Joint odds ratio.
For diabetes, we found the largest JOR for a combination of and decreased NDVI (JOR: 1.13; 95% CI: 1.10, 1.16). The combined JOR was larger than the single-exposure ORs and similar to the JOR of , road traffic noise, and decreased NDVI and of , , road traffic noise, and decreased NDVI (Figure 3). For hypertension, the largest JOR was also found for a combination of and decreased NDVI (JOR: 1.06; 95% CI: 1.04, 1.08). However, the JOR was similar to the OR of in the single-exposure model (OR: 1.06; 95% CI: 1.04, 1.07).
Figure 3.
Joint odds ratios (JORs) for associations of air pollution, road traffic noise, and decreased surrounding green with diabetes and hypertension. The JORs are based on the CRI methods and represents the odds for a 1-unit [interquartile range (IQR)] increase in air pollution and road traffic noise and a 1-unit decrease in surrounding green exposure relative to the odds for no increase (no decrease in surrounding green) in any of the exposures. Results are given as JOR [95% confidence interval (CI)] per continuous increase for air pollution and road traffic noise and decrease for surrounding green (IQR for Normalized Difference Vegetation Index (NDVI) : 0.13, IQR for : , IQR for : , increment for road traffic noise: ) (main model). bORs are based on effect estimates of single-exposure models, cJORs are based on effect estimates of two-exposure models, dJORs are based on effect estimates of three- or four-exposure models. Note: , nitrogen dioxide; , oxidative potential (OP) with the dithiothreitol (DTT) assay.
Potential for interaction.
We hypothesized that the association with exposure to air pollution is strongest (increased odds) in the highest road traffic noise quintile and vice versa. Further, we hypothesized that the association with air pollution and road traffic noise is strongest (increased odds) in the lowest surrounding green quintile and that the association with surrounding green is strongest (decreased odds) in the lowest air pollution or road traffic noise quintile. The conditional associations showed some indications for multiplicative interactions in the hypothesized directions between combinations of exposure variables and the odds of diabetes (Table 5). In the lowest quintile, an IQR increase in NDVI was associated with lower odds of diabetes, whereas in the highest quintiles, no significant association of NDVI was observed. The associations of with the odds of diabetes was slightly stronger in the highest road traffic noise quintile compared to the other quintiles. The conditional associations showed no clear pattern of interactions for the odds of hypertension (Table S7). When we assessed interactions using continuous by continuous exposures terms, we found similar patterns as when we used continuous by categorical interaction terms (Table S8).
Table 5.
Multiplicative interactions of surrounding green (NDVI ), air pollution (), and road traffic noise (Lden) on the odds of diabetes.
| Stratified exposure variable | Quintile | Linear exposure variable | ||
|---|---|---|---|---|
| OR (95% CI) | ||||
| NDVI | Road traffic noise (Lden) | |||
| NDVI | Q1 () | — | 1.00 (0.94, 1.05) | 0.98 (0.95, 1.01) |
| Q2 () | — | 1.00 (0.94, 1.06) | 1.02 (0.99, 1.05) | |
| Q3 () | — | 1.08 (1.02, 1.14) | 1.01 (0.98, 1.05) | |
| Q4 () | — | 1.08 (1.02, 1.14) | 1.02 (0.99, 1.06) | |
| Q5 () | — | 1.09 (1.02, 1.15) | 1.00 (0.97, 1.03) | |
| p.inta | — | 0.05 | 0.34 | |
| Q1 () | 0.89 (0.85, 0.93) | — | 1.00 (0.97, 1.02) | |
| Q2 () | 0.88 (0.83, 0.93) | — | 1.00 (0.97, 1.03) | |
| Q3 () | 0.91 (0.86, 0.96) | — | 1.01 (0.97, 1.04) | |
| Q4 () | 0.99 (0.94, 1.05) | — | 1.02 (0.99, 1.05) | |
| Q5 () | 1.04 (0.99, 1.10) | — | 1.00 (0.97, 1.03) | |
| p.inta | — | 0.78 | ||
| Road traffic noise (Lden) | Q1 () | 0.90 (0.86, 0.95) | 1.08 (1.03, 1.13) | — |
| Q2 () | 0.88 (0.84, 0.93) | 1.09 (1.03, 1.14) | — | |
| Q3 () | 0.92 (0.88, 0.97) | 1.08 (1.03, 1.14) | — | |
| Q4 () | 0.92 (0.88, 0.96) | 1.07 (1.02, 1.13) | — | |
| Q5 () | 0.93 (0.90, 0.97) | 1.12 (1.07, 1.17) | — | |
| p.inta | 0.48 | 0.78 | — | |
Note: Results of multiplicative interactions are given as OR (95% CI) per 1-unit increase (IQR for NDVI : 0.13; IQR for : , 5 dB for Lden) in quintiles of the second variable (conditional effects). Models were adjusted for sex, age, marital status, region of origin, education, work, standardized household income, smoking habits, number of cigarettes/day, alcohol consumption, number of alcohol glasses/week, physical activity, body mass index and neighborhood socioeconomic status (SES). —, no data; CI, confidence interval; Lden, daily average noise level; NDVI, Normalized Difference Vegetation Index; , oxidative potential (OP) metric with dithiothreitol (DTT) assay; OR, odds ratio.
p.int shows the -value for the overall interaction.
Mediation Analyses
Based on the results of single-exposure regression models with NDVI surrounding greenness, we only conducted mediation analyses of surrounding greenness with the odds of diabetes. Assuming underlying assumptions of the mediation analyses hold, the association between surrounding greenness and diabetes can be partly explained by decreased levels of or (Table 6). The proportion mediated was higher for NDVI surrounding greenness compared with NDVI. Of the total estimated effect of NDVI, 38% (95% CI: 22, 60) could be explained by decreased concentrations. For NDVI, the proportion mediated (via ) was 27% (95% CI: 13, 44).
Table 6.
Mediation analyses of NDVI surrounding greenness (binary) and mediators and (continuous) on the odds of diabetes.
| Indicator | Mediator | Proportion mediated (95% CI) |
|---|---|---|
| NDVI | 0.27 (0.13, 0.44) | |
| NDVI | 0.20 (0.08, 0.33) | |
| NDVI | 0.38 (0.22, 0.60) | |
| NDVI | 0.34 (0.15, 0.53) |
Note: Models were adjusted for sex, age, marital status, region of origin, education, work, standardized household income, smoking habits, number of cigarettes/day, alcohol consumption, number of alcohol glasses/week, physical activity, body mass index, and neighborhood socioeconomic status (SES). CI, confidence interval; NDVI, Normalized Difference Vegetation Index; , nitrogen dioxide; , oxidative potential (OP) metric with dithiothreitol (DTT) assay.
Discussion
In single-exposure models, we found that surrounding green was associated with decreased odds of diabetes, while exposure to air pollution and road traffic noise was associated with increased odds of diabetes. Road traffic noise was not associated with diabetes after adjustment for air pollution (, ) or surrounding green, whereas associations with surrounding green and air pollution were attenuated but still evident in mutually adjusted models. JORs of combinations of air pollution and decreased surrounding green were higher than the ORs from the single-exposure models for diabetes. Air pollution and surrounding green, but not road traffic noise, were associated with hypertension in single-exposure models. The weak inverse association of surrounding green with hypertension attenuated and lost significance when adjusted for air pollution. Only was associated with stroke and heart attack.
Relationship between Environmental Exposures
Exposures to surrounding green, air pollution, and road traffic noise were, overall, moderately correlated, suggesting that confounding between the three exposures is possible. Because correlations were moderate, multicollinearity of exposures was not an issue in our regression analyses. We were therefore able to study the individual and combined associations of exposure to surrounding green, air pollution, and road traffic noise with cardiometabolic disease.
The moderate negative correlations of surrounding green with air pollutants and road traffic noise that we found were also reported by other studies (Hystad et al. 2014; Thiering et al. 2016; Dadvand et al. 2012). The relationship between surrounding green and air pollution is probably due to several mechanisms. A causal relationship between surrounding green and air pollution could be removal of air pollutants from the air by uptake via leaf stomata or deposition to leaf surfaces, especially of trees. However, according to several studies, this effect is likely small and mainly limited to (Setälä et al. 2013; Tallis et al. 2011; Nowak et al. 2006; Escobedo and Nowak 2009). Moreover, trees could increase air pollution concentrations by reducing dispersion of air pollution, especially in urban canyons. Another more likely explanation for the negative correlation between surrounding green and air pollution is the absence of air pollution sources within green areas (Wesseling et al. 2011).
Exposure to road traffic noise was moderately correlated ( between 0.23 and 0.46) with air pollution exposure in our study. This is in line with other studies, according to a review by Tétreault et al. (2013). Correlations with road traffic noise were higher for pollutants with strong local traffic sources (, ) than for pollutants with lower impact of local traffic (, ). The moderate correlation of road traffic noise and traffic-related air pollutants is likely due to different features of local traffic affecting noise and pollution (Boogaard et al. 2009). Both exposures increase with higher traffic intensity in a street. Lower traffic speed in urban areas is typically associated with lower noise levels but can result in higher air pollution emissions. Road surface will affect traffic noise but not air pollution.
In this study, air pollution and road traffic noise exposures were predicted by models, which are (partly) based on land-use variables. Due to the use of similar land-use predictor variables and models with modest explained variability, correlations between modeled exposures can be higher or lower than between true exposures, respectively. Also, in the LUR model of and in the STAMINA model (road traffic noise) but not in other models, an indicator of green space was included as a (marginal) predictor (Yang et al. 2015; Schreurs et al. 2010), potentially leading to overestimation of the relationship between surrounding green and and road traffic noise. However, the correlation coefficients we found between modeled air pollution and noise exposures are similar to studies that evaluated correlations between measured air pollution and noise exposures in cities (Davies et al. 2009; Allen et al. 2009). Moreover, correlations between measured air pollution concentrations at the Dutch ESCAPE measurement sites and surrounding green and modeled road traffic noise were similar to correlations of modeled air pollution concentrations (Table S9).
Confounding
In our single-exposure models, surrounding green, air pollution, and road traffic noise were associated with diabetes. This is in line with other studies that evaluated exposures to these exposures (Brown et al. 2016; Astell-Burt et al. 2014; Dalton et al. 2016; Eze et al. 2015; Balti et al. 2014; Wang et al. 2014a; Dzhambov 2015).
We found that the association between air pollution and diabetes was confounded by surrounding green, and vice versa. The majority of the studies that evaluated the link between air pollution or surrounding green and diabetes did not adjust for the other exposure (Dalton et al. 2016; Astell-Burt et al. 2014; Ngom et al. 2016; Maas et al. 2009; Eze et al. 2015; Balti et al. 2014). Findings of other studies regarding mutual confounding of surrounding green, air pollution, and noise associations are inconsistent. Eze et al. (2014) reported that the association between and diabetes was attenuated but still positive after adjustment for road traffic noise. However, road traffic noise was not associated with diabetes after adjustment for (Eze et al. 2014). In another study, Eze et al. (2017) found that road traffic noise remained associated with diabetes after adjustment for or surrounding green (which were both not associated with diabetes). Sørensen et al. (2013) showed that road traffic noise exposure remained associated with the odds of diabetes after adjustment for .
The weak association between surrounding green and hypertension that we found in single-exposure models attenuated and lost significance after adjustment for air pollution, whereas adjustments for surrounding green or road traffic noise barely affected associations of air pollution with hypertension. The lack of an association with road traffic noise is in line with a recent meta-analysis (Fuks et al. 2017).
Results of the CRI confirmed the results of our two-exposure models for diabetes and hypertension. The JOR of exposure to a combination of air pollution and decreased surrounding green for diabetes is underestimated by ORs from single-exposure models. As the inclusion of or road traffic noise does not increase the JOR of and decreased NDVI surrounding greenness, a combination of and decreased NDVI surrounding greenness is sufficient to characterize the JOR of combined exposures to air pollution, road traffic noise, and decreased surrounding greenness on diabetes. For hypertension, the CRI showed that the JOR of exposure to a combination of air pollution and decreased surrounding green or the JOR of exposure to air pollution, road traffic noise, and decreased surrounding green is similar to the OR of air pollution from a single-exposure model. Of all environmental exposures, only was associated with stroke and heart attack. Associations of with stroke and heart attack were stronger in the elderly population compared with the full population. This might reflect greater susceptibility and/or reduced exposure misclassification in the elderly, since they may spend more time at or near their residences than younger adults. We did not find any association of surrounding green or road traffic noise with heart attack or stroke. Other studies evaluating associations of surrounding green, air pollution, and road traffic noise with stroke and heart attack morbidity showed mixed results. Some studies found associations with surrounding green or road traffic noise, while others reported no relationship (Atkinson et al. 2013; Babisch 2014; Brown et al. 2016; Cesaroni et al. 2014; Maas et al. 2009; Pereira et al. 2012; Stafoggia et al. 2014; Vienneau et al. 2015). Possible explanations for the different findings are differences in study design, adjustments for covariates, definitions of health outcomes, study populations, and exposure assessment methods (especially for surrounding green).
Interaction
As Hicken et al. (2014) reported that stronger associations of air pollution for people with psychological distress and traffic noise (positively) and surrounding green (inversely) are associated with psychological distress (Seidler et al. 2017; Gascon et al. 2015), we hypothesized that the association with exposure to air pollution is strongest (increased odds) in the highest road traffic noise quintile and vice versa, that the association with air pollution and road traffic noise is strongest (increased odds) in the lowest surrounding green quintile, and that the association with surrounding green is strongest (decreased odds) in the lowest air pollution or road traffic noise quintile. Surrounding green was associated with lower odds of diabetes in areas with lower air pollution levels, but not in areas with high air pollution levels. This could be because surrounding green in low air pollution areas might be more aesthetically attractive and therefore have a stronger impact on psychological stress, which could in turn lead to diabetes. Further, for diabetes, we found a very weak indication for potential effect measure modification between and road traffic noise. Most other studies reported no indications for interactions between air pollution and road traffic noise (Bodin et al. 2016; Sørensen et al. 2013; Selander et al. 2009), except for Sørensen et al. (2014).
Mediation
Assuming underlying assumptions of the mediation analyses hold, the association between NDVI surrounding greenness and diabetes was partly mediated by decreased concentrations of air pollution. The proportion mediated was dependent on the buffer size of surrounding greenness and on the air pollution variable.
The choice to treat air pollution and road traffic noise as confounder or mediator of the surrounding green–health association affects the effect size one should use to evaluate potential health impacts of surrounding green. If air pollution is primarily a confounder, the adjusted slopes for surrounding green from Table 3 (ORs of two-exposure models) should be used. Otherwise, the slopes from Table 2 (ORs of single-exposure models) should be used, and we expect that about 20–38% of the association between surrounding green and diabetes may be related to reduced air pollution. Higher greenness may lead to lower road traffic noise and air pollution concentrations by limiting dispersion by green barriers or by scavenging of air pollution. These mechanisms only provide a partial explanation of the empirical correlation between greenness and air pollution/road traffic noise. A stronger component is that in a greener area, there are fewer sources of air pollution and road traffic noise, and, therefore, pollution is lower. This reflects a common source (or lack thereof) and thus not a causal pathway from green to health.
Surrounding green may affect health via several pathways other than reduced air pollution; it may stimulate physical activity (and thereby reduce overweight) and decrease stress. In our mediation analyses, we adjusted for physical activity and weight status. Yet an estimated direct effect of surrounding green on diabetes remained. This might be due to lower stress levels.
Strengths and Limitations
Strengths of this study include the large population size ( subjects) with national coverage and the ability to adjust for SES and lifestyle factors. Furthermore, we were able to study confounding, interaction (on the multiplicative scale), and mediation of several environmental exposures on diabetes, hypertension, stroke, and heart attack morbidity. We used multiple indicators of surrounding green and air pollution exposure, and all indicators were calculated at the address level. Moreover, all environmental exposures were assessed between 2009 and 2011, i.e., relatively close before the time the survey was administered (2012). The use of recent health and exposure data increases the relevance for current policies.
This study also has limitations. The cross-sectional study is more prone to potential selection bias than longitudinal designs. We had no information about the year of onset of cardiometabolic diseases, and hence, we do not know whether exposures precede the health outcome. The biologically most relevant time period for effects of exposure to the environmental exposures (surrounding green, air pollution, and road traffic noise) and incidence of cardiometabolic outcomes is not well known. For air pollution, the hypothesis is that average exposure in the past 2 y is especially important for cardiometabolic diseases (Schwartz et al. 2008; Puett et al. 2008). Although we characterized exposure by 2009–2010 estimates, studies have shown that the spatial variation of air pollution and traffic noise exposure levels remain stable over periods of about 10 y in Western countries (Eeftens et al. 2011; Fecht et al. 2016). Current exposure estimates hence represent past exposure contrasts. However, subjects may have moved after development of the disease. This residential mobility may lead to some likely nondifferential exposure misclassification and subsequently an underestimation of the associations with health outcomes. Moreover, we did not have time–activity data, which may also lead to exposure error and potentially an underestimation of the associations. Further, we evaluated prevalence of a disease instead of incidence. As a result of their diseases, subjects may have changed their lifestyles.
Another limitation is the use of self-reported health outcomes, which may cause some error due to under- or overreporting. Studies evaluating the validity of self-reported health outcomes showed moderate to very good agreements between questionnaire responses and medical records for diabetes, hypertension, and myocardial infarction; agreements for stroke varied per study (Okura et al. 2004; Schneider et al. 2012; Hansen et al. 2014; Muggah et al. 2013; Machón et al. 2013). Strak et al. (2017) previously reported that 84.9% of this study population with self-reported diabetes has also been prescribed diabetes medication, based on an external dataset. Moreover, they observed similar associations between air pollution and prevalence of diabetes when investigating self-reported physician-diagnosed diabetes and diabetes medication prescription as separate outcomes. Fuks et al. (2017) found that air pollution was associated with self-reported hypertension but not with measured hypertension. The more consistent associations between environmental exposures and diabetes compared with the cardiovascular outcomes could be due to better reporting of the disease. Another explanation is that the exposures could be more strongly associated with fatal cardiovascular events. Several studies found associations of air pollution with fatal heart attacks and strokes but not or less strong with nonfatal heart attacks or strokes (Miller et al. 2007; Sørensen et al. 2014; Puett et al. 2009; Rosenlund et al. 2006, 2008, 2009). The associations reported in this study might be less strong than associations with total () heart attacks and strokes.
In this study, we evaluated the association between modeled exposures to air pollution and road traffic noise and cardiometabolic morbidity. Exposure assessment methods to determine air pollution concentrations and noise levels at residential addresses are well developed and commonly evaluated (Wang et al. 2013, 2014b; Schreurs et al. 2010). However, exposure assessment models may differ in their accuracy to predict the exposure. Performance of the LUR models differed between air pollutants (Table S1) and may have affected associations. A moderate LUR model performance could lead to weaker associations. Further, if LUR models predict air pollution concentrations at residential addresses more precisely than the STAMINA model predicts road traffic noise at residential addresses, it could explain the more robust associations of air pollution exposures in this study. Because of the lack of noise measurements, we cannot test this hypothesis. Surrounding green is measured and not modeled, but a major issue is how well-measured surrounding green reflects biologically relevant green exposure.
We were not able to verify the four important underlying confounding assumptions required for the mediation analyses. However, we included major confounders in our mediation analyses and hence believe that the assumptions are reasonable. We performed a mediation analysis in a cross-sectional analysis. The general limitations of cross-sectional studies with regard to the temporality of exposure–response relationships do not apply to the mediation analysis because we assessed mediation between environmental factors where the relationship is immediate. This would be different when we had performed a mediation analysis with an intermediate health marker (e.g., blood pressure) where the relationship may not be immediate. Further, we did not test for interactions between surrounding green and air pollution in the mediation analyses, as we did not find indications for interpretable interactions in the hypothesized direction in the two-exposure models.
Conclusion
In single-exposure models, we found that surrounding green was associated with decreased odds of diabetes, while exposure to air pollution and road traffic noise was associated with increased odds of diabetes. After adjustment for air pollution (, ) or surrounding green, the association of road traffic noise with diabetes attenuated and lost significance. Two-exposure analyses showed that associations of surrounding green and air pollution with diabetes generally remained, even though they were attenuated. Our results suggest that studies including only one of the correlated exposures (surrounding green, air pollution, and road traffic noise) may overestimate the association of diabetes attributed to that exposure. The joint impact of exposure to a combination of surrounding green and air pollution may be underestimated by the associations from single-exposure models. Future studies would benefit from including multiple environmental exposures to evaluate individual and combined associations.
Supplementary Material
Acknowledgments
This research was carried out in the framework of the National Institute for Public Health and the Environment (RIVM) Strategic Program (SPR; S/121004 HERACLES), in which expertise and innovative projects prepare RIVM to respond to future issues in health and sustainability. The Dutch Public Health Monitor 2012 (Gezondheidsmonitor Volwassenen GGD-en, CBS en RIVM) was conducted by 28 Public Health Services (GGD), Statistics Netherlands (CBS), and the RIVM. Statistical analyses were further facilitated by CBS. The study was approved by the authorized review board. We like to thank D. Houthuijs, M. Schipper, and T. Wiggers for their input.
References
- Allen RW, Davies H, Cohen MA, Mallach G, Kaufman JD, Adar SD. 2009. The spatial relationship between traffic-generated air pollution and noise in 2 US cities. Environ Res 109(3):334–342, PMID: , 10.1016/j.envres.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astell-Burt T, Feng X, Kolt GS. 2014. Is neighborhood green space associated with a lower risk of type 2 diabetes? Evidence from 267,072 Australians. Diabetes Care 37(1):197–201, PMID: , 10.2337/dc13-1325. [DOI] [PubMed] [Google Scholar]
- Atkinson RW, Carey IM, Kent AJ, van Staa TP, Anderson HR, Cook DG. 2013. Long-term exposure to outdoor air pollution and incidence of cardiovascular diseases. Epidemiology 24(1):44–53, PMID: , 10.1097/EDE.0b013e318276ccb8. [DOI] [PubMed] [Google Scholar]
- Babisch W. 2014. Updated exposure-response relationship between road traffic noise and coronary heart diseases: a meta-analysis. Noise Health 16(68):1–9, PMID: , 10.4103/1463-1741.127847. [DOI] [PubMed] [Google Scholar]
- Balti EV, Echouffo-Tcheugui JB, Yako YY, Kengne AP. 2014. Air pollution and risk of type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Res Clin Pract 106(2):161–172, PMID: , 10.1016/j.diabres.2014.08.010. [DOI] [PubMed] [Google Scholar]
- Beelen R, Hoek G, Vienneau D, Eeftens M, Dimakopoulou K, Pedeli X, et al. . 2013. Development of NO 2 and NO x land use regression models for estimating air pollution exposure in 36 study areas in Europe–the ESCAPE project. Atmos Environ 72:10–23, 10.1016/j.atmosenv.2013.02.037. [DOI] [Google Scholar]
- Bodin T, Björk J, Mattisson K, Bottai M, Rittner R, Gustavsson P, et al. . 2016. Road traffic noise, air pollution and myocardial infarction: a prospective cohort study. Int Arch Occup Environ Health 89(5):793–802, PMID: , 10.1007/s00420-016-1115-9. [DOI] [PubMed] [Google Scholar]
- Boogaard H, Borgman F, Kamminga J, Hoek G. 2009. Exposure to ultrafine and fine particles and noise during cycling and driving in 11 Dutch cities. Atmos Environ 43(27):4234–4242, 10.1016/j.atmosenv.2009.05.035. [DOI] [Google Scholar]
- Brown SC, Lombard J, Wang K, Byrne MM, Toro M, Plater-Zyberk E, et al. . 2016. Neighborhood greenness and chronic health conditions in Medicare beneficiaries. Am J Prev Med 51(1):78–89, PMID: , 10.1016/j.amepre.2016.02.008. [DOI] [PubMed] [Google Scholar]
- Cesaroni G, Forastiere F, Stafoggia M, Andersen ZJ, Badaloni C, Beelen R, et al. . 2014. Long term exposure to ambient air pollution and incidence of acute coronary events: prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. BMJ 348:f7412, PMID: , 10.1136/bmj.f7412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crouse DL, Peters PA, Hystad P, Brook JR, van Donkelaar A, Martin RV, et al. . 2015. Ambient PM2.5, O3, and NO2 exposures and associations with mortality over 16 years of follow-up in the Canadian Census Health and Environment Cohort (CanCHEC). Environ Health Perspect 123(11):1180–1186, PMID: , 10.1289/ehp.1409276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crouse DL, Pinault L, Balram A, Hystad P, Peters PA, Chen H, et al. . 2017. Urban greenness and mortality in Canada's largest cities: a national cohort study. Lancet Planet Health 1(7):e289–e297, PMID: , 10.1016/S2542-5196(17)30118-3. [DOI] [PubMed] [Google Scholar]
- Dadvand P, de Nazelle A, Triguero-Mas M, Schembari A, Cirach M, Amoly E, et al. . 2012. Surrounding greenness and exposure to air pollution during pregnancy: an analysis of personal monitoring data. Environ Health Perspect 120(9):1286–1290, PMID: , 10.1289/ehp.1104609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton AM, Jones AP, Sharp SJ, Cooper AJ, Griffin S, Wareham NJ. 2016. Residential neighbourhood greenspace is associated with reduced risk of incident diabetes in older people: a prospective cohort study. BMC Public Health 16(1):1171, PMID: , 10.1186/s12889-016-3833-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies HW, Vlaanderen JJ, Henderson SB, Brauer M. 2009. Correlation between co-exposures to noise and air pollution from traffic sources. Occup Environ Med 66.5:347–350, PMID: , 10.1136/oem.2008.041764. [DOI] [PubMed] [Google Scholar]
- Dzhambov AM. 2015. Long-term noise exposure and the risk for type 2 diabetes: a meta-analysis. Noise Health 17(74):23–33, PMID: , 10.4103/1463-1741.149571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzhambov A, Markevych I, Tilov B, Arabadzhiev Z, Stoyanov D, Gatseva P, et al. . 2018. Lower noise annoyance associated with GIS-derived greenspace: pathways through perceived greenspace and residential noise. Int J Environ Res Public Health 15(7):E1533, 10.3390/ijerph15071533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eeftens M, Beelen R, de Hoogh K, Bellander T, Cesaroni G, Cirach M, et al. . 2012. Development of land use regression models for PM2.5, PM2.5 absorbance, PM10 and PMcoarse in 20 European study areas; results of the ESCAPE project. Environ Sci Technol 46(20):11195–11205, PMID: , 10.1021/es301948k. [DOI] [PubMed] [Google Scholar]
- Eeftens M, Beelen R, Fischer P, Brunekreef B, Meliefste K, Hoek G. 2011. Stability of measured and modelled spatial contrasts in NO2 over time. Occup Environ Med 68(10):765–770, PMID: , 10.1136/oem.2010.061135. [DOI] [PubMed] [Google Scholar]
- Escobedo FJ, Nowak DJ. 2009. Spatial heterogeneity and air pollution removal by an urban forest. Landsc Urban Plan 90(3–4):102–110, 10.1016/j.landurbplan.2008.10.021. [DOI] [Google Scholar]
- EU Directive. 2002. Directive 2002/49/EC of the European Parliament and the Council of 25 June 2002 relating to the assessment and management of environmental noise. J European Communities 189:12–25. [Google Scholar]
- Eze IC, Foraster M, Schaffner E, Vienneau D, Héritier H, Rudzik F, et al. . 2017. Long-term exposure to transportation noise and air pollution in relation to incident diabetes in the SAPALDIA study. Int J Epidemiol 46(4):1115–1125, PMID: , 10.1093/ije/dyx020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eze IC, Hemkens LG, Bucher HC, Hoffmann B, Schindler C, Künzli N, et al. . 2015. Association between ambient air pollution and diabetes mellitus in Europe and North America: systematic review and meta-analysis. Environ Health Perspect 123(5):381–389, PMID: , 10.1289/ehp.1307823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eze IC, Schaffner E, Fischer E, Schikowski T, Adam M, Imboden M, et al. . 2014. Long-term air pollution exposure and diabetes in a population-based Swiss cohort. Environ Int 70:95–105, PMID: , 10.1016/j.envint.2014.05.014. [DOI] [PubMed] [Google Scholar]
- Fecht D, Hansell AL, Morley D, Dajnak D, Vienneau S, Beevers MB, et al. . 2016. Spatial and temporal associations of road traffic noise and air pollution in London: implications for epidemiological studies. Environ Int 88:235–242, PMID: , 10.1016/j.envint.2015.12.001. [DOI] [PubMed] [Google Scholar]
- Floud S, Blangiardo M, Clark C, de Hoogh K, Babisch W, Houthuijs D, et al. . 2013. Exposure to aircraft and road traffic noise and associations with heart disease and stroke in six European countries: a cross-sectional study. Environ Health 12:89, PMID: , 10.1186/1476-069X-12-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox J, Monette G. 1992. Generalized collinearity diagnostics. J Am Stat Assoc 87(417):178–183, 10.2307/2290467. [DOI] [Google Scholar]
- Fuks KB, Weinmayr G, Foraster M, Dratva J, Hampel R, Houthuijs D, et al. . 2014. Arterial blood pressure and long-term exposure to traffic-related air pollution: an analysis in the European Study of Cohorts for Air Pollution Effects (ESCAPE). 122(9):896–905, PMID: , 10.1289/ehp.1307725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuks KB, Weinmayr G, Basagaña X, Gruzieva O, Hampel R, Oftedal B, et al. . 2017. Long-term exposure to ambient air pollution and traffic noise and incident hypertension in seven cohorts of the European study of cohorts for air pollution effects (ESCAPE). Eur Heart J 38(13):983–990, PMID: , 10.1093/eurheartj/ehw413. [DOI] [PubMed] [Google Scholar]
- Gascon M, Sánchez-Benavides G, Dadvand P, Martínez D, Gramunt N, Gotsens X, et al. . 2018. Long-term exposure to residential green and blue spaces and anxiety and depression in adults: a cross-sectional study. Environ Res 162:231–239, PMID: , 10.1016/j.envres.2018.01.012. [DOI] [PubMed] [Google Scholar]
- Gascon M, Triguero-Mas M, Martínez D, Dadvand P, Forns J, Plasència A, et al. . 2015. Mental health benefits of long-term exposure to residential green and blue spaces: a systematic review. Int J Environ Res Public Health 12(4):4354–4379, PMID: , 10.3390/ijerph120404354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen H, Schäfer I, Schön G, Riedel-Heller S, Gensichen J, Weyerer S, et al. . 2014. Agreement between self-reported and general practitioner-reported chronic conditions among multimorbid patients in primary care-results of the MultiCare cohort study. BMC Fam Pract 15(1):39, PMID: , 10.1186/1471-2296-15-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartig T, Mitchell R, de Vries S, Frumkin H. 2014. Nature and health. Annu Rev Public Health 35:207–228, PMID: , 10.1146/annurev-publhealth-032013-182443. [DOI] [PubMed] [Google Scholar]
- Hicken MT, Dvonch JT, Schulz AJ, Mentz G, Paul J. 2014. Fine particulate matter air pollution and blood pressure: The modifying role of psychosocial stress. Environ Res 133:195–203, PMID: , 10.1016/j.envres.2014.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hystad P, Davies HW, Frank L, Van Loon J, Gehring U, Tamburic L, et al. . 2014. Residential greenness and birth outcomes: evaluating the influence of spatially correlated built-environment factors. Environ Health Perspect 122(10):1095–1102, PMID: , 10.1289/ehp.1308049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai K, Keele L, Tingley D. 2010. A general approach to causal mediation analysis. Psychol Methods 15(4):309–334, PMID: , 10.1037/a0020761. [DOI] [PubMed] [Google Scholar]
- James P, Hart JE, Banay RF, Laden F. 2016. Exposure to greenness and mortality in a nationwide prospective cohort study of women. Environ Health Perspect 124(9):1344–1352, PMID: , 10.1289/ehp.1510363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerrett M, Burnett RT, Beckerman BS, Turner MC, Krewski D, Thurston G, et al. . 2013. Spatial analysis of air pollution and mortality in California. Am J Respir Crit Care Med 188(5):593–599, PMID: , 10.1164/rccm.201303-0609OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadaster. 2010. TOP10NL Database. https://www.kadaster.com/automatic-generalisation [accessed 20 January 2016].
- Klompmaker JO, Hoek G, Bloemsma LD, Gehring U, Strak M, Wijga AH, et al. . 2017. Green space definition affects associations of green space with overweight and physical activity. Environ Res 160:531–540, PMID: , 10.1016/j.envres.2017.10.027. [DOI] [PubMed] [Google Scholar]
- Knol FA. 1998. Van hoog naar laag; van laag naar hoog: de sociaal-ruimtelijke ontwikkeling van wijken tussen 1971–1995 (in Dutch). The Hague, the Netherlands: Sociaal en Cultureel Planbureau.
- Lippmann M, Chen LC, Gordon T, Ito K, Thurston GD. 2013. National Particle Component Toxicity (NPACT) Initiative: integrated epidemiologic and toxicologic studies of the health effects of particulate matter components. Res Rep Health Eff Inst (177):5–13, PMID: . [PubMed] [Google Scholar]
- Maas J, Verheij RA, de Vries S, Spreeuwenberg P, Schellevis FG, Groenewegen PP. 2009. Morbidity is related to a green living environment. J Epidemiol Community Health 63(12):967–973, PMID: , 10.1136/jech.2008.079038. [DOI] [PubMed] [Google Scholar]
- Machón M, Arriola L, Larrañaga N, Amiano P, Moreno-Iribas C, Agudo A, et al. . 2013. Validity of self-reported prevalent cases of stroke and acute myocardial infarction in the Spanish cohort of the EPIC study. J Epidemiol Community Health 67(1):71–75, PMID: , 10.1136/jech-2011-200104. [DOI] [PubMed] [Google Scholar]
- Markevych I, Schoierer J, Hartig T, Chudnovsky A, Hystad P, Dzhambov AM, et al. . 2017. Exploring pathways linking greenspace to health: theoretical and methodological guidance. Environ Res 158:301–317, PMID: , 10.1016/j.envres.2017.06.028. [DOI] [PubMed] [Google Scholar]
- Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL, et al. . 2007. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med 356(5):447–458, PMID: , 10.1056/NEJMoa054409. [DOI] [PubMed] [Google Scholar]
- Muggah E, Graves E, Bennett C, Manuel DG. 2013. Ascertainment of chronic diseases using population health data: a comparison of health administrative data and patient self-report. BMC Public Health 13:16, PMID: , 10.1186/1471-2458-13-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Münzel T, Sørensen M, Gori T, Schmidt FP, Rao X, Brook J, et al. . 2016a. Environmental stressors and cardio-metabolic disease: part I–epidemiologic evidence supporting a role for noise and air pollution and effects of mitigation strategies. Eur Heart J 38(8):550–556, PMID: , 10.1093/eurheartj/ehw269. [DOI] [PubMed] [Google Scholar]
- Münzel T, Sørensen M, Gori T, Schmidt FP, Rao X, Brook FR, et al. . 2016b. Environmental stressors and cardio-metabolic disease: part II–mechanistic insights. Eur Heart J 38(8):557–564, PMID: , 10.1093/eurheartj/ehw294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngom R, Gosselin P, Blais C, Rochette L. 2016. Type and proximity of green spaces are important for preventing cardiovascular morbidity and diabetes—a cross-sectional study for Quebec, Canada. Int J Environ Res Public Health 13(4):423, PMID: , 10.3390/ijerph13040423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nieuwenhuijsen MJ, Khreis H, Triguero-Mas M, Gascon M, Dadvand P. 2017. Fifty shades of green: pathway to healthy urban living. Epidemiology 28(1):63–71, PMID: , 10.1097/EDE.0000000000000549. [DOI] [PubMed] [Google Scholar]
- Nowak DJ, Crane DE, Stevens JC. 2006. Air pollution removal by urban trees and shrubs in the United States. Urban For Urban Green 4(3–4):115–123, 10.1016/j.ufug.2006.01.007. [DOI] [Google Scholar]
- Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. 2004. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol 57(10):1096–1103, PMID: , 10.1016/j.jclinepi.2004.04.005. [DOI] [PubMed] [Google Scholar]
- Pereira G, Foster S, Martin K, Christian H, Boruff BJ, Knuiman M, et al. . 2012. The association between neighborhood greenness and cardiovascular disease: an observational study. BMC Public Health 12:466, PMID: , 10.1186/1471-2458-12-466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puett RC, Hart JE, Yanosky JD, Paciorek C, Schwartz J, Suh H, et al. . 2009. Chronic fine and coarse particulate exposure, mortality, and coronary heart disease in the Nurses’ Health Study. Environ Health Perspect 117(11):1697–1701, PMID: , 10.1289/ehp.0900572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puett RC, Schwartz J, Hart JE, Yanosky JD, Speizer FE, Suh H, et al. . 2008. Chronic particulate exposure, mortality, and coronary heart disease in the nurses’ health study. Am J Epidemiol 168(10):1161–1168, PMID: , 10.1093/aje/kwn232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenlund M, Bellander T, Nordquist T, Alfredsson L. 2009. Traffic-generated air pollution and myocardial infarction. Epidemiology 20(2):265–271, PMID: , 10.1097/EDE.0b013e318190ea68. [DOI] [PubMed] [Google Scholar]
- Rosenlund M, Berglind N, Pershagen G, Hallqvist J, Jonson T, Bellander T. 2006. Long-term exposure to urban air pollution and myocardial infarction. J Epidemiology 17(4):383–390, PMID: , 10.1097/01.ede.0000219722.25569.0f. [DOI] [PubMed] [Google Scholar]
- Rosenlund M, Picciotto S, Forastiere F, Stafoggia M, Perucci CA. 2008. Traffic-related air pollution in relation to incidence and prognosis of coronary heart disease. Epidemiology 19(1):121–128, PMID: , 10.1097/EDE.0b013e31815c1921. [DOI] [PubMed] [Google Scholar]
- Schneider AL, Pankow JS, Heiss G, Selvin E. 2012. Validity and reliability of self-reported diabetes in the atherosclerosis risk in communities study. Am J Epidemiol 176(8):738–743, PMID: , 10.1093/aje/kws156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreurs EM, Jabben J, Verheijen ENG. 2010. STAMINA-Model Description, Standard Model Instrumentation for Noise Assessments. RIVM Report 680740003/2010. Bilthoven, Netherlands: National Institute for Public Health and the Environment (RIVM). [Google Scholar]
- Schwartz J, Coull B, Laden F, Ryan L. 2008. The effect of dose and timing of dose on the association between airborne particles and survival. Environ Health Perspect 116(1):64–69, PMID: , 10.1289/ehp.9955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidler A, Hegewald J, Seidler AL, Schubert M, Wagner M, Dröge P, et al. . 2017. Association between aircraft, road and railway traffic noise and depression in a large case-control study based on secondary data. Environ Res 152:263–271, PMID: , 10.1016/j.envres.2016.10.017. [DOI] [PubMed] [Google Scholar]
- Selander J, Nilsson ME, Bluhm G, Rosenlund M, Lindqvist M, Nise G, et al. . 2009. Long-term exposure to road traffic noise and myocardial infarction. Epidemiology 20(2):272–279, PMID: , 10.1097/EDE.0b013e31819463bd. [DOI] [PubMed] [Google Scholar]
- Setälä H, Viippola V, Rantalainen A-L, Pennanen A, Yli-Pelkonen V. 2013. Does urban vegetation mitigate air pollution in northern conditions? Environ Pollut 183:104–112, PMID: , 10.1016/j.envpol.2012.11.010. [DOI] [PubMed] [Google Scholar]
- Sørensen M, Andersen ZJ, Nordsborg RB, Becker T, Tjønneland A, Overvad K, et al. . 2013. Long-term exposure to road traffic noise and incident diabetes: a cohort study. Environ Health Perspect 121(2):217–222, PMID: , 10.1289/ehp.1205503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sørensen M, Lühdorf P, Ketzel M, Andersen ZJ, Tjønneland A, Overvad K, et al. . 2014. Combined effects of road traffic noise and ambient air pollution in relation to risk for stroke? Environ Res 133:49–55, PMID: , 10.1016/j.envres.2014.05.011. [DOI] [PubMed] [Google Scholar]
- Stafoggia M, Cesaroni G, Peters A, Andersen ZJ, Badaloni C, Beelen R, et al. . 2014. Long-term exposure to ambient air pollution and incidence of cerebrovascular events: results from 11 European cohorts within the ESCAPE project. Environ Health Perspect 122(9):919–925, PMID: , 10.1289/ehp.1307301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Netherlands. 2015. Opbouw en instructie totaalbestand Gezondheidsmonitor Volwassenen 2012. https://www.cbs.nl/nl-nl/onze-diensten/methoden/onderzoeksomschrijvingen/korte-onderzoeksbeschrijvingen/gezondheidsmonitor [accessed 3 November 2015].
- Strak M, Janssen N, Beelen R, Schmitz O, Vaartjes I, Karssenberg D, et al. . 2017. Long-term exposure to particulate matter, NO2 and the oxidative potential of particulates and diabetes prevalence in a large national health survey. Environ Int 108:228–236, PMID: , 10.1016/j.envint.2017.08.017. [DOI] [PubMed] [Google Scholar]
- Tallis M, Taylor G, Sinnett D, Freer-Smith P. 2011. Estimating the removal of atmospheric particulate pollution by the urban tree canopy of London, under current and future environments. Landsc Urban Plan 103(2):129–138, 10.1016/j.landurbplan.2011.07.003. [DOI] [Google Scholar]
- Tétreault LF, Perron S, Smargiassi A. 2013. Cardiovascular health, traffic-related air pollution and noise: are associations mutually confounded? A systematic review. Int J Public Health 58(5):649–666, PMID: , 10.1007/s00038-013-0489-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiering E, Markevych I, Brüske I, Fuertes E, Kratzsch J, Sugiri D, et al. . 2016. Associations of residential long-term air pollution exposures and satellite-derived greenness with insulin resistance in German adolescents. Environ Health Perspect 124(8):1291–1298, PMID: , 10.1289/ehp.1509967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. 2014. Mediation: R package for causal mediation analysis. J Stat Softw 59(5):1–38, 10.18637/jss.v059.i05.26917999 [DOI] [Google Scholar]
- Van Kempen E, Babisch W. 2012. The quantitative relationship between road traffic noise and hypertension: a meta-analysis. J Hypertens 30(6):1075–1086, PMID: , 10.1097/HJH.0b013e328352ac54. [DOI] [PubMed] [Google Scholar]
- VanderWeele TJ. 2016. Mediation analysis: a practitioner's guide. Annu Rev Public Health 37:17–32, PMID: , 10.1146/annurev-publhealth-032315-021402. [DOI] [PubMed] [Google Scholar]
- Vienneau D, Schindler C, Perez L, Probst-Hensch N, Röösli M. 2015. The relationship between transportation noise exposure and ischemic heart disease: a meta-analysis. Environ Res 138:372–380, PMID: , 10.1016/j.envres.2015.02.023. [DOI] [PubMed] [Google Scholar]
- Villeneuve PJ, Jerrett M, Su JG, Burnett RT, Chen H, Wheeler AJ, et al. . 2012. A cohort study relating urban green space with mortality in Ontario, Canada. Environ Res 115:51–58, PMID: , 10.1016/j.envres.2012.03.003. [DOI] [PubMed] [Google Scholar]
- Wang M, Beelen R, Basagana X, Becker T, Cesaroni G, de Hoogh K, et al. . 2013. Evaluation of land use regression models for NO2 and particulate matter in 20 European study areas: the ESCAPE project. Environ Sci Technol 47(9):4357–4364, PMID: , 10.1021/es305129t. [DOI] [PubMed] [Google Scholar]
- Wang M, Beelen R, Bellander T, Birk M, Cesaroni G, Cirach M, et al. . 2014a. Performance of multi-city land use regression models for nitrogen dioxide and fine particles. Environ Health Perspect 122(8):843–849, PMID: , 10.1289/ehp.1307271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B, Xu D, Jing Z, Liu D, Yan S, Wang Y. 2014b. Mechanisms in endocrinology: effect of long-term exposure to air pollution on type 2 diabetes mellitus risk: a systemic review and meta-analysis of cohort studies. Eur J Endocrinol 171(5):R173–R82, PMID: , 10.1530/EJE-14-0365. [DOI] [PubMed] [Google Scholar]
- Wesseling J, van der Zee S, van Overveld A. 2011. Het effect van vegetatie op de luchtkwaliteit: Update 2011. RIVM Rapport 680705019. Bilthoven, Netherlands: National Institute for Public Health and the Environment (RIVM). [Google Scholar]
- Yang A, Wang M, Eeftens M, Beelen R, Dons E, Leseman DL, et al. . 2015. Spatial variation and land use regression modeling of the oxidative potential of fine particles. Environ Health Perspect 123(11):1187–1192, PMID: , 10.1289/ehp.1408916. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.